Abstract
The treatment of Zenker diverticulum has faced a substantial evolution during the last century. The traditional open surgical approach has been progressively flanked and subsequently almost completely overcome by the less invasive and easier transoral approach.
Transoral stapling of the septum between the diverticulum and the esophagus and laser diverticulotomy has gained consensus, being minimally invasive, relatively inexpensive, and associated with very few complications. However, they require the placement of a rigid diverticuloscope and general anesthesia. The placement of the diverticuloscope is not possible in all the patients and especially in the elderly.
Since its introduction in 1995, flexible endoscope-assisted cricopharyngeal myotomy quickly became one of the first-line treatments for the Zenker diverticulum. The procedure is performed by using a 9-mm endoscope, under sedation. Age of patients, previous treatments, and impossibility to hyperextend the neck are no longer limits for the transoral treatment. The outcomes of the procedure are excellent. The advent of peroral endoscopic myotomy additionally expanded the therapeutic possibilities, with promising results also in the treatment of the smallest pouches.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Zenker diverticulum
- Cricopharyngeal myotomy
- Dysphagia
- Endoscopy
- Peroral endoscopic myotomy
- Septotomy
- Esophagus
- Deglutition disorders
9.1 Introduction, Etiology, Epidemiology, and Pathophysiology
Zenker diverticulum is a hypopharyngeal, acquired, pulsion, false diverticulum that develops in an area of weakness of the posterior hypopharynx known as the Killian triangle. Killian triangle is located in the hypopharynx and delimited by two very strong pharyngoesophageal muscles, the horizontal fibers of the cricopharyngeal muscle and the oblique fibers of the inferior pharyngeal constrictor.
Zenker diverticulum was first recognized and described in the second half of the eighteenth century by the British pathologist Abraham Ludlow. After an autopsy performed on a 50-year-old male patient who regurgitated undigested food and died after an episode of “obstructed deglutition,” Ludlow observed the abnormality of “pharyngeal preternatural bag, wide sac reaching down into thorax.” Ludlow eventually published the observation in 1767 after presenting it to the Royal Society of Physicians where he described it as an esophageal hypopharyngeal diverticulum [1].
However, only in 1874 the German physicians and pathologists Friedrich Albert von Zenker and Hugo Wilhelm von Ziemssen made a more detailed and precise description and hypothesized a possible etiopathogenesis. Since then, the name of Zenker is chiefly associated with the pulsion diverticula of the hypopharynx [1].
Zenker diverticulum is different from other diverticula of the upper part of the esophagus and especially from the Killian-Jamieson diverticulum, an outpouching of the lateral pharyngoesophageal wall. This pulsion-type diverticulum protrudes through a muscular gap in the anterolateral wall of the cervical esophagus distal to the cricopharyngeal muscle, named the Killian-Jamieson space [2].
The pathophysiology of the Zenker diverticulum has not yet been completely understood. However, it is generally accepted that the significant increase of the intrapharyngeal pressure and the consequent protrusion of the mucosa through a locus minoris resistentiae (the Killian dehiscence) is caused by an inadequate relaxation of the cricopharyngeal muscle (and subsequent incomplete opening of the upper esophageal sphincter) during the swallow-induced contraction of the lower pharyngeal constrictor muscle. The cause of this swallowing disorder and miscoordination is largely unknown.
Achalasia or cricopharyngeal spasms, cricopharyngeal incoordination, and congenital weakness have been implicated [3, 4].
Gastroesophageal reflux may lead to esophageal and cricopharyngeal spasm and may have a role in Zenker diverticulum creation. Gastroesophageal reflux would induce a dyskinetic-hyperkinetic reaction that can involve the upper esophageal sphincter and the cricopharyngeal muscle. Furthermore, gastroesophageal reflux has been observed in up to two thirds of the patients with Zenker diverticulum [5].
Zenker diverticula most commonly present in middle-aged and elderly individuals: diverticula are extremely rare under the age of 40 [6], but more frequent during the seventh and eighth decades of life, with a 1.5-fold male predominance [7].
There is a certain geographical variation in the prevalence of Zenker diverticulum, being higher in Northern than in Southern Europe and higher in the United States, Canada, and Australia than in Indonesia and Japan [6, 8].
Even if the real prevalence of the disease is unknown, because many patients with diverticula remain asymptomatic, it is estimated that the prevalence among the general population is between 0.01% and 0.11% [8].
As development of cricopharyngeal motility disorders and Zenker diverticulum is directly related to aging, the prevalence of Zenker diverticulum is expected to increase due to the increased aging of population [7].
9.2 Symptoms, Clinical History, and Diagnosis
Progressively worsening oropharyngeal dysphagia, both for solids and liquids, is the predominant symptom associated with Zenker diverticulum. Even if small diverticula can be occasionally responsible for very severe symptoms, because the incomplete relaxation of the cricopharyngeal muscle may lead to severe outflow obstruction, usually the worst clinical presentations are in patients with large diverticula. In patients with large diverticula, both the non-relaxing cricopharyngeal muscle and the extrinsic compression from the enlarged and fulfilled pouch itself are likely to explain the dysphagia experienced by patients [7, 9].
In these cases, patients may experience a kind of “delayed” dysphagia. Swallowing of solids is relatively normal at the very beginning of meal, and dysphagia almost abruptly occurs with the third or fourth bite. At this time drinking can worsen the situation. This phenomenon has a logical explanation. During the first bites, part of the ingested food easily enters into the pharyngeal pouch and the patient has no critical symptoms. However, when the diverticulum, that is comprised and wedged between the spine and the upper esophagus, is filled with food, it compresses and restricts the upper esophagus, until dysphagia becomes critical and complete. This presentation is usually pathognomonic of the Zenker diverticulum.
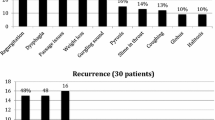
Regurgitation of undigested food is a very frequent symptom and it is due to bolus entrapment in the pharyngeal pouch. In many cases, especially in the case of large diverticula, regurgitation occurs hours after ingestion (rumination) (Table 9.1).
Pharyngeal stasis of secretions, chronic cough, sensation of a lump in the throat, chronic aspiration, halitosis, and hoarseness are also very common symptoms caused by a pharyngeal pouch and outlet obstruction.
Whistling, crepitus, and cervical borborygmi are usually associated with very large pouches and are almost pathognomonic of Zenker diverticula [6]. With time, weight loss may occur, because of inability of patients to have a regular and adequate diet.
Sometimes, particularly in elderly patients, aspiration pneumonia can be the presenting symptom and clearly represents a fearing complication of the disease [6, 7, 10].
More rarely, diverticulitis, peptic ulceration, bleeding, tracheal fistulas, fistula to the prevertebral ligament with cervical osteomyelitis, and vocal cord paralysis may occur [11, 12].
Squamous cell carcinoma may occur in the setting of a Zenker diverticulum. It is a rare situation, with an incidence of 0.4–1.5%, and should be taken into account in the case of abrupt worsening of dysphagia or alarm symptoms including local pain hemoptysis or hematemesis [13,14,15].
In patients with oropharyngeal dysphagia and suspected Zenker diverticulum, esophagography is often the most useful and reliable diagnostic tool [16, 17]. It is minimally invasive and inexpensive and quickly permits to exclude other possible causes of dysphagia. Pharyngeal pouches are perfectly visible, especially in the lateral view, and a definitive measurement of the size of the diverticulum is possible. Dynamic continuous fluoroscopy is usually preferred to evaluate possible swallowing disorders, especially in the case of small pouches. Additionally, evidence overflows, and aspiration can be seen (Fig. 9.1).
