Abstract
Background
Inflammation and wound healing play critical roles in the integration of biologic and biodegradable meshes (BMs) at hernia repair sites. Monocytes/macrophages (M/MØs) are key cells controlling inflammation and wound healing. These cells release inflammatory cytokines and growth factors such as interleukin (IL)-1β, IL-6, IL-8, and vascular endothelial growth factor (VEGF) upon activation. Although BMs have been increasingly used in hernia repairs worldwide, to date, investigations of inflammatory responses to various BMs have been limited.
Methods
Mesh samples of three acellular human dermis-derived biologic meshes (AlloDerm, AlloMax, FlexHD) and one biodegradable synthetic mesh (Bio-A) were placed in 96-well plates. Human peripheral blood mononuclear cells (PBMCs) were isolated from six healthy subjects, added to each well, and incubated for 7 days. Culture supernatants were assayed for IL-1β, IL-6, IL-8, and VEGF levels using a multiplex bead-base immunoassay system (Bio-Plex).
Results
All four meshes induced cytokine expression from activated M/MØs to varying degrees in vitro. FlexHD induced significantly more IL-1β (2,591 pg/ml) than AlloMax (517 pg/ml), AlloDerm (48 pg/ml), or Bio-A (28 pg/ml) (p < 0.001). AlloMax stimulated a significantly greater quantity of IL-6 (38,343 pg/ml) than FlexHD (19,317 pg/ml), Bio-A (191 pg/ml), or AlloDerm (103 pg/ml) (p < 0.05). Interleukin-8 and VEGF displayed trends similar to that of IL-6. There were no significant differences in cytokine production between AlloDerm and Bio-A.
Conclusion
This study demonstrated that human macrophages are activated by human dermis-derived biologic and biodegradable meshes in vitro. A wide range of cytokine and growth factor induction was seen among the different mesh products. These differences in M/MØ activation may be related to the proprietary processing technologies of the studied meshes. The study results raise the possibility that these differences in M/MØ activation could indicate varying intensities of inflammation that control integration of different biologic meshes at the sites of hernia repair.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Hernia repair continues to be the most common surgical procedure performed worldwide, with approximately 800,000 herniorrhaphies performed in the United States annually [1, 2] and more than 20 million performed worldwide [3]. Whereas the majority of these procedures are for inguinal hernias, ventral hernia repairs make up a substantial number of cases (~15%). Regardless of the hernia type, successful repair typically relies on the use of a prosthetic implant for reinforcement. Since the first clinical use of synthetic mesh for herniorrhaphy by Usher in 1958 [4, 5], a wide variety of mesh materials have become available for use in hernia repair. Although synthetic meshes are most commonly used, they are contraindicated for infected or potentially contaminated fields [4, 6–8]. Biologic and biodegradable meshes (BMs) offer safer alternatives to nondegradable synthetic meshes where contamination is a concern.
Currently, available BMs are derived from human dermis, porcine dermis, porcine small intestine submucosa, bovine dermis, or bovine pericardium. Although studies have shown BMs to be of great use for hernia repair in infected fields, they have been shown to fail in up to 30% of cases [9–12]. Reducing failure rates with BMs has been difficult, and although their inherent design to biodegrade after implantation is a major factor, other specific causes of mesh failure have yet to be elucidated.
The body initiates powerful inflammatory and reparative responses to biomaterials after implantation. This tissue response can aid in the integration of the mesh biomaterial at the site of implantation via normal wound-healing mechanisms. Conversely, it can induce exaggerated inflammatory and fibrotic responses, which may promote rapid mesh degradation with resultant weakening or failure of the mesh material or excessive scarring that impedes mesh function [13].
The balance between appropriate wound healing and deleterious sequelae is believed to be controlled by cytokines, growth factors, and other chemical-signaling molecules, with monocytes/macrophages (M/MØs) playing pivotal roles [14–17]. For our study, we chose four key M/MØ-secreted regulatory and modulatory chemical-signaling molecules, namely, interleukin (IL)-1β, IL-6, IL-8, and vascular endothelial growth factor (VEGF). All four have important functions necessary for proper wound healing and mesh integration, among other immunoregulatory functions. These various functions allow cytokines to serve as useful markers of M/MØ activation in vitro and to potentially influence in vivo tissue responses to BMs.
