Abstract
Background
Incisional hernias are a common complication following abdominal surgery and represent about 80% of all ventral hernia. In uncomplicated postoperative follow-up they develop in about 11% of cases and in up to 23% of cases with wound infections or other forms of wound complications. While conventional mesh repair has been the standard of care in the past, the use of laparoscopic surgery is increasing. It therefore remains uncertain which technique should be recommended as the standard of care.
Objectives
To compare the medical effectiveness and safety of conventional mesh and laparoscopic incisional hernia repair.
Methods
A structured literature search of databases accessed through the German Institute of Medical Documentation and Information (DIMDI) was conducted. English and German literature published until August 2005 was included and their methodological quality assessed.
Results
The search identified 17 relevant publications and included 15 studies for final assessment. Among those were one meta-analysis, one randomized clinical trial (RCT) ,and 13 cohort studies. All studies suffered from significant methodological limitations, such as differences in baseline characteristics between treatment groups, small case numbers, and the lack of adjustment for relevant confounders. Overall, medical effectiveness and safety were similar for both surgical approaches. However, there was a trend towards lower recurrence rates, length of hospital stay, and postoperative pain as well as decreased complication rates for the laparoscopic repair in the majority of studies. The impact of the technique of mesh implantation and mesh fixation as well as the impact of certain patien- related factors was not systematically assessed in any of the studies.
Conclusion
No conclusive differences could be identified between the operative techniques. There was, however, some evidence for a trend towards similar or slightly improved outcomes associated with the laparoscopic procedure. There remains an urgent need for high-quality prospective studies to evaluate this question conclusively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Incisional hernias are defined as a visible and palpable bulge, commonly developing as a complication of abdominal surgical procedures. In Germany, ventral hernia are the second most common hernia type and about 80% of those are represented by incisional hernia [1–4]. Following abdominal surgery, incisional hernia develop in about 11% of cases and in up to 23% of cases with wound infections or other forms of wound complications [5, 6]. The majority of incisional hernia develop within the first two postsurgical years and more than 80% within three years of surgery [2]. The localization and size of the incisional hernia can vary according to the causal abdominal scar. While conservative treatment options can only be used supportively, operative procedures are the only therapeutic treatment option [7]. Operative treatment of incisional hernia should therefore be considered timely, as an increase in hernia size is likely and the risk of developing serious complications, involving emergency surgery, is considerable [7, 8]. Traditionally, open suture repair was used for incisional hernia repair but was associated with recurrence rates as high as 50% [5, 9, 10]. Various surgical approaches have therefore been developed to reduce these unacceptably high complication rates. Nowadays this routinely involves the implantation of alloplastic mesh to strengthen the abdominal wall. Only in hernias smaller than 3 cm in diameter may a wound closure using nonabsorbable sutures be applied [7]. While laparoscopic surgery routinely involves intraperitoneal mesh implantation (IPOM), various implantation techniques for open procedures, such as onlay, inlay, sublay, and underlay, have been developed. Among open repair techniques, the retromuscular sublay technique is currently most commonly used and is considered the standard of care due to decreased recurrence and infection rates [7, 11–13]. Similar to its routine use in laparoscopic surgery, the underlay (intraperitoneal) technique has recently been proposed as an alternative to the sublay technique. However, so far there is little experience with this approach [14].
Both in open and laparoscopic surgery, routine implantation of alloplastic mesh in incisional hernia repair leads to marked reductions in recurrence rates, as low as 0–10% [8, 13, 15]. Though recurrence rates for the open and the laparoscopic surgical approaches have decreased, the superiority of one mesh technique over the other could not be established. While supporters of the laparoscopic approach argue that it could be associated with decreased wound infection rates, less postoperative pain and shorter length of hospital stay, critics emphasize the increased risk of serious complications, such as unrecognized bowel perforations [8, 16, 17]. Furthermore, while the use of metal tacks is currently recommended, there is considerable debate about the additional use of sutures for mesh fixation in laparoscopic surgery [10]. Uncertainty therefore remains regarding the most appropriate techniques or which technique might, under specific patient-related circumstances, be associated with advantages over the other.