Zenker diverticula should be differentiated from the less common and smaller Killian-Jamieson diverticula [2, 18]. In these cases, diverticula originate from the anterolateral cervical esophagus, distally to the cricopharyngeal muscle. Discrimination between the two diverticula is crucial, because endoscopic treatment is very effective, safe, and reliable for the Zenker diverticula, but much less for the Killian-Jamieson.
Not rarely, upper GI endoscopy is used for the primary evaluation of patients with dysphagia. However, when a pharyngeal diverticulum is suspected, endoscopy should be carried out cautiously, on well-sedated patients, because of a high risk of iatrogenic perforation. From a diagnostic point of view, endoscopy does not add very much to the barium esophagram. Size of the diverticulum and location are more accurately seen on X-ray than by endoscopy. However, the role of endoscopy is particularly important to evaluate patients with recurrent symptoms after transoral cricopharyngeal myotomy, because it permits to reliably evaluate the depth of the residual septum, any possible scarring, and, as a consequence, the possibility of an endoscopic retreatment.
Zenker diverticulum may also be diagnosed by transcutaneous ultrasonography [19]. Ultrasonography could be useful to differentiate the diverticulum from a thyroid nodule or a big mass [20]. However, the role of ultrasonography in the evaluation of Zenker diverticulum is limited to some specific clinical situations.
CT scan and MRI are only anecdotally used for the evaluation of a Zenker diverticulum. Usually they are performed to exclude other possible causes of esophageal dysphagia, including esophageal or pharyngeal neoplasms of mediastinal masses. In contrast, their role becomes predominant when a carcinoma is suspected.
9.3 Indication for Treatment and Aims
Treatment is usually reserved for symptomatic diverticula. Diverticula can remain asymptomatic for years, the natural history of this disease is uncertain, and the risk of operative complications is definitely higher than the risk of aspiration or cancer. This is especially true if we consider that often patients with pharyngeal pouches are particularly old and fragile, with a variety of age-related comorbidities that can additionally compromise the perioperative course.
The primary aims of treatment are to reduce the obstacle to normal pharyngeal emptying, which is essentially represented by the non-relaxing upper esophageal sphincter, and to eliminate the pharyngeal reservoir represented by the pouch.
The upper esophageal sphincter is composed of the posterior surface of the thyroid and cricoid cartilage and three muscles: inferior pharyngeal constrictor, cricopharyngeal muscle, and muscularis propria of the cervical esophagus [21]. Functionally, the cricopharyngeal muscle is the main and dominant portion of the sphincter. It is approximately 1.6–1.9 cm in length [6, 9]. Since the main pathophysiological alteration associated with the Zenker diverticulum is the incomplete swallow-induced relaxation of the cricopharyngeal muscle, a cricopharyngeal myotomy is always necessary, independently of the additional procedures that will be performed to eliminate the pharyngeal reservoir (creation of a plain esophagodiverticulostomy with a transection of the septum, diverticulectomy, or suspension diverticulopexy) [22].
Cricopharyngeal myotomy alone reduces the sphincter resting pressure and normalizes both the upper esophageal sphincter opening (relaxation) and the intrabolus pressure, as demonstrated by pharyngoesophageal manometry [9, 23,24,25,26,27].
Some experts recommend extending the myotomy for 2–3 cm into the muscularis propria of the proximal esophagus, beyond the cricopharyngeal muscle, since both these muscles appear to be involved in the pathogenesis of Zenker diverticulum [26]. However, in the case of a transoral approach, it could be associated with an increased risk of mediastinum exposure and perforation or vascular injury, especially in case of huge floating or plunging diverticula [7].
In contrast, the simple elimination of the pharyngeal reservoir and pouch, by means of a diverticulectomy, diverticulostomy, diverticulopexy, or inversion without a cricopharyngeal myotomy, is no longer an acceptable treatment given the high rate of long-term recurrence and complications [28].
Currently there are three main treatment options for Zenker diverticulum: open surgery, with a transcervical approach, transoral rigid endoscopy (including cricopharyngeal myotomy with endoscopic stapling, carbon dioxide laser, or vessel tissue sealer), and transoral flexible endoscopy (including needle knife cricopharyngeal myotomy or submucosal peroral endoscopic myotomy).
9.4 Open Transcervical Approach
The classical open transcervical surgical operations include an external neck incision, usually along the anterior border of the left sternocleidomastoid muscle, the identification, dissection, and exposition of the pharyngeal pouch and of his neck, followed by the myotomy. Myotomy is performed approximately 2 cm proximally into lower pharyngeal constrictor to 5 cm distally through the cricopharyngeal and into the proximal part of the esophagus [10].
Following myotomy, the pharyngeal pouch can be (1) surgically excised, usually with a linear stapling device (diverticulectomy), (2) uplifted and retracted toward the prevertebral fascia and suspended as by suture to the prevertebral fascia or the posterior pharyngeal wall (diverticulopexy) with the collar of the sac in a non-dependent position, or (3), finally, inverted into the esophageal lumen (diverticulum inversion or invagination) [29,30,31]. Average-sized diverticula can be treated with a combined cricopharyngeal myotomy and diverticulopexy; smaller diverticula are more frequently treated with suspension or cricopharyngeal myotomy alone [6, 32].
In a large review of more than 2800 patients from 41 studies who underwent open surgery for Zenker diverticulum, overall morbidity occurred in 10.5% of patients, with the most frequent complications being recurrent nerve injury in 3.3%, leaks or perforation in 3.3%, cervical infections in 1.8%, and hematomas in 1% of patients. Mortality after open surgery was reported in 0.6% of patients [33].
In the general trend versus less invasive approaches and therapies, new techniques and new devices have been implemented in the last decades, and transoral endoscopic treatment [34] and flexible endoscopy [27, 35] have gained in popularity over open surgery with a concurrent decrease in mortality and morbidity.
Therefore, open surgery still remains a mainstay in the management of symptomatic diverticula, but it is nowadays recommended almost exclusively for small symptomatic or huge Zenker diverticula and always in patients at low surgical risk [32].
9.5 Transoral Cricopharyngeal Myotomy: Rigid Endoscopy
The transoral approach was especially developed to overcome some limits of the open transoral approach and in particular the relatively high frequency of associated adverse events, complications, and mortality [33]. Many patients with Zenker diverticulum are elderly and with comorbidities.
The rationale behind the transoral approach is that a septum containing the cricopharyngeal muscle and the proximal part of the esophagus divides the pharyngeal pouch from the esophagus. The septum can be easily identified in the hypopharynx and divided until the bottom of the pouch. Therefore, the diverticular sac is joined to the esophagus, eliminating simultaneously the pharyngeal outlet obstruction and the pharyngeal reservoir (Fig. 9.2).
9.5.1 Endoscopic Electrocautery
The first successful endoscopic treatment of a Zenker diverticulum was reported by Moscher in 1917, but this approach was abandoned for years because of a high incidence of complications, especially mediastinal infections [33].
Lately, as early as in 1936, Gosta Dohlman performed the endoscopic cricopharyngeal myotomy on a series of patients, but published the results only many years later [36]. Dohlman described substantial key improvements to the Mosher’s method, using a bivalved rigid diverticuloscope and employing diathermic excision and hemostasis of the cricopharyngeal muscle and common wall between the esophagus and the diverticulum. In a series of 100 patients, he reported no cases of mediastinitis and a very low recurrent rate (7%). Similar outcomes were reported by other authors by using the Dohlman technique, with a complications rate of 7.8% (the most frequent adverse events being subcutaneous emphysema in 2.9% of patients and mediastinitis in 2.1%) and a mortality rate of 0.2%. Clinical success in some series was reported as high as 91–92% [33].
