Abstract
Background
Prophylactic surgery for patients carrying a positive RET proto-oncogene proved to be highly effective in curing those likely to experience the development of a medullary carcinoma. Video-assisted procedures have been proved feasible for central compartment dissection.
Methods
A total of 15 patients (7 men and 8 women) with a positive RET proto-oncogene underwent total thyroidectomy and central compartment lymphadenectomy via a video-assisted approach. The mean age of the patients was 32.5 years. The echographically estimated mean volume was 10.3 ml, and the mean diameter of the main nodule was 8.8 mm. Preoperative ultrasound showed an absence of lateral neck lymph node involvement in all cases. No drain was used. Direct laryngoscopy was performed in all cases 1 month after surgery.
Results
The mean operative time was 67.3 min. A transient hypoparathyroidism occurred in one patient, and a permanent hypoparathyroidism occurred in another patient. No laryngeal nerve palsy was present. All the patients were discharged on postoperative day 1. Histology showed a medullary carcinoma in 10 patients and diffuse C-cell hyperplasia in 5 patients. The mean number of lymph nodes removed was 5.1. None of these nodes proved to be metastatic. Calcitonin levels were undetectable in all six patients who had a follow-up period longer than 1 year.
Conclusion
Video-assisted central compartment lymphadenectomy was proved to be effective and safe. The procedure demonstrated a complication rate comparable with that for the conventional procedure, a better cosmetic outcome, and less postoperative pain. Although the video-assisted access proved to be a valid option for the treatment of patients carrying a positive RET proto-oncogene, a greater number of cases with a longer follow-up period is necessary to estimate the impact of the video-assisted approach on central neck lymphadenectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Prophylactic thyroidectomy for RET proto-oncogene carriers before a clinically evident medullary carcinoma develops is currently performed in several centers, with a very high cure rate [7, 10, 16, 17]. One of the most important surgical steps for these patients is a careful central compartment node clearance, which is mandatory for all patients who present with positive pentagastrin test results. For this reason, endocrine surgeons were highly reluctant to adopt minimally invasive procedures to remove thyroid and lymph nodes for these patients [5]. On the other hand, the small size of the involved glands, which do not yet harbor big tumors, makes these patients ideal candidates for minimally invasive video-assisted thyroidectomy. Findings have shown that this procedure gives excellent results and is very well accepted by patients for its excellent cosmetic outcome and less painful postoperative course [1, 13].
In a previous preliminary report [14], the possibility that operating on these patients via a minimally invasive video-assisted procedure guarantees an adequate level 6 lymphadenectomy was demonstrated. The excellent results obtained in this small group of patients stimulated us to recruit, during the past year, a greater number of patients to allow a final evaluation of the results obtained with surgery via a minimally invasive access. Moreover, a longer follow-up period has made it possible to draw some conclusions in terms of oncologic radicality, as demonstrated by calcitonin serum levels measured after surgery.
Methods
Between January 2002 and July 2005, 15 patients with a positive genetic test for RET proto-oncogene were selected to undergo a prophylactic total thyroidectomy and central neck compartment dissection in our department. All these patients gave their informed consent for surgery using a minimally invasive video-assisted procedure.
Technique
Once the thyroidectomy is accomplished through the central unique access, as previously reported [15], the central compartment is approached. For this purpose, the endoscope is placed at the head of the patient, thus allowing a full vision of the superior mediastinum (Fig. 1). The recurrent laryngeal nerve is followed as the main anatomic landmark. All the lymphatic tissue between the carotid sheath and the trachea is dissected until the innominate trunk is reached, first on the right side and then on the left side.
Currently, all the lymphatic tissue is extracted through the central incision and divided from the tracheal plane on the midline under direct vision by means of the Harmonic CS-14C (Ethicon Endosurgery, Cincinnati, OH, USA) No drains were used in any case.
The 15 patients (8 women and 7 men) in this study had a mean age of 32.5 years (range, 10–56 years). All the patients underwent the following preoperative examinations: blood basal calcitonin level (Ct), pentagastrin stimulation test (Pg), plasmatic and urinary catecholamines, and neck ultrasound examination (US).
Of the 11 patients with a normal Ct level (<10 pg/ml), 4 had high basal levels ranging from 12 to 157 pg/ml. Of the 15 study patients, 12 had positive Pg test results ranging from 31 to 2,083 pg/ml. Only three patients showed negative Pg test results, with values ranging from 17 to 20 pg/ml. These three patients were in the group with normal Ct results. All the patients had normal serum and urinary catecholamine values.
The mean ultrasound estimated volume was 10.3 ml (range, 4–28 ml), and the mean detected volume of the main nodule was 8.8 mm (range, 4–19 mm). Five patients showed a micronodular pattern with only an inhomogeneous pattern and no nodules at ultrasound examination. Direct laryngoscopy was performed for all the patients 1 month after surgery.
