Abstract
Background
Previous studies have relied on conversion rate and operative time for construction of learning curves in laparoscopic colorectal surgery. The authors hypothesized that conversion rate and operative time were less important than complication and readmission rates in defining good outcomes and hence the learning curve.
Methods
A database of 287 consecutive laparoscopic colorectal resections from a single tertiary referral center was analyzed. Outcome measures included operative time, conversion rate, major and minor complications, length of hospital stay, and the 15- and 30-day hospital readmission rate. Data were analyzed both by surgeons and by quartile case numbers.
Results
A total of 151 right colectomies and 136 left colectomies were performed between 1995 and 2005. For both right and left colectomies, the conversion rate decreased in each of the first three quartiles, reaching a nadir of 0% for right colectomies and 3% for left colectomies in the third quartile. The conversion rates increased slightly in the fourth quartile. The operative time remained stable for three quartiles, then increased slightly in the fourth quartile. Two surgeons managed 199 of the 287 cases. Analysis of the two high-volume surgeons demonstrated that for left-sided resections, the surgeon with the shorter operative times had the higher major complication rate (13% vs 2%), overall complication rate (22% vs 2%), 30-day readmission rate (13% vs 0%), and length of stay (3.8 vs 3.1 days) (p < 0.05 for all comparisons).
Conclusions
In this series, operative time failed to decrease with experience, and shorter operative times did not correlate with better clinical outcomes. The failure of operative time to decline with experience often reflects surgeons’ willingness to attempt more difficult cases rather than an accurate representation of a “learning curve.” Therefore, complication and readmission rates are more important than operative time and conversion rates for evaluating the learning curve and quality of laparoscopic colorectal surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopic colon surgery is a technically difficult procedure that requires advanced training for the surgeon. Previous studies have attempted to capture the so-called “learning curve” in that training process. Most frequently, technical indicators such as conversion rate and operative time have been used to measure such learning curves [8].
We argue that laparoscopic colon surgery and surgeons performing laparoscopic colon surgery should be evaluated no differently than other surgical procedures and surgeons, with patient outcome considered paramount. We further hypothesize that technical improvements reflected by shorter operative time or lower conversion rate do not always translate into better patient outcomes. We propose that outcome measures such as mortality and morbidity rate, length of hospital stay, and readmission rate not only be incorporated into future evaluation of any new laparoscopic surgical procedure, but also be emphasized as the most important indicators of surgeon performance.
Patients and methods
Patients
Between October 1995 and June 2005, 287 consecutive laparoscopic colorectal procedures were performed at the Massachusetts General Hospital in Boston. This represents our early experience with laparoscopic colon surgery (Fig. 1). A database approved by the institutional review board was constructed retrospectively for evaluation of these cases. Specifically, patient demographics, indications for surgery, surgical techniques, operative time, and conversion to open surgery were recorded according to the hospital record. Patient outcome measures such as major and minor complications, length of postoperative hospital stay, and both 15- and 30-day readmissions also were included in the database.
Surgeons and surgical techniques
Eight surgeons performed all the laparoscopic colon surgery during the study period. Among them, two high-volume surgeons performed 70% (199/287) of the procedures. These two surgeons used similar techniques.
Right-sided colonic resections were performed using a lateral-to-medial approach. Briefly, the lateral peritoneal attachments of the right colon were first lysed using the Harmonic Scalpel. The ileocolic pedicle then was divided intracorporeally using a vascular stapler. The colon was either first exteriorized through a 5-cm incision by enlargement of a trocar site followed by resection and primary anastomosis extracorporeally or first anastomosed intracorporeally with terminal ileum followed by specimen extraction. Most cases (134/151) in this series were managed with extracorporeal anastomoses.