Since then, the endoscopic approach has evolved quickly over time , and especially in the last 30 years with the introduction of carbon dioxide laser and new surgical devices derived from the laparoscopic armamentarium.
9.5.2 Carbon Dioxide Laser Diverticulotomy
Carbon dioxide laser-aided diverticulotomy was first introduced in 1981 by Van Overbeek [37, 38]. It is a contactless and sutureless technique, where the septum between the diverticulum and esophagus is divided by using the high-energy and high-focus laser beam. The advantages over electrocautery include less tissue trauma, less postoperative pain, and quicker recovery.
The operation is performed under general anesthesia with orotracheal intubation. The patient is positioned supine, and the neck should be completely extended. A bivalved Weerda diverticuloscope in its closed position is introduced into the esophageal inlet under direct vision or better under video monitoring. The diverticuloscope is then retracted slowly and opened to expose the septum between the esophagus and diverticulum: the anterior blade of the diverticuloscope is placed inside the esophagus, the posterior blade inside the diverticular pouch. The diverticuloscope is then advanced again until the bottom of the diverticulum is completely exposed. The septum will become clearly visible between the two valves of the diverticuloscope.
An operating microscope with a 400-mm lens and attached CO2 laser micromanipulator is introduced into the diverticuloscope and focused on the common wall. The septum is transected at the midline, down to the bottom of the pharyngeal pouch. During transection, the fibers of the cricopharyngeal muscle can be clearly identified, as they retract laterally when they are cut [7].
No sutures or stitches are applied after the transection of the septum on the edges of the septum. The high-power laser energy provides less thermal tissue damage compared to electrocoagulation and favors a rapid healing of the cut surface [39, 40].
On the other hand, the procedure is strictly operator-dependent, and the risk of perforation and mediastinitis in unexperienced hands should not be underestimated.
In 2013, in a review about the surgical treatment of Zenker diverticulum [33], more than 1000 patients who underwent carbon dioxide laser procedure were included. Overall complication rate was 9.4%, and mortality rate was 0.2%. Common complications were subcutaneous emphysema (3%), mediastinitis (1.3%), fistula (1.1%), and bleeding (1%). Another review included 894 patients in 13 studies. Overall, clinical failure occurred in 21.7% of patients, being the vast majority early failures (88.6%) [41].
The benefits of laser-assisted approach include the relative elegance and simplicity of the procedure in expert hands and, more important, the possibility of extending the myotomy almost until the bottom of the diverticulum. On the other hand, laser is not available in every center, and the learning curve can be challenging.
9.5.3 Stapler-Assisted Diverticulotomy
In 1993, Collard in Belgium and Martin Hirsch in England performed the first cases of cricopharyngeal myotomy with the use of a laparoscopic linear cutting stapler . The procedure is performed with the patient supine, with the extended neck and under general anesthesia. A bivalved Weerda diverticuloscope is introduced in order to expose the party wall between the diverticulum and the esophagus. The small caliber linear cutting stapler is introduced through the diverticuloscope down to the septum. The cartridge blade is put into the esophagus and the anvil blade in the pouch. Then, the stapler is secured with the septum between the two blades, and the two double (or triple) lines of staples are fired, in order to seal the diverticulum and the esophageal wall. The cutting blade is thus advanced and the septum between the two staple lines is divided.
In the last years, stapler-assisted cricopharyngeal myotomy became very popular . The sealing of the diverticulum and the esophagus, before the myotomy, minimizes the risk of complications. In addition, as compared to the carbon dioxide laser-assisted myotomy, this technique is less operator dependent, more reliable, quicker, and more easily available in every surgical center.
Antibiotics are not routinely given before or after the procedure. Absence of skin incision, shorter operative time, minimal or absent postoperative pain, quicker resumption of oral feeding, reduced hospital stay and overall operative costs, and lower rate of complications are some of the advantages of stapler-assisted cricopharyngeal myotomy over standard open surgical procedures.
On its counterpart, a careful selection of patients is necessary, with a special attention to the size of the pouch. Stapler-assisted procedure is not indicated for diverticula that are smaller than 3 cm, essentially because of some intrinsic characteristics of the laparoscopic staplers. The stapler anvil extends for 1–1.5 cm beyond the end of the staples, and the staples extend for few millimeters beyond the distal end of the knife blade: it means the residual pouch after the treatment is usually 1.5 cm deep. Some staplers with shorter not-functioning ends are available now, or the ends of the stapling device can be trimmed, in order to approximate the end of the cut to the bottom of the diverticulum.
Endoscopic stapling is better suited to medium-sized diverticula, 3–5 cm in depth. Smaller pouches will not accommodate the anvil of the stapler; diverticula deeper than 6 cm may represent a relative contraindication, because the cartridge is only 5 cm long and a too large residual pouch will remain after a single stapling [24, 25].
Over time, the technique was modified by applying traction sutures through the lateral edges of the common wall to provide proximal tension on the cricopharyngeal bar to ease engagement of the septum inside the stapler jaws [42, 43].
Clinical outcomes of this approach vary a lot in the different studies. Overall complication rate is 7%, which is comparable to the complication rate of carbon dioxide laser-assisted myotomy. Mortality rate is 0.3%. The most frequent complications are dental injuries (2%), caused by the large and rigid diverticuloscope, esophageal mucosal damages (1.6%), and perforations (1.6%) [33].
In a large cohort study by Bonavina et al. [29], 181 patients underwent stapler-assisted cricopharyngeal myotomy and were followed for a mean of 27 months. Mean operative time was 19 minutes, and postoperative hospitalization was 3 days. No mortality or severe complications occurred, but 1.1% of patients experienced dental injury. Conversions to open surgery were necessary in eight cases: seven were due to poor exposure and one to mucosal tear during the endoscopy. Of the patients undergoing the endoscopic stapling approach, 92% were symptom-free at the date of last follow-up.
In another cohort retrospective study published by a North American group [44], 337 patients underwent attempted staple-assisted myotomy. Technical failures, due to inadequate septum exposure, occurred in 3.9% of cases. Mean operative time was 28.8 minutes. The average hospital stay was 0.36 days, with 300 (92.6%) patients being discharged home on the same day of surgery. Symptom improvement was recorded in 93.5% of patients who were treated with success. There was a 4.0% major complication rate.
In a large review of 1089 patients treated by stapler-assisted myotomy, overall success rate was recorded in 81% of patients. Perioperative failures, due to a variety of reasons, were recorded in 6.2% of patients [41].
9.5.4 Harmonic Scalpel-Assisted Myotomy
Harmonic scalpel is used in laparoscopic surgery to simultaneously coagulate and cut vessels and tissues, with a minimal thermal injury to surrounding organs and structures. The harmonic scalpel uses ultrasounds inducing protein denaturation such that vessels are sealed, providing adequate and effective timely hemostasis.