Apart from these various approaches to incisional hernia repair, the type of mesh, the mesh–tissue overlap and the mesh fixation play an important role in the short- and long-term outcome following both procedures [7, 10, 18].
The aim of this systematic review is therefore to identify comparative studies evaluating the effectiveness of the two mesh techniques, open compared to laparoscopic surgery for incisional hernia repair, and to investigate the impact of the type of mesh implantation and mesh fixation technique on outcome.
Methods
The objectives of this systematic review were as follows:
-
1.
Compare the medical efficacy/effectiveness and safety of conventional and laparoscopic incisional hernia repair.
-
2.
Identify techniques of mesh implantation (e.g. onlay, inlay, sublay, IPOM) that have advantages over other techniques.
-
3.
Identify factors (e.g. sex, age, recurrent hernia, hernia size, adiposity) where certain techniques have advantages over other techniques.
Relevant publications were identified by means of a structured search (Table 1) of databases accessed through the German Institute of Medical Documentation and Information (DIMDI) as well as by a manual search. The former included the following electronic resources:
SOMED, Cochrane Library – Central, MEDLINE Alert, MEDLINE, CATFILEplus, ETHMED, GeroLit, HECLINET, AMED, CAB Abstracts, GLOBAL Health, IPA, Elsevier BIOBASE, BIOSIS Previews, EMBASE, EMBASE Alert, SciSearch, Cochrane Library – CDSR, NHS-CRD-DARE, NHS-CRD-HTA as well as NHS-EED.
In addition identification of grey literature was attempted through the notification of national surgical associations.
The present report includes literature published up until 31st August 2005. The search parameters can be found in the appendix. There were no restrictions on the target population.
The inclusion criteria were:
-
Primary studies, systematic reviews, meta-analyses and health technology assessments
-
Studies comparing conventional and laparoscopic mesh-implantation techniques
-
Surgical Indication: incisional and ventral hernia
-
Published in English and German
The exclusion criteria were:
-
Outcome parameters deviating from medical effectiveness/efficacy and safety
-
Narrative reviews, congress abstracts, case reports, and case series
-
Surgical indication: other hernia repair and primary ventral hernia
In the process of study selection against the above criteria, assessment of titles and abstracts for relevance was performed independently by two researchers before full-text documents were assessed. The methodological quality of the included studies was assessed applying the criteria recommended by the Scottish intercollegiate guidelines network grading review group (Table 1) [19]. If feasible, a meta-analysis was planned.
Results
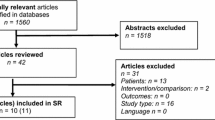
The literature search identified 693 medical publications including 152 relevant to the research question. Attempts to identify grey literature were not successful, while 10 further publications were identified through manual search, leaving a total of 162 reports for review of full texts. Of those, 17 studies were identified as relevant to the particular topic, including two systematic reviews, one health technology assessment (HTA), one RCT and 13 cohort studies (Figure. 1).
The characteristics of the included studies are presented in Table 2. The health technology assessment by Pham et al. [20] and the systematic review by Cassar and Munro [8] did not add any information beyond the included primary studies which had been identified through the present literature search. They were therefore excluded from further assessment.
The selection process left 15 studies for final assessment, of which only five exclusively investigated incisional hernia repair. The 10 remaining studies focused on ventral hernia repair in general, including incisional hernia repair. The majority of the studies followed an observational study design, often using historical cohorts or prospective laparoscopic and historical conventional control groups (Table 2). Furthermore, marked differences in participants’ baseline characteristics, length of follow-up and assessment of outcome measures could be observed between and within studies. This had two important implications: comparability across studies was decreased, and differences within studies led to a substantial risk of bias, thereby compromising the methodological quality of most studies.
