Abstract
Background
National rates of laparoscopic antireflux surgery grew steadily in the 1990s. Since then, a highly visible randomized trial has questioned the long-term effectiveness of antireflux surgery, several new endoscopic therapies have been developed, and proton pump inhibitors have become available over the counter. Whether these recent developments have had an impact on the use of antireflux surgery remains unknown.
Methods
Using data from the Nationwide Inpatient Sample, this study identified all patients older than 18 years who underwent antireflux surgery between 1994 and 2003. Sampling weights were used to estimate the total number of procedures performed in the United States each year. Population-based rates were determined using denominators from U.S. census data.
Results
Confirming the results of earlier studies, this study found that the annual number of antireflux procedures grew rapidly during the 1990s, peaking at 31,695 (15.7 cases per 100,000 adults) in 1999. After 1999, surgical rates declined steadily, falling approximately 30% by 2003 to 23,998 (11 cases per 100,000; p < 0.0001). Use of antireflux procedures fell more precipitously among younger patients (39% for 30- to 49-year-olds vs 12.5% for those older than 60 years; p < 0.0001) and at teaching hospitals (36% vs 23% at nonteaching hospitals; p < 0.0001). The proportion of cases managed laparoscopically remained stable after 1999.
Conclusions
The use of antireflux surgery in the United States has declined substantially. Although other factors may be involved, this trend may reflect new questions about the long-term effectiveness of surgery and suggests the need for prospective randomized clinical trials assessing current therapies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
The rates for antireflux surgery in the United States increased dramatically during the 1990s. Between 1990 and 1997, population-based rates of antireflux surgery rose nearly threefold, from 4.4 to 12 procedures per 100,000 adults [4]. Increases in procedure rates were no doubt attributable in part to the dissemination of laparoscopic techniques for fundoplication.
After the introduction of laparoscopic Nissen fundoplication in 1991, the proportion of antireflux procedures performed laparoscopically increased to 65% by 1997 [3, 4]. Growing interest in antireflux surgery also may have been fueled by the results of a large randomized controlled trial from the Department of Veterans Affairs (VA) Cooperative Studies Program demonstrating the early effectiveness of surgical therapy [16].
Over the past few years, however, several factors may have dampened enthusiasm for antireflux surgery. Late follow-up data from the same VA trial raised questions about the long-term effectiveness of surgery in terms of alleviating reflux symptoms and keeping patients off medications [17]. Although not a primary end point of the study, higher long-term mortality was noted among the patients undergoing surgery. Other factors that may have reduced patient referrals to surgeons for antireflux surgery include the availability of over-the-counter proton pump inhibitors since 2003 and new endoscopic therapies for treating gastroesophageal reflux.
Whether these recent developments have had a measurable effect on the use of antireflux surgery has not been explored. For this reason, we examined recent trends in procedure rates using data from the Nationwide Inpatient Sample (NIS), the largest all-payer inpatient care database in the United States.
Methods
Database
Hospital discharge data were obtained from the NIS on the Healthcare Cost and Utilization Project for the years 1994 to 2003. The NIS was designed to provide national estimates of health care utilization. The database consists of all discharge abstracts from a 20% stratified probability sample of U.S. nonfederal, nonmilitary hospitals. The hospitals are divided into strata on the basis of five characteristics: ownership/control, bed size, teaching status, urban/rural location, and U.S. region.
Each year, the NIS provides information on 5 to 8 million inpatient stays from approximately 1,000 hospitals. The data include patient-level clinical, demographic, and resource use information. Discharge data are weighted to facilitate the calculation of national estimates of utilization measures [6].
