Abstract
Background
This study aimed to evaluate the learning curve for laparoscopic colectomy of a surgical fellow in an university colorectal unit using a structured training protocol.
Methods
This study analyzed the data from 100 consecutive patients who had laparoscopic colectomy performed by a surgical fellow between 11/2004 and 12/2007. The structured training protocol required the fellow to assist more than 40 laparoscopic colectomies before embarking on his first case. Rectosigmoidectomy was prioritized during the initial experience. Operative times were analyzed to represent the learning curve. Other outcome data including conversion and operative outcome were also evaluated.
Results
The following procedures were performed: 49 rectosigmoidectomies, 38 right colon resections, and 13 other resections. Median operative time was 150 min, and conversion rate was 1%. Overall postoperative morbidity rate was 28% (major morbidity 3%). Three patients required early reoperation. There was no operative death. Median hospital stay was 8 days. Operative times reached their lowest point at period of cases 45–50, and remained relatively stable afterwards. Comparing the first 50 and second 50 cases, the only difference observed was more frequent presence of a supervisor in the theater in the first 50 cases (74% versus 52%, p = 0.02), while the other parameters including types of procedures, postoperative recovery, hospital stay, and morbidity rate were not different.
Conclusions
Our results indicated that laparoscopic colectomy training can be safely performed under a structured protocol. The surgeon can perform laparoscopic colectomies more independently after 50 cases, without jeopardizing the clinical outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopic colectomy is an established minimally invasive procedure for treatment of both benign and malignant large bowel disease. Compared with open colectomy, it is associated with faster postoperative recovery and lower morbidity [1–4]. Recent randomized control trial and meta-analysis confirmed comparable oncological outcomes between laparoscopic and open colorectal surgery [1, 5–8]. We have previously reported that laparoscopic colectomy was feasible and safe in the hands of experienced laparoscopic surgeons [2, 7].
Laparoscopic colectomy is a technically demanding procedure with a steep learning curve. The learning curve reported in literature is highly variable, ranging from 20 to 70 cases [9–15]. A structured program was established in our centre for training surgical fellow in laparoscopic colectomy. We would like to evaluate the learning curve of the first surgical fellow (J.C.M.L.) trained in a university colorectal unit using this structured training protocol and assess its feasibility.
Materials and methods
Between November 2004 and December 2007, 100 consecutive patients underwent laparoscopic colectomy by a surgical fellow were included in this study. Demographic data, intraoperative findings, operative procedures, postoperative parameters, morbidities, and outcomes were prospectively collected into our colorectal database.
Our unit had four experienced laparoscopic colorectal surgeons. They work together and provide team approach in laparoscopic colorectal surgery. They all supervised or assisted the surgical fellow (J.C.M.L.) to perform the operations in this study. Before starting hands-on laparoscopic colectomy, he had attended a training course, performed at least 75 basic laparoscopic procedures (cholecystectomy or appendectomy), and assisted in more than 40 laparoscopic colectomies. In order to ensure patient safety and oncological clearance as well as facilitate learning, the initial cases were highly selected. The sequence would be starting from benign disease to early cancer then more advanced disease. The operation to start was sigmoidectomy, followed by anterior resection then right hemicolectomy and then resection of lower rectum tumor.
We had standardized the preoperative preparations, operative steps, instrumentations, and postoperative care. Our technique of laparoscopic colectomy has been reported previously [2, 7]. In principle, we mobilized the colon, followed by transection of the lymphovascular pedicles. For left colon resection, distal transection was performed intracorporeally by linear stapler. A port wound was extended to deliver the specimen under the protection of a plastic bag. The division of the bowel was then performed extracorporeally. The ileocolic anastomosis was performed extracorporeally either handsewn or functional side-to-side anastomosis with linear stapler, while the colo-colic or colorectal anastomosis was performed intracorporeally with circular stapler for left colon resection or rectum, respectively. Postoperatively, diet was resumed as soon as bowel function returned clinically. Patients were discharged when they tolerated diet and regained ambulation. Patients were regarded to be suffering from prolonged ileus if they were unable to resume diet after postoperative day 4 and required parenteral nutrition supplementation. Time to full ambulation was defined as time when the patient could walk independently in the ward without assistance.