With the exception of [21], all reports presented parameters of medical effectiveness as an outcome measure. Safety parameters were presented by all the identified studies. However, the precision of reporting and definition of reported outcomes varied widely. The main outcome measures of medical effectiveness and medical safety identified in this review are presented in Tables 3 and 4. None of the studies reported outcomes related to quality of life or time to initiation of normal activities.
Effectiveness (Table 3)
A consistently shorter length of hospital stay was reported for the laparoscopic procedure. While six studies [4, 16, 22–25] found significantly shorter stays, the remaining studies only observed a trend towards shorter stays in hospital for laparoscopic surgery. Only four studies [22, 23, 25, 26] reported postoperative pain or the need for postoperative pain medication. They consistently found advantages associated with laparoscopic surgery, although only two studies observed statistically significant differences [22, 25]. The evidence on operative time was inconclusive. Only three studies [23, 27, 28] found significantly shorter operative times in conventional surgery, while two studies [24, 29] found significant advantages associated with the laparoscopic technique. Of the remaining studies a trend towards shorter operative time in conservatively operated patients was observed. Recurrence rates were reported in 12 studies and varied from 0 to 35%. While none of the studies reported statistically significant differences between treatment groups, only one study [29] observed (slightly) higher recurrence rates in the laparoscopic surgery group. All the remaining studies found slightly or markedly lower recurrence rates associated with laparoscopic surgery.
Safety (Table 4)
Complication rates varied from 2 to 67%, depending greatly on definition and measurement precision. Laparoscopic surgery was consistently associated with a trend towards lower overall complication rates, with four studies [4, 16, 23, 27] reporting statistically significant differences in favor of laparoscopy. Comparison of specific complications presented difficulties due to varying definitions and the lack of statistical analysis in the majority of studies. However, rates of wound infection and ileus were consistently reported to be lower in laparoscopic groups while intestinal perforation tended to occur less frequently in open surgery. The evidence on seroma formation and reoperation was inconclusive.
Additional research questions
Data on the remaining research questions were scarce. No study planned to compare different techniques of mesh implantation or mesh fixation. Similarly none of the studies investigated patient related characteristics and their impact on the choice of operative technique.
Due to the heterogeneity in study design and study quality, a meta-analysis was not considered appropriate and therefore not conducted.
Discussion
Abdominal operative procedures associated with laparotomies are among the most frequent surgical procedures. Despite marked advances in areas such as operative and anaesthetic techniques as well as the development of supportive devices, this type of surgery is still associated with substantial postoperative morbidity. A serious and frequent complication following this kind of surgery is the development of incisional hernias, which is in turn often associated with recurrences. While recurrence rates following incisional hernia repair in the past have been as high as 50%, improvements in their treatment have led to a marked reduction in recurrence rates in recent years [7, 30–32]. The development and implantation of alloplastic mesh has been especially advantageous and, with the exception of very small hernias, is currently considered routine treatment in the treatment of incisional hernia, both in conventional and laparoscopic surgery [7]. As the laparoscopic repair of incisional hernias has become more common in recent years and the outcome of both have improved substantially there is considerable uncertainty as to the choice of the most appropriate technique.
In an attempt to answer this question, the present systematic review identified 15 relevant studies targeting these two surgical procedures for incisional and ventral hernia repair. Only five studies explicitly focused on the treatment of incisional hernia, while 10 studies investigated ventral and incisional hernia; None of these, however, reported results separately for ventral and incisional hernias.
With recurrence rates of 0 to 35%, the results confirm the improved outcome associated with current techniques of incisional hernia repair. Especially studies with highest recurrence rates [3, 23] either had long follow-up periods or used non-mesh repairs in some of their participants. Overall, outcomes of medical effectiveness and safety did not provide evidence for a substantial difference between the two surgical approaches. However, there is considerable heterogeneity in the reported study results and different outcome measures.