Patient selection
We used International Classification of Diseases (ICD-9) procedure and diagnosis codes to identify all hospitalizations during which an antireflux procedure was performed, according to the method established by Finlayson et al. [4]. Specifically, the procedure codes 44.65 (esophagogastroplasty) and 44.66 (other procedure for creation of esophagogastric sphincteric competence) were used to identify an antireflux procedure. Given the more general description of code 44.65, we excluded records with this procedure code that did not also include the diagnosis codes for esophagitis, gastroesophageal reflux, esophageal ulcer, or diaphragmatic hernia, namely, 530.10, 530.11, 530.19, 530.81, 530.20, and 553.3. For both procedure codes, we excluded cases with a diagnosis code for achalasia (530.0), esophageal cancer ((150.0–150.5, 150.8–150.9), or diaphragmatic hernia with obstruction (552.3) or gangrene (551.3). We also excluded cases coded as an emergency hospital admission.
Before 2004, there were no specific ICD-9 codes to identify whether antireflux procedures were performed laparoscopically. Using the approach of Finlayson et al. [4], we estimated the number of laparoscopic antireflux operations from cases with a separate laparoscopic code listed in addition to the procedure codes listed earlier. These additional codes included those for diagnostic laparoscopy (54.21), laparoscopic cholecystectomy (54.22), and laparoscopic lysis of adhesions (54.51). We also included cases with antireflux surgery codes associated with a live discharge and a hospital stay of 2 days or longer.
Data analysis
Our primary objective was to evaluate secular trends in rates of antireflux surgery in the United States from 1994 to 2003. For the numerator, the annual number of antireflux procedures performed was estimated using sampling weights provided with the NIS data set. For the denominator, we used data from the U.S. Census Bureau to obtain year-specific estimates of both the total adult population (age 18 years and older) as well as the population for individual age groups. This allowed us to determine overall and age-specific trends in surgical utilization.
After the surgical rates had been plotted, it was readily apparent that utilization increased steadily throughout the 1990s, peaked in 1999, and fell rapidly through 2003. Given the monotonic nature of the decline after 1999, we applied linear regression methods to assess the significance of the rate decrease between 1999 and 2003.
For a better understanding of the trends in overall rates, we sought to determine whether patient, hospital, or operative characteristics associated with antireflux surgery have changed over time. Secular trends for dichotomous variables (gender, in-hospital mortality, concurrent splenectomy, operative approach, hospital teaching status) were tested for significance using logistic regression, with year as a continuous independent variable. The Wilcoxin rank-sum test was used to evaluate continuous dependent variables (patient age, length of hospital stay). The Cochran–Mantel–Haenszel test was used to assess the significance of differences in the rate of decline in antireflux surgery by age group, gender, and hospital type, adjusting for year. All statistical analyses were conducted using SAS software version 9.1.2 (SAS Institute Inc, Cary, NC, USA).
Results
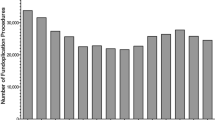
Confirming the results of previous studies, we found that the rates of antireflux surgery for adults climbed steadily throughout the 1990s, peaking in 1999 at 31,695 cases (15.7 per 100,000) (Fig. 1). This was more than twice the number of cases managed in 1994 (12,661, or 6.6 per 100,000). After 1999, however, the number of antireflux operations declined substantially, falling to 23,998 cases (11 per 100,000) by 2003, a drop of 30% (p < 0.002) (Fig. 1).
Trends in surgery utilitzation after 1999 varied by age, gender, and hospital teaching status. The decline in antireflux operations was greatest among younger patients (Fig. 2). Between 1999 and 2003, surgery rates fell by 38% for patients 18 to 39 years of age, as compared to 12.5% for patients older than 60 years (p < 0.0001). The median age of patients undergoing surgery rose accordingly, from 48 to 52 years (p < 0.0001) (Table 1). In addition, utilization of antireflux surgery declined to a greater extent among male patients (41% vs 22% among females; p < 0.0001) and at teaching hospitals (36% vs 23% at nonteaching hospitals; p < 0.0001) (Fig. 2).
There was no appreciable change in operative approach or surgical outcomes during the study period. The proportion of cases managed laparoscopically remained stable between 1999 and 2003 (69% vs 68%; p = 0.548). In addition, there were no changes in the rates of splenectomy (0.9%), in-hospital mortality (0.3%), or median length of hospital stay (2 days (Table 1).
