Abstract
Background
Laparoscopic colorectal resection (LCR) is gaining popularity. Nonetheless, open surgery remains an important technique. Thus, surgeons should be technically proficient in both open and laparoscopic surgery. One question however remains unanswered: Can training for open and LCR occur simultaneously? The objective of this paper is to review the learning curve for open and laparoscopic colon resection of one surgeon who underwent a rigorous training program.
Methods
A review of consecutive patients who underwent surgery for colon and rectosigmoid junction cancers by one trainee surgeon was performed. This surgeon had completed his basic surgical residency but had limited experience in colorectal cancer surgery. In total, 75 patients were included in this study. All operations were supervised by at least one staff surgeon with experience of more than 300 LCR cases. The trainee surgeon was allowed to train in both laparoscopic and open colorectal resection simultaneously.
Results
Forty-three patients underwent laparoscopic resection, while 32 patients underwent open surgery. Age, gender, mean body mass index (BMI), preoperative risk, and history of past abdominal surgery showed no significant difference between laparoscopic and open groups. There were no differences in tumor stage [International Union against Cancer (UICC)] or tumor size (p = 0.068 and 0.228, respectively). The morbidity rate for open and laparoscopic surgery was 3.1% (1/32) and 4.7% (2/43), respectively (p = 0.484). Operation time decreased with increasing experience, and plateaued after 25 cases in the laparoscopic group and 22 cases in the open group. The learning curve for open cases was 11 cases, and 7 for laparoscopic surgery.
Conclusions
Surgeons who have completed a basic surgical residency but have limited colorectal surgery experience can learn both open and laparoscopic colorectal surgery simultaneously in an effective manner under supervision by well-experienced surgeons.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopic colorectal resection (LCR) is gaining popularity. Prospective randomized control studies have revealed some benefits of LCR for colorectal cancer compared with open surgery [1–5]. Nonetheless, open surgery remains an important technique. Thus, surgeons should be technically proficient in both open and laparoscopic surgery.
LCR is believed to be technically more difficult than open surgery and thought to require more intensive training to ensure safe and oncologic operation [6, 7]. There are many reports regarding the learning curve for performing LCR [7–15]. The learning curve is generally accepted to be approximately 30 procedures based on decline in operative time, intraoperative complications, and conversion rate. One question however remains unanswered: Can training for open and LCR occur simultaneously?
We hypothesized that surgeons who have finished a basic 4-year surgical residency program according to the Japanese system can learn both open and laparoscopic colorectal cancer resection efficiently simultaneously as long as they are well supervised. The objective of this study is to review the learning curve for open and laparoscopic colon resection of one surgeon who underwent a rigorous training program.
Patients and methods
A review of consecutive patients who underwent surgery for colon and rectosigmoid junction cancers from May 2005 to December 2007 by one trainee surgeon at Jichi Medical University Saitama Medical Center was performed. This surgeon had completed his basic surgical residency but had limited experience in colorectal cancer surgery and D3 dissection. Prior to commencement of the colorectal training, this surgeon had performed 350 cases of general surgery operations as first surgeon, including 80 cases of appendectomy, 62 cases of hernia repair, 46 cases of laparoscopic cholecystectomy, 10 cases of gastrectomy, and 21 cases of colectomy. Colectomies included five cases of ileocecal resection, nine cases of sigmoid colectomy, and seven cases of right hemicolectomy. He had also been an assistant in more than 1,000 other cases during a 4-year surgical residency program in Japan.
Because this study was designed to investigate the learning curve for laparoscopic and open colorectal surgery under supervision by experts, difficult cases were excluded from this study. Exclusion criteria were as follows: (1) patients who underwent combined procedures such as cholecystectomy, hepatectomy, and hysterectomy, (2) tumor located near the splenic flexure or in the rectum, and (3) T4 tumors that directly invaded adjacent organs or structures. In total, 75 patients were included in this study. All operations were supervised by at least one staff surgeon with experience of more than 300 LCR cases. The trainee surgeon was allowed to train in both laparoscopic and open colorectal resection simultaneously. When the surgeon performed more than 80% of the procedure, it was credited to this surgeon. Patient characteristics and oncological outcomes were analyzed.
Standardized procedures were performed for all cases. For left-sided lesions, medial-to-lateral approach was performed in laparoscopic surgery, while lateral-to-medial approach was done in open surgery. Laparoscopic left-sided colon resection began with ligation of proximal vascular pedicles, followed by mobilization and resection of bowel with anastomosis. For right-sided lesions, both procedures were performed using lateral-to-medial approach, which began with mobilization of the bowel, followed by exploration of the retroperitoneum, ligation of vascular pedicles, and resection of bowel with anastomosis. D3 dissection (exposure of the root of the feeding vessels) was performed when indicated.
