Abstract
Background
Conversion to open cholecystectomy is still required in some patients. The aim of this study was to evaluate preoperative factors associated with conversion to open cholecystectomy in elective cholecystectomy and acute cholecystitis.
Methods
The records of 1,804 patients who underwent cholecystectomy from May 1992 to January 2004 were reviewed retrospectively. The demographics and preoperative data of patients who required conversion to laparotomy were compared to those with successful laparoscopic cholecystectomy.
Results
Conversion to open cholecystectomy was needed in 94 patients (5.2%),of which 44 (2.8%) had no inflammation and 50 (18.4%) had acute inflammation of the gallbladder. Male gender, age older than 60 years, previous upper abdominal surgery, diabetes, and severity of inflammation were all significantly correlated with an increased conversion rate to laparotomy. Also, the conversion from laparoscopic to open cholecystectomy in acute cholecystitis patients was associated with greater white blood cell count, fever, elevated total bilirubin, aspartate transaminase, and alanine transaminase levels, and the various types of inflammation.
Conclusions
None of these risk factors were contraindications to laparoscopic cholecystectomy. This may help predict the difficulty of the procedure and permit the surgeon to better inform patients about the risk of conversion from laparoscopic to open cholecystectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopic cholecystectomy (LC) has become the treatment of choice for gallstones [24]. However, technical difficulties can make the conversion to open cholecystectomy inevitable, the consequences of which may overshadow all advantages of the laparoscopic procedure, making this approach unsafe, uneconomical and inefficient. Determining variables associated with the risk of conversion would be useful for evaluating patients preoperatively, thus avoiding wasteful laparoscopic attempts by proceeding directly to an open operation. Unfortunately, the reported factors indicating a risk for conversion from laparoscopic to open cholecystectomy have been inconsistent.
The aim of this study was to define predictive factors of conversion in unselected patients who had undergone an LC in elective and acute cases.
Materials and methods
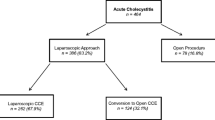
We analyzed the data of 1,804 consecutive patients who underwent LC between May 1992 and January 2004 in the Second Department of Surgery at Alexandroupolis University Hospital. The clinical presentations were symptomatic cholelithiasis in 1,510 patients, acute cholecystitis in 272, and gallbladder polyps in 22. The clinical diagnosis of acute cholecystitis was based on the presence of right upper quadrant pain, fever, elevated white blood cell count (WBC >9,000/cc), signs of inflammation on ultrasound, and operative findings. The diagnosis of empyema or hydrops of the gallbladder was based on the presence of pus or mucus in the gallbladder when aspirated laparoscopically. The severity of acute cholecystitis was then classified as acute edematous cholecystitis, hydrops, or suppurative cholecystitis. All the resected specimens were examined histopathologically, which revealed correlations between clinical diagnosis and histopathology of 83% for acute cholecystitis and 78.4% for empyema. In the elective group, all gallbladders showed features of chronic cholecystitis.
Data included gender, age, history of acute cholecystitis or pancreatitis, previous abdominal surgery, fever, body mass index (BMI), and concomitant disease (ischemic heart disease, diabetes mellitus, or hypertension). Fever was defined as a temperature of at least 37.5°C. Preoperative laboratory analysis included WBC count, and total serum bilirubin, aspartate transaminase, and alanine transaminase levels, WBC counts were dichotomized at 9,000/ml.
Patients were categorized by age as < 40, 40–60, and > 60 years. We also divided previous abdominal surgery into upper and lower abdominal surgery. BMI values were grouped as ≤ 24.9, 25.0–29.9, and ≥ 30 kg/m2
The LC was performed using a standard four-puncture technique in all patients. Pneumoperitoneum was created using a Veress needle except in a few patients who had previously undergone a midline incision and in those with suspected adhesions, in whom it was created using the Hasson technique. Intraoperative cholangiography was also performed selectively in patients with uncertain anatomy, suspicion of stone at the common bile duct, or common bile duct injury.
Statistical analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences, version 11.0 (SPSS, Chicago, IL, USA). Categorical variables are expressed as frequencies (and percentage), and continuous variables are expressed as the mean ± standard deviation. The chi-square test was used to evaluate potential associations between categorical variables, whereas odds ratios (ORs) and 95% confidence intervals (CIs) were calculated using simple logistic regression analysis. A multivariate stepwise logistic regression model was constructed to explore the independent effect of variables that showed a significant influence on conversion by univariate analysis. The patient’s gender, age, severity of inflammation, diabetes, and history of previous upper or lower abdominal surgery were included as independent variables. All tests were two tailed, and statistical significance was defined as p <0.05.
