Abstract
Background
One advantage of laparoscopic surgery over open surgery is the absence of laparotomic incisions. This advantage is reduced when an auxiliary incision is performed to remove surgical specimens larger than the trocar.
Methods
A special incision was performed at umbilical trocar level that enabled removal of a large surgical specimen as in right hemicolectomy (colic), gastric resection, and splenic surgery.
Results
The authors have used this method routinely for 10 years for all cases requiring removal of a surgical specimen too large for the normal incision of a 10-mm trocar.
Conclusion
The authors maintain that this method avoids the use of auxiliary incisions, which undo the many benefits of laparoscopic surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In abdominal laparoscopic surgery, removal of a surgical specimen with a diameter greater than that of the trocar (e.g., colon, spleen, stomach) normally is performed by auxiliary minilaparotomy, with enlargement of a trocar incision, or by a other forms of laparotomy (i.e., Pfannenstiel). These different incisions are not specified in the literature, and different authors use different methods. The great disadvantage of these techniques is that they eliminate or seriously reduce the benefits of laparoscopic surgery over open surgery, which results in the formation of adhesions, longer postoperative recovery, poor aesthetics, and greater incidence of incisional hernia.
This study describes a special incision at the level of the umbilical trocar that enables, in almost all cases, removal of surgical specimens varying greatly in shape and size with or without the help of an endobag. This approach is associated with minimum aesthetic impact, little tissue trauma, quick healing, and optimum patient compliance.
Surgical techniques
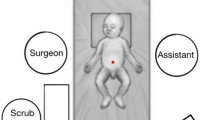
The umbilical trocar (10 mm) is removed for extraction of the specimen. An endobag is inserted through the incision. The specimen is placed into it, and the abdominal cavity is deflated. For the extraction, the umbilical incision is extended three-fourths of the way along the circumference of the umbilicus along the umbilical ring. When the subcutaneous connective tissue is stretched apart, the place at which the linea alba fits onto the umbilical ring is apparent. A 3- to 5-cm incision is made in a cranium caudal direction, and in some cases transversally. The preperitoneal area is dilated, reaching the peritoneum, and its incision is extended. Sometimes, further cutaneous incision in a radial direction is necessary (Fig. 1).
With dilation and slight exertion of traction on the bag, lessening the friction on the passage, the removal is carried out aseptically without the risk of any neoplastic seeding (Fig. 2). The closure is performed by layers of the incisions using an interrupted suture. The circumference of the cutaneous incision is hidden by the umbilical scar, and the incision on the fascia is only a few centimeters long (Fig. 3). This avoids the disadvantage of an additional incision on the abdominal wall, which is a more delicate area during surgery.
Results
Since 1994, we have applied the new method described in this report routinely for all the patients treated laparoscopically in our hospital who required removal of a large abdominal specimen. In this manner, we have treated 352 consecutive patients followed in the Department of General, Vascular, and Mininvasive Surgery at Spoleto Hospital, all of them eligible for laparoscopic surgery. Specifically, we performed 69 splenectomies, 138 right hemicolectomies, and 115 gastric resections. The skin incision remains within the umbilical scar, similar to the incision made in the normal placement of the trocar. This guarantees excellent results from an aesthetic point of view. There are no particular risks involved. Rarely, we have found a recanalized umbilical vein due to portal hypertension, whereas we have frequently observed the presence of previously undiagnosed umbilical hernias, which have been discovered and treated, thanks to this technique.
The clinical outcome was determined by a follow-up evaluation, which consisted of physical evaluation. Clinical assessments were made at the first, third, and sixth months after surgery. We have had three wound infections, of which one caused an incisional hernia. The remaining two wound infections healed with simple medication, and no neoplastic contamination occurred. To prevent any umbilical ischemia, the incision must not extend more than three-fourths of the umbilicus circumference.
Conclusion
One criticism leveled at laparascopic surgery used for operations requiring the removal of a large specimen (right colectomy, gastrectomy, splenectomy) is the stated requirement that a minilaparotomy or auxiliary incision on the abdominal wall must be performed to remove the specimen. By means of the described technique, specimens of considerable size, up to a maximum diameter of 6 or 7 cm, can be removed without reducing the advantages of laparoscopy. The incision has no contraindications or limitations apart from cases in which the great size of the tumor would contraindicate laparoscopy at the outset. We maintain that this incision has all the advantages of laparoscopic surgery, which would be lessened by the use of laparotomic incisions even if small. This method guarantees optimum functional recovery as well as the best aesthetic result possible because the cutaneous incision remains hidden by the umbilical scar, and the fascial incision is sufficiently long to allow removal of a large surgical specimen.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Casciola, L., Codacci-Pisanelli, M., Ceccarelli, G. et al. A Modified Umbilical Incision for Specimen Extraction After Laparoscopic Abdominal Surgery. Surg Endosc 22, 784–786 (2008). https://doi.org/10.1007/s00464-007-9584-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-007-9584-2