Abstract
Background
The incidence of Zenker’s diverticulum is low (2/100,000). Standard surgical treatment is cricopharyngeal myotomy with diverticulectomy. Various minimally invasive surgical approaches pursued recently have treated Zenker’s diverticulum adequately. The functional minimally invasive therapy is performed alternatively using an Endo-Gia stapler inserted transorally to perform an esophageal diverticulostomia, or using thermal coagulation applied by a carbon dioxide (CO2) or argon plasma laser. The key to a successful procedure is adequate exposure of the diverticulum by insertion of a pharynx spreader before the surgery.
Methods
Since 1996, 31 patients who underwent minimally invasive diverticulostomies performed in our clinic have been included prospectively in the current study. All the patients were examined endoscopically before and after surgery. Furthermore, the intraesophageal and intragastric pressure was examined by transesophageal manometry, and the pH in the esophagus and stomach was determined by pH-metry. A barium swallow was performed to exclude leakage at the stapler suture line as proof of sufficient anastomoses. Manometry showed that the upper esophageal sphincter functioned normally before and after surgery. The results were compared with those of patients undergoing conventional procedures.
Results
The median follow-up period after resection of the diverticulum was 46 months. Both the Gastrointestinal Quality-of-Life Index (GQLI) (p < 0.001) and the modified dysphagia score (GHDS) increased significantly, indicating that the operations were successful. The minimally invasive procedure is faster than cricopharyngeal myotomy and significantly safer. It is better tolerated by patients, and they are discharged earlier.
Conclusion
Transoral esophagodiverticulosomy has become the standard procedure for Zenker’s diverticulum in the authors’ department. The endoscopic minimally invasive approach proved to be safer than standard surgical procedures. It offers a significantly shorter operation time and postoperative hospital stay (p < 0.001).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Zenker’s diverticulum, first observed by Ludlow in 1769 [11], became widely known after it was described in a surgical book by Zenker and von Ziemssen [24] in 1878. The anatomy of the Zenker’s diverticulum was precisely described by Kilian in 1908.
Diverticula develop in the Kilian triangle and occur twice as often in men than in women approximately 40 years of age. The symptoms are increased dysphagia and a globus sensation in the throat combined with foetor ex ore and regurgitation of undigested food. The diagnosis is based on radiography of the esophagus and endoscopy.
The standard surgical procedure for Zenker’s diverticulum is the resection of the diverticulum through an incision on the left side of the neck combined with myotomy of the musculus cricopharyngeus. This surgical approach was first described by Mosher [13] in 1917. The first alternative approaches using minimal surgery were published in 1960 by Dohlman and Matisson [6], who applied diathermia to treat the diverticulum. In 1984, Overbeek et al. [16] endoscopically treated Zenker’s diverticulum with lasers. In 1993, Collard performed the first esophagodiverticulostomy using an endoscopic stapler [3]. The treatment is based on a functional resection of the diverticulum by anastomosis of the esophagus and the diverticulum wall using an Endo-Gia stapler inserted transorally. We summarize our long-term experience with therapy of Zenker’s diverticulum using a modified multifire Endo-Gia linear stapler (Tyco Health Care, Neustadt an der Donau, Germany) (Fig. 3) in combination with the Kastenbauer–Wollenberg spreader (developed by Professors Kastenbauer and Wollenberg, Munich, Germany, Fig. 1).
Materials and methods
From 1996 to 2005, we included 31 patients (24 men and 7 women, ages 68 ± 10 years) with a symptomatic Zenker’s diverticulum in a prospective trial to evaluate the safety and long-term results for esophagodiverticulostomy using a modified Endo-Gia stapler (Tyco Healthcare). Before and after the planned procedure, we performed an esophagogastroduodenoscopy, a gastrografin radiography of the esophagus, and a stationary manometry.
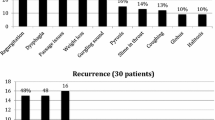
Each patient was evaluated by the Gastrointestinal Quality-of-Life Index (GQLI) according to Eypasch et al. [8], and a dysphagia score (GHDS) was determined on the basis of the following parameters (Table 3): dysphagia, odynophagia, foetor ex ore, regurgitation, awakening at night, cough, and vomiting. These symptoms were ranked according to their frequency as follows: 4 (always), 3 (more than once weekly), 2 (less than once weekly), 1 (less than once monthly), or 0 (no symptoms). All the patients were questioned about their subjective comfort, which was ranked according to a “smiley score” by the patient using the following choices: 1 (very good), 2 (good), 3 (satisfactory), 4 (bad), or 5 (very bad).