To date, biomaterial research involving leukocyte activation and cytokine induction has been focused on synthetic biomaterials [16, 17]. However, few studies have investigated the inflammatory and immunogenic responses of biologic meshes. We recently developed an in vitro model characterizing the interactions between leukocytes and BMs using human peripheral blood mononuclear cells (PBMCs) [18]. Current investigations have sought to establish broader cytokine profiles of the host response to human-derived and biodegradable BMs using fresh human PBMCs.
Materials and methods
Surgical meshes and mesh preparation
For this study, representative acellular human dermis-derived biologic meshes were used including AlloDerm (LifeCell Corp, Branchburg, NJ, USA), AlloMax (CR Bard/Davol Inc, Cranston, RI, USA), and FlexHD (MTF/Ethicon Inc, Somerville, NJ, USA). One synthetic biodegradable mesh, Bio-A (WL Gore & Assoc, Flagstaff, AZ, USA), was used. Bio-A is a nonwoven network of polyglycolic acid (PGA) and trimethylene carbonate (TMC) (www.goremedical.com). Using sterile technique, 5-mm circular mesh samples were prepared with a sterilized paper drill.
Blood product isolation
Peripheral blood mononuclear cells were used as an enriched source of M/MØs. After institutional review board approval and signed informed consent were obtained, PBMCs were isolated and prepared from six healthy volunteers. Approximately 60 ml of peripherally drawn blood was anticoagulated with 200 μl of heparin sodium. The PBMCs were obtained by standard differential centrifugation of anticoagulated whole blood using Histopaque-1077 (Sigma-Aldrich, St. Louis, MO, USA) as a density gradient agent.
After removal of the PBMC layer, the PBMCs were washed three times with sterile normal saline (0.9%). The cell number for each PBMC preparation was determined with standard microscopic quantitation using an AO Bright-Line hemocytometer (Hausser Scientific, Horsham, PA, USA). The resulting cells were resuspended in approximately 10 to 30 ml of RPMI 1640 tissue culture medium based on total cell counts to achieve a concentration of 8.0 × 106 cells/ml of solution. Subsequently, 125 μl of this solution was added to the in vitro cell activation platform, as described in the next section.
In vitro cell activation platform
To develop a simple in vitro cell activation platform, standard sterile 96-well tissue culture–treated polystyrene plates (Corning, Corning, NY, USA) were used. Each well received its components (mesh ± cells and tissue culture media) in sterile fashion in a laminar flow hood. The stock tissue culture media (TCM) was composed of RPMI 1640 medium (Sigma-Aldrich, St. Louis, MO, USA), 10% fetal bovine serum (Gemini Bio-Products, West Sacramento, CA, USA), 1% penicillin-streptomycin, and 0.2% Amphotericin B (Invitrogen Corp., Carlsbad, CA, USA).
Four 5-mm circle pieces of each mesh type were placed in their designated wells (24 per mesh product). Next, 125 μl of leukocyte–TCM solution was placed into the designated wells (concentration of 1.0 × 106 cells per well after dilution with TCM based on the initial cell count). The control wells did not receive any mesh pieces, but likewise received 125 μl of leukocyte–TCM solution. The resulting tissue culture plates were left undisturbed for 20 min at 37°C to allow the cells to settle on the mesh or well bottom, thus ensuring initial adhesion without disruption. An additional 125 μl of TCM then was placed inside the wells to reach 250 μl of solution in each well. Whereas the negative control well received an additional 125 μl of TCM, the positive control well received 125 μl of a TCM–lipopolysaccharide (LPS) solution (concentration of 100 ng LPS/ml TCM). The resulting 96-well plates were incubated at 37°C with 5% carbon dioxide for 7 days.