Results
The mean operative time for total thyroidectomy and central neck compartment dissection with the video-assisted technique was 67.3 min (range, 40–120 min). All the patients were discharged from the hospital the day after surgery (<24 h).
After surgery, 2 of the 15 patients demonstrated signs of hypoparathyroidism (Table 1), which required therapy with calcium carbonate and vitamin D for 20 days. After this period, therapy was discontinued in both cases. One patient fully recovered, and was normocalcemic 3 months after surgery. The other patient experienced permanent hypoparathyroidism. In this patient, despite a parathyroid hormone value of 20 pg/ml, the serum calcium level was demonstrated to be lower than normal (7.8 mg/dl 2 years after surgery). This patient required oral calcium and vitamin D3 supplementation to be free of hypocalcemia symptoms. No laryngeal nerve palsy was registered.
Histology showed a single focus of medullary carcinoma in six patients (range, 1–8 mm), a multifocal medullary thyroid carcinoma in four patients (main nodule diameter, 8, 7, 4, and 3 mm, respectively), and C-cell hyperplasia in five patients. In one of the patients with C-cell hyperplasia, histology showed a microscopic (1 mm) papillary carcinoma.
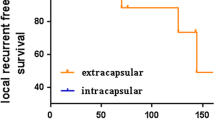
None of the patients had proven metastases to the lymphatic tissue of the central neck compartment. Of the 15 study patients, 8 had a postoperative follow-up period longer than 6 months (mean, 22.1 months; range, 8–44 months). Calcitonin levels were undetectable in all of these 8 patients. The mean number of lymph nodes removed was 5.1 (range, 2–13). Despite the low number of lymph nodes removed in nine patients, it must be stressed that fat tissue of the central neck compartment and a part of the thymus was removed in all these patients.
Pathologic evaluation of lymphatic tissue from the central compartment usually showed a small number of lymph nodes in this series of patients. Indeed, for all patients showing C-cell hyperplasia or a very small focus of medullary carcinoma, there was no macroscopic involvement of lymph nodes. In these cases, our pathologist suggested that a difficult sampling (macroscopic absence of disease outside the thyroid gland) of lymphatic tissue was the reason for the small number of lymph nodes removed. In the other cases, with larger thyroid nodules (8, 7, and 5 mm), the average number of lymph nodes removed in central compartment rose from 4.8 to 12.3 (range, 11–13). At the 2-month follow-up evaluation, all the patients were in excellent condition and highly satisfied with their cosmetic outcome. The calcitonin levels were undetectable for all six patients who had a follow-up period longer than 1 year.
Discussion
The minimum surgical operation for RET gene mutation carriers [4, 7, 10, 16, 17] who already present positive pentagastrin stimulation test results is a total thyroidectomy and a central compartment node clearance. For a long time, this prevented endocrine surgeons from operating on these patients with minimally invasive procedures despite the generally small size of the involved thyroids. The main concern was the difficulty of performing an accurate lymphadenectomy at this level [5].
The excellent results obtained by several authors [2, 9, 14] as evidenced by the number of removed lymph nodes in both the central and lateral neck compartments when surgery was performed via minimally invasive approaches convinced us to go ahead with our experience. During the past year, it was proposed that all patients selected for prophylactic thyroidectomy and central compartment clearance should undergo surgery via a video-assisted procedure. All gave their consent after careful presentation of information about the adopted technique and the possible risks. The most feared complication associated with central compartment lymphadenectomy is hypoparathyroidism [3]. Actually, in our preliminary report [14], we had to describe a transient hypocalcemic crisis with two patients. Both patients fully recovered in 3 weeks, showing normal calcium and parathormone levels.
As a consequence, the lymphatic dissection involved an attempt to preserve the inferior parathyroid blood supply by performance of a blunt dissection and avoidance of ligatures. The Harmonic Scalpel was used only during the last step of the procedure to divide the fat and the lymphatic tissue from the trachea. The use of this device, according to some authors, supposedly reduces hypoparathyroidism [12]. In the current series, the result seemed to be satisfactory in terms of hypoparathyroidism incidence. The incidence of the two main postoperative complications involved with thyroid surgery did not differ from that of the main series dealing with prophylactic standard thyroidectomy [4, 7, 10, 16, 17]. In particular, minimally invasive video-assisted thyroidectomy proved not to put the recurrent nerve in any jeopardy, as demonstrated in other previous reports [14].
The postoperative course was completely uneventful (no lymph spillage or neck hematoma was registered), and the use of drainage was never required, allowing a 24-h surgery for all patients. Despite the short follow-up period (8–44 months), the results in terms of postoperative calcitonin are very encouraging. In fact, this highly sensitive marker [11] for medullary carcinoma was undetectable in all cases, and this is the best proof that a satisfactory result was fully reached, at least in terms of procedure completeness at the neck level,. Of course, it still is too early for conclusions to be drawn about possible recurrences because it is well known that they can occur even in the presence of a negative calcitonin after the first surgery [6].