Regarding the specific outcome measures of efficacy and safety, it has to be acknowledged that none of the studies alone is able to provide strong evidence for the superiority of one surgical approach. Considering measures of medical efficacy, such as length of hospital stay and postoperative pain, studies consistently reported superior or a trend towards superior outcome associated with the laparoscopic approach. The evidence regarding recurrence rates is less clear and inconsistent for operative time. In terms of safety, the studies also consistently reported a trend towards decreased overall complication rates, wound infection rates, and postoperative ileus associated with laparoscopic surgery, while there seems to be a trend towards higher rates of intraoperative intestinal perforations associated with laparoscopy. Especially if unrecognized, this represents a serious and potentially life-threatening complication. Study results on postoperative seroma formation and reoperation rates were inconsistent. However, any conclusions drawn from these results require caution, given the following considerations.
With only two exceptions, one RCT and one meta-analysis, all studies followed an observational study design, mainly involving historical cohorts or historical controls. In most studies, this type of patient selection led to substantial differences in the participants’ baseline characteristics between intervention groups, such as age, BMI, hernia size, and recurrent hernia repair. As laparoscopically operated patients seemed to represent a more-complex case mix in most studies, this could confound study results considerably, possibly favoring the results of conventional surgical techniques. Marked differences also occurred concerning the length of follow-up, mainly resulting in shorter follow-up durations for laparoscopically treated patients and thereby probably resulting in lower recurrence rates of participants undergoing laparoscopic repair. None of the observational studies adjusted for these differences, thereby compromising validity and complicating interpretation.
Similarly, the only RCT is of fair quality, limited by small case numbers, missing information on allocation procedure, outcome assessment, follow-up rates and on participants’ BMI or overweight status. Overall, the internal validity of included studies is relatively poor, limiting the ability to draw reliable conclusions from these studies.
While there are considerable limitations associated with the identified studies, there is currently no better evidence available when comparing these two operative procedures in terms of their medical effectiveness and safety. Pham et al. [20] and Cassar and Munro [8] performed previous health technology assessments and reviews addressing related research questions. While including not all available studies, they reached similar conclusions.
Although the evidence provided by the included studies is weak, this review supports the concepts of incisional hernia repair. For instance, the minimally invasive procedure’s association with improved recovery and less postoperative pain, decreased infection rates, and postoperative ileus due to less-extensive traumatization. Similarly, there have been concerns of higher unrecognized enterotomy rates associated with laparoscopy, which found some confirmation in this review [13]. On the other hand an increase in seroma formation associated with laparoscopic surgery could not be found but has frequently been mentioned in previous reports concerned with incisional hernia repair [13].
Recurrence rate is usually considered to be the major outcome of interest in incisional hernia repair [7, 10]. This review identified similar recurrence rates for both procedures, at best indicating a trend toward superiority of laparoscopic surgery. These results are consistent with previous and more-recent reports indicating similar or slightly reduced recurrence rates associated with laparoscopic surgery [8, 33–36]. While some studies included in this review reported considerably higher rates, this could be due to several reasons. Firstly, the identified studies are partly outdated and do not reflect currently recommended best practice for hernia repair. Secondly, some of the studies performed open procedures but only in selected participants using the mesh approach or used techniques such as inlay or overlay mesh implantation that are known to result in higher recurrence rates compared to the retromuscular sublay technique [3, 4, 27, 37, 38]. Thirdly, recurrence rates increase with the length of follow-up [7]. Long follow-up [23] or differences in length of follow-up could thereby explain the considerable differences in recurrence rates between laparoscopic and conventional surgery in some of the studies. Both Klinge et al. [7] and LeBlanc et al. [10] recently reported overviews of open and laparoscopic repair, respectively, including studies in their report with recurrence rates higher than 10%. This indicates the heterogeneity in outcome following incisional hernia repair, depending on many patient- and procedure-related issues. In addition to substantial differences in the baseline characteristics within and between the included studies, the surgeons’ experience is of particular importance when comparing recurrence rates of these two operative procedures. However, many studies did not give any information in this regard.