Left-sided colon resections, including left hemicolectomies, transverse colectomies including the splenic flexure, sigmoid colectomies, and low anterior resections were performed by first mobilizing the splenic flexure with the Harmonic Scalpel. The descending and/or sigmoid colon then were freed from lateral peritoneal attachments and elevated against the anterior abdominal wall. The inferior mesenteric artery pedicle was divided with a vascular stapler. The distal sigmoid colon or rectum was cleared off and divided with an EndoGIA stapler (US Surgical Corp., Norwalk, CT). The proximal colon then was exteriorized and transected at the desired proximal margin. The metal anvil of an EEA stapler (US Surgical Corp., Norwalk, CT) was secured in the colonic lumen with a purse-string suture. The colon was returned into the abdomen, and a stapled anastomosis was completed with the EEA stapler inserted transanally.
The techniques used by the six low-volume surgeons varied. For example, one surgeon preferred hand-assisted laparoscopic colon resection, whereas another surgeon exteriorized the colon through a Pfannenstiel-type incision and divided vessels extracorporeally.
Definition of conversion to open surgery
A case of laparoscopic colon resection is considered converted to open surgery if an incision is made for any purpose other than anastomosis or specimen extraction. This determination is made at the time of surgery by the operating surgeon, as documented by the operative report. The records of all 26 cases converted to open surgery were carefully studied to ensure that all surgeons adhered to this uniform definition consistently throughout the study period.
Data analysis
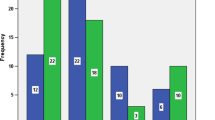
For purposes of our analyses, cases were first divided into right- and left-sided resections. Within each group, the cases were further divided into four quartiles in chronologic order. In general, the first quartile cases were performed between 1995 and 2000, the second quartile cases between 2000 and 2001, the third quartile cases between 2002 and 2003, and the fourth quartile cases between 2004 and 2005 (Fig. 1). Approximately 30 to 40 cases were included in each quarter. Surgical outcomes including operative time, conversion, major and minor complications, length of hospital stay, and 15- and 30-day readmissions were calculated for each quartile.
In addition, cases managed by the two high-volume surgeons were analyzed separately so their individual learning curves could be tracked accurately for laparoscopic colon surgery. Their surgical outcomes indicators were compared by Student t-test (for operative time) and chi-square test (for all other indicators). A p value less than 0.05 was regarded as statistically significant.
Results
A total of 287 consecutive patients (135 men and 152 women) underwent laparoscopic colon resection between October 1995 and June 2005. The average patient age at the time of surgery was 59.5 years (range, 22–96 years). The indications for surgery were malignant diseases in 84 patients (73 colon cancers, 6 rectal cancers, 1 appendiceal cancer, and 4 carcinoids) and benign diseases in 203 patients (84 colorectal polyps cases, 94 diverticulitis cases, 17 Crohn’s disease cases, 2 ischemic colitis cases, 6 others). Analyses of case indications by quartile failed to show any significant shifts with time, except for a trend toward more left-sided resections performed for diverticular disease in the later quartiles (p = 0.11, chi-square test, data not shown).
Right-sided resections included mostly right colectomies. Left-sided resections included 102 sigmoid colectomies, 12 low anterior resections, 8 transverse colectomies, and 14 left hemicolectomies. Patient characteristics are summarized in Table 1 for right- and left-sided resections.
Overall outcomes
Operative time
As shown in Table 2, the mean operative time was 150 min (range, 50–275 min) for right-sided resections and 181 min (range, 64–371 min) for left-sided resections. This difference was highly significant (p < 0.05). Interestingly, the quartile mean operative time did not decrease for right-sided resections, and actually increased slightly for left-sided colectomies over the last two quartiles.
Conversion to laparotomy
The overall rate of conversion to laparotomy was higher for left- than for right-sided resections (19% vs 7%; p = 0.001). Quartile analyses showed that the conversion rate for right-sided resection decreased steadily to a nadir of 0 in the third quartile, but increased slightly in the fourth quartile. Similarly, the number of cases converted to open surgery decreased for left-sided resection as well, reaching a nadir of 3% (1 in 34 consecutive cases) before increasing slightly in the fourth quartile to 12%.