Recently, harmonic scalpels have been successfully used for the cricopharyngeal myotomy, in combination with a rigid Weerda diverticuloscope [45] or with a soft diverticuloscope in combination with flexible endoscopes [46]. This technique can be particularly effective for the management of small diverticula, which are known to be more difficult to be treated with a linear stapler. The cutting surface of the harmonic scalpels reaches the very distal end of the device, and therefore it is possible to extend the diverticulotomy almost until the bottom of the pharyngeal pouch. Furthermore, the diameter of the harmonic scalpel (5 mm) is significantly smaller than the diameter of the vast majority of laparoscopic linear stapler (10 mm), the rigid articulated end is shorter, and it is easier to be maneuvered inside the rigid diverticuloscope. Few studies have been published so far including few patients [45, 47,48,49] with technical and clinical outcomes similar to those of stapler-assisted myotomy.
9.6 Transoral Cricopharyngeal Myotomy: Flexible Endoscopy
The management of Zenker diverticulum has undergone a series of revolutionary changes in recent years, one of the most important being the use of flexible endoscopy. In 1995, Ishioka in Brazil and Mulder in the Netherlands reported on the first patients with Zenker diverticulum treated by using a flexible endoscope and a precut needle knife or monopolar forceps [27, 35]. Lately, argon plasma coagulation was used, instead [50]. The principles of treatment are the same as rigid endoscopy: the septum between the diverticulum and the upper esophagus contains the cricopharyngeal muscle, and when it is cut during the procedure, the myotomy is completed, creating at the same time a common opening between the esophagus and the pouch.
If at the very beginning, immediately after the first pioneering experiences, the flexible approach was indicated only in patients at high risk for surgery, elderly and malnourished patients, or those with cardiovascular severe comorbidities, nowadays, in many centers, the treatment of Zenker diverticulum became an almost exclusive prerogative of interventional GI endoscopists. Bremner and De Meester considered the “flexible endoscopy” approach to the pharyngeal pouch to be a milestone in the field of gastrointestinal endoscopy [51].
The use of a flexible endoscope for the management of the Zenker diverticulum has some crucial and key advantages as compared with the use of a rigid endoscope. First cricopharyngeal myotomy can be performed in the endoscopy suite, without the need for general anesthesia and orotracheal intubation, because the flexible endoscope has a small diameter, usually less than 10 mm, and it does not cause any trauma or injury to the hypopharynx. Theoretically the procedure could be performed on outpatients, dramatically reducing the costs of hospitalization. Furthermore, the flexible endoscope approach can be virtually performed on all the patients, including those where the rigid endoscope cannot be correctly placed, because of upper teeth protrusion, inadequate jaw opening, or insufficient neck mobility, the last being very frequent in elderly patients [10].
When comparing flexible endoscope cricopharyngeal myotomy versus stapler-assisted procedure, similar outcomes in terms of hospital stay, dysphagia symptom score improvement, and complication rates are usually reported, at the cost of a significantly longer procedure time for endostapling [52].
There are at least three different techniques for cricopharyngeal myotomy by using a flexible endoscope: (1) the freehand, cap-assisted procedure, (2) the diverticuloscope-assisted, and (3) the peroral endoscopic myotomy or Z-POEM.
9.6.1 Preparation of Patients
Patients are kept fasting for 8–12 hours. However, they are usually recommended to drink a lot the day before the procedure, to flush the debris away from the pharyngeal pouch, especially in the case of large diverticula. Accidental aspiration during anesthesia can be a cause of severe complications. Furthermore, the visualization of the diverticular pouch during the myotomy can be compromised if debris are not carefully removed before.
The flexible endoscope cricopharyngeal myotomy can be performed either in the operating theater or (preferably) in a well-equipped endoscopy suite. Even if the procedure can be performed under propofol sedation in the vast majority of cases, the anesthesia equipment, including all the necessary for orotracheal intubation and ventilation, should be available in the room.
Any diagnostic endoscope can be used for the procedure, even if a certain preference goes to small caliber endoscopes (about 9 mm) with a water jet channel. Water jet can be extremely useful in case of incidental bleeding during the procedure, although a certain attention should be kept if the patient has not been intubated, because of the risk of aspiration.
Although there are no comparative data, there is a sufficient body of evidence in a relatively comparable treatment modalities that carbon dioxide reduces the risk of subcutaneous emphysema and pneumomediastinum. Therefore, carbon dioxide insufflation should be preferred over room air insufflation [17].
Antibiotic prophylaxis is not routinely administered before the procedure, because it does not reduce the risk of complications [17].
The procedure can be performed either with conscious sedation or under general anesthesia with propofol or endotracheal intubation according to local practice and expertise [7]. The choice between sedation and orotracheal intubation may depend also on the final technique used for the myotomy. The preliminary placement of a soft diverticuloscope protects the airways and minimizes the risk of aspiration. In such cases, the procedure can be safely performed under propofol sedation. In contrast, when the hand-free cap-assisted technique or the Z-POEM is used, intubation may be someway preferred by some operators.
Patients are placed in a left lateral position. The head, the neck, and the dorsal spine should be perfectly in line, in order to improve the visualization of the septum and of the diverticular pouch. If the head of the patients is turned on a side, the diverticulum may appear distorted or compressed and the procedure becomes trickier. A vacuum surgical mattress, if available, can be used to maintain the patient in the correct lateral left position under general anesthesia.
9.6.2 Freehand, Cap-Assisted Myotomy
A large bore nasogastric tube is sometimes inserted in the esophagus to obtain a better exposure of the septum, stabilize the diverticulum, and protect the esophageal wall by accidental thermal injury during sectioning of the septum [53].
Other experts prefer to use transparent caps or oblique-end distal hoods on the tip of the endoscope to help improve visualization and exposure of the septum and stabilize the endoscope in the hypopharynx and the cautery instrument [54]. The choice between one and the other device basically relies on the local availability and the preferences of the endoscopist (Fig. 9.3).
When the septum is well exposed and visualized, it can be divided by using a variety of cutting methods and needle knives. Again, none is definitely superior to the other; however needle knives should be thick enough to favor coagulation of tissue during the cutting of the septum . Thick precut needle knives, hook knives, or other devices from the ESD armamentarium, monopolar or bipolar forceps, and argon plasma coagulation have been successfully used over the years.
A hook knife enables the cricopharyngeal muscle fibers to be isolated, pulled upward, and then cut. Theoretically, the upward pull of the septal fibers minimizes the risk of perforation. Scissor-shaped cutting tools (like SB knife Jr., Sumitomo Bakelite Co., Tokyo, Japan) allow for an incision from the apex to the base of the septum but with a scissor-like movement, which pulls the muscle fibers toward the endoscope while cutting [17].
One of the cheapest needle knives is more than enough to complete the procedure safely and efficiently. However, in a recent multicenter, retrospective study, clinical success was found to be higher with hook knife (96.7%), compared to needle knife (76.6%) or insulated tip knife (47.6%) [55].
Argon plasma coagulation has been used in the early experience instead of needle knives or scissors. Argon plasma can offer the benefits of a deep coagulation of tissues and vessels, therefore reducing the risk of bleeding. On the other hand, the procedure needs more sessions, and the risk of thermal injuries to the surrounding structures is higher than with the needle knife [56]. Nowadays the use of argon plasma coagulation for the treatment of Zenker diverticulum has been almost completely abandoned.
Blended current is usually applied through the knives, to cut the septum by minimizing the risk of bleeding and thermal injuries to the surrounding structures and organs. However, the proper settings for every cutting device should be asked to the manufacturer of the electrosurgical generator.
The septum is usually divided in the middle by moving the tip of the endoscope and the knife from the inside of the esophagus toward the posterior esophageal wall or in the opposite direction. The two edges of the septum will immediately split and separate after the incision, showing the fibers of the cricopharyngeal muscle and of the posterior esophageal wall [7, 10].