The majority of studies identified in this review performed open surgery, using the retromuscular sublay technique and none of the studies performed a priori comparisons of different techniques of mesh implantation. While it was therefore not possible to compare different techniques of mesh implantation, use of the sublay technique currently reflects the standard of care in most cases [7, 11, 39]. Although there is no trial report available comparing different techniques, these recommendations are the result of very high recurrence rates associated with the inlay technique and reports of recurrences lifting up the mesh as well as higher infection rates associated with the onlay technique [7, 12, 13, 40, 41]. This review tried to address another controversial question in current incisional hernia repair. Namely the topic of mesh fixation in laparoscopic hernia repair. However, only the study by van´t Riet et al. [42] reported results on different techniques of mesh-fixation in laparoscopic surgery. In a small subsample of patients (n = 6) mesh fixation with suture and tacks produced no recurrences, while in the remaining 16 patients with clip fixation only three (19%) recurrences occurred. Small case numbers as well as the lack of information on any relevant patient characteristics and confounders prohibits any conclusions being drawn from these observations. Similarly, there is no evidence from prospective trials comparing different techniques of mesh fixation in laparoscopic incisional hernia repair [10]. LeBlanc et al. found that the majority of authors tend to use a combination of metal tacks and transfascial sutures in the fixation of the alloplastic mesh to ensure low recurrence rates. In view of limited evidence, however, they too consider a prospective trial necessary to answer this controversial question [10].
Despite the attempt to conduct a comprehensive and systematic search strategy to gather all available scientific knowledge, the lack of prospective high-quality studies remains the major limitation of this systematic review. While this greatly decreases the ability to answer specified research questions, it must be regarded as a general lack of appropriate studies. Additionally, publication bias as an important source of bias in systematic reviews cannot be entirely excluded. However, we attempted to identify further relevant investigations by contacting the appropriate surgical associations. This attempt did not lead to any additional results and thereby provides some indication that the comprehensive search strategy used in this study successfully identified relevant studies.
For reasons related to the contractor of this systematic review, the German Institute of Medical Documentation and Information, the search strategy dated back to August 2005. We therefore performed an update of this search using Medline until November 2006, to identify more-recent publications. Three further studies meeting the original inclusion criteria could thereby be retrieved [33, 43, 44]. Similar to the majority of studies, all of these followed an observational study design and had similar methodological limitations to those described previously. While their level of evidence has to be rated as moderate to low, they reported results in accordance with findings of this review. Namely indicating reduced length of hospital stay, postoperative pain, complication rates, and an increase in operative time associated with laparoscopic surgery. The only study reporting recurrence rates found a trend favuring laparoscopy but no statistical significant difference [33].
In conclusion this systematic review illustrates a substantial lack of high-quality studies comparing conventional and laparoscopic procedures for incisional and ventral hernia repair. It thereby confirms the urgent need for prospective and carefully designed trials investigating this topic. In this view, the results of a currently ongoing RCT investigating these two procedures are of major interest to answer controversial questions relating to incisional hernia repair.
Despite the lack of high-quality comparative studies, the present review confirms positive outcomes associated with both mesh approaches and provides evidence for the efficacy and safety of both techniques.
While study results of comparisons of both techniques are difficult to interpret, laparoscopic incisional hernia repair seems to be at least as efficacious and safe as conventional incisional hernia repair. The results also indicate some advantages associated with laparoscopic incisional hernia repair, regarding length of hospital stay, postoperative pain, wound infection rates and postoperative ileus. These results, however, require confirmation by high-quality randomized controlled trials. In the case of nonrandomized studies adjustment for possible confounders is essential to increase the validity of these studies.