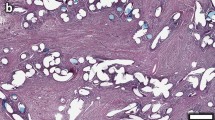
On experimental day 7, the resulting culture supernatants were transferred to a new 96-well plate and centrifuged at 3,000 rpm for 3 min to create a PBMC pellet at the bottom of each V-shaped well. This step helped to limit cellular contamination of the supernatants. The resulting culture supernatant samples were transferred from the centrifuged plate, separated into multiple aliquots, and preserved at −70°C for ease of further testing. The resulting BMs from each study were fixed in buffered formalin, processed, embedded in paraffin, and sectioned. The sections were stained with hematoxylin and eosin (H&E) for histologic evaluation.
Cytokine expression
To determine cytokine concentrations of IL-1β, IL-6, IL-8, and VEGF in the various culture supernatants, we used a bead-based multiplex immunoassay system (Bio-Plex; Bio-Rad, Hercules, CA, USA). Due to highly elevated levels of IL-8 in pilot experiments, samples undergoing IL-8 analysis were diluted 1:50 in TCM, whereas samples undergoing IL-1β, IL-6, and VEGF analysis were diluted 1:5 in TCM.
All standards, cytokine beads, detection antibodies, and reagents used in this study were manufactured by Bio-Rad. In brief, premixed standards were reconstituted with TCM. After the 96-well filter plates (MultiScreen HTS; Millipore Corp., Billerica, MA, USA) had been prewetted with assay buffer A (assay buffer), they were vacuum filtered. Anticytokine bead solution (IL-1β, IL-6, IL-8, and VEGF) was prepared with assay buffer and added to each well, then vacuum-filter washed twice with wash buffer A (wash buffer). Standards and culture supernatant samples were added to corresponding wells and allowed to incubate on a plate shaker in darkness for 30 min.
After this and subsequent incubations, the plate was vacuum filtered, followed by three vacuum-filter washings with wash buffer. Detection antibody solution (IL-1β, IL-6, IL-8, and VEGF) was prepared with detection antibody diluent, added to each well, and incubated on a plate shaker in darkness for 30 min. Streptavidin–phycoerythrin solution was prepared with assay buffer, added to each well, and incubated on a plate shaker in darkness for 10 min. After final washings, each well’s contents were resuspended with assay buffer. Each plate was run through the Bio-Plex array reader, in which peak fluorescence was measured along with the corresponding specific cytokine bead (IL-1β, IL-6, IL-8, or VEGF). Finally, cytokine levels were quantitated for each culture supernatant sample using Bio-Plex Manager software (Bio-Rad, Hercules, CA, USA) and expressed as picograms (pg) of cytokine per milliliter (ml) of culture supernatant.
Statistical analysis
For each mesh group, IL-1β, IL-6, IL-8, and VEGF levels were compared using analysis of variance (ANOVA) and Student’s t-test. All p values less than 0.05 were considered statistically significant.
Results
Mesh-induced cytokine expression
Cytokine data were obtained from assayed culture supernatants after 7 experimental days and expressed as mean picograms of IL-1β, IL-6, IL-8, and VEGF per milliliter of culture supernatant. As seen in Fig. 1, cytokine expression varied among different mesh products. For IL-1β, there were statistically significant differences between AlloDerm, AlloMax, FlexHD, and Bio-A, except for AlloDerm versus Bio-A (p = 0.17) (Table 2). As the highest inducer of IL-1β (2,591 pg/ml; range, 37–8,601 pg/ml), FlexHD stimulated more than five times the production of IL-1β versus AlloMax (517 pg/ml; range, 6–2,161 pg/ml) and more than 50 times that of AlloDerm (48 pg/ml; range, 2–262 pg/ml) or Bio-A (28 pg/ml; range, 6–97 pg/ml) (Table 1).
