Abstract
Aim
To see whether prophylactic central compartment dissection is recommended for advanced papillary thyroid cancer or as part of selective neck node dissection. Central compartment dissection is a technically demanding surgical procedure and carries a higher incidence of complications. The present retrospective case-control study analysed the impact of prophylactic central compartment dissection on the long-term outcome of advanced (N0-T3/T4) papillary thyroid cancer.
Materials and methods
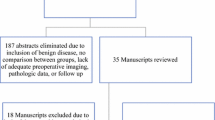
Case records of patients operated on for papillary thyroid cancer from 2005 to 2010 were reviewed and patients with Tumour stage 3–4 and N0 nodal status were included in the study. The institutional protocol was to perform total thyroidectomy with central compartment dissection during the early phase of the study period (2005 to 2008) but this strategy was shifted to total thyroidectomy alone during the latter phase. Fifty-five patients were included in the study and 29 of the cohort had total thyroidectomy with prophylactic central compartment dissection as the primary surgery and the remaining 26 had a total thyroidectomy as the primary surgical procedure.
Result
Patients were followed up for a median duration of 115 months and found to have no significant difference in the incidences of loco-regional recurrences between the groups. (n:4 (14%) Vs n: 3 (12%) p = .463). The disease-free survival and overall survival were not significantly different in the groups. There was a trend to an increase in the incidence of permanent hypoparathyroidism in patients who had central compartment dissection.
Conclusion
Prophylactic central compartment dissection did not influence the 10-year outcome of advanced node-negative papillary thyroid cancers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prophylactic lymph node dissection is performed for cancer having a high predilection for lymphatic spread and the procedure removes possible metastatic lymph nodes and helps to stage cancer accurately. The primary mode of spread of papillary thyroid cancer is through lymphatic channels and the first station of spread is the central compartment [1, 2]. Prophylactic central compartment dissection (PCCD) was the routine primary surgical treatment for papillary thyroid cancer (PTC) [3]. The central compartment houses many vital structures, so dissection is technically demanding. Unintentional injuries in these structures cause long-lasting morbidity [4]. Contrarily, recurrences in the central compartment shall infiltrate the laryngeal nerves, larynx, and trachea resulting in devastating morbidity. Reviews had shown a decreased incidence of recurrences among patients who had PCCD [5]. However, this advantage was not significant in low-risk PTC and the routine practice of PCCD was discontinued and recommended only for selective situations [6].
Updated American Thyroid Association guidelines recommend PCCD for T3/T4 tumours, as part of modified radical neck dissection (MRND), and when the information helps to plan treatment [7]. The strong recommendation was supported by moderate evidence. Similar recommendations are seen in other practice guidelines [8, 9]. The majority of subjects in studies related to PCCD had T1 or T2 tumours [10, 11] and the impact of the procedure on the long-term outcome of the node-negative T3/T4 PTC was not explored. Node-negative advanced PTC is rare and the surgical procedure is technically challenging even for a trained high-volume surgeon.
The present retrospective cohort study was designed to analyse the long-term effect of PCCD on N0- PTC with T3/T4 tumours. We hypothesised that PCCD independently would not positively influence disease-free survival of N0 papillary thyroid cancer with T3/T4 tumours.
Materials and methods
Case records of patients operated on the confirmed cytological diagnosis of papillary thyroid carcinoma from 2005 to 2010 were reviewed. Patients reporting for thyroid nodules had complete clinical examination, thyroid function studies (Free T4 & TSH) and neck ultrasound. The aspiration for cytology from thyroid nodules and suspicious lymph nodes was done under ultrasound guidance. The cytological study was based on the guidelines from the Papanicolaou Society (1996) [12]. Those patients who had concurrent sonological, cytological or frozen section diagnoses of lymph node metastasis in the central compartment and deep cervical chain were excluded. The final histology was reviewed and the tumour stage was graded based on the AJCC staging manual 8th edition and patients who had T3/T4 tumours included in the study [13].
The primary surgery for clinically N0 PTC patients was total thyroidectomy and PCCD during the initial phase of the study period (2005 to 2008) but during the latter phase (2008–2010) the primary surgery was total thyroidectomy alone. Laryngeal examination for assessment of the vocal cords was done preoperatively and postoperatively.
The external division of superior laryngeal nerves (EBSLN), parathyroid, and recurrent laryngeal nerves (RLN) were identified. The RLN was dissected to the level of innominate veins and the lymph nodes with the soft tissue were harvested from the pre-laryngeal, perithyroidal, pre-tracheal and paratracheal stations preserving intact parathyroid glands. Clinically suspicious lymph nodes seen during the operation were sent for frozen section studies. When parathyroid glands showed evidence of ischaemia auto-transplantation was done in the sternomastoid muscle.