References
Statistisches Bundesamt. Gesundheitsberichterstattung des Bundes 2003
Hoer J, Lawong G, Klinge U, Schumpelick V (2002) Factors influencing the development of incisional hernia. A retrospective study of 2,983 laparotomy patients over a period of 10 years. Chirurg 73(5):474–480
Ramshaw BJ, Esartia P, Schwab J, Mason EM, Wilson RA, Duncan TD, Miller J, Lucas GW, Promes J (1999) Comparison of laparoscopic and open ventral herniorrhaphy. Am Surg 65(9):827–831
Gonzalez R, Rehnke RD, Ramaswamy A, Smith CD, Clarke JM, Ramshaw BJ (2005) Components separation technique and laparoscopic approach: a review of two evolving strategies for ventral hernia repair. Am Surg 71(7):598–605
Mudge M, Hughes LE (1985) Incisional hernia: a 10 year prospective study of incidence and attitudes. Br J Surg 72(1):70–1
Schumpelick V, Arlt G, Klinge (1997) Hernienchirurgie: Versorgung von Nabelhernie und Narbenhernie. Deutsches Ärzteblatt 22;94(51–52)
Klinge U, Conze J, Krones CJ, Schumpelick V (2005) Incisional hernia: open techniques. World J Surg 29(8):1066–1072
Cassar K, Munro A (2002) Surgical treatment of incisional hernia. Br J Surg 89(5):534–545
van der Linden FT, van Vroonhoven TJ (1988) Long-term results after surgical correction of incisional hernia. Neth J Surg 40(5):127–129
LeBlanc KA (2005) Incisional hernia repair: laparoscopic techniques. World J Surg 29(8):1073–1079
Schumpelick V, Junge K, Rosch R, Klinge U, Stumpf M (2002) Retromuscular mesh repair for ventral incision hernia in Germany. Chirurg 73(9):888–894
Schumpelick V (2000) Hernien, 4th ed. Georg Thieme Verlag Stuttgart-New York
Millikan KW (2003) Incisional hernia repair. Surg Clin North Am 83(5):1223–1234
Millikan KW, Baptista M, Amin B, Deziel DJ, Doolas A (2003) Intraperitoneal underlay ventral hernia repair utilizing bilayer expanded polytetrafluoroethylene and polypropylene mesh. Am Surg 69(4):287–291
Kingsnorth AN (2004) A clinical classification for patients with inguinal hernia. Hernia 8(3):283–284
Goodney PP, Birkmeyer CM, Birkmeyer JD (2002) Short-term outcomes of laparoscopic and open ventral hernia repair: a meta-analysis. Arch Surg 137(10):1161–1165
Wright BE, Niskanen BD, Peterson DJ, Ney AL, Odland MD, VanCamp J, Zera RT, Rodriguez JL (2002) Laparoscopic ventral hernia repair: are there comparative advantages over traditional methods of repair? Am Surg 68(3):291–295
Rosch R (2003) Welche Anforderungen sollte ein ideales Netz erfüllen? Chir Gastroenterol 19(2):7–11
Harbour R, Miller J (2001) A new system for grading recommendations in evidence based guidelines. BMJ 323(7308):334–336
Pham CT, et al. (2004) Laparoscopic Ventral Hernia Repair. An Accelerated Systematic Review. ASERNIP-S Report No.41 Adelaide South Australia, ASERNIP-S 34. The Royal Australian College of Surgeons
Robbins SB, Pofahl WE, Gonzalez RP (2001) Laparoscopic ventral hernia repair reduces wound complications. Am Surg 67(9):896–900
Bencini L, Sanchez LJ, Boffi B, Farsi M, Scatizzi M, Moretti R (2003) Incisional hernia: repair retrospective comparison of laparoscopic and open techniques. Surg Endosc 17(10):1546–1551
Park A, Birch DW, Lovrics P (1998) Laparoscopic and open incisional hernia repair: a comparison study. Surgery 124(4):816–821
Carbajo MA, Martin del Olmo JC, Blanco JI, de la Cuesta C, Toledano M, Martin F, Vaquero C, Inglada L (1999) Laparoscopic treatment vs open surgery in the solution of major incisional and abdominal wall hernias with mesh. Surg Endosc 13(3):250–252