Discussion
Like previous studies using similar methods and data sources, this population-based study demonstrated a rapid rise in antireflux surgery rates during the 1990s. In contrast, the utilization of antireflux surgery declined dramatically after its peak in 1999. The overall population-based rate for antireflux surgery fell by 30% between 1999 and 2003, with no indication of a plateau in declining operative rates.
A potential limitation of this study is that the NIS database does not include operations performed at outpatient surgical centers. Recently, there has been increasing interest in laparoscopic antireflux surgery performed at outpatient centers, with several reports documenting the safety of this approach [5, 13]. Still, the majority of antireflux operations are performed in an inpatient setting. Although the annual rate of outpatient procedures is unknown, it is unlikely that these cases account for a significant proportion of the observed decline in antireflux surgery.
Our study does not explicitly address the question of why rates of antireflux surgery have declined in recent years, but there are several potential explanations. To begin with, there appears to be uncertainty among gastroenterologists, other referring physicians, and perhaps even surgeons regarding the overall benefits of antireflux surgery. Although the introduction of laparoscopic techniques has improved patient acceptance of antireflux surgery, several authors have voiced concern about the associated morbidity and long-term effectiveness of these procedures [1, 7, 8]. Supporting these concerns, long-term outcomes from a widely publicized randomized trial comparing open surgical and medical therapy for gastroesophageal reflux disease (GERD) demonstrated that 62% of patients in the surgical arm had resumed antireflux medications 10 years after treatment [17]. Our finding that rates of antireflux surgery have declined most sharply among younger patients suggests that referring physicians may be reserving surgical therapy for patients with refractory, long-standing disease.
Another factor underlying declining surgery rates may be growing interest in nonsurgical treatments of GERD. Medical therapy with proton pump inhibitors (PPIs) has proved to be highly effective in controlling reflux symptoms for most patients and currently is generally considered to be the mainstay of treatment. Given their safety profile, there also has been less concern about long-term use of PPIs for maintenance therapy [9]. Furthermore, the recent approval of omeprazole for over-the-counter use has meant that PPIs are now readily available to patients and less expensive.
In addition to medical therapy, endoscopic treatments for GERD have been introduced as an alternative to surgery. Although data on long-term effectiveness are lacking, more than 10,000 of these endoluminal procedures have been performed in the United States [14].
Although our study does not provide data on this question, it is possible that declining rates for antireflux surgery are causally related to the rapid growth of bariatric surgery during the same time period [18]. The two groups of procedures tend to be performed by general surgeons with overlapping skills and interests. As the practices of many of these surgeons have become saturated with bariatric surgery, it is possible that they have become less “aggressive” with regard to GERD. Furthermore, gastric bypass may have replaced fundoplication for some patients with GERD, given recent evidence that this bariatric procedure may be the most effective treatment for GERD for obese patients [11, 12].
Finally, it is worth considering the possibility that the drop in rates for antireflux surgery may be attributable to a “reservoir effect.” After the introduction of laparoscopic cholecystectomy in 1991, overall cholecystectomy rates rose sharply over several years, then declined (although to a rate higher than before 1991) [2, 19]. Some have speculated that these trends reflect a “reservoir” of mildly symptomatic patients not quite bothered enough to have open surgery before 1991 [10]. Thus, the rates grew rapidly as pent-up demand was met by new technology, but fell again once it was exhausted. Although conceptually plausible, this explanation seems less likely to explain trends in antireflux surgery. Given the nearly 20 million Americans with significant GERD [15], it is hard to imagine that surgeons made a significant dent in the reservoir of patients with GERD by managing 20,000 to 30,000 cases per year during the 1990s.
Whether justified or not, it is clear that fewer patients with GERD are undergoing surgical intervention. Which therapeutic approach—medical, surgical, or endoscopic—is best suited for which patients is an important question that remains unanswered. Our study suggests the need for prospective, randomized trials to compare current therapies and to define appropriate algorithms for the management of this very common disease.