Quality assessment and analysis of learning curve was performed by plotting cumulative summation (CUSUM) curves, and the moving average method was used to assess changes in operation time for both laparoscopic surgery and open surgery. CUSUM curve has emerged as a popular tool to monitor quality of surgery [16]. CUSUM allows one to judge whether a given variation in performance is acceptable, or whether the variation is greater than could be expected from random variation and thus may be a concern. As previous report utilized CUSUM to assess the learning curve for surgical treatment, CUSUM (S n ) was defined as S n = Σ(X i − X 0), where X i is an individual attempt and X 0 is the predetermined acceptable failure rate for the procedure, with X i assigned a score of 0 for success and 1 for failure [13, 14]. The acceptable failure rate was defined such that, when the target success rate was set at 90%, the acceptable failure rate was 10% (X 0 was set at 0.1). For the CUSUM curve we defined “failure” has occurring when any of the following occurred: (1) perioperative major morbidity and mortality, (2) intraoperative blood loss >1,000 ml, or (3) long operative time more than two standard deviations above the department average (>240 min for open surgery, >270 min for LCR).
The moving average method was also used to assess changes in operation time for qualification of the learning curve. Creating an average of values that moves with the addition of new data results in smoothing of the value of the variable being analyzed.
Statistical analysis was performed using SPSS version 17.0 (SPSS Inc., Chicago, IL) for Windows. The chi-square test or Fisher’s exact test was used for comparison of categorical variables as appropriate, and Student’s t-test was used for comparison of continuous variables. Values of p < 0.05 were regarded as statistically significant.
Results
A total of 75 patients were included in this study. The choice of surgical procedure was basically determined by patient preference, with LCR performed as default. Consequently, 43 patients underwent laparoscopic resection, while 32 patients underwent open surgery. Patient characteristics are presented in Table 1. Age, mean BMI, American Society of Anesthesiologists (ASA) score, and history of past abdominal surgery showed no significant difference between laparoscopic and open groups.
Tumor characteristics are listed in Table 2. There were no differences in tumor stage (UICC) or tumor size (p = 0.068 and 0.194, respectively). Extent of lymph node involvement or distant metastasis did not show significant difference. There were a significantly larger number of harvested lymph nodes in the laparoscopic group (p = 0.012). Operative outcomes are listed in Table 3. In laparoscopic surgery, operative time was significantly longer, while estimated blood loss was significantly less. The morbidity rate for open and laparoscopic surgery was 3.1% (1/32) and 4.7% (2/43), respectively (p = 0.484). Morbidities were small bowel obstruction for open surgery, and major leakage and bleeding that required blood transfusion for laparoscopic surgery. Mortality rate was 0% in both groups during this study. There were three cases of conversion to open surgery from initially performed laparoscopic surgery during this study; reasons for conversion were severe small bowel adhesion to abdominal wall due to previous laparotomy for duodenal ulcer in one case, and two cases of bleeding which were difficult to control by laparoscopic operation.
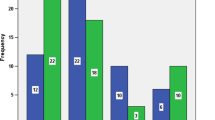
The moving average of the operation time for open and laparoscopic surgery is shown in Fig. 1. For both groups, operation time decreased with increasing experience, and plateaued after 25 cases in the laparoscopic group and 22 cases in the open group.
CUSUM curves are shown in Fig. 2. In the laparoscopic group, surgical morbidity was observed in two cases, and operative time was longer than 270 min in five cases. In the open group, surgical morbidity occurred in one case, and operative time exceeded 240 min in three cases. There were no cases exceeding 1,000 ml blood loss in either approach. The learning curve for open cases was 11 cases and 7 for laparoscopic surgery.
Discussion
The 4-year basic surgical residency program in Japan involves attainment of basic surgical skills. Basic surgical residents start with basic procedures such as appendectomy, cholecystectomy, and hernia repair [17–21]. They then progress to open colorectal cancer surgery. LCR is learned later, after proficiency in open colorectal resections. With efforts to standardize LCR technique and supervision from expert surgeon in LCR, it has become easier for a trainee surgeon to learn the technical skills of LCR. We thus hypothesized that LCR could be learned simultaneously with open colorectal surgery.
In this study, we excluded tumors that were located near the splenic flexure, at the descending colon, and the rectum, as these locations are technically more difficult and may not be suitable for operation by trainee. Cases of tumors that were invading adjacent organs were also excluded for similar reasons.