Mild bleedings may occur during the myotomy and are usually stopped by using forced coagulation deployed with the same needle knife or, if necessary and available, coagulation forceps. Only anecdotally, spurting severe bleeding should be controlled using different measures, including epinephrine injection or fibrin glue.
The major issue of the procedure remains the correct balancing of the extension of the myotomy. A short myotomy may be insufficient and lead to early recurrences of symptoms. A cause of failure can be an incomplete myotomy of the cricopharyngeal muscle and/or insufficient marsupialization of the diverticular sac that leaves the food still entrapped inside the pouch. On the other hand, if the myotomy is extended beyond the bottom of the diverticulum, there will be an increased risk of perforation and mediastinitis. In the vast majority of cases, the septotomy is stopped between 5 and 10 mm from the bottom of the pouch.
In order to minimize the risk of perforation after the myotomy , clips are widely used at the base of the septotomy by the majority of endoscopists, despite there is no evidence of their impact on adverse events [17, 57].
After the procedure, the patients are usually kept fasting for 24 hours and allowed liquid diet the next day if their course is unremarkable. Contrast studies are not usually performed after the cricopharyngeal myotomy, before feeding [17].
9.6.3 Soft Diverticuloscope-Assisted Myotomy
Another device employed for the endoscopic treatment of Zenker diverticulum is the flexible diverticuloscope (ZD overtube, ZDO-22–30; Cook Medical, Winston-Salem, NC, USA), which mimics the effect of the rigid Weerda diverticuloscope. The flexible diverticuloscope significantly improves the fixation of the septum, its exposure, and visualization and, at the same time, protects the posterior diverticular and anterior esophageal wall by accidental thermal injuries (Fig. 9.4).
The diverticuloscope consists of a soft rubber overtube with two distal duck-bill flaps of 40 and 25 mm that, respectively, protect the esophageal and diverticular wall (Fig. 9.5).
For the placement of the diverticuloscope, a current and precise alignment of the head of the patient, neck, and chest is necessary, as explained before. The overtube is loaded over the endoscope that is pushed through the esophagus into the stomach. The diverticuloscope is then advanced over the endoscope up to a black marker indicating the average distance (16 cm) between the septum and teeth line. When the overtube is pushed forward, the short flap is kept aligned to the posterior side of the neck (where the diverticulum is) and the long flap is aligned anteriorly. In order to ease the passage of the diverticuloscope into the pharynx, the neck of the patient can be slightly hyperextended and two fingers inserted into the patient’s mouth to protect the posterior pharyngeal wall and push the distal end of the diverticuloscope inside. Once the diverticuloscope is in place, the endoscope is withdrawn to finally check under direct visual control the correct alignment and make further adjustments. After positioning of the diverticuloscope, the septum should be clearly visible in the center of the overtube, ready to be cut (Fig. 9.6).
Diverticuloscope-assisted myotomy. (a) The diverticuloscope has been correctly positioned, and the septum between the diverticulum and the esophagus well fixed and exposed. (b) The septum is cut in the middle by using a needle knife and electrocoagulation. (c) The two edges of the septum will immediately split after being divided, showing the fibers of the cricopharyngeal muscle and of the posterior esophageal wall. (d) An endoscopic clip is placed on the short residual part of the septum, to minimize the risk of perforation and bleeding
Sometimes, the positioning of the diverticuloscope can be a little bit more difficult. The placement of a very stiff guidewire (Savary guidewire, Cook Medical, Winston-Salem, NC, USA) into the stomach can facilitate the introduction of the overtube and the additional adjustments of the diverticuloscope under direct endoscopic control.
Cricopharyngeal myotomy can proceed now normally, by using the same variety of knives or scissors that can be used for the hands-free cap-assisted myotomy.
Some authors reported on the use of harmonic scalpels alongside the flexible endoscope, usually by using a small caliber endoscope (4.5 mm) to control the procedure [58].
The soft diverticuloscope really permits a clear vision of the septum of the diverticulum and a better control of the endoscope and devices. In the case of bleeding or need for flushing, the risk of aspiration pneumonia is significantly reduced, because the larynx and airways are completely bypassed by the overtube.
The major limit of the diverticuloscope-assisted procedure is the size of the diverticulum. The shorter flap, that is inserted into the diverticular pouch, is approximately 2.5 cm long. Consequently, in the case of smaller diverticula, the position of the diverticuloscope is less stable, with a consequent reduced exposition of the septum. Furthermore, the flexible diverticuloscope is currently not commercially available in many countries, including the United States, and this limited its widespread use.
Whether or not a diverticuloscope is mandatory for the safe and effective completion for the cricopharyngeal myotomy has been object of discussion [59, 60]. However, according to the published literature, overall use of a diverticuloscope does not seem to have a significant impact on success or complications, and the choice whether or not to use a diverticuloscope is left to the endoscopist’s discretion [17, 57].
9.6.4 Peroral Endoscopic Myotomy (Z-POEM)
On the wake of the treatment of achalasia and gastroparesis , novel procedures have been implemented for the treatment of Zenker diverticulum. Tunneling techniques used to cut the lower esophageal sphincter (peroral endoscopic myotomy, POEM) and the pylorus (G-POEM) have been modified and applied for the treatment of the Zenker diverticula (Z-POEM) [61, 62]. The procedure is still under evaluation, with few data on the long-term follow-up, but is definitely worth full consideration [17]. Z-POEM is performed under general anesthesia or deep sedation. Similarly, to the classic esophageal POEM, a standard high-definition endoscope, with a transparent distal hood attached on the tip, is used. Carbon dioxide insufflation is absolutely necessary, to minimize the risk of gas-related complications and adverse events. The endoscope in inserted into the hypopharynx, until the diverticulum and the septum are identified. A mucosal bleb is created by injection of 10 ml saline solution and indigo carmine approximately 1–2 cm proximal to the septum. A small longitudinal mucosa incision is performed along the major axis of the septum, with a triangle-tip knife or other ESD knives. The tip of the endoscope is advanced into the submucosal space, with the help of the distal attachment and by gently dissecting the submucosal fibers. Submucosal dissection and tunneling are performed by using the ESD knife and, according to the endoscopist’s preferences, spray coagulation, swift coagulation, or blend cut current. Similarly to esophageal POEM, the submucosal dissection is performed in the direction of the septum, along the surface of the muscle layer. Particular attention is devoted not to burn or damage the mucosal layer above the endoscope. Once the septum is reached and identified, a careful dissection on both the esophageal and diverticular side of the septum is completed. Cricopharyngeal myotomy and septotomy are then performed, by using the same needle knife used for the dissection, scissor-type ESD knives or other devices. The septum is cut until the bottom of the diverticular sac, or deeper, without any additional risk of complication, because the area of the septotomy is covered by intact mucosa. At the very end of the procedure, the original small mucosal incision can be secured with the application of 3–5 endoscopic clips. After the procedure patients are kept fasting for 24 hours, and antibiotics are usually administered. The day after a liquid diet is allowed [63].
The procedure is really interesting and promising, even if it is technically more challenging than simple needle knife septotomy. The main advantage is the chance to treat even very small diverticula that may not be amenable to classic transoral myotomy [64] and the possibility to extend very safely the myotomy until the end of the pouch and on the esophageal wall, thus reducing the risk of recurrence [65].