Results
A total of 1,804 patients underwent LC between May 1992 and January 2004 [1,379 females (76.4%) and 425 males (23.6%)]. The age of the patients was 52.66 ± 14.66 years (range, 15–87); females were aged 51.45 ± 14.81 years (range, 16–87), whereas males were aged 56.60 ± 13.55 years (range, 15–86).
Conversion to open surgery occurred in 94 patients (5.2%), of which 44 (2.8%) had no inflammation and 50 (18.41%) had acute inflammation of the gallbladder. The reasons for conversion to open cholecystectomy are summarized in Table 1. The most common reason for conversion was the inability to define the anatomy in Calot’s triangle (n = 70); 24 (1.5 %) of these cases had no inflammation and 46 (16.9%) had an inflamed gallbladder. The other cases of conversion (n = 24) involved bleeding from cystic artery (n = 3), common bile duct injury (n = 2), cancer of the gallbladder (n = l), polyps of the gallbladder (n = l), cholecystoduodenal fistula (n = 6), spilled stone (n=2), and inadequately created pneumoperitoneum (n = 9). There were no cases of injury to major vessels or death.
The various preoperative characteristics correlating with conversion are shown in Table 2. Significant predictors of conversion based on univariate analysis were male gender (p = 0.027), higher age (p = 0.001), diabetes (p < 0.001), previous upper abdominal surgery (p < 0.001), and severity of inflammation. There was no relationship between the likelihood of conversion and BMI (p = 0.913), cardiovascular disease (p = 0.404), hypertension (p = 0.992), or history of acute cholecystitis or pancreatitis (p = 0.407).
Multivariate analysis with a multiple logistic regression model showed that the significantly independent predictive factors for conversion were increased age, severity of inflammation, and previous upper abdominal surgery (Table 3). Predictors of conversion to open cholecystectomy were age >60 years (OR, 4.74; 95% CI, 2.08–0.67; P < 0.001), severity of inflammation (OR, 7.07;95% CI, 4.49–11.14; p < 0.001), and previous upper abdominal surgery (OR, 3.36;95% CI, 1.49–7.57; P = 0.003).
The same analysis restricted to the patients with inflamed gallbladder showed that the following factors were predictive of conversion to open cholecystectomy: male gender (p = 0.016), increasing age (p = 0.035), elevated WBC count (p = 0.041), fever (p < 0.001), total bilirubin > 1.2 mg/dl (p = 0.033), aspartate transaminase > 60 U/L (p < 0.001), alanine transaminase >60 U/L (p = 0.002), degree of inflammation (p = 0.048), history of diabetes (p < 0.001), and previous upper abdominal surgery (p = 0.027) (Table 4).
Multivariate analysis with a multiple logistic regression model showed that the significantly independent predictive factors for conversion in patients with inflamed gallbladder were male gender (p = 0.047), increased age (p = 0.039), severity of inflammation (p = 0.0048), fever (p = 0.009), and elevated WBC count (p = 0.035).
Discussion
Laparoscopic cholecystectomy (LC) is accepted as the gold standard treatment for symptomatic cholelithiasis [4, 24], shown to have a lower morbidity, a less painful postoperative, course a shorter hospital stay, earlier recovery, quicker resumption of normal activities, and improved cosmesis compared to open cholecystectomy [6, 15, 25]. More recently, LC has gained acceptance as the surgical treatment for acute cholecystitis [13, 16, 17, 19, 26]. However, the risk of conversion to open cholecystectomy is always present.
The acceptable conversion rate in patients who undergo an elective LC is 3–5% [2, 5], and that for acute cholecystitis is 6–35% [14, 20]. In our study, the conversion rate was 2.9% for elective LC and 18.4% for acute cholecystitis. We do not consider conversion as failure but rather as a prudent and purposeful alteration of the operative plan due to anatomic problems that avoids further complications.
Patients treated successfully by the laparoscopic approach were younger than 60 years, irrespective of whether they presented with uncomplicated cholecystolithiasis or with acute cholecystitis. Increased age has been consistently noted in the literature as a preoperative risk factor for conversion, [9, 22], perhaps due to a longer history of gallstones and increased number of cholecystitis attacks [9, 18, 22]. Several authors claim that being male does not affect the conversion rate [9, 23], whereas others (including us) have found such a correlation. The underlying reason is unclear but it may be attributable to men being less likely than women to seek medical attention [3, 27].
Diabetes and previous upper abdominal surgery also affected the conversion rate. Previous abdominal surgery was a factor predicting the necessity for conversion from laparoscopic to open cholecystectomy, but the majority of adhesions from prior abdominal surgery do not alter the anatomy of the abdominal right upper quadrant so it does not negatively impact the likelihood of a successful LC. However, previous upper abdominal surgery is associated with an increased need for adhesiolysis, a higher open conversion rate, and a prolonged operating time. Diabetes mellitus was associated with increased conversion rates in our study, whereas others have not reported such correlation, [1, 12, 22]. Such a relationship is perhaps due to the presence of acute inflammation or changes in the wall from microvascular diseases.