Previous reports evaluating the learning curve of laparoscopic colorectal surgery included some different factors from those utilized herein [7, 9, 13, 22, 23]. To evaluate quality of LCR, we did not include number of lymph nodes harvested, as standard D2 or D3 operations for early and advanced tumors, respectively, were performed in all cases. Extent of dissection was ensured by the supervisor in every case. Conversion to open surgery was also not included in this study. In our previous study, trainee surgeon did not cause more conversion in LCR if they were well supervised [24]. So, we do not believe that conversion to open surgery is a good indicator to assess quality of LCR under good supervision. Besides, conversion rate should be evaluated as proficiency of laparoscopic surgery only. We considered blood loss more than 1,000 ml and long operative time as failure, as our previous study showed that these were independent predictors of poorer outcome (data to be published in the American Journal of Surgery).
Monitoring quality in surgical treatment has been a topic of interest for many. Direct observation by a supervisor and graphical representation of the learning curve are two common ways of assessing individual competence, but both are likely to be subjective [25, 26]. Assessment of surgeon competency should be dynamic and enable quantitative and continuous evaluation of surgeon performance. CUSUM allows continuous monitoring of surgical performance using clearly defined situations of failure and provides objective evaluation. CUSUM has emerged as a popular tool for performance monitoring in surgery since its first application to evaluate surgical outcomes by de Leval et al. [27]. CUSUM methodology has been applied to describe quality in colorectal surgery in several studies [8, 13, 14]. In this study, the CUSUM curve demonstrated downward slope after 11 cases in open group and 7 cases in laparoscopic group, which implies that the surgeon had acquired sufficient skills for index procedures.
The moving time average stabilized after 25 cases for laparoscopic colorectal surgery and 22 cases for open surgery, which implies that a further 18 and 11 cases were required to stabilize operation time in laparoscopic and open surgery, respectively. These patterns suggest that the trainee surgeon was able to perform the procedure safely at an early stage, and this was then followed by reduction in operative time when technical skills were further improved.
The learning curve for LCR in our study was similar to one previous report [13], while other reports demonstrated larger number of cases for the learning curve [7, 10, 12, 15]. The accelerated learning curve demonstrated herein is likely to be a result of the following: Firstly, the trainers in this series were extremely experienced in both laparoscopic and open colorectal surgery. Each of the trainers had carried out more than 300 cases of LCR. With this experience, it was possible for them to impart a technique for both open and laparoscopic surgery that has already been well established and standardized. This enabled easier learning, as the trainee did not have to contend with different techniques of different supervising surgeons. Secondly, the ever-present supervision of the experienced staff surgeons enabled the trainee to commit fewer mistakes intraoperatively, especially in identification of anatomical structures and planes of dissection. Furthermore, the radicality of oncologic surgery was maintained [24].
Conclusions
Surgeons who have completed basic surgical residency but have limited colorectal surgery experience can learn both open and laparoscopic colorectal surgery simultaneously in an effective manner under supervision by well-experienced surgeons.
References
Hewett PJ, Allardyce RA, Bagshaw PF, Frampton CM, Frizelle FA, Rieger NA, Smith JS, Solomon MJ, Stephens JH, Stevenson AR (2008) Short-term outcomes of the Australasian randomized clinical study comparing laparoscopic and conventional open surgical treatments for colon cancer: the ALCCaS trial. Ann Surg 248(5):728–738
Braga M, Vignali A, Gianotti L, Zuliani W, Radaelli G, Gruarin P, Dellabona P, Di Carlo V (2002) Laparoscopic versus open colorectal surgery: a randomized trial on short-term outcome. Ann Surg 236(6):759–766 disscussion 67
Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM, Heath RM, Brown JM (2007) Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol 25(21):3061–3068
Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Pahlman L, Cuesta MA, Msika S, Morino M, Lacy AM (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6(7):477–484