Operative time was measured from skin incision to completion of wound closure. Mean operative time of every five consecutive cases was used to plot a learning curve. Conversion rate and perioperative outcome were also analyzed. The patients were divided into two successive groups for statistical analysis: the first 50 cases belonged to group 1, and the second 50 cases belonged to group 2. The learning curves for rectosigmoidectomy (sigmoidectomy, anterior resection, and low anterior resection) and right colonic resections (right hemicolectomy and extended right hemicolectomy) were also analyzed.
The staging reported in this study was based on the 6th edition of the American Joint Committee on Cancer (AJCC) manual [16]. All patients were followed up every 3 months in the first year, every 4 months in the second year, and every 6 months thereafter. Demographic data, operative outcomes, and complications were analyzed by Pearson chi-squared test, Fisher’s exact test, and Mann–Whitney U-test. Significant difference was defined when p value < 0.05. All numerical values are expressed as median with the corresponding range in parenthesis. Statistical analyses were performed with SPSS for Windows.
Results
From November 2004 to December 2007, 100 patients (59 men, 41 women) of median age 70 years (range 30–91 years) underwent laparoscopic colectomy for varies condition. Eighty-five patients suffered from adenocarcinoma of colon. There were 10, 32, 29, and 14 patients who suffered from stage I, II, III, and IV disease, respectively. Eighty-six of 100 patients were of American Society of Anesthesiologists (ASA) score less than III. There was no surgical mortality in this series. Overall morbidity rate was 28% (3% major, 25% minor). One case (1%) was converted to open because of locally advanced disease. During the study period, there were 445 laparoscopic colorectal resections performed in our unit and the overall conversion rate was 5%.
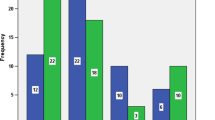
The operative time of all patients is shown in Fig. 1. Mean operative time started to drop at the period of cases 16–20 (120 min) and the operative time increased thereafter. The operative time dropped again at the period of cases 46–50 (141 min). The learning curve for rectosigmoidectomy and right colon resection were also analyzed separately; mean operative time dropped to a low point at 31–35 cases and 16–20 cases, respectively (Fig. 2).
When comparing the two consecutive periods, there was no significant difference between the two groups in terms of age, gender or comorbidities (Table 1). The operative results are summarized in Table 2. The median operative time, blood loss, and number of lymph nodes retrieved were also similar between the two groups. The presence of supervisor in theatre was more frequent in group 1 then in group 2 (74% versus 52%, p = 0.02). The surgical outcomes are shown in Table 3. The time to full ambulation, time to resume soft diet, time to first bowel motion, and hospital stay were similar between the two groups. The postoperative complications showed no significant differences between the two groups.
Comparing elective rectosigmoidectomy and right colon resection, there were no significant differences in demographic data. Median operative time was significantly longer (157.5 versus 130 min; p = 0.005) and number of lymph node retrieval was significantly higher (18 versus 15; p = 0.006) for right colon resection than for rectosigmoidectomy (Table 4). Time to resume soft diet was significantly longer in the right colon resection group (5 versus 4 days; p = 0.001), but time to full ambulation, time to first bowel motion, and hospital stay were similar between the two groups (Table 5). Right colon resection group had more postoperative ileus (19.2% versus 2.04%; p = 0.02) and reoperation (11.5% versus 0%; p = 0.04) than rectosigmoidectomy group. Reasons for reoperation included anastomotic leak, intra-abdominal collection, and intestinal obstruction. Other postoperative complications showed no significant differences between the two groups.
Discussion
The key to the widespread application of any surgical procedure is based on ability to treat the disease effectively with minimal morbidity and to transfer the technique to a large number of surgeons. Laparoscopic colectomy is a technically demanding procedure that requires high degree of spatial resolution, dexterity, and technical skills. The assessment of trainee progress and operator competency is an important aspect of quality assurance in patient care.
Having four surgeons practising similar technique, we have more opportunities to share experience and learn from each other. This group learning effect might reduce the number of procedures required to acquire proficiency. This is the basis of our structured training. In our protocol, the training surgeon is required to assist more than 40 laparoscopic colectomies before starting his first case. During this process, he can have greater appreciation of anatomy, gain experience in laparoscope manipulation, and learn to provide countertraction. In order to facilitate the initial training of the training surgeon, we intend to select less complicated cases, including benign disease and early cancer of sigmoid and upper rectum. The operative time in the first 15–20 cases may reflect learning progress with this case selection. Therefore, there is an initial drop in operation time, but it increases in the latter period of training because there will be no more case selection.