9.6.5 Results of Transoral Cricopharyngeal Myotomy by Using a Flexible Endoscope
Several case series were published since 1995 and demonstrated the efficacy and safety of flexible endoscopy in the management of Zenker diverticula, with very high clinical success rates.
A recent systematic review and meta-analysis included and analyzed a total of 813 patients [57]. Reported pooled success rate was 91% with an adverse event rate of 11.3% and an 11% recurrence rate. Severe complications, including bleeding and perforation, were managed conservatively in all the patients but two, in whom surgical drainage of an abscess was necessary.
In another more recent review study [66], focused on flexible endoscopy and including 589 patients, immediate symptom response after treatment was obtained in 88% of patients, with an overall complication rate of 13%, including 5% of bleeding and 7% of perforations. The vast majority of perforation was treated conservatively. The pooled data demonstrated an overall recurrence rate of 14%. When using the diverticuloscope, pooled success and adverse events rates were 84% and 10%, respectively.
Bleeding is usually intraoperative and is controlled endoscopically by electrocautery devices or clips. Micro perforations may occur during the procedure and are responsible for asymptomatic and uncomplicated subcutaneous emphysema. However, this finding does not mandate surgical operation and have a silent and self-limiting course in the vast majority of cases. The use of carbon dioxide during myotomy significantly reduces this event [10].
Unfortunately, there is a large degree of heterogeneity in the flexible endoscopic approach with no current standardization in the procedure itself or the postoperative care. No formal definition of clinical success exists, and the lower success rate reported in some series is very likely due to the fact that clinical remission was assessed according to the absence of a pool of symptoms and not only dysphagia. When success is defined according to dysphagia alone, clinical success rises to 90–100% [7].
The definition of success should be based solely on improvement and evaluation of symptoms and not on radiological findings. Often, a residual pouch is identified on postoperative radiograms, but if this finding is not associated with dysphagia or other symptoms, it should not be considered as a recurrence or indicate an unsuccessful treatment.
Furthermore, differently from surgery, flexible endoscopy is easily repeatable, without major problems or difficulties. In some series outcomes were assessed after one treatment session, while in other series it was determined after multiple treatment sessions [7].
Some authors indicate that the size of the diverticulum dictates the safety of the procedure with one-stage approaches for small- to medium-sized diverticula (up to 4 cm) and multiple stages in the approach for large diverticula (>4 cm) [54].
Whether a diverticuloscope is needed for the flexible endoscopic septotomy is still a matter of debate [17]. However, clear indications cannot be retrieved from the literature, because of controversial results. In a retrospective study published in 2007 on a total of 39 patients, 28 were treated with a cap-assisted and 11 with a diverticuloscope-assisted procedure [59]. The procedure time and complication rate was significantly greater with the cap than with diverticuloscope assistance. The clinical remission rate, evaluated using a pool of symptoms, was significantly higher after the diverticuloscope-assisted procedure compared with the cap technique (82% vs. 29%).
Nevertheless, in another recent retrospective study on 77 patients, 60 were treated with diverticuloscope assistance and 17 with cap assistance. Only in three patients treated with the diverticuloscope assistance were reported complications, and treatment success was not dissimilar in the two groups (68% and 60% in the diverticuloscope- and cap-assisted procedures, respectively) [60].
Depth of myotomy and size of the diverticulum may be important prognostic factors that determine clinical success in flexible endoscope approach. A retrospective single-center study on 89 patients recently analyzed the clinical success of flexible endoscopy diverticuloscope-assisted septotomy to identify potential prognostic variables [67]. Success was defined according to the improvement of all Zenker-related symptoms and not only dysphagia. Clinical success at the intention-to-treat analysis was 69%, 64%, and 46% at 6, 24, and 48 months, respectively. Adverse events occurred in three patients: perforation in two (2%) and postprocedural bleeding in one (1%). Independent variables for failure at 6 months were a septotomy length ≤25 mm and pretreatment pouch size ≥50 mm, whereas at 48 months, they were septotomy length ≤25 mm and posttreatment pouch size ≥10 mm. Success rates for ZD ranging in size from 30 mm to 49 mm with a septotomy >25 mm were 100% and 71% at 6 months and 48 months, respectively. Additional studies showed that small diverticula make the transoral procedure more difficult [28, 68].
This limitation may perhaps be overcome by the submucosal tunneling procedure (Z-POEM). Very few case reports and small series have been published so far on this innovative technique [61, 62, 69,70,71].
One of largest series included 19 patients who underwent Z-POEM and seven patients treated with a conventional needle-knife technique [65]. Clinical success was achieved in 89.5% of Z-POEM patients and 100% of non-tunneled flexible endoscopic patients. Recurrences occurred in 11.7% and 42.9% of patients of the Z-POEM and conventional treatment group, respectively (p = 0.096). There were four complications, including one pharyngeal perforation requiring open surgical repair in a patient with a small pouch with an associated cricopharyngeal bar in the Z-POEM group.
Another prospective study specifically focused on the role of a modified Z-POEM, called peroral endoscopic septotomy (POES), in small Zenker diverticula [64]. Differently from the traditional Z-POEM, the mucosal incision is performed directly on the septum, without the need for tunneling, but includes a submucosal dissection on both the sides of the septum and the following myotomy through the submucosal space.
Twenty patients were included in the series and were treated without orotracheal intubation. Mean size of diverticulum was 17.5 mm. Average procedure time was 14 minutes. No complications or adverse events occurred. Dysphagia significantly improved in 19 patients and no recurrences were reported at a mean follow-up time of 12.0 months.
In a multicenter international retrospective study, 75 patients were included [72]. The mean size of pharyngeal pouch was 3 cm. The overall technical success rate was 97.3%. Adverse events occurred in 6.7% (one mild bleed and four perforations, all managed conservatively). The mean procedure time was 52.4 minutes, and mean length of hospital stay was 1.8 days. Clinical success was achieved in 92% of patients. At the 12-month follow-up, only one patient reported symptom recurrence.
Due to the lack of long-term follow-up data, more studies are needed to define the role of Z-POEM in the management of Zenker diverticulum [17].
9.7 Conclusion
The treatment of Zenker diverticulum had a substantial evolution during the last century. Transoral approach, either rigid or flexible, is now considered easier, less invasive, reliable, with decreased morbidity and mortality compared with the open approach and has continued to gain popularity. Once reserved only to few elderly patients with comorbidities, nowadays transoral endoscopic cricopharyngeal myotomy has become the first-line treatment for the vast majority of patients with Zenker diverticula.
The level of evidence for superiority of flexible versus rigid endoscopic techniques for treatment of pharyngeal diverticula is limited based on currently available information.
The flexible endoscope approach is less standardized compared to the Collard operation with stapling devices, being the indications and choice of devices and techniques slightly different among the different centers. Nevertheless, flexible endoscopy is a good choice for the vast majority of patients with a Zenker diverticula. It is really minimally invasive and perceived by the patients more like a gastroscopy than an operation. The limits represented by the age of patients, previous treatments, local anatomy, and comorbidities almost completely disappear when using a flexible endoscope, being the procedure performed under sedation and with a 9-mm endoscope.
Open surgery is still indicated for very large diverticula, because a substantial part of the septum remains after the first endoscopic cricopharyngeal myotomy.
Nonetheless, interventions performed by a flexible endoscope are always repeatable, and the second and third sessions are always much less demanding than the first one.
Therefore, flexible endoscopic approach can be applied even to large diverticula, safely and efficiently, knowing that in these cases the procedure will be completed in two or three sessions.