Intra- and postoperative complications as well as adverse events during the follow-up period after the operation and the length of hospital stay were evaluated. The intraoperative course, operation time, and length of hospital stay were compared with those for a group of 32 patients (24 men and 8 women, ages 65 ± 11 years) treated with standard operation procedures between January 1992 and December 2004. Before the operation, the patients were informed about the different surgical techniques and treated with surgery according to their choice.
Surgical technique
All the patients were intubated transorally and positioned on the back with a reclined throat. To enable insertion and positioning of the modified Endo-Gia, the oropharynx and the entrance to the diverticulum were exposed by insertion of the Kastenbauer–Wollenberg spreader in collaboration with our Head–Neck–Ear Department. As compared with a conventional spreader, which opens in a duck beak manner two-dimensionally, the Kastenbauer–Wollenberg spreader enables the spreading of height and width at the same time (Fig. 1). One arm of the spreader is positioned in the esophagus, and the other is positioned at the entrance of the diverticulum (Fig. 2).
The Endo-Gia stapler is modified as shown in Fig. 3. The anvil is shortened on an abrasive belt as close as 1 mm to the metal clips by a medical technician. This is performed at low speed to avoid plastic deformation of the material attributable to extensive heat. Burrs are removed, and the stapler is resterilized. The tip of the anvil is shortened to allow the cutting and stapling line to reach as close as possible to the bottom of the diverticulum (Fig. 3). This results in a complete disruption of the tissue between the diverticlum and the esophagus.
The Endo-Gia stapler is inserted into the esophagus such that the short end is introduced into the diverticulum and the stapler branch with the magazine is positioned in the esophagus (Fig. 4). In the case of a large diverticulum, more than one stapler magazine can be applied to ensure a complete esophagodiverticulostomy. If the incision of the esophagodiverticulostomy is not completely to the bottom of the diverticulum, the incision is lengthened with a microtome up to an additional 2 mm. During the operation, the length of the staple suture is measured.
Results
A total of 31 planned minimally invasive diverticulostomies were performed successfully. One conversion to a conventional cricomyotomy with resection of the diverticulum had to be performed because 2 cm of the esophagus had been dissected during insertion of the Kastenbauer–Wollenberg spreader. The operation was successful, and the patient recovered without further complications (Table 1).
The median operation time was 35 min (range, 15–115 min). The median operation time was significantly shorter (35 vs 80 min; p < 0.001) than for the patients in the open surgery group (n = 32, Table 5). The longest operation time (115 min) was caused by a difficulty placing the Kastenbauer–Wollenberg spreader in the diverticulum because of a difficult esophageal anatomy. The median stapler suture length was 3.5 cm, and the maximum length was 7.5 cm (Table 2).
All the transoral minimally invasive procedures were performed without measurable blood loss. In one patient, visible bleeding from the suture line was treated successfully with a 5-mm metal clip (Fig. 5). In one patient, a prosthesis broke due to the insertion of the Kastenbauer–Wollerberg spreader. In six patients, a 1- to 3-mm-long dissection at the aboral end of the esophagodiverticulostomy occurred. All of these patients were treated successfully with fibrin glue applied endoscopically (Table 1). All the treated patients recovered without further complications and remained relapse free after the minimally invasive procedure.
Patients who did not experience any complications were fed with tea in the evening and a normal diet from postoperative day 2. All six patients with dissection of the esophagodiverticulostomy were fed with tea on postoperative day 1, light food on postoperative day 2, and a normal diet on postoperative day 3. The median postoperative hospital length of stay was 4 days for the 24 patients without complications and 10.5 days for the patients who experienced dissections. The overall hospital length of stay was 5 days (Table 2). The median postoperative stay (5 vs 10 days; p < 0,001, Table 5) was significantly shorter than for the 32 patients who underwent standard operation procedures between January 1992 and December 2004.
The median follow-up time for 30 (97%) of the 31 patients was 46 months. One patient who experienced relapse symptoms of dysphagia because of an insufficient esophagodiverticulostomy was treated successfully by minimally invasive surgery 22 months after his first procedure.
One patient who experienced a relapse decided to undergo open resection of the diverticulum and a cricomyotomy. One of the patients had to undergo reoperation with transoral minimally invasive surgery due to incomplete dissection of the diverticulum. Both of these patients remained relapse free after the second operation. Of the patients who had a control gastroscopy, 28 did not show any signs of a relapse. In some of the patients, staples of the esophagodiverticulotomy could be detected endoscopically or by radiography. In none of these patients did the gastrografin swallow detect any residuum of the diverticulum in the proximal esophagus.