The reasons for conversion to open surgery varied between left- and right-sided resections (Table 3). The majority of right-sided conversions (60%) occurred because of inadequate mobilization of the colon. In three cases, the right colon was densely adhered to the pelvic sidewall. In one case, a cecal cancer was found to invade the bladder and the sigmoid colon. Two other cases were converted secondary to the patient’s body habitus. Obesity prevented adequate mobilization and exteriorization of the specimen.
Approximately one-third of the left-sided conversions were secondary to unsatisfactory colorectal anastomosis. These conversions resulted from inability to complete the rectal dissection (n = 2), inability to fully advance the EEA stapler transanally (n = 1), rectal laceration during insertion of the EEA stapler (n = 3), or unsatisfactory EEA staple line at rigid sigmoidoscope air insufflation test (n = 3). An unsatisfactory colorectal anastomosis carries with it a high morbidity rate. Of the nine cases converted for that reason, the patients in three cases went on to experience postoperative anastomotic leak, which necessitated a colostomy in two patients and image-guided catheter drainage in the third patient.
An additional 20% of the left-sided conversions (n = 5) resulted from inability to mobilize the colon. Of these five cases, two resulted from inability to mobilize the splenic flexure during the second quartile. Although there was no intraoperatively recognized ureteral injury in this series, two cases of left-sided resection (12%) had to be converted because of inability to identify or follow the left ureter.
Complications
There was no surgical mortality in this series of 287 patients. The overall morbidity rate was 13.5% (4.5% major and 9.1% minor complications). Table 4 categorizes all the complications in this series. Overall, major surgical complications such as anastomotic leak, ureteral injury, intraabdominal abscess, and wound dehiscence occurred at a rate less than 1%, respectively. The only category of major complication that exceeded a rate of 1% involved access-related injuries. The details of those four injuries are listed in the footnotes of Table 4. A total of 13 patients (4.5%) were readmitted for symptoms of bowel obstruction. This occurred more frequently after right-sided (6.6%) than after left-sided (2.2%) resections. All but one patient was treated expectantly without operative intervention. Although right-sided resections resulted in fewer major complications, they were associated with significantly more minor complications. This resulted in comparable overall morbidity rates for right- and left-sided resections (15% vs 13%; p = 0.60).
Because of the overall low rates, it is difficult to discern any progress made in reducing morbidities. The only convincing trend can be observed in the incidences of major complications with left-sided resections. There were five major complications during the first 34 cases (2 anastomotic leaks, 1 trocar-site hernia, 1 epigastric vessel injury, and 1 evisceration). In the third and fourth quartiles, however, only one major complication per quartile was recorded.
Length of stay and readmissions
Unlike open colectomies, for which a standardized clinical pathway exists [7], there is no uniform postoperative pathway for laparoscopic colon surgery at our institution. Rather, individual surgeons determine postoperative care and discharge planning for their patients. Patients typically are discharged when their pain is well controlled with oral narcotics and they can tolerate a liquid diet. They do not have to pass flatus or have a bowel movement before discharge. In the current series, the median length of hospital stay for both right- and left-sided resections was the same at 3 days.
In this series, 8% of the patients required readmission after their initial discharge from the hospital. This is similar to an open series previously reported from our institution [7]. Details of readmissions within 15 and 30 days after surgery are provided in Table 5. Readmissions were more common after right-sided resections because ileus or partial small bowel obstruction occurred more often in these patients. Possible explanations for this observation are given in the Discussion section.
Surgeon-specific outcomes
In addition to comparing right- and left-sided laparoscopic colon resections, we also performed in-depth analyses of the cases managed by the two high-volume surgeons. During the study period, these two surgeons managed 96 and 103 cases, respectively. Taken together, they managed 199 of the 287 cases (70%). Because these two surgeons started performing laparoscopic colon surgery at about the same time and adopted similar operative techniques, their personal first 100 cases may represent a true learning curve for this procedure.
Tables 6a and 6b list the 199 cases managed by these two surgeons and their outcomes. For right-sided resections, surgeon A was slightly faster than surgeon B. There were no significant differences in conversion rates or any of the patient outcomes measures (p = NS).