References
DeVault KR, Castell DO (2005) Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease. Am J Gastroenterol 100: 190–200
Ferreira MR, Bennett RL, Gilman SC, Mathewson S, Bennett CL (1999) Diffusion of laparoscopic cholecystectomy in the Veterans Affairs health care system, 1991–1995. Eff Clin Pract 2: 49–55
Finlayson SR, Birkmeyer JD, Laycock WS (2003) Trends in surgery for gastroesophageal reflux disease: the effect of laparoscopic surgery on utilization. Surgery 133: 147–153
Finlayson SR, Laycock WS, Birkmeyer JD (2003) National trends in utilization and outcomes of antireflux surgery. Surg Endosc 17: 864–867
Finley CR, McKernan JB (2001) Laparoscopic antireflux surgery at an outpatient surgery center. Surg Endosc 15: 823–826
HCUP (2003) Nationwide Inpatient Sample (NIS). Agency for Healthcare Research and Quality
Kahrilas PJ (1999) Laparoscopic antireflux surgery: silver bullet or the emperor’s new clothes? Am J Gastroenterol 94: 1721–1723
Klaus A, Hinder RA, DeVault KR, Achem SR (2003) Bowel dysfunction after laparoscopic antireflux surgery: incidence, severity, and clinical course. Am J Med 114: 6–9
Metz DC (2004) Managing gastroesophageal reflux disease for the lifetime of the patient: evaluating the long-term options. Am J Med 117(Suppl 5A): 49S–55S
Nenner RP, Imperato PJ, Rosenberg C, Ronberg E (1994) Increased cholecystectomy rates among Medicare patients after the introduction of laparoscopic cholecystectomy. J Community Health 19: 409–415
Patterson EJ, Davis DG, Khajanchee Y, Swanstrom LL (2003) Comparison of objective outcomes following laparoscopic Nissen fundoplication versus laparoscopic gastric bypass in the morbidly obese with heartburn. Surg Endosc 17: 1561–1565
Perry Y, Courcoulas AP, Fernando HC, Buenaventura PO, McCaughan JS, Luketich JD (2004) Laparoscopic Roux-en-Y gastric bypass for recalcitrant gastroesophageal reflux disease in morbidly obese patients. JSLS 8: 19–23
Ray S (2003) Result of 310 consecutive patients undergoing laparoscopic Nissen fundoplication as hospital outpatients or at a freestanding surgery center. Surg Endosc 17: 378–380
Rothstein RI, Dukowicz AC (2005) Endoscopic therapy for gastroesophageal reflux disease. Surg Clin North Am 85: 949–965
Sandler RS, Everhart JE, Donowitz M, Adams E, Cronin K, Goodman C, Gemmen E, Shah S, Avdic A, Rubin R (2002) The burden of selected digestive diseases in the United States. Gastroenterology 122: 1500–1511
Spechler SJ (1992) Comparison of medical and surgical therapy for complicated gastroesophageal reflux disease in veterans. The Department of Veterans Affairs Gastroesophageal Reflux Disease Study Group. N Engl J Med 326: 786–792
Spechler SJ, Lee E, Ahnen D, Goyal RK, Hirano I, Ramirez F, Raufman JP, Sampliner R, Schnell T, Sontag S, Vlahcevic ZR, Young R, Williford W (2001) Long-term outcome of medical and surgical therapies for gastroesophageal reflux disease: follow-up of a randomized controlled trial. JAMA 285: 2331–2338
Trus TL, Pope GD, Finlayson SR (2005) National trends in utilization and outcomes of bariatric surgery. Surg Endosc 19: 616–620
Urbach DR, Stukel TA (2005) Rate of elective cholecystectomy and the incidence of severe gallstone disease. CMAJ 172: 1015–1019
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Finks, J.F., Wei, Y. & Birkmeyer, J.D. The rise and fall of antireflux surgery in the United States. Surg Endosc 20, 1698–1701 (2006). https://doi.org/10.1007/s00464-006-0042-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-006-0042-3