DeMaria EJ, Moss JM, Sugerman HJ (2000) Laparoscopic intraperitoneal polytetrafluoroethylene (PTFE) prosthetic patch repair of ventral hernia. Prospective comparison to open prefascial polypropylene mesh repair. Surg Endosc 14(4):326–329
Zanghi A, Di Vita M, Lomenzo E, De Luca A, Cappellani A (2000) Laparoscopic repair vs open surgery for incisional hernias: a comparison study. Ann Ital Chir 71(6):663–667
McGreevy JM, Goodney PP, Birkmeyer CM, Finlayson SR, Laycock WS, Birkmeyer JD (2003) A prospective study comparing the complication rates between laparoscopic and open ventral hernia repairs. Surg Endosc 17(11):1778–1780
Chari R, Chari V, Eisenstat M, Chung R (2000) A case controlled study of laparoscopic incisional hernia repair. Surg Endosc 14(2):117–119
Olmi S, Magnone S, Erba L, Bertolini A, Croce E (2005) Results of laparoscopic versus open abdominal and incisional hernia repair. JSLS 9(2):189–195
Anthony T, Bergen PC, Kim LT, Henderson M, Fahey T, Rege RV, Turnage RH (2000) Factors affecting recurrence following incisional herniorrhaphy. World J Surg 24(1):95–100
George CD, Ellis H (1986) The results of incisional hernia repair: a twelve year review. Ann R Coll Surg Engl 68(4):185–187
Luijendijk RW, Hop WC, van den Tol MP, de Lange D, Braaksma MM, IJzermans JN, Boelhouwer RU, de Vries BC, Salu MK, Wereldsma JC, et al. (2000) A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med 10;343(6):392–398
Lomanto D, Iyer SG, Shabbir A, Cheah WK (2006) Laparoscopic versus open ventral hernia mesh repair: a prospective study. Surg Endosc 20(7):1030–1035
Chowbey PK, Sharma A, Khullar R, Mann V, Baijal M, Vashistha A (2000) Laparoscopic ventral hernia repair. J Laparoendosc Adv Surg Tech A 10(2):79–84
Franklin ME, Dorman JP, Glass JL, Balli JE, Gonzalez JJ (1998) Laparoscopic ventral and incisional hernia repair. Surg Laparosc Endosc 8(4):294–299
Koehler RH, Voeller G (1999) Recurrences in laparoscopic incisional hernia repairs: a personal series and review of the literature. JSLS 3(4):293–304
Holzman MD, Purut CM, Reintgen K, Eubanks S, Pappas TN (1997) Laparoscopic ventral and incisional hernioplasty. Surg Endosc 11(1):32–35
Olmi S, Magnone S, Erba L, Bertolini A, Croce E (2005) Results of laparoscopic versus open abdominal and incisional hernia repair. JSLS 9(2):189–195
Klinge U, Klosterhalfen B, Conze J, Limberg W, Obolenski B, Ottinger AP, Schumpelick V (1998) Modified mesh for hernia repair that is adapted to the physiology of the abdominal wall. Eur J Surg 164(12):951–960
Machairas A, Misiakos EP, Liakakos T, Karatzas G (2004) Incisional hernioplasty with extraperitoneal onlay polyester mesh. Am Surg 70(8):726–729
Schumpelick V (1996) Hernien, 3rd ed. Ferdinand Enke Verlag Stuttgart
van’t RM, Vrijland WW, Lange JF, Hop WC, Jeekel J, Bonjer HJ (2002) Mesh repair of incisional hernia: comparison of laparoscopic and open repair. Eur J Surg 168(12):684–689
Beldi G, Ipaktchi R, Wagner M, Gloor B, Candinas D (2006) Laparoscopic ventral hernia repair is safe and cost effective. Surg Endosc 20(1):92–95
Earle D, Seymour N, Fellinger E, Perez A (2006) Laparoscopic versus open incisional hernia repair: a single-institution analysis of hospital resource utilization for 884 consecutive cases. Surg Endosc 20(1):71–75
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Müller-Riemenschneider, F., Roll, S., Friedrich, M. et al. Medical effectiveness and safety of conventional compared to laparoscopic incisional hernia repair: A systematic review. Surg Endosc 21, 2127–2136 (2007). https://doi.org/10.1007/s00464-007-9513-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-007-9513-4