The learning curve for an operation refers to the number of cases required to acquire the technique with minimal operative time and complication rate. Previous studies have analyzed the learning curve in laparoscopic colectomy [9–15]. The most frequently used technical indicators of the learning curve were operative time, conversion rate, and operative complications [15, 17, 18]. The outcome variables can be classified into clinical process and task efficiency, or patient outcome. The present study measured operative time, conversion rate, postoperative recovery, and complications. The first two variables represent clinical process and task efficiency and the latter two variables represent patient outcome.
The mean operative time of five consecutive cases was used to plot a learning curve. This is more representative than a single case because it reflects the performance of the surgeon throughout the study period. Some studies use moving-average method to demonstrate the change of the operative time [14, 18]. This technique cannot show the operative time during the early part of the study (for example during the first ten cases) and the trend over time.
In some series, operative time failed to decrease with experience [19] and shorter operative times did not correlate with better clinical outcomes [19]. The failure of operative time to decline with experience often reflects surgeons’ willingness to attempt more difficult cases rather than an accurate representation of a learning curve. In our study, the learning curve reached plateau at around 46–50 cases. The operative time actually went up thereafter, and this may reflected the fact that more challenging cases were performed.
Using operative time as a solitary indicator for surgical performance might be inadequate [13–15, 20, 21]. Some authors use conversion and intraoperative complication rate as the outcome variable which is plotted against time, showing a decreasing trend with time [10, 12, 13, 17, 21, 22]. Because of the low conversion and intraoperative complication rate, we do not attempt to use these factors to plot a learning curve. Lymph nodes involvement is a major prognostic factor for colorectal cancer, and the current AJCC manual recommends assessment of 12 or more lymph nodes for accurate staging [16]. Lymph node retrieval can be influenced by factors, including patient, surgeon, and pathologist. Lymph node involvement is often regarded as an indicator of surgical performance [18]. In our study, lymph node retrieval was the same between the two time periods. In fact, the only significantly different result was the presence of supervisor in theatre. Based on the observation that mean operative time reached a low point at the period of cases 46–50 and on the significant difference in percentage supervisor presence in theatre, we think the steady state was reached after approximately 46–50 interventions for the surgeon.
In general, right colon resections are regarded as simpler procedures to perform, also requiring less time to perform [19]. However some studies showed right hemicolectomy had higher conversion rate [15] and minor complication rate [19]. Our result showed that right colon resections resulted in longer operative time, more time to resume soft diet, and more postoperative complications (postoperative ileus and reoperation) than rectosigmoidectomy. These results support our protocol in starting straightforeword rectosigmoidectomy during initial training period.
Patient safety is a major concern at anytime of a surgeon’s career, especially during the training period, and patient benefit should not be jeopardized by lack of surgical experience. The current study supported that skill of laparoscopic colectomy can be taught and acquired safely under this structured training protocol. For surgical fellow trained in an established centre, a structured training protocol can be formulated. The protocol should include standardization of operative steps, instrumentation, and postoperative care plan. The training surgeon has to observe at least ten resections, followed by assisting 30–40 cases. The initial cases should be started, preferably rectosigmoidectomy, with direct supervision of an experienced surgeon. Meanwhile, the training surgeon continues to assist and observe other surgeons. With time, the surgical fellow can operate independently and supervision will be provided for difficult or complicated cases only.
Several studies suggest that evaluation of surgical performances based solely on operative time is inappropriate [13–15, 20, 21]. Assessment of a learning curve should also include surgical outcomes and degree of independence. The current study demonstrated the performance of a surgical fellow in terms of operative time and operative morbidity. With appropriate supervision, patient outcome and safety can be maintained throughout the training period.
In conclusion, our study shows the training process of a surgical fellow in performing laparoscopic colectomy. The surgeon can perform laparoscopic colectomies more independently after approximately 50 cases, without jeopardizing the clinical outcome.
