Abstract
Background
Treatment of splenic flexure (SF) colon cancer is not standardized. A laparoscopic approach is considered a challenging procedure.
Methods
This review examines a single-institution experience with laparoscopic colon resection for cancer of the SF. Intraoperative, pathologic, and postoperative data of patients who underwent laparoscopic SF resection were reviewed to assess for oncologic safety as well as early- and medium-term outcomes.
Results
Between September 2004 and January 2009, laparoscopic SF resection was performed for 15 patients with SF. Two cases of conversion were reported, and for three patients, colonic resection was robot assisted. In all cases, the anastomosis was completed intracorporeally. The distal margin was 3.8 ± 2.5 cm, and the proximal margin was 7.8 ± 3.7 cm from the tumor site. The mean number of harvested nodes was 9.2 ± 5.3. The mean operative time was 183.6 ± 45 min, and the blood loss was 98 ± 33 ml. No major morbidity was recorded.
Conclusions
Laparoscopic partial resection seems to be feasible and safe for the treatment of early-stage and locally advanced SF cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Carcinoma of the splenic flexure (SF) is a rare condition. Accounting for approximately 3 to 8% of all colon cancers, it is associated with a high risk of obstruction and poor prognosis [1, 2]. Treatment for SF carcinoma is considered challenging and not fully standardized [3]. In fact, both the SF and the transverse colon were never included in randomized controlled trials designed to assess the efficacy of laparoscopic surgery as a curative treatment for colon cancer [4, 5]. The reasons for exclusion of SF cancer from the trials include technical difficulties with laparoscopic identification of the middle and left colic vessels and subsequent lymph node dissection.
Other main controversies that contribute to the status of laparoscopic SF resection as a yet nonstandardized procedure involve the appropriate extent of surgery and the risk of inadvertent splenectomy [2, 6]. Recommendations for SF cancer range from left partial resection to extended right hemicolectomy in association with splenectomy and distal pancreatectomy [2]. Moreover, the risk for an inadvertent splenectomy is higher for SF tumors than for colon cancer at other sites, leading to higher postoperative morbidity and mortality [6].
This study reviews our experience treating SF tumors by a laparoscopic approach and analyzes our attitude for its management. The study also included patients undergoing laparoscopic robot-assisted resection, an approach with promising applications for such a site of colon cancer because of its fixed position and the need for fine manipulation.
Materials and methods
Patients
Between September 2004 and January 2009, a minimally invasive approach was proposed for all patients who had histologically proved SF carcinoma without marks of its infiltration of the surrounding organs (small bowel, spleen, pancreas and stomach) on the preoperative abdominal computed tomography (CT) scan. The SF was defined as the tract between the distal third of the transverse colon and the first part of the descending colon [7]. For patients with a more advanced stage or bulky disease, an open resection was the operation of choice, and in the case of adjacent organ involvement, an en bloc resection was performed.
The data for all the patients who underwent laparoscopic and robot-assisted colorectal surgery during the study period were recorded in a computer database designed for teaching and research purposes. The preoperative workup included physical examination, colonoscopy, total-body CT, and blood count. Precise preoperative location of the tumor was considered mandatory, and for patients whose barium enema or CT scan did not clearly identify the lesion mainly for its small dimensions, colonoscopy was repeated to perform the India ink tattooing of the lesion.
Definitive diagnosis of SF cancer was confirmed intraoperatively by observation of the lesion or tattoo. The clinical parameters analyzed included patient characteristics, operative variables, pathologic examination, and short- and medium-term outcomes. The perioperative data included operative time, blood loss, conversion rate, perioperative complications, and length of hospital stay. Operative time was calculated as the time between pneumoperitoneum induction and port-site closure. Intraoperative blood loss was measured by subtraction of aspirated and instilled fluids. Pathologic examination confirmed the type, grade, stage of disease (TNM), number of lymph nodes harvested, and longitudinal margins of excision.
The patients were evaluated weekly with clinical examinations during the 30 days after discharge. They then were followed up every 6 months with physical examination, tumor markers, liver ultrasound, computer tomography, chest X-ray, and colonoscopy.
Surgical technique
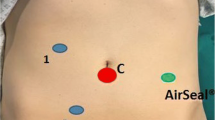
The laparoscopic operation starts with pneumoperitoneum induction at 12 mmHg using a Veress needle, followed by positioning of one camera port and three working trocars. The positions of the trocars are shown in Fig. 1 and do not differ between the traditional laparoscopic and the robot-assisted procedures. The patient is kept in the 20° anti-Trendelenburg position during the whole procedure for removal of the small bowel from the Treitz angle.
Surgical technique mandates identification of the inferior mesenteric artery at its origin and of the inferior mesenteric vein at the level of the duodenojejunal flexure. The left colonic artery is identified and encircled as well as the respective vein, a branch of the inferior mesenteric vein. Both vessels are ligated and divided at their root.