Patients who had vocal cord dysfunction were reviewed monthly for 6 months and if the normality was not regained, they were considered to have permanent palsy. Serum albumin-corrected calcium was estimated every day at 6 am during the immediate postoperative period and serum level < 8.5 mg/dl was considered hypocalcaemia. Patients who had hypocalcaemia were reviewed monthly for 6 months and those with persistent hypocalcaemia were considered to have permanent hypocalcaemia.
All patients had a 5mCi whole-body scan 3 weeks after operation when TSH was noted above 25uIU/ml. Radioiodine ablation was done 3 to 4 weeks after the primary operation and the TSH suppression regimen was followed based on the ATA protocol (2006) [3].
The patients were reviewed at 6 monthly intervals for 3 years and all those found cured were scheduled for yearly visits. Others remained on 6 monthly reviews or as required based on individual cases. Stimulated thyroglobulin (Tg) and thyroglobulin antibodies (TgAbs) were estimated during the first 3 visits and later changed to unstimulated values if the serum levels remained persistently below 10 ng/ml. A neck ultrasound was done routinely and an I 131 scintigraphy / FDG PET scan was done in selected patients.
Data Collection
Demographic features: (Age and sex); Tumour-related features: (Size of the tumour, multifocality, vascular invasion, extra-thyroid invasion.); Details of treatment: (type of primary surgical procedure, amount of radioiodine received, presence of incidental locoregional and distant metastases on whole body scan, details of additional surgical procedures, details of additional radioiodine treatment.)
Outcome: The endpoint of the study was the condition of the patient during the last visit in 2021 which was assessed based on the characteristics defined in ATA guidelines [4].
1, Excellent response: Suppressed Tg < 0.2ng/ml, Neck ultrasound showed no abnormal features.2. Biochemical incomplete response: The stimulated Tg is > 10 ng/ml (suppressed 1 ng/ml), I131 WBS and Neck ultrasound did not reveal any abnormality. 3. Structural incomplete response: Patients with proven local or distant metastases. 4. Indeterminate response: Suspicious biochemical or imaging features that cannot be classified as benign or metastases.
For analysis, patients are grouped into one with the excellent response (No evidence of Disease –NED) and the others with the undesirable response (U E) which included disease-specific mortality, biochemical incomplete response, structural incomplete response, and indeterminate response.
Details of the cause of death of patients who expired during the follow-up period were reviewed. The PTC disease status at the time of death is carried forward for further analysis. The last observational variable carried forward method was used to fill in the missing data at random.
Statistics
The cohort was divided into the PCCD group (Total Thyroidectomy with prophylactic central compartment dissection) and the TT group (Total Thyroidectomy alone). Group-to-group analysis was done to identify the prevalence of excellent responses in the groups. Cross-tabulations were done to describe the association between the demographic features, tumour-related features, and type of surgical treatment to find an association with the outcome employing the Chi-square test (p = .05). SPSS 17.0 was used for statistical calculations.
Results
We analysed data from 312 patients and 55 eligible patients with a mean age of 44.11 years (SD 16.097; median 41) were included in the study. The study cohort included 20 males (36.4%) and 35 (63.6%) females. The mean tumour size was 46.58 mm (sd:21.316) 41 showed a classic variant of PTC, 13 had infiltrating follicular variants and one had a columnar cell variant.
The PCCD group included 29 (52.7%) patients and the TT group 26 (47.3%) patients. The demographic and pathologic features of the groups are shown in Table 1. The median duration of follow-up was 132 months (120–172) (Table 1).
The mean number of lymph nodes harvested was 8.59 [5,6,7,8,9,10,11,12,13,14] and incidental metastases were noted in 15 (51.7%). The size of metastases ranged from 1 to 4 mm (mean 2.34 mm) and the deposits were confined to lymph nodes. The lymph node ratio (LNR) ranged from 0 to 0.91.
Postoperative management: All patients received postoperative remnant I131 ablation 3 to 4 weeks after thyroidectomy (40 mCi to 100 mCi). The post-therapy whole body scan (WBS) showed evidence of incidental loco-regional metastases in 21 patients and incidental distant metastases in 2 patients. (Osseous-1, pulmonary-1). Incidental lateral neck metastases were seen in 10 (33%) patients of the PCCD group and 11 (44%) of the TT group. One patient in the PCCD group had incidental pulmonary metastasis and one patient in the TT group had incidental osseous (femoral head) and isolated pulmonary metastasis.
A total of 8 patients needed additional surgical procedures during the study period, which included modified neck dissection [6], excision of soft tissue recurrences [1], tracheal resection [1], and tracheostomy [1] (Table 2).