The satisfaction of patients with their scar was very high, thus confirming that the minimally invasive operation proposed to this group of patients might convince them to be more willing to undergo surgery even before their pentagastrin test shows positive results. Besides, the less painful course, as already demonstrated in several prospective studies [1, 8, 13], can constitute a further advantage of the minimally invasive approach for these patients, although its impact is certainly less important and more difficult to demonstrate with respect to the cosmetic outcome.
References
Bellantone R, Lombardi CP, Bossola M, Boscherini M, De Crea C, Alesina PF, Traini E (2002) Video-assisted vs conventional thyroid lobectomy: a randomized trial. Arch Surg 137: 301–304
Bellantone R, Lombardi CP, Raffaelli M, Boscherini M, Alesina PF, Princi P (2002) Central neck lymph node removal during minimally invasive video-assisted thyroidectomy for thyroid carcinoma: a feasible and safe procedure. J Laparoendosc Adv Surg Tech A 12: 181–185
Cheah WK, Arici C, Ituarte PH, Siperstein AE, Duh QY, Clark OH (2002) Complications of neck dissection for thyroid cancer. World J Surg 26: 1013–1016
Dralle H, Gimm O, Simon D, Frank-Raue K, Gortz G, Niederle B, Wahl RA, Kocm B, Walgenbach S, Hampel R, Ritter MM, Spelsberg F, Heiss A, Hinze R, Hoppner W (1998) Prophylactic thyroidectomy in 75 children and adolescents with hereditary medullary thyroid carcinoma: German and Austrian experience. World J Surg 22: 744–751
Duh QY (2003) Presidential address: minimally invasive endocrine surgery: standard of treatment or hype? Surgery 134: 849–857
Franc S, Piccoli-Sire P, Cohen R, Bardet S, Maes B, Murat A, Krivitzky A, Modigliani E (2001) Complete surgical lymph node resection does not prevent authentic recurrences of medullary thyroid carcinoma. Clin Endocrinol 55: 403–409
Frilling A, Dralle H, Eng C, Raue F, Broelsch CE (1995) Presymptomatic DNA screening in families with multiple endocrine neoplasia type 2 and familial medullary thyroid carcinoma. Surgery 118: 1099–1104
Ikeda Y, Takami H, Sasaki Y, Takayama J, Niimi M, Kan S (2002) Comparative studies of thyroidectomies: endoscopic surgery vs conventional open surgery. Surg Endosc 16: 1741–1745
Kitagawa W, Shimizu K, Akashu H, Tanaka S (2003) Endoscopic neck surgery with lymph node dissection for papillary carcinoma of the thyroid using a totally gasless anterior neck skin lifting method. J Am Coll Surg 196: 990–994
Lips CJM, Landsvater RM, Hoppener JWM, et al. (1994) Clinical screening is compared with DNA anlysis in families with multiple endocrine neoplasia type 2A. N Engl J Med 331: 828–835
Machens A, Schneyer U, Holzhausen HJ, Dralle H (2005) Prospects of remission in medullary thyroid carcinoma according to basal calcitonin level. J Clin Endocrinol Metab 904: 2029–2034
Meurisse M, Defechereux T, Maweja S, Degauque C, Vandelaer M, Hamoir E (2000) Evaluation of the Ultracision ultrasonic dissector in thyroid surgery: prospective randomized study. Ann Chir 125: 468–472
Miccoli P, Berti P, Raffaelli M, Materazzi G, Baldacci S, Rossi G (2001) Comparison betweem minimally invasive video-assisted thyroidectomy and conventional thyroidectomy: a prospective randomized study. Surgery 130(6): 1039–1043
Miccoli P, Elisei R, Berti P, Materazzi G, Agate L, Castagna MG, Cosci B, Faviana P, Ugolini C, Pinchera A (2004) Video-assisted prophylactic thyroidectomy and central compartment nodes clearance in two RET gene mutation adult carriers. J Endocrinol Invest 27: 557–561
Miccoli P, Materazzi G (2004) Minimally invasive video-assisted thyroidectomy (MIVAT). Surg Clin North Am 84: 735–741
Pacini F, Romei C, Miccoli P, Elisei R, Mocinaro E, Mancusi F, Iacconi P, Basolo F, Martino E, Pinchera A (1995) Early treatment of hereditary medullary thyroid carcinoma after attribution of multiple endocrine neoplas type 2 gene carrier status by screening for “RET” gene mutations. Surgery 118: 1031–1035
Wells SA, Chi DD, Toshima K, et al. (1994) Predictive DNA testing and prophylactic thyroidectomy in patients at risk for multiple endocrine neoplasia type 2A. Ann Surg 22: 237–250
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miccoli, P., Elisei, R., Donatini, G. et al. Video-assisted central compartment lymphadenectomy in a patient with a positive RET oncogene: initial experience. Surg Endosc 21, 120–123 (2007). https://doi.org/10.1007/s00464-005-0642-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-005-0642-3