The recent introduction of the Z-POEM permitted to overcome the limits of flexible endoscopy in the management of small diverticula. Cricopharyngeal myotomy can be now be performed under the mucosal layer, after submucosa tunneling, and be extended to cut completely the cricopharyngeal muscle and some muscular fibers of the upper third of the esophagus, by eliminating completely the pharyngeal outlet obstruction and the pouch.
In conclusion, a variety of different approaches to Zenker diverticulum are currently available, everyone with advantages and shortcomings. An individualized and tailored approach should be utilized. Flexible endoscopy, with its various techniques, plays now a very central role in the management of Zenker diverticulum, being perfectly adaptable, in the vast majority of clinical situations, to the need of patients and physicians.
References
Simic AP, Gurski RR, Pesko PM. The story beyond the Zenker’s pouch. Acta Chir Iugosl. 2009;56:9–16.
Haddad N, Agarwal P, Levi JR, et al. Presentation and management of Killian Jamieson diverticulum: a comprehensive literature review. Ann Otol Rhinol Laryngol. 2020;129:394–400.
Sutherland HD. Cricopharyngeal achalasia. J Thorac Cardiovasc Surg. 1962;43:114–26.
Belsey R. Functional disease of the esophagus. J Thorac Cardiovasc Surg. 1966;52:164–88.
Veenker EA, Andersen PE, Cohen JI. Cricopharyngeal spasm and Zenker’s diverticulum. Head Neck. 2003;25:681–94.
Ferreira LE, Simmons DT, Baron TH. Zenker’s diverticula: pathophysiology, clinical presentation, and flexible endoscopic management. Dis Esophagus. 2008;21:1–8.
Bizzotto A, Iacopini F, Landi R, et al. Zenker’s diverticulum: exploring treatment options. Acta Otorhinolaryngol Ital. 2013;33:219–29.
Watemberg S, Landau O, Avrahami R. Zenker’s diverticulum: reappraisal. Am J Gastroenterol. 1996;91:1494–8.
Cook IJ, Gabb M, Panagopoulos V, et al. Pharyngeal (Zenker’s) diverticulum is a disorder of upper esophageal sphincter opening. Gastroenterology. 1992;103:1229–35.
Law R, Katzka DA, Baron TH. Zenker’s Diverticulum. Clin Gastroenterol Hepatol. 2014;12:1773–82. quiz e1111–1772.
Siddiq MA, Sood S, Strachan D. Pharyngeal pouch (Zenker’s diverticulum). Postgrad Med J. 2001;77:506–11.
Sen P, Kumar G, Bhattacharyya AK. Pharyngeal pouch: associations and complications. Eur Arch Otorhinolaryngol. 2006;263:463–8.
Khan AS, Dwivedi RC, Sheikh Z, et al. Systematic review of carcinoma arising in pharyngeal diverticula: a 112-year analysis. Head Neck. 2014;36:1368–75.
Bowdler DA, Stell PM. Carcinoma arising in posterior pharyngeal pulsion diverticulum (Zenker’s diverticulum). Br J Surg. 1987;74:561–3.
Bradley PJ, Kochaar A, Quraishi MS. Pharyngeal pouch carcinoma: real or imaginary risks? Ann Otol Rhinol Laryngol. 1999;108:1027–32.
Grant PD, Morgan DE, Scholz FJ, et al. Pharyngeal dysphagia: what the radiologist needs to know. Curr Probl Diagn Radiol. 2009;38:17–32.
Weusten B, Barret M, Bredenoord AJ, et al. Endoscopic management of gastrointestinal motility disorders - part 2: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2020;52:600–14.
Costantini M, Zaninotto G, Rizzetto C, et al. Oesophageal diverticula. Best Pract Res Clin Gastroenterol. 2004;18:3–17.
Lixin J, Bing H, Zhigang W, et al. Sonographic diagnosis features of Zenker diverticulum. Eur J Radiol. 2011;80:e13–9.
Shanker BA, Davidov T, Young J, et al. Zenker’s diverticulum presenting as a thyroid nodule. Thyroid. 2010;20:439–40.
Skrobic OM, Simic AP, Radovanovic NS, et al. Current concepts in the anatomy and origin of pharyngeal diverticula. Acta Chir Iugosl. 2009;56:17–24.
Herbella FA, Patti MG. Modern pathophysiology and treatment of esophageal diverticula. Langenbeck’s Arch Surg. 2012;397:29–35.
Ishioka S, Felix VN, Sakai P, et al. Manometric study of the upper esophageal sphincter before and after endoscopic management of Zenker’s diverticulum. Hepato-Gastroenterology. 1995;42:628–32.
Zaninotto G, Narne S, Costantini M, et al. Tailored approach to Zenker’s diverticula. Surg Endosc. 2003;17:129–33.
Rizzetto C, Zaninotto G, Costantini M, et al. Zenker’s diverticula: feasibility of a tailored approach based on diverticulum size. J Gastrointest Surg. 2008;12:2057–64; discussion 2064-2055.
Zaninotto G, Costantini M, Boccu C, et al. Functional and morphological study of the cricopharyngeal muscle in patients with Zenker’s diverticulum. Br J Surg. 1996;83:1263–7.
Ishioka S, Sakai P, Maluf Filho F, et al. Endoscopic incision of Zenker’s diverticula. Endoscopy. 1995;27:433–7.
Gutschow CA, Hamoir M, Rombaux P, et al. Management of pharyngoesophageal (Zenker’s) diverticulum: which technique? Ann Thorac Surg. 2002;74:1677–82; discussion 1682-1673.
Bonavina L, Bona D, Abraham M, et al. Long-term results of endosurgical and open surgical approach for Zenker diverticulum. World J Gastroenterol. 2007;13:2586–9.
Simic A, Radovanovic N, Stojakov D, et al. Surgical experience of the national institution in the treatment of Zenker’s diverticula. Acta Chir Iugosl. 2009;56:25–33.
Mantsopoulos K, Psychogios G, Kunzel J, et al. Evaluation of the different transcervical approaches for Zenker diverticulum. Otolaryngol Head Neck Surg. 2012;146:725–9.
Nehring P, Krasnodebski IW. Zenker’s diverticulum: aetiopathogenesis, symptoms and diagnosis. Comparison of operative methods. Prz Gastroenterol. 2013;8:284–9.
Yuan Y, Zhao YF, Hu Y, et al. Surgical treatment of Zenker’s diverticulum. Dig Surg. 2013;30:207–18.
Collard JM, Otte JB, Kestens PJ. Endoscopic stapling technique of esophagodiverticulostomy for Zenker’s diverticulum. Ann Thorac Surg. 1993;56:573–6.
Mulder CJ, den Hartog G, Robijn RJ, et al. Flexible endoscopic treatment of Zenker’s diverticulum: a new approach. Endoscopy. 1995;27:438–42.
Dohlman G, Mattsson O. The endoscopic operation for hypopharyngeal diverticula: a roentgencinematographic study. AMA Arch Otolaryngol. 1960;71:744–52.
Hoeksema PE, van Overbeek JJ. The CO2 laser in laryngeal diseases. Acta Otorhinolaryngol Belg. 1981;35:23–7.
van Overbeek JJ, Hoeksema PE, Edens ET. Microendoscopic surgery of the hypopharyngeal diverticulum using electrocoagulation or carbon dioxide laser. Ann Otol Rhinol Laryngol. 1984;93:34–6.