The SF is mobilized by division of the gastrocolic and splenocolic ligaments, and the transverse mesocolon is detached from its connection to the pancreatic body and tail. The greater omentum is divided using the Harmonic scalpel and the left part removed en bloc with the SF. The left branch of the middle colic vein is clipped at its origin as well as the ascending branch of the first sigmoid vessel.
When the SF has been well demarked, the colon is transected with multiple fires of the linear stapler, and a side-to-side completely intracorporeal stapled anastomosis is performed. The remaining enterotomy is closed in a single layer with a running intracorporeal suture (Fig. 2). The specimen is routinely extracted through the umbilical port, as previously described [8].
Operative details of laparoscopic splenic flexure (SF) partial resection. A Tumor tattoo. B Dissection and ligation of the left colic vein (LFC) at its root in the inferior mesenteric vein (IMV). C Dissection of the left colic artery (LCA). IMA inferior mesenteric artery. D The specimen fully mobilized. E Intracorporeal anastomosis
For the robot-assisted procedure, the dissection usually is performed using the hook cautery or scissors with the right arm and a Cadiere forceps (Intuitive Surgical Inc., Sunny-vale, CA) with the left arm. In the current study, the four-arm da Vinci HD robotic system (Intuitive Surgical Inc., Sunny-vale, CA) was used for all the procedures.
Results
During the study period, a minimally invasive approach was proposed for 15 patients. In the same span of time, another 11 patients underwent open left partial colectomy due to advanced tumor stage requiring an en bloc multivisceral resection or bulky disease. The patients’ characteristics are summarized in Table 1.
Intraoperative and pathologic data
The intraoperative and pathologic data are summarized on Table 2. In 13 cases (86%), a laparoscopic colon resection was performed without conversion or intraoperative complications, and in 3 cases, the operation was completely robot assisted. For two patients, laparoscopic SF resection was converted due to obesity and intraoperative suspicion of pancreatic tail infiltration, respectively.
Intraoperative coloscopy was necessary in two cases (16%) for clear identification of the tumor site. A tumor-free resection margin was demonstrated in all the specimens, and the tumor distance from the proximal and distal margins was proper. The mean number of harvested nodes was 9.2.
Outcome
The 30-day mortality was nil, and no cases of major morbidity were encountered (Table 2).
The mean hospital stay was 7 days, in the same range as the institutional hospital stay for patients undergoing laparoscopic colon resection of tumors at other sites (data not shown).
With regard to oncologic results, we evaluated all patients during a mean follow-up period of 29 months. One patient died of distant metastases 10 months after surgery, and local recurrences were not registered.
Discussion
To date, agreement on the choice of surgical treatment for SF cancers still has not been reached. As for other colon cancer sites, the resected area must encompass the mesentery to the origin of the major vessels in an attempt to reduce local recurrence by removal of involved lymph nodes. Two major vessels, the middle colic artery and the inferior mesenteric artery, nourish the SF, and the resection of carcinomas originating from this site should include removal of the lymph nodes up to the origin of the superior and inferior mesenteric vessels, respectively.
To achieve this result, different types of operations have been advocated. Sadler et al. [9] recommended an extended right hemicolectomy with removal of involved nodes, a procedure also performed by the laparoscopic hand-assisted approach [10]. Other investigators have suggested left partial colectomy, with ligation of both the left branch of the middle colic artery and the left colic artery at their origins to remove nodes likely to be involved [11]. On the other hand, Levien et al. [1] demonstrated that SF cancers are not associated with a worse prognosis than other colon cancers and that dual lymphatic drainage does not confer a survival disadvantage, so extended resection is unnecessary.
These data are paralleled by those of prospective and retrospective studies demonstrating a comparable oncologic outcome after left hemicolectomy and segmental resection for the treatment of left-sided colon cancers [12, 13].
Concerning SF cancer, the effectiveness of segmental resection could be determined by its lymphatic spread as described in the study of Nakagoe et al. [2]. These authors showed that the majority of positive nodes of a SF cancer are distributed along the paracolic arcade and the left colic artery. The nodes of the middle colic artery and its left branch were involved in a negligible number of cases (0 and 4.2%, respectively), thus not influencing the oncologic outcome.
Therefore, significant pieces of evidence suggest that a segmental resection could be effective for the treatment of SF cancer in its earlier phases. The use of a laparoscopic approach proved to be especially suitable for mobilizing and resecting the SF, and its fixed position led us to use the da Vinci system to manage the last three cases of the laparoscopic series. Moreover, laparoscopic segmental SF resection can be completed safely without identification and isolation of the middle colic vessels, a step considered demanding in laparoscopic surgery [14].