The majority of the patients who experienced symptoms such as dysphagia, odynophagia, foetor ex ore, regurgitation, or awakening at night because of reflux had significantly fewer symptoms after the surgery (Table 3). Most of the patients were free of any symptoms after surgical therapy. This is documented by the significant increase in their GQLI after therapy as well as the significant increase in their subjective comfort, as measured by the smiley score (p < 0.001) (Table 4).
Discussion
In 1998, the National Confidential Enquiry Into Perioperative Deaths (NCEPOD 1998, London) in head and neck surgery concluded that endoscopic procedures used to manage Zenker’s diverticulum are safer, faster, and less invasive than conventional surgical approaches, causing less comorbidity [19]. We show that the minimally invasive stapler esophagodiverticulostomy using a modified Endo-Gia stapler is safer than a diverticulosomy performed with other techniques. We found a morbidity rate of 2.6% in our patient cohort, as compared with 7.4% in the literature for patients treated with a carbon dioxide (CO2) laser, 8.1% for patients treated with electrocauter, and 11.8% for patients treated with conventional open surgery.
The better outcome probably is attributable to a complete staple suture, which reduces the risk for perforation of the esophagus and thus reduces the risk for mediastinitis. Although we observed small dissections of the esophagus in 6 of 31 patients after stapler esophagodiverticulostomy, we were able to treat the dissection endoscopically with fibrin glue successfully. Most important for a successful minimally invasive intervention is complete exposure of the diverticulum lumen by insertion of the Kastenbauer–Wollenberg spreader. This exposes the hypopharynx in width and height at the same time.
In our cohort of patients, a normal diet was achieved within 3 days (median), and the mean hospital length of stay was 6 days. With the conventional surgical treatment of Zenker’s diverticulum, the mean hospital length of stay is 7 days (range, 4–11 days), and the time until a normal diet is achieved varies between 4 and 9 days [2, 7, 10, 15, 21, 23]. Our results agree with those of other studies reporting 0.6 to 4 days as the mean hospital length of stay and 0.1 to 3 days for recovery of a normal diet among patients treated with endoscopic diverticulostomy [1, 4, 7, 9, 14, 17, 18, 21, 22].
The relapse rates for patients treated with conventional diverticulectomy and cricomyotomy vary from 0% to 19% (mean, 6.8%) during median follow-up times of 36 months [2, 5, 12, 20, 23]. In contrast, the relapse rates for patients treated with minimally invasive esophagodiverticulostomies in studies that have median follow-up times of 16 months vary between 0% and 9% (mean, 3.6%) [1, 17, 14, 22].
These results are in contrast to those reported by Counter et al. [4], who investigated the long-term results 61 months after surgery for patients treated with minimally invasive diverticulostomies. These authors reported relapse rates of 22%. In contrast to our surgical approach, these authors used conventional, nonmodified stapler tips for the surgery.
We found recurring diverticula in 6.5% of our patients (n = 2) treated with the modified Endo-Gia stapler. We hypothesize that this favorable result is attributable to the shortened anvil of the applied Endo-Gia, which allows the complete lumen of the diverticulum to be dissected to the base. In case of a diverticulum relapse, these patients could successfully be resubmitted to a transoral reesophagodiverticulostomy with an Endo-Gia stapler.
To our knowledge, the transorally performed diverticulostomy with the modified Endo-Gia stapler is the safest surgical procedure for the treatment of Zenker’s diverticulum. In contrast to the conventional surgical procedure and other minimally invasive surgical approaches such as diathermia and use of a CO2 laser, diverticulostomy with the Endo-Gia stapler leads to fewer postoperative complications, fewer relapses, and a shortened hospital length of stay. Therefore, it is thus superior to the other approaches.
Our results, as compared with others, presumably arise from modification of the Endo-Gia stapler anvil, which allows a deeper, more complete anastomosis of the diverticulum and the esophageal lumen.