Obesity, especially morbid obesity, is reported as a risk hazard factor in conversion to open cholecystectomy [9, 11]. We did not corroborate this finding, although obesity was one of the factors affecting the operating time required for gallbladder dissection.
LC in acute cholecystitis is safe and feasibility as reported in numerous publications [7, 8, 10, 21]. The high rates of conversion from laparoscopic to open cholecystectomy for acute cholecystitis result from the technical difficulty of managing severe inflammatory adhesions around the acutely inflamed gallbladder, making dissection of Calot’s triangle and recognition of the anatomy more hazardous. In our series, the overall conversion rate was 18.4% for acute cholecystitis and was an independent predictor of conversion. The conversion rates according to pathology were 14.0% for acute cholecystitis, 15.5% for hydrops (mucocele), and 25.8% for empyema of the gallbladder, suggesting that the conversion rate varies with the form of acute cholecystitis.
In our study, we also found that the conversion rates in patients with acute inflammation of the gallbladder were associated with fever and laboratory data. Specifically, a temperature of >37.5°C increased the likelihood of conversion 10-fold, a WBC count >9000/ml and total bilirubin >1.2 mg/dl doubled it, and aspartate transaminase and alanine transaminase levels of >60 U/L tripled it. Factors independently associated with conversion when LC was attempted for acute cholecystitis include male patients, age older than, 60 years, increased WBC count ( >9,000/ml), severity of inflammation, and temperature higher than 37.5°C.
In conclusion, none of the risk factors assessed are contraindications, to LC, but they may help to predict the difficulty of the procedure. This would permit the surgeon to better inform patients about the risk of conversion from laparoscopic to open cholecystectomy. The decision about when to convert to open cholecystectomy is made by the surgeon during the course of the procedure on an individual and often subjective basis
References
A Alponat CK Kum BC Koh A Rajnakova PM Goh (1997) ArticleTitlePredictive factors for conversion of laparoscopic cholecystectomy World J Surg 21 629–633 Occurrence Handle9230661
G Berci JM Sackier (1991) ArticleTitleThe Los Angeles experience with laparoscopic cholecystectomy Am J Surg 161 382–384 Occurrence Handle10.1016/0002-9610(91)90602-A Occurrence Handle1825762
A Bickel A Rappaport V Kanievski I Vaksman M Haj N Geron A Eitan (1996) ArticleTitleLaparoscopic management of acute cholecystitis: prognostic factors for success Surg Endosc 10 1045–1049 Occurrence Handle10.1007/s004649900237 Occurrence Handle8881049
R Bittner (2004) ArticleTitleThe standard of laparoscopic cholecystectomy Langenbecks Arch Surg 389 157–163 Occurrence Handle10.1007/s00423-004-0471-1 Occurrence Handle15188083
A Cuschieri F Dubois J Mouiel P Mouret H Becker G Buess M Trede H Troidl (1991) ArticleTitleThe European experience with laparoscopic cholecystectomy Am J Surg 161 385–387 Occurrence Handle10.1016/0002-9610(91)90603-B Occurrence Handle1825763
DD Deizel KW Millikan SG Economou A Doolas S-T Ko MC Airan (1993) ArticleTitleComplications of laparoscopic cholecystectomy: a national survey of 4,292 hospitals and analysis of 77,604 cases Am J Surg 165 9–14 Occurrence Handle8418705
CA Del Pin ParticleDel KS Arthur C Honig EM Silverman (2002) ArticleTitleLaparoscopic cholecystectomy: relationship of pathology and operative time JSLS 6 149–154 Occurrence Handle12113419
S Eldar HT Siegelnann D Buzaglo I Matter A Cohen E Sabo J Abrahamson (2002) ArticleTitleConversion of laparoscopic cholecystectomy to open cholecystectomy in acute cholecystitis: artificial neural networks improve the prediction of conversion World J Surg 26 79–85 Occurrence Handle10.1007/s00268-001-0185-2 Occurrence Handle11898038
GM Fried JS Barkun HH Sigman L Joseph D Clas J Garzon EJ Hinchey JL Meakins (1994) ArticleTitleFactors determining conversion to laparotomy in patients undergoing laparoscopic cholecystectomy Am J Surg 167 35–39 Occurrence Handle10.1016/0002-9610(94)90051-5 Occurrence Handle8311138
LE Hammarstrom S Mellander H Rudstrom (2001) ArticleTitleA prognostic index of unsuccessful laparoscopic cholecystectomy for acute calculous cholecystitis Int J Surg Invest 2 387–392