Of the cohort, 7 patients had loco-regional recurrences (soft tissue and lymph nodes), two developed distant metastases during the follow-up period and one patient in each group died of cancer. Incidences of loco-regional recurrences were not significantly different between the PCCD and the TT groups (n:4 (14%) Vs n: 3 (12%) p = .463).
The overall survival (OS) and disease-free survival (DFS) were 94.5% (n:52) and 87.3% (n: 48) respectively. The OS and DFS did not vary significantly between the PCCD group and the TT group. Details related to the outcomes and the status of the disease at the end of the study are noted in Table 3 and Table 4 respectively (Table 3 and 4)
Postoperative complications: Eleven patients (37.9%) of the PCCD group and 4 patients (15.3%) of the TT group had transient hypocalcaemia (p = .069). Two patients (6.8%) in the PCCD group and none in the TT group had permanent hypocalcaemia (p = .086). One patient in the PCCD group had temporary right vocal cord palsy which was found to recover during the review after a month of the operation.
Discussion
Approximately 50% of N0 patients undergoing PCCD had occult metastases [14] and the lymph node positivity was high among T3/T4 patients but a linear association was not always seen [15]. The present study cohort showed 51.7% positivity among those who underwent PCCD and the metastatic foci were confined to the lymph nodes and size ranging from 1 to 4 mm.
The micro-metastasis was defined as a focus less than 2 mm in size, and this delineation was postulated from studies of biologically aggressive malignancies like breast and lung cancer [16]. Lee YM et al. [17] suggested a revision of the size definition of micro-metastasis to 3.5 mm considering the different biological behaviour of PTC. The metastatic foci of the patients of the present study group were less than 3.5 mm except for that of one patient.
In the majority of instances, PCCD yielded lymph nodes with micro-metastases and the impact of such deposits in altering the outcome of PTC was not been substantially proven [18]. . The lymph node ratio was well known to influence the outcome of PTC. Chang et al. [19] observed that LNR modified with the inclusion of micro-metastases was less accurate in predicting local recurrence than LNR calculated otherwise. So micro-metastases in lymph nodes are unlikely to exert influences on the outcome of PTC.
The regional recurrences of PTC are of two types; lymph node metastases and soft tissue recurrences [18]. The majority of local recurrences are found in regional nodes and could be considered as a natural sequel in the course of cancer. However soft tissue recurrences have more serious consequences and indicate a biological aggressive behaviour. We did not find a significant difference in the rate of regional recurrences of both types in the two groups.
Systematic reviews have recorded significant risk reduction for local recurrences associated with PCCD, however, the advantage could be due to the upstaging of the disease whereby patients become eligible for adjuvant radioiodine ablation [14].
Most of the studies had established higher rates of complications associated with PCCD [3, 19] and the study cohort had a trend to have a higher incidence of permanent hypocalcaemia. Preservation of intact vascularised inferior parathyroid is technically demanding since the tiny vessels from inferior thyroid arteries are at risk during the dissection of para-tracheal and pre-tracheal lymph nodes. There is a trend to increased incidence of hypocalcaemia in PCCD group of the present cohort though the surgical team performs 300 to 400 thyroidectomies annually.
Conclusion
Prophylactic central compartment dissection does not influence positively the long-term outcome of T3/T4 papillary thyroid cancer. There was a trend to increase the incidences of permanent hypocalcaemia in the PCCD group. Hence our study does not show any added advantage for prophylactic central compartment dissection, however systematic reviews have shown some added advantage in recurrence free survival.