Mesh-induced cytokine expression from day 7 culture supernatants. Each graph corresponds to one cytokine, as labeled. Values, expressed as picograms (pg) per milliliter (ml), represent mean cytokine production for each mesh. Both controls, namely, negative (“cells only”) and positive (cells and LPS, lipopolysaccharide), were unexposed to mesh. Cytokine levels were obtained using Bio-Plex multiplex immunoassay kits. See Table 1 for detailed cytokine expression numbers
As shown in Table 1, IL-6 data also displayed varied levels between mesh products. However, AlloMax induced a significantly higher quantity of IL-6 (38,343 pg/ml; range, 579–121,204 pg/ml) than FlexHD (19,317 pg/ml; range, 293–42,973 pg/ml) (Table 1). As with IL-1β, a minimal quantity of IL-6 was induced by both AlloDerm (103 pg/ml; range, 5–657 pg/ml) and Bio-A (191 pg/ml; range, 18–990 pg/ml) (Table 1). Cytokine expression for both IL-8 and VEGF followed trends similar to that of IL-6, as can be seen in Fig. 1. Table 1 displays further cytokine level data.
Discussion
When contraindications exist for placement of synthetic prosthetic meshes during hernia repair, biologic meshes (BMs) typically are used [4, 6–8]. Key to a successful hernia repair is proper integration of the BM scaffold through cellular and fibrovascular ingrowth followed by tissue remodeling [6, 19]. Implantation of a BM induces an acute and possible chronic inflammatory response. Although initial inflammation is necessary for activation of the immune response and promotion of wound healing and mesh remodeling, excessive inflammation may lead to rapid degradation or encapsulation of the BM [20–22]. This balance of tissue reactions is controlled by monocytes/macrophages (M/MØs), the crucial mediators of wound healing and mesh integration.
Biologic meshes are being used in increasing numbers. However, the mediators and mechanisms controlling inflammatory and immune responses to various human tissue-derived BMs have not been substantially investigated. In a pilot study, we previously demonstrated IL-1β production from PBMCs in response to human-derived BMs [18]. Our current study investigated a broad range of various cytokine productions in a larger population of healthy subjects.
Interleukin-1β is a key regulatory cytokine necessary for the integration of implanted biomaterials. It acts as a principal inducer of the acute inflammatory response, with functions including stimulation of the acute phase response and hematopoiesis as well as promotion of wound-healing functions via fibroblast activation and recruitment [23–25].
In this experiment, we observed elevated activation of M/MØs from FlexHD in terms of IL-1β production compared with that of the other three mesh products. Elevated production of IL-1β may assist in mesh integration through fibroblast proliferation and stimulation, which would result in cellular repopulation followed by native collagen matrix deposition. On the other hand, as Barrientos et al. [26] elucidate, chronically induced IL-1β may lead to exaggerated activity of matrix metalloproteinases (MMPs). This in turn could lead to accelerated degradation of the implanted biomaterial, with resultant mesh failure and hernia recurrence. The true clinical implications of an exaggerated IL-1β production by FlexHD remain unknown. This phenomenon undoubtedly warrants further investigation.
Acute-phase responses also are strongly influenced by IL-6, which lends itself as both a pro- and an antiinflammatory cytokine [27–29]. Through stimulation of acute-phase proteins such as C-reactive protein, IL-6 plays an important role in innate immunity. Other functions of IL-6 include lymphocyte activation, differentiation, and proliferation [27, 30, 31]. Its antiinflammatory activities may serve as counterregulatory agents limiting tissue degradation through possible incitement of MMP inhibitors [27]. Stimulation of acute inflammation and innate immunity is likewise a function of IL-8 via its principal action as a potent chemokine.
In addition, IL-8 activates neutrophils and acts as a direct angiogenesis stimulator through endothelial chemotaxis and induction of endothelial proliferation [29, 31, 32]. Although data demonstrating cytokine induction from BMs are limited, Xu et al. [22] showed a qualitative elevation of IL-6 from 10- and 20-day serum samples after implantation of AlloDerm in an animal model. Our experiment demonstrated highly elevated levels of IL-6 and IL-8 in the AlloMax group (Fig. 1; Table 1). Compared with AlloMax, FlexHD, although still highly elevated compared with AlloDerm and Bio-A, induced less than one-half of IL-6 and one-fourth of IL-8.