Fleshman J, Sargent DJ, Green E, Anvari M, Stryker SJ, Beart RW Jr, Hellinger M, Flanagan R Jr, Peters W, Nelson H (2007) Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Ann Surg 246(4):655–662; discussion 62–64
Jamali FR, Soweid AM, Dimassi H, Bailey C, Leroy J, Marescaux J (2008) Evaluating the degree of difficulty of laparoscopic colorectal surgery. Arch Surg 143(8):762–767; discussion 8
Li JC, Hon SS, Ng SS, Lee JF, Yiu RY, Leung KL (2009) The learning curve for laparoscopic colectomy: experience of a surgical fellow in an university colorectal unit. Surg Endosc 23(7):1603–1608
Tekkis PP, Senagore AJ, Delaney CP, Fazio VW (2005) Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg 242(1):83–91
Reichenbach DJ, Tackett AD, Harris J, Camacho D, Graviss EA, Dewan B, Vavra A, Stiles A, Fisher WE, Brunicardi FC, Sweeney JF (2006) Laparoscopic colon resection early in the learning curve: what is the appropriate setting? Ann Surg 243(6):730–735; discussion 5–7
Simons AJ, Anthone GJ, Ortega AE, Franklin M, Fleshman J, Geis WP, Beart RW Jr (1995) Laparoscopic-assisted colectomy learning curve. Dis Colon Rectum 38(6):600–603
Fukunaga Y, Higashino M, Tanimura S, Takemura M, Osugi H (2008) Laparoscopic colorectal surgery for neoplasm. A large series by a single surgeon. Surg Endosc 22(6):1452–1458
Wishner JD, Baker JW Jr, Hoffman GC, Hubbard GW II, Gould RJ, Wohlgemuth SD, Ruffin WK, Melick CF (1995) Laparoscopic-assisted colectomy. The learning curve. Surg Endosc 9(11):1179–1183
Choi DH, Jeong WK, Lim SW, Chung TS, Park JI, Lim SB, Choi HS, Nam BH, Chang HJ, Jeong SY (2009) Learning curves for laparoscopic sigmoidectomy used to manage curable sigmoid colon cancer: single-institute, three-surgeon experience. Surg Endosc 23(3):622–628
Dincler S, Koller MT, Steurer J, Bachmann LM, Christen D, Buchmann P (2003) Multidimensional analysis of learning curves in laparoscopic sigmoid resection: eight-year results. Dis Colon Rectum 46(10):1371–1378; discussion 8–9
Schlachta CM, Mamazza J, Seshadri PA, Cadeddu M, Gregoire R, Poulin EC (2001) Defining a learning curve for laparoscopic colorectal resections. Dis Colon Rectum 44(2):217–222
Yap CH, Colson ME, Watters DA (2007) Cumulative sum techniques for surgeons: a brief review. Aust N Z J Surg 77(7):583–586
Lin YY, Shabbir A, So JB (2009) Laparoscopic appendectomy by residents: evaluating outcomes and learning curve. Surg Endosc 24(1):125–130
Friedman RL, Pace BW (1996) Resident education in laparoscopic cholecystectomy. Surg Endosc 10(1):26–28
Kauvar DS, Braswell A, Brown BD, Harnisch M (2006) Influence of resident and attending surgeon seniority on operative performance in laparoscopic cholecystectomy. J Surg Res 132(2):159–163
Wilkiemeyer M, Pappas TN, Giobbie-Hurder A, Itani KM, Jonasson O, Neumayer LA (2005) Does resident post graduate year influence the outcomes of inguinal hernia repair? Ann Surg 241(6):879–882; discussion 82–84
Anderson BO, Sun JH, Moore EE, Thompson LL, Harkin AH, Bartle EJ (1989) The development and evaluation of a clinical test of surgical resident proficiency. Surgery 106(2):347–352; discussion 52–53
Bowles TA, Watters DA (2007) Time to CUSUM: simplified reporting of outcomes in colorectal surgery. Aust N Z J Surg 77(7):587–591
Park IJ, Choi GS, Lim KH, Kang BM, Jun SH (2009) Multidimensional analysis of the learning curve for laparoscopic resection in rectal cancer. J Gastrointest Surg 13(2):275–281
Maeda T, Tan KY, Konishi F, Tsujinaka S, Mizokami K, Sasaki J, Kawamura YJ (2009) Trainee surgeons do not cause more conversions in laparoscopic colorectal surgery if they are well supervised. World J Surg 33(11):2439–2443
Elliot DL, Hickam DH (1987) Evaluation of physical examination skills. Reliability of faculty observers and patient instructors. JAMA 258(23):3405–3408
Van Rij AM, McDonald JR, Pettigrew RA, Putterill MJ, Reddy CK, Wright JJ (1995) Cusum as an aid to early assessment of the surgical trainee. Br J Surg 82(11):1500–1503
de Leval MR, Francois K, Bull C, Brawn W, Spiegelhalter D (1994) Analysis of a cluster of surgical failures. Application to a series of neonatal arterial switch operations. J Thorac Cardiovasc Surg 107(3):914–923; discussion 23–24
Disclosures
Authors Maeda, Tan, Konishi, Tsujinaka, Mizokami, Sasaki, and Kawamura have no conflicts of interest or financial ties to disclosure.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maeda, T., Tan, K.Y., Konishi, F. et al. Accelerated learning curve for colorectal resection, open versus laparoscopic approach, can be attained with expert supervision. Surg Endosc 24, 2850–2854 (2010). https://doi.org/10.1007/s00464-010-1063-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-010-1063-5