For left-sided resections, surgeon B was faster than surgeon A (156 vs 182 min; p = 0.002). Both surgeons had similar conversion rates. Surgeon A’s patients, however, enjoyed significantly better outcomes than surgeon B’s patients. Specifically, surgeon A’s major and minor complication rates were significantly lower than those of surgeon B. On the average, surgeon A’s patients stayed 0.7 day less in the hospital than surgeon B’s patients. In addition, surgeon A had no readmissions within 30 days, whereas surgeon B had a readmission rate exceeding 10% for the same period.
Postoperative transfusions also were analyzed. Whereas 10% of surgeon B’s patients (10/103) received postoperative transfusion (1 to 7 units of packed red blood cells), none of surgeon A’s patients required postoperative transfusion. Postoperative transfusion requirements were significantly correlated with major complications, but not with minor or overall complications (Table 7).
Discussion
The current study first reiterates what has been stated in many other reports [2–4, 8], that laparoscopic colorectal surgery can be performed safely with minimal risk to patients. There was no perioperative mortality in 287 consecutive cases at our institution. Major surgical complications such as anastomotic leak, ureteral injury, intraabdominal abscess formation, and wound dehiscence all occurred at a rate less than 1%, respectively. The overall morbidity rate of 13.5% is comparable with the morbidity rate of 16.7% from a concurrent series of open colorectal resections performed by a different surgeon at the same institution [7]. The 30-day readmission rate was 8%, which also is comparable with the readmission rate of 6.5% reported in that open series. The median length of hospital stay in the series was 3 days, almost 1 day shorter than the median stay of 3.7 days reported for the concurrent open series.
Our results are also in line with those of other published laparoscopic colectomy series. Bennett et al. [2] reported a series of 1,194 laparoscopic colectomies with an overall conversion rate of 23% and a morbidity rate of 20%. The Clinical Outcomes of Surgical Therapy (COST) study of 872 patients reported a conversion rate of 21% and a morbidity rate of 21% [3]. Recently, Tekkis et al. [8] published a series of 900 patients undergoing laparoscopic colon surgery. For right-sided resections, the conversion rate was 8.1%, and the complication rate was 20.8%. For left-sided resection, the conversion rate was 15.3%, and complication rate was 17.8%. Our conversion rates were 7% for right-sided resections and 19% left-sided resections, and our overall complication rates were, respectively, 15% and 13%.
In general, right-sided resections are regarded as simpler procedures requiring less time to perform than left-sided resections. Curiously, however, our right-sided resections resulted in more morbidity than our left-sided resections. Others have reported similar findings [8]. Closer inspection showed that this high morbidity rate was caused primarily by bowel obstructive symptoms requiring either prolonged hospitalization after surgery or readmission after discharge.
We initially hypothesized that the transient ileus/obstruction phenomenon of right-sided resection was attributable to the way that extracorporeal anastomoses are constructed. Excess traction applied to the terminal ileum and colon may cause venous congestion or a small hematoma in the bowel mesentery, which in turn would cause prolonged edema at the anastomosis postoperatively. Further analyses, however, showed that intracorporeal anastomoses actually had a higher incidence of postoperative bowel obstructive complications than extracorporeal anastomoses (11.8% vs 5.2%; p < 0.05). It is thus unclear to us why right-sided resections carry a higher incidence of postoperative ileus than left-side resections, or whether it is a phenomenon unique only to laparoscopic colon surgery.
Previous studies have used two technical parameters, conversion rate and operative time, as convenient surrogates for constructing the learning curve. Reports of these studies concluded that with practice and experience, operative time [1], conversion rate [5, 6], or both [4, 8] fall, indicating mastery of laparoscopic colorectal surgery by the surgeon. On the basis of our data, we question whether these technical parameters are the correct surrogates for measuring the learning curve. When analyzed by quartiles, our mean operative time for right-sided resections did not change significantly, and it actually went up for left-sided resections. We submit that as surgeons become more experienced, they take on more challenging cases, perhaps offsetting their increasing operative speed and declining conversion rate. The same argument has been put forth by others [8]. Our data demonstrated a trend toward increasing numbers of left-sided resections being performed for diverticular disease in the later quartiles. It is generally more difficult to perform a laparoscopic colon resection for diverticular disease than to laparoscopically resect either polyp or early-stage cancer.