References
Machens A, Hinze R, Thomusch O et al (2002) Pattern of nodal metastasis for primary and reoperative thyroid cancer. World J Surg 26:22–28
Wada N, Duh QY, Sugino K et al (2003) Lymph node metastasis from 259 papillary thyroid microcarcinomas: frequency, pattern of occurrence and recurrence, and optimal strategy for neck dissection. Ann Surg 237:399–407
Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Sherman SI, Tuttle RM (2006) The American Thyroid Association Guidelines Taskforce. Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 16:109–142
Giordano D, Valcavi R, Thompson GB, Pedroni C, Renna L, Gradoni P, Barbieri V (2012) Complications of central neck dissection in patients with papillary thyroid carcinoma: results of a study on 1087 patients and review of the literature. Thyroid. ;22(9):911-7. https://doi.org/10.1089/thy.2012.0011. Epub 2012 Jul 24. PMID: 22827494
Lang BH-H, Ng S-H, Lincoln LH, Lau BJ, Cowling KP, Wong, Yat Wan K A (2013) Systematic review and Meta-analysis of Prophylactic Central Neck dissection on short-term Locoregional recurrence in papillary thyroid Carcinoma after total thyroidectomy. Thyroid 23(9):1087–1098
American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer, Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Pacini F, Schlumberger M, Sherman SI, Steward DL, Tuttle RM (2009) Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. ;19(11):1167 – 214. doi: 10.1089/thy.2009.0110. Erratum in: Thyroid. 2010;20(8):942. Hauger, Bryan R [corrected to Haugen, Bryan R]. Erratum in: Thyroid. 2010;20(6):674-5. PMID: 19860577
Haugen BR, Alexander EK, Bible KC et al (2015) American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: the American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid; 26:1–133
Filetti S, Durante C, Hartl D et al (2019) ESMO Clinical Practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 30(12):1856–1883
Gallardo E, Medina J, Sánchez JC et al (2019) SEOM clinical guideline thyroid cancer. Clin Transl Oncol 22:223–235. https://doi.org/10.1007/s12094-019-02284-8
Gambardella C, Patrone R, Di Capua F et al (2019) The role of prophylactic central compartment lymph node dissection in elderly patients with differentiated thyroid cancer: a multicentric study. BMC Surg 18(Suppl 1):110. https://doi.org/10.1186/s12893-018-0433-0
Viola D, Materazzi G, Valerio L, Molinaro E, Agate L, Faviana P, Seccia V, Sensi E, Romei C, Piaggi P, Torregrossa L, Sellari-Franceschini S, Basolo F, Vitti P, Elisei R, Miccoli P (2015) Prophylactic Central Compartment Lymph Node Dissection in Papillary thyroid carcinoma: clinical implications derived from the first prospective randomized controlled single Institution Study, The Journal of Clinical Endocrinology & Metabolism, V:100, Issue 4, A, Pages 1316–1324
Guidelines of the Papanicolaou Society of Cytopathology for the Examination of Fine-Needle Aspiration Specimens from Thyroid Nodules (1996) The Papanicolaou Society of Cytopathology Task Force on standards of Practice. Mod Pathol 9(6):710–715
Amin MB, Edge S, Greene F, Byrd DR, Brookland RK et al (eds) (2017) American Joint Committee on Cancer. Thyroid - differentiated and Anaplastic Carcinoma. AJCC Cancer Staging Manual, 8th edn. Springer, New York, NY, pp 881–898
Hughes DT, Rosen JE, Evans DB, Grubbs E, Wang TS, Solórzano CC (2018) Prophylactic Central Compartment Neck dissection in papillary thyroid Cancer and effect on Locoregional recurrence. Ann Surg Oncol 25(9):2526–2534. https://doi.org/10.1245/s10434-018-6528-0Epub 2018 May 21. PMID: 29786126
Lang BH, Wong KP, Wan KY, Lo CY (2012) Impact of routine unilateral central neck dissection on preablative and postablative stimulated thyroglobulin levels after total thyroidectomy in papillary thyroid carcinoma. Ann Surg Oncol 19(1):60–67. https://doi.org/10.1245/s10434-011-1833-xEpub 2011 Jun 17. PMID: 21681379; PMCID: PMC3251780
Seigel RJ (1996) Surgical pathology of lymph nodes in cancer staging: routine and specialized techniques. Surg Oncol Clin Nth Am 5:25–31
Lee YM, Park JH, Cho JW, Hong SJ, Yoon JH (2019) The definition of lymph node micrometastases in pathologic N1a papillary thyroid carcinoma should be revised. Surgery 165(3):652–656. https://doi.org/10.1016/j.surg.2018.09.015
Cranshaw IM, Carnaille B (2008) Micrometastases in thyroid cancer. An important finding? Surg Oncol 17(3):253–258. https://doi.org/10.1016/j.suronc.2008.04.005
Chang YW, Kim HS, Jung SP, Kim HY, Lee JB, Bae JW, Son GS (2017) Significance of micrometastases in the calculation of the lymph node ratio for papillary thyroid cancer. Ann Surg Treat Res 92(3):117–122. https://doi.org/10.4174/astr.2017.92.3.117Epub 2017 Feb 24. PMID: 28289664; PMCID: PMC5344800
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
There are no financial or non-financial interests that are directly or indirectly related to the work submitted for publication.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Revathy, A., Sekhar, S.R., Gopalakrishnan Nair, C. et al. Prophylactic Central Compartment Dissection on the Long-Term Outcome of Advanced (N0-T3/T4) Papillary Thyroid Cancer. Indian J Otolaryngol Head Neck Surg 76, 3256–3260 (2024). https://doi.org/10.1007/s12070-024-04660-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-024-04660-5