Finally, VEGF appears to act in a proinflammatory and pro–wound-healing manner. Its main functions of angiogenesis stimulation and promotion of vascular permeability assist with recruitment of both pro- and antiinflammatory mediators [17, 29, 33]. Evidence also supports VEGF as a direct inducer of chronic inflammation secondary to the stimulation of proinflammatory cytokines in endothelial cells [34, 35]. Angiogenesis is one of the most important factors for mesh integration, thus giving vital roles to angiogenic cytokines and growth factors such as IL-8 and VEGF. Without an adequate vascular supply, continued inflammatory cells cannot be recruited to sites of tissue repair, thus limiting immune function and retarding scaffold remodeling.
Although not as profound, VEGF levels paralleled those of IL-6 and IL-8 in our study. AlloMax continued to display greater cytokine induction than the other three meshes (Fig. 1; Table 1). Whether this translates to faster matrix remodeling and native collagen deposition in vivo is questionable. However, angiogenesis is believed to be intensified with such a heightened response.
Regarding mesh composition, all three biologic meshes tested are composed of cadaver-donated human dermis. However, each mesh product undergoes a different method of processing, decellularization, and sterilization from each manufacturer before distribution (Table 3). Given the various solvents and methods used by each manufacturer for processing and sterilization, the long-term effects of these proprietary methods have the potential to influence the decellularized tissue. It is likely that the processing affects or modifies the matrix in a way that is undetected grossly and microscopically but induces lasting biochemical and biomolecular changes [13, 36, 37]. These matrix alterations in turn may influence foreign recognition and antigen presentation, causing a varying response by tissue macrophages. Such deferential immunogenic potential may, in turn, affect mesh performance in the clinical setting. Profound activation of proinflammatory cytokines by FlexHD and AlloMax may be deleterious to the performance of these grafts compared with AlloDerm.
Due to the aforementioned processing of dermal tissues and the high production costs associated with procuring human-derived tissues, scientists are continuously developing synthetic biodegradable scaffolds [38]. One popular synthetic scaffold on the market is Bio-A, which we have included in our evaluation with biologic meshes due to its biodegradability in vivo. Although it is a synthetic scaffold, Bio-A exhibits properties similar to those of biologic meshes. Its resorption time, reported to be approximately 6 months (www.goremedical.com), is similar to the degradation times seen in non–cross-linked acellular dermis [4, 21, 22].
Interestingly, we found that Bio-A and AlloDerm were very similar in inducing a minimal amount cytokine production from PBMCs (Fig. 1). Although PGA and TMC are commonly used in suture material, it is unclear whether the low level of macrophage stimulation results from the limited bioreactivity of the degradation products. Perhaps the large amount of PGA:TMC within the mesh produces a toxicity that inhibits nearby cells. This assertion, however, needs further investigation.
Conclusion
We have shown that biologic and biodegradable mesh prostheses induce a wide range of cytokine responses from PBMCs in vitro. Moreover, although the three human dermis-derived dermis products use the same initial tissue type from human cadavers, each displays profound differences in provoking cellular responses. AlloMax was the greatest inducer in three of the four tested cytokines. AlloDerm, on the other hand, was the lowest inducer of the biologic meshes, with results similar to those of Bio-A, a biodegradable synthetic mesh. The likely explanation for the wide variation in biologic responses lies in the different proprietary processing and sterilization techniques used by the mesh manufacturers.
Although we did not correlate cytokine expression with in vivo mesh performance, our results raise the possibility that the differences in M/MØ activation indicate varying intensities of local inflammation that control integration of different biologic meshes at the sites of hernia repair. We believe this study provides a strong foundation for future comparative immunologic studies in vivo. Overall, further understanding of the immunologic effects of cadaveric biologic meshes will not only allow for comparison between existing products but may also lead to mesh modifications and subsequent improvements in their clinical performance.