Furthermore, when we analyzed the data from the two high-volume surgeons, we found that the faster surgeon actually had much higher morbidity rates, particularly after left-sided resections (Table 6). By collecting surgeon-specific data, we demonstrated that operative time alone may not be the best measurement of where a surgeon stands on his or her learning curve in performing laparoscopic colorectal surgery. As painstaking as it is to collect patient outcome data such as complication and readmission rates, they are critical for evaluation of surgical skills.
One limitation of this retrospective study was its lack of certain patient information such as body mass index and cormorbidies. Analyses of such information would have allowed us to quantify case difficulties both across quartiles and between individual surgeons. When surgical indications were analyzed by surgeon, surgeon B was found to have performed more resections for cancer than surgeon A (data not shown). However, because the majority of the cancer cases were early stage, we do not believe that the degree of case difficulty differed significantly between the two surgeons because of indication.
Postoperative blood transfusion was required for 10% of surgeon B’s patients, but not for any of surgeon A’s patients. Because a significant correlation exists between postoperative transfusion and major complication, it can be hypothesized either that blood transfusion leads to a weakened immune system, and hence complication, or that complication leads to bleeding, and hence transfusion requirement. Moreover, because two of the three major complications requiring postoperative transfusion (enterotomy upon entry and inferior epigastric artery transection) occurred intraoperatively before any blood transfusion, the latter hypothesis is more likely to be true.
In conclusion, we caution against establishing arbitrary criteria for certifying surgeons to perform new procedures. Instead, we propose that meaningful patient outcome data such as mortality, morbidity, and readmission rates be used as the major measure of surgeon competency (i.e., learning curve mastery) for performing laparoscopic colorectal surgery, or any other advanced laparoscopic procedures. In a practice environment where pay-for-performance is imminent, any preemptive measures taken to ensure quality are likely to be rewarded.
References
Agachan F, Joo JS, Sher M, Weiss EG, Nogueras JJ, Wexner SD (1997) Laparoscopic colorectal surgery: do we go faster? Surg Endosc 11: 331–335
Bennett CL, Stryker SJ, Ferreira MR, Adams J, Beart RW (1997) The learning curve for laparoscopic colorectal surgery: preliminary results from a prospective analysis of 1,194 laparoscopic-assisted colectomies. Arch Surg 132: 41–45
Clinical Outcomes of Surgical Therapy Study Group (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350: 2050–2059
Marusch F, Gastinger I, Schneider C, Scheidbach H, Konradt J, Bruch HP, Kohler L, Barlehner E, Kockerling F, LCSSG (2001) Experience as a factor influencing the indications for laparoscopic colorectal surgery and the results. Surg Endosc 15: 116–120
Pandya S, Murray J, Coller J, Rusin LC (1999) Laparoscopic colectomy: indications for conversion to laparotomy. Arch Surg 134: 471–475
Shah PR, Joseph A, Haray PN (2005) Laparoscopic colorectal surgery: learning curve and training implications. Postgrad Med J 81: 537–540
Stephen AE, Berger DL (2003) Shortened length of stay and hospital cost reduction with implementation of an accelerated clinical care pathway after elective colon resection. Surgery 133: 277–282
Tekkis PP, Senagore AJ, Delaney CP, Fazio VW (2005) Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg 242: 83–91
Acknowledgment
The authors acknowledge the assistance of Deborah McGrath, RN, in the preparation of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, W., Sailhamer, E., Berger, D.L. et al. Operative time is a poor surrogate for the learning curve in laparoscopic colorectal surgery. Surg Endosc 21, 238–243 (2007). https://doi.org/10.1007/s00464-006-0120-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-006-0120-6