References
Lacy AM, Garcia-Valdecasas JC, Delgado S, Castells A, Taura P, Pique JM, Visa J (2002) Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet 359:2224–2229
Leung KL, Meng WC, Lee JF, Thung KH, Lai PB, Lau WY (1999) Laparoscopic-assisted resection of right-sided colonic carcinoma: a case–control study. J Surg Oncol 71:97–100
Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Pahlman L, Cuesta MA, Msika S, Morino M, Lacy AM, Colon cancer Laparoscopic or Open Resection Study Group (COLOR) (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6:477–484
Schwenk W, Haase O, Neudecker J, Muller JM (2005) Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev 20(3):CD003145
Fleshman J, Sargent DJ, Green E, Anvari M, Stryker SJ, Beart RW Jr, Hellinger M, Flanagan R Jr, Peters W, Nelson H (2007) Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Trial Group. Ann Surg 246:655–664
Jackson TD, Kaplan GG, Arena G, Page JH, Rogers SO Jr (2007) Laparoscopic versus open resection for colorectal cancer: a metaanalysis of oncologic outcomes. J Am Coll Surg 204:439–446
Leung KL, Kwok SP, Lam SC, Lee JF, Yiu RY, Ng SS, Lai PB, Lau WY (2004) Laparoscopic resection of rectosigmoid carcinoma: prospective randomised trial. Lancet 363:1187–1192
Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM, MRC CLASICC trial group (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial)—multicentre, randomised controlled trial. Lancet 365:1718–1726
Senagore AJ, Ma Luchtefeld, Mackeigan JM (1995) What is the learning curve for laparoscopic colectomy? Am Surg 61:681–685
Simons AJ, Anthone GJ, Ortega AE, Franklin M, Fleshman J, Gesi WP, Beart RW Jr (1995) Laparoscopic-assisted colectomy learning curve. Dis Colon Rectum 38:600–603
Wishner JD, Baker JW Jr, Hoffman GC, Hubbard GWII, Gould RJ, Wohlgemuth SD, Ruffin WK, Melick CF (1995) Laparoscopic-assisted colectomy. The learning curve. Surg Endosc 9:1179–1183
Agachan F, Joo JS, Sher M, Weiss EG, Nogueras JJ, Wexner SD (1997) Laparoscopic colorectal surgery. Do we get faster? Surg Endosc 11:331–335
Schlachta CM, Mamazza J, Seshadri PA, Cadeddu M, Gregoire R, Poulin EC (2001) Defining a learning curve for laparoscopic colorectal resections. Dis colon Rectum 44:217–222
Dincler S, Koller MT, Steurer J, Bachmann LM, Christen D, Buchmann P (2003) Multidimensional analysis of learning curves in laparoscopic sigmoid resection: eight-year results. Dis Colon Rectum 46:1371–1379
Tekkis PP, Senagore AJ, Delaney CP, Fazio VW (2005) Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg 242:83–91
Greene FLP, Page DL, Fleming ID, Fritz A, Balch CM, Haller DG, Morrow M (2002) AJCC cancer staging manual, 6th edn. Springer, Philadelphia
Marusch F, Gastinger I, Schneider C, Scheidback H, Konradt J, Bruch HP, Kohler L, Barlehner E, Kockerling F, Laparoscopic Colorectal Surgery Study Group (LCSSG) (2001) Experience as a factor influencing the indications for laparoscopic colorectal surgery and the results. Surg Endosc 15:116–120
Choi DH, Jeong WK, Lim SW, Chung TS, Park JI, Lim SB, Choi HS, Nam BH, Chang HJ, Jeong SY (2008) Learning curves for laparoscopic sigmoidectomy used to manage curable sigmoid colon cancer: single-institute, three-surgeon experience. Surg Endosc. doi:10.1007/s00464-008-9753-y
Chen W, Sailhamer E, Berger DL, Rattner DW (2007) Operative time is a poor surrogate for the learning curve in laparoscopic colorectal surgery. Surg Endosc 21:238–243
Tilney HS, Lovegrove RE, Purkayastha S, Heriot AG, Darzi AW, Tekkis PP (2006) Laparoscopic vs open subtotal colectomy for benign and malignant disease. Colorectal Dis 8:441–450
Bennett CL, Stryker SJ, Ferreira MR, Adams J, Beart RW (1997) The learning curve for laparoscopic colorectal surgery. Preliminary results from a prospective analysis of 1194 laparoscopic-assisted colectomies. Arch Surg 132:41–44
Larach SW, Patankar Sk Ferrara A, Williamson PR, Perozo SE, Lord AS (1997) Complications of laparoscopic colorectal surgery. Analysis and comparison of early vs. latter experience. Dis Colon Rectum 40:592–596
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, J.C.M., Hon, S.S.F., Ng, S.S.M. et al. The learning curve for laparoscopic colectomy: experience of a surgical fellow in an university colorectal unit. Surg Endosc 23, 1603–1608 (2009). https://doi.org/10.1007/s00464-009-0497-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-009-0497-0