References
Gray SH, Hawn MT, Itani KM (2008) Surgical progress in inguinal and ventral incisional hernia repair. Surg Clin North Am 88:17–26, vii
Rutkow IM (2003) Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin North Am 83:1045–1051, v–vi
Kingsnorth A, LeBlanc K (2003) Hernias: inguinal and incisional. Lancet 362:1561–1571
Bachman S, Ramshaw B (2008) Prosthetic material in ventral hernia repair: how do I choose? Surg Clin North Am 88:101–112, ix
Udwadia T (2006) Inguinal hernia repair: the total picture. J Min Access Surg 2:144–146
Jin J, Rosen MJ, Blatnik J, McGee MF, Williams CP, Marks J, Ponsky J (2007) Use of acellular dermal matrix for complicated ventral hernia repair: does technique affect outcomes? J Am Coll Surg 205:654–660
Milburn ML, Holton LH, Chung TL, Li EN, Bochicchio GV, Goldberg NH, Silverman RP (2008) Acellular dermal matrix compared with synthetic implant material for repair of ventral hernia in the setting of perioperative Staphylococcus aureus implant contamination: a rabbit model. Surg Infect Larchmt 9:433–442
Saettele TM, Bachman SL, Costello CR, Grant SA, Cleveland DS, Loy TS, Kolder DG, Ramshaw BJ (2007) Use of porcine dermal collagen as a prosthetic mesh in a contaminated field for ventral hernia repair: a case report. Hernia 11:279–285
Hiles M, Record Ritchie RD, Altizer AM (2009) Are biologic grafts effective for hernia repair? A systematic review of the literature. Surg Innov 16:26–37
Schuster R, Singh J, Safadi BY, Wren SM (2006) The use of acellular dermal matrix for contaminated abdominal wall defects: wound status predicts success. Am J Surg 192:594–597
Shaikh FM, Giri SK, Durrani S, Waldron D, Grace PA (2007) Experience with porcine acellular dermal collagen implant in one-stage tension-free reconstruction of acute and chronic abdominal wall defects. World J Surg 31:1966–1972; discussion 1973–1964, 1975
Bellows CF, Albo D, Berger DH, Awad SS (2007) Abdominal wall repair using human acellular dermis. Am J Surg 194:192–198
Badylak SF (2004) Xenogeneic extracellular matrix as a scaffold for tissue reconstruction. Transpl Immunol 12:367–377
Badylak SF, Valentin JE, Ravindra AK, McCabe GP, Stewart-Akers AM (2008) Macrophage phenotype as a determinant of biologic scaffold remodeling. Tissue Eng Part A 14:1835–1842
Gordon S, Taylor PR (2005) Monocyte and macrophage heterogeneity. Nat Rev Immunol 5:953–964
Schachtrupp A, Klinge U, Junge K, Rosch R, Bhardwaj RS, Schumpelick V (2003) Individual inflammatory response of human blood monocytes to mesh biomaterials. Br J Surg 90:114–120
Schutte RJ, Parisi-Amon A, Reichert WM (2009) Cytokine profiling using monocytes/macrophages cultured on common biomaterials with a range of surface chemistries. J Biomed Mater Res A 88:128–139
Orenstein S, Kaur M, Klueh U, Kreutzer D, Novitsky Y (2009) Activation of human monocytes by human biologic meshes in vitro (abstract). J Surg Res 151:290
Butler CE (2006) The role of bioprosthetics in abdominal wall reconstruction. Clin Plast Surg 33:199–211, v–vi
Jansen PL, Mertens Pr P, Klinge U, Schumpelick V (2004) The biology of hernia formation. Surgery 136:1–4
Sandor M, Xu H, Connor J, Lombardi J, Harper JR, Silverman RP, McQuillan DJ (2008) Host response to implanted porcine-derived biologic materials in a primate model of abdominal wall repair. Tissue Eng Part A 14:2021–2031
Xu H, Wan H, Sandor M, Qi S, Ervin F, Harper JR, Silverman RP, McQuillan DJ (2008) Host response to human acellular dermal matrix transplantation in a primate model of abdominal wall repair. Tissue Eng Part A 14:2009–2019