References
Burstin PP, Merry D (1998) Endoscopic stapling treatment of pharyngeal pouch. Aust N Z J Surg 68: 532–535
Cerdan FO, Gonzalez EM, Garcia DH (1998) Diagnostic and treatment of Zenker’s diverticulum: review of our series pharyngoesophageal diverticula. Hepatogastroenterology 45: 447–450
Collard JM, Otte JB, Kestens PJ (1993) Endoscopic stapling technique of esophagodiverticulostomy for Zenker’s diverticulum. Ann Thorac Surg 56: 573–576
Counter P, Hilton M, Baldwin DL (2002) Long-term follow-up of endoscopic stapled diverticulotomy. Ann R Coll Surg Engl 84: 89–92
Crescenzo D, Trastek V, Allen M, Deschamps C, Pairolero P (1998) Zenker’s diverticulum in the elderly: is operation justified? Ann Thorac Surg 66: 347–350
Dohlmann G, Matisson O (1960) The endoscopic operation for hypopharyngeal diverticula: a roentgencinematographic study. Arch Otolaryngol 71: 744–752
van Eeden S, Lloyd RV, Tranter RM (1999) Comparison of the endoscopic stapling technique with more established procedures for pharyngeal pouches: results and patient satisfaction survey. J Laryngol Otol 113: 237–240
Eypasch E, Williams JI, Wood-Dauphinee S, Ure BM, Schmulling C, Neugebauer E, Troidl H (1995) Gastrointestinal Quality-of-Life Index: development, validation, and application of a new instrument. Br J Surg. 82: 216–222
Jaramillo MJ, McLay KA, McAteer D (2001) Long-term clinicoradiological assessment of endoscopic stapling of pharyngeal pouch: a series of cases. J Laryngol Otol 115: 462–466
Laccourreye O, Menard M, Cauchois R, Huart J, Jouffre V, Brasnu D, Laccourreye H (1994) Esophageal diverticulum: diverticulopexy versus diverticulectomy. Laryngoscope 104: 889–892
Ludlow A (1769) A case of obstructed deglutition from a preternatural dilatation of and bag formed in the pharynx. Med Observations Inquiries 3: 85–101
Morton R, Bartley J (1993) Inversion of Zenker’s diverticulum: the preferred option. Head Neck 15: 253–256
Mosher HP (1917) Webs and pouches of the esophagus: their diagnosis and treatment. Surg Gynecol Obstet 25: 175–187
Narne S, Cutrone C, Bonavina L, Chella B, Peracchia A (1999) Endoscopic diverticulotomy for the treatment of Zenker’s diverticulum: results in 102 patients with staple-assisted endoscopy. Ann Otol Rhinol Laryngol 108: 810–815
Nguyen H, Urquhart A (1997) Zenker’s diverticulum. Laryngoscope 107: 1436–1440
Overbeek van JJ, Hoeksema PE, Edens ET (1984) Microendoscopicsurgery of the hypopharyngeal diverticulum using electrocoagulation or carbon dioxide laser. Ann Otol Rhinol Laryngol 93: 34–36
Peracchia A, Bonavina L, Narne S, Segalin A, Antoniazzi L, Marotta G (1998) Minimally invasive surgery for Zenker’s diverticulum: analysis of results in 95 consecutive patients. Arch Surg 133: 695–700
Philippsen LP, Weisberger EC, Whiteman TS, Schmidt JL (2000) Endoscopic stapled diverticulotomy: treatment of choice for Zenker’s diverticulum. Laryngoscope 110: 1283–1286
Resouly A (1998) Pharyngeal Pouch Surgery Section Location 3.2. The Report of the National Confidential Enquiry Into Perioperative Deaths: 1996/7 Report London, NCEPOD
Schmit PJ, Zuckerbraun L (1992) Treatment of Zenker’s diverticulum by cricopharyngeus myotomy under local anesthesia. Am Surg 58: 710–716
Smith SR, Genden EM, Urken ML (2002) Endoscopic stapling technique for the treatment of Zenker diverticulum vs standard open-neck technique: a direct comparison and charge analysis. Arch Otolaryngol Head Neck Surg 128: 141–144
Sood S, Newbegin CJ (2000) Endoscopic stapling of pharyngeal pouches in patients from the Yorkshire region. J Laryngol Otol 114: 853–837
Zbaren P, Schar P, Tschopp L, Becker M, Hausler R (1999) Surgical treatment of Zenker’s diverticulum: transcutaneous diverticulectomy versus microendoscopic myotomy of the cricopharyngeal muscle with CO2 laser. Otolaryngol Head Neck Surg 121: 482–487
Zenker FA, von Ziemssen H (1878) Dilatations of the esophagus. Cyclopedia Pract Med 3: 46–48
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00464-007-9466-7
Rights and permissions
About this article
Cite this article
Lang, R.A., Spelsberg, F.W., Winter, H. et al. Transoral diverticulostomy with a modified Endo-Gia stapler: results after 4 years of experience. Surg Endosc 21, 532–536 (2007). https://doi.org/10.1007/s00464-006-9036-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-006-9036-4