A comparison between a standard laparoscopic approach and a robot-assisted surgery for the treatment of SF cancer is beyond the aims of this study, but a facilitated vascular dissection and SF takedown were thought to be the main advantages of a robotic procedure. Postoperative morbidity was negligible, and cases of anastomotic failure were not recorded. Intracorporeal anastomosis was performed using the same technique we standardized in a large series of right colon resections [15]. Nevertheless, preservation of the inferior mesenteric and middle colic arteries could account for the good anastomotic healing much more than our experience with this technique. The absence of local relapse during the follow-up period supports good local control of the disease, justifying the recruitment of patients with SF cancer in future prospective randomized studies.
In conclusion, although our experience is limited and appropriate indications must be set by future studies, we believe that laparoscopic and robot-assisted SF segmental resection can be feasible and safe for patients with early-stage SF cancer. To date, in the absence of randomized studies, an open wider colon resection remains mandatory for cases of SF colon cancer in its advanced stages.
References
Levien DH, Gibbons S, Begos D, Byrne DW (1991) Survival after resection of carcinoma of the splenic flexure. Dis Colon Rectum 34:401–403
Nakagoe T, Sawai T, Tsuji T, Jibiki M, Ohbatake M, Nanashima A, Yamaguchi H, Yasutake T, Kurosaki N, Ayabe H, Ishikawa H (2001) Surgical treatment and subsequent outcome of patients with carcinoma of the splenic flexure. Surg Today 31:204–209
Schlachta CM, Mamazza J, Poulin EC (2007) Are transverse colon cancers suitable for laparoscopic resection? Surg Endosc 21:396–399
Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Pahlman L, Cuesta MA, Msika S, Morino M, Lacy AM (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6:477–484
Hazebroek EJ (2002) COLOR: a randomized clinical trial comparing laparoscopic and open resection for colon cancer. Surg Endosc 16:949–953
McGory ML, Zingmond DS, Sekeris E, Ko CY (2007) The significance of inadvertent splenectomy during colorectal cancer resection. Arch Surg 142:668–674
Steffen C, Bokey EL, Chapuis PH (1987) Carcinoma of the splenic flexure. Dis Colon Rectum 30:872–874
Casciola L, Codacci-Pisanelli M, Ceccarelli G, Bartoli A, Di Zitti L, Patriti A (2008) A modified umbilical incision for specimen extraction after laparoscopic abdominal surgery. Surg Endosc 22:784–786
Sadler GP, Gupta R, Foster ME (1992) Carcinoma of the splenic flexure: a case for extended right hemicolectomy? Postgrad Med J 68:487
Chew SS, Adams WJ (2007) Laparoscopic hand-assisted extended right hemicolectomy for cancer management. Surg Endosc 21:1654–1656
Dagradi V, Mozzo C, Lolli P, Piccinelli D, Ayvazian W, Briani GF (1982) Surgical treatment of cancer of the splenic flexure. Chir Ital 34:893–896
Rouffet F, Hay JM, Vacher B, Fingerhut A, Elhadad A, Flamant Y, Mathon C, Gainant A (1994) Curative resection for left colonic carcinoma: hemicolectomy vs. segmental colectomy: a prospective, controlled, multicenter trial. French Association for Surgical Research. Dis Colon Rectum 37:651–659
Secco GB, Ravera G, Gasparo A, Percoco P, Zoli S (2007) Segmental resection, lymph nodes dissection, and survival in patients with left colon cancer. Hepatogastroenterology 54(74):422–426
Kim HJ, Lee IK, Lee YS, Kang WK, Park JK, Oh ST, Kim JG, Kim YH (2009) A comparative study on the short-term clinicopathologic outcomes of laparoscopic surgery versus conventional open surgery for transverse colon cancer. Surg Endosc 23(8):1812–1817
Casciola L, Ceccarelli G, Di Zitti L, Valeri R, Bellochi R, Bartoli A, Barbieri F, Spaziani A, D’Ajello M (2003) Laparoscopic right hemicolectomy with intracorporeal anastomosis: technical aspects and personal experience. Minerva Chir 58:621–627
Acknowledgments
The authors thank Dr Luigi Maria Lapalorcia for language revision and the nurse staff of the Operating Block, Department of Surgery, Hospital San Matteo degli Infermi for their daily work.
Disclosures
Graziano Ceccarelli, Alessia Biancafarina, Alberto Patriti, Alessandro Spaziani, Alberto Bartoli, Raffaele Bellochi, Massimo Codacci Pisanelli, and Luciano Casciola have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ceccarelli, G., Biancafarina, A., Patriti, A. et al. Laparoscopic resection with intracorporeal anastomosis for colon carcinoma located in the splenic flexure. Surg Endosc 24, 1784–1788 (2010). https://doi.org/10.1007/s00464-009-0853-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-009-0853-0