Kaback LA, Smith TJ (1999) Expression of hyaluronan synthase messenger ribonucleic acids and their induction by interleukin-1 beta in human orbital fibroblasts: potential insight into the molecular pathogenesis of thyroid-associated ophthalmopathy. J Clin Endocrinol Metab 84:4079–4084
Oncul O, Yildiz S, Gurer US, Yeniiz E, Qyrdedi T, Top C, Gocer P, Akarsu B, Cevikbas A, Cavuslu S (2007) Effect of the function of polymorphonuclear leukocytes and interleukin-1 beta on wound healing in patients with diabetic foot infections. J Infect 54:250–256
Yamada Y, Itano N, Hata K, Ueda M, Kimata K (2004) Differential regulation by IL-1 beta and EGF of expression of three different hyaluronan synthases in oral mucosal epithelial cells and fibroblasts and dermal fibroblasts: quantitative analysis using real-time RT-PCR. J Invest Dermatol 122:631–639
Barrientos S, Stojadinovic O, Golinko MS, Brem H, Tomic-Canic M (2008) Growth factors and cytokines in wound healing. Wound Repair Regen 16:585–601
Barton BE (1997) IL-6: insights into novel biological activities. Clin Immunol Immunopathol 85:16–20
Heinrich PC, Behrmann I, Haan S, Hermanns HM, Muller-Newen G, Schaper F (2003) Principles of interleukin (IL)-6-type cytokine signaling and its regulation. Biochem J 374:1–20
Sunderkotter C, Steinbrink K, Goebeler M, Bhardwaj R, Sorg C (1994) Macrophages and angiogenesis. J Leukoc Biol 55:410–422
Novitsky YW, Litwin DE, Callery MP (2004) The net immunologic advantage of laparoscopic surgery. Surg Endosc 18:1411–1419
Labler L, Rancan M, Mica L, Harter L, Mihic-Probst D, Keel M (2009) Vacuum-assisted closure therapy increases local interleukin-8 and vascular endothelial growth factor levels in traumatic wounds. J Trauma 66:749–757
Mukaida N, Harada A, Matsushima K (1998) Interleukin-8 (IL-8) and monocyte chemotactic and activating factor (MCAF/MCP-1), chemokines essentially involved in inflammatory and immune reactions. Cytokine Growth Factor Rev 9:9–23
Berse B, Brown LF, Van de Water L, Dvorak HF, Senger DR (1992) Vascular permeability factor (vascular endothelial growth factor) gene is expressed differentially in normal tissues, macrophages, and tumors. Mol Biol Cell 3:211–220
Yoo SA, Bae DG, Ryoo JW, Kim HR, Park GS, Cho CS, Chae CB, Kim WU (2005) Arginine-rich antivascular endothelial growth factor (anti-VEGF) hexapeptide inhibits collagen-induced arthritis and VEGF-stimulated productions of TNF-alpha and IL-6 by human monocytes. J Immunol 174:5846–5855
Lee TH, Avraham H, Lee SH, Avraham S (2002) Vascular endothelial growth factor modulates neutrophil transendothelial migration via upregulation of interleukin-8 in human brain microvascular endothelial cells. J Biol Chem 277:10445–10451
Badylak SF, Gilbert TW (2008) Immune response to biologic scaffold materials. Semin Immunol 20:109–116
Gilbert TW, Sellaro TL, Badylak SF (2006) Decellularization of tissues and organs. Biomaterials 27:3675–3683
Blackwood KA, McKean R, Canton I, Freeman CO, Franklin KL, Cole D, Brook I, Farthing P, Rimmer S, Haycock JW, Ryan AJ, MacNeil S (2008) Development of biodegradable electrospun scaffolds for dermal replacement. Biomaterials 29:3091–3104
Acknowledgment
This study was funded in part by institutional support from the University of Connecticut Health Center.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Orenstein, S.B., Qiao, Y., Kaur, M. et al. Human monocyte activation by biologic and biodegradable meshes in vitro. Surg Endosc 24, 805–811 (2010). https://doi.org/10.1007/s00464-009-0664-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-009-0664-3