CH Hutchinson LW Traverse FT Lee (1994) ArticleTitleLaparoscopic cholecystectomy. Do preoperative factors predict the need to convert to open? Surg Endosc 8 875–878 Occurrence Handle10.1007/BF00843458 Occurrence Handle7992153
S Kanaan K Murayama L Merriam L Dawes J Prystowsky R Rege R Joehl (2002) ArticleTitleRisk factors for conversion of laparoscopic to open cholecystectomy J Surg Res 106 20–24 Occurrence Handle10.1006/jsre.2002.6393 Occurrence Handle12127803
C-K Kum E Eypasch R Lefering D Math A Paul E Neugebauer H Troidl (1996) ArticleTitleLaparoscopic cholecystectomy for acute cholecystitis: Is it really safe? World J Surg 20 43–49 Occurrence Handle10.1007/s002689900008 Occurrence Handle8588411
PB Lai KH Kwong KL Leung SP Kwok AC Chan SC Chung WY Lau (1998) ArticleTitleRandomized trial of early versus delayed laparoscopic cholecystectomy for acute cholecystitis Br J Surg 85 764–767 Occurrence Handle10.1046/j.1365-2168.1998.00708.x Occurrence Handle9667702
CM Lo CL Liu ECS Lai ST Fan J Wong (1996) ArticleTitleEarly versus delayed laparoscopic cholecystectomy for treatment of acute cholecystitis Ann Surg 223 37–42 Occurrence Handle10.1097/00000658-199601000-00006 Occurrence Handle8554416
JA Lujan P Parrilla R Robles JA Torralba J Garcia Ayllon R Liron F Sanchez- Bueno (1995) ArticleTitleLaparoscopic cholecystectomy in the treatment of acute cholecystitis J Am Coll Surg 181 75–77 Occurrence Handle7599776
B Navez D Mutter Y Russier M Vix F Jamali D Lipski E Cambler P Guiot J Leroy J Marescaux (2001) ArticleTitleSafety of laparoscopic approach for acute cholecystitis: retrospective study of 609 cases World J Surg 25 1352–1356 Occurrence Handle10.1007/s00268-001-0122-4 Occurrence Handle11596902
JH Peter W Krailadsiri R Incarbone CG Bremner E Froes AP Ireland P Crookes AE Ortega GA Anthone SA Stain (1994) ArticleTitleReasons for conversion from laparoscopic to open cholecystectomy in an urban teaching hospital Am J Surg 168 555–559 Occurrence Handle7977995
K Prakash G Jacob V Lekha A Venugopal B Venugopal H Ramesh (2002) ArticleTitleLaparoscopic cholecystectomy in acute cholecystitis. Factors associated with conversion SurgEndosc 16 180–183
DW Rattner C Ferguson AL Warshaw (1993) ArticleTitleFactors associated with successful laparoscopic cholecystectomy for acute cholecystitis Ann Surg 217 233–236 Occurrence Handle8452401
M Rosen F Brody J Ponsky (2002) ArticleTitlePredictive factors for conversion of laparoscopic cholecystectomy Am J Surg 184 254–258 Occurrence Handle10.1016/S0002-9610(02)00934-0 Occurrence Handle12354595
JR Sanabria S Gallinger R Croxford SM Strasberg (1994) ArticleTitleRisk factors in elective laparoscopic cholecystectomy for conversion to open cholecystectomy J Am Coll Surg 179 696–704 Occurrence Handle7952482
P Schrenk R Woisetschlager WU Wayand (1995) ArticleTitleLaparoscopic cholecystectomy. Cause of conversion in 1300 patients and analysis of risk factors Surg Endosc 9 25–28 Occurrence Handle10.1007/BF00187880 Occurrence Handle7725209
H Seeliger A Fürst C Zülke KW Jauch (2002) ArticleTitleSurgical management of bile duct injuries following laparoscopic cholecystectomy: analysis and follow-up of 28 cases Langenbecks Arch Surg 387 286–293 Occurrence Handle10.1007/s00423-002-0330-x Occurrence Handle12447554
InstitutionalAuthorNameSouthernSurgeons Club (1991) ArticleTitleA prospective analysis of 1518 laparoscopic cholecystectomies N Engl J Med 334 1073–1078
M Suter A Meyer (2001) ArticleTitleA 10-year experience with the use of laparoscopic cholecystectomy for acute cholecystitis Is it safe? Surg Endosc 15 1187–1192 Occurrence Handle10.1007/s004640090098
A Zisman R Gold-Deutch E Zisman M Nefri Z Halpern G Lin A Halevy (1996) ArticleTitleIs male gender a risk factor for conversion of laparoscopic into open cholecystectomy? Surg Endosc 10 892–894 Occurrence Handle10.1007/s004649900191 Occurrence Handle8703145
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Simopoulos, C., Botaitis, S., Polychronidis, A. et al. Risk factors for conversion of laparoscopic cholecystectomy to open cholecystectomy. Surg Endosc 19, 905–909 (2005). https://doi.org/10.1007/s00464-004-2197-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-004-2197-0