Kos MP, David EF, Mahieu HF. Endoscopic carbon dioxide laser Zenker’s diverticulotomy revisited. Ann Otol Rhinol Laryngol. 2009;118:512–8.
Helmstaedter V, Engel A, Huttenbrink KB, et al. Carbon dioxide laser endoscopic diverticulotomy for Zenker’s diverticulum: results and complications in a consecutive series of 40 patients. ORL J Otorhinolaryngol Relat Spec. 2009;71:40–4.
Verdonck J, Morton RP. Systematic review on treatment of Zenker’s diverticulum. Eur Arch Otorhinolaryngol. 2015;272:3095–107.
Bonavina L, Bona D, Aiolfi A, et al. Transoral septum stapling of Zenker diverticulum is feasible and safe through a soft overtube. Surg Innov. 2015;22:207–9.
Provenzano L, Salvador R, Cutrone C, et al. Traction on the septum during transoral septotomy for Zenker diverticulum improves the final outcome. Laryngoscope. 2020;130:637–40.
Wilken R, Whited C, Scher RL. Endoscopic staple diverticulostomy for Zenker’s diverticulum: review of experience in 337 cases. Ann Otol Rhinol Laryngol. 2015;124:21–9.
Fama AF, Moore EJ, Kasperbauer JL. Harmonic scalpel in the treatment of Zenker’s diverticulum. Laryngoscope. 2009;119:1265–9.
Hondo FY, Maluf-Filho F, Giordano-Nappi JH, et al. Endoscopic diverticulotomy by harmonic scalpel (Ultracision): an experimental model. Endoscopy. 2009;41(Suppl 2):E104–5.
Nielsen HU, Trolle W, Rubek N, et al. New technique using LigaSure for endoscopic mucomyotomy of Zenker’s diverticulum: diverticulotomy made easier. Laryngoscope. 2014;124:2039–42.
Andersen MF, Trolle W, Anthonsen K, et al. Long-term results using LigaSure™ 5 mm instrument for treatment of Zenker’s diverticulum. Eur Arch Otorhinolaryngol. 2017;274:1939–44.
Pons-Beltrán V, García Morales N, Sáez-González E, et al. A long-term prospective study of the efficacy and safety of endoscopic septotomy using the LigaSure® system for the treatment of Zenker’s diverticulum. Rev Esp Enferm Dig. 2019;111:378–83.
Wahab PJ, Mulder CJ, den Hartog G, et al. Argon plasma coagulation in flexible gastrointestinal endoscopy: pilot experiences. Endoscopy. 1997;29:176–81.
Bremner CG, DeMeester TR. Endoscopic treatment of Zenker’s diverticulum. Gastrointest Endosc. 1999;49:126–8.
Repici A, Pagano N, Fumagalli U, et al. Transoral treatment of Zenker diverticulum: flexible endoscopy versus endoscopic stapling. A retrospective comparison of outcomes. Dis Esophagus. 2011;24:235–9.
Mulder CJ, Costamagna G, Sakai P. Zenker’s diverticulum: treatment using a flexible endoscope. Endoscopy. 2001;33:991–7.
Christiaens P, De Roock W, Van Olmen A, et al. Treatment of Zenker’s diverticulum through a flexible endoscope with a transparent oblique-end hood attached to the tip and a monopolar forceps. Endoscopy. 2007;39:137–40.
Mittal C, Diehl D, Draganov P, et al. Practice patterns, techniques, and outcomes of flexible endoscopic myotomy for Zenker’s diverticulum: retrospective, multi-center study. Endoscopy. 2020. https://doi.org/10.1055/a-1219-4516.
Rabenstein T, May A, Michel J, et al. Argon plasma coagulation for flexible endoscopic Zenker’s diverticulotomy. Endoscopy. 2007;39:141–5.
Ishaq S, Hassan C, Antonello A, et al. Flexible endoscopic treatment for Zenker’s diverticulum: a systematic review and meta-analysis. Gastrointest Endosc. 2016;83:1076–89.e1075
Diez Redondo P, Núñez Rodríguez H, de Benito Sanz M, et al. Endoscopic treatment of Zenker’s diverticulum with Ligasure: simple, safe and effective. Endosc Int Open. 2019;7:E203–e208.
Costamagna G, Iacopini F, Tringali A, et al. Flexible endoscopic Zenker’s diverticulotomy: cap-assisted technique vs. diverticuloscope-assisted technique. Endoscopy. 2007;39:146–52.
Bresteau C, Barret M, Guillaumot MA, et al. Do we still need a diverticuloscope for the flexible endoscopic septotomy of Zenker’s diverticulum? J Gastroenterol Hepatol. 2020;35:630–3.
Li QL, Chen WF, Zhang XC, et al. Submucosal tunneling endoscopic septum division: a novel technique for treating Zenker’s diverticulum. Gastroenterology. 2016;151:1071–4.
Brewer Gutierrez OI, Moran R, Yang J, et al. Successful single-session cricopharyngeal and Zenker’s diverticulum peroral endoscopic myotomy. Endoscopy. 2018;50:E220–e221.
Brewer Gutierrez OI, Ichkhanian Y, Spadaccini M, et al. Zenker’s diverticulum per-oral endoscopic myotomy techniques: changing paradigms. Gastroenterology. 2019;156:2134–5.
Repici A, Spadaccini M, Belletrutti PJ, et al. Peroral endoscopic septotomy for short-septum Zenker’s diverticulum. Endoscopy. 2020;52:563–8.
Klingler MJ, Landreneau JP, Strong AT, et al. Endoscopic mucosal incision and muscle interruption (MIMI) for the treatment of Zenker’s diverticulum. Surg Endosc. 2020. https://doi.org/10.1007/s00464-020-07861-5.
Li LY, Yang YT, Qu CM, et al. Endoscopic needle-knife treatment for symptomatic esophageal Zenker’s diverticulum: a meta-analysis and systematic review. J Dig Dis. 2018;19:204–14.
Costamagna G, Iacopini F, Bizzotto A, et al. Prognostic variables for the clinical success of flexible endoscopic septotomy of Zenker’s diverticulum. Gastrointest Endosc. 2016;83:765–73.
Jones D, Aloraini A, Gowing S, et al. Evolving management of Zenker’s diverticulum in the endoscopic era: a North American experience. World J Surg. 2016;40:1390–6.
Delis K, Robotis J, Sachitzi E, et al. Submucosal tunneling endoscopic septum division of a Zenker’s diverticulum. Ann Gastroenterol. 2018;31:634.
Hajifathalian K, Dawod Q, Saumoy M, et al. Submucosal tunneling endoscopic septum division for treatment of Zenker’s diverticulum. Endoscopy. 2018;50:E340–e341.
Hernández Mondragón OV, Solórzano Pineda MO, Blancas Valencia JM. Zenker’s diverticulum: submucosal tunneling endoscopic septum division (Z-POEM). Dig Endosc. 2018;30:124.
Yang J, Novak S, Ujiki M, et al. An international study on the use of peroral endoscopic myotomy in the management of Zenker’s diverticulum. Gastrointest Endosc. 2020;91:163–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Costamagna, G., Familiari, P., Landi, R. (2021). Indication, Technique, and Results of Endoscopic Cricomyotomy. In: Horgan, S., Fuchs, KH. (eds) Innovative Endoscopic and Surgical Technology in the GI Tract . Springer, Cham. https://doi.org/10.1007/978-3-030-78217-7_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-78217-7_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-78216-0
Online ISBN: 978-3-030-78217-7
eBook Packages: MedicineMedicine (R0)