Abstract
Background
It is recommended that most patients between 18-80 years old, who have had an endoscopic retrograde cholangiopancreatography (ERCP) for choledocholithiasis, should be offered cholecystecytomy. However, we were uncertain whether this was the correct advice for patients over 80.
Method
A retrospective case note analysis was performed on 81 patients over 80, who had had an ERCP for choledocholithiasis. The primary end points were further biliary symptoms, cholecystectomy, death from biliary independent causes, and those still alive without further biliary symptoms.
Results
The records of 81 patients (median age 87; range, 80-96 years) were analyzed. Of the patients, 11% experienced further biliary symptoms at a median time of 4.5 months [interquartile range (IQR), 2.25-8.5 months] from the ERCP; 6% received cholecystectomy; 61% were still alive with no further biliary symptoms at a median time of 17 months (IQR, 12.25-23.75 months) after ERCP; and 22% had died from biliary independent causes at a median time of 9 months after ERCP (IQR, 3-12 months).
Conclusion
Expectant treatment can be recommended in this group of patients. Those who do present with further biliary symptoms do so soon after ERCP. Therefore, we recommend follow-up for 12 months after ERCP, prior to discharge.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Endoscopic retrograde cholangiopancreatography (ERCP) is commonly employed in the management of choledocholithiasis. Following ERCP, the advice for expectant treatment or subsequent cholecystectomy appears to be variable and the decision to operate is often empirical. In a prospective, randomized, multicenter trial of 120 patients, between the ages of 18 and 80 years, 47% of the patients were reported to have experienced a further biliary event when managed expectantly after ERCP for bile duct stones [2]. However, other studies have indicated that only 4-12% of patients develop further biliary symptoms if managed expectantly after ERCP [5]. Other factors that have been demonstrated to predict the development of biliary events after ERCP include multiple small gallbladder stones, a nonpatent cystic duct, and young age [3].
The management of patients over the age of 80 years, who have had an ERCP for choledocholithiasis, is going to present an increasingly common management dilemma. Figures from the Government Actuary’s Department (http://www.gad.gov.uk) indicate that the population of those over 80 years is set to increase from 2.3 million in 1995 to 3.5 million in 2025. The life expectancy of a 65-year-old woman is 84 years and for an 80-year-old woman it is 89 years.
We therefore conducted a study to assess whether patients over the age of 80 years should be managed surgically or expectantly following an ERCP for bile duct stones.
Methods
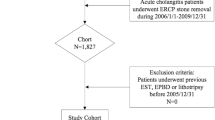
We conducted a retrospective case note study of all patients, over the age of 80 years, who had had an ERCP for choledocholithiasis within a single trust, over a 3-year period. There were four primary end points:
-
1.
Patients who were admitted to hospital with a further biliary event after ERCP. Biliary events were defined as biliary colic, cholecystitis, cholangitis, pancreatitis, obstructive jaundice, gallbladder perforation, and carcinoma of the gallbladder.
-
2.
A cholecystectomy.
-
3.
Those patients who were still alive and had not required hospital admission with further biliary symptoms.
-
4.
Those patients who had died from biliary independent causes.
We excluded any patients who had previously had a cholecystectomy. Complications of the ERCP itself were not recorded, since the aim of the study was to examine the outcome of the patients following their ERCP episode.
Statistical analysis was performed using version 10 of the statistical package for social sciences data base (SPSS), and a Mann-Whitney U test was applied to the data.
Results
A total of 81 patients fitted the study criteria, and the notes for all 81 patients were retrieved and analyzed. The patients had a median age of 87 years (range, 80-96 years). There was no difference in the age distribution for all four groups (Fig. 1). The median length of time from ERCP to one of the primary end points was 13 months (range, 1-41 months).
Nine of the 81 patients (11%) were admitted to hospital with further biliary symptoms after their ERCP. This occurred at a median time of 4.5 months (interquartile range [IQR], 2.25-8.5 months) after the ERCP. Of these nine patients, three had cholangitis, two had pancreatitis, two had cholecystitis, one had a perforated gallbladder, and one had a carcinoma of the gallbladder. The initial ERCPs were described as successful in all of these patients except one, who re-presented with cholangitis. Three of these patients subsequently died of their biliary disease. One of the patients with cholangitis died of pneumonia 19 days after admission. The patient with the perforated gallbladder died 5 days after admission and the patient with carcinoma of the gallbladder died of carcinomatosis.
Five of the 81 patients (6%) received a cholecystectomy. This was performed at a median time of 2 months (IQR, 2-3.5 months) after the ERCP. Four of these were laparoscopic procedures and one was an elective open procedure. There was one postoperative complication; a common bile duct stone 9 months after the operation. Of the patients, 49 of 81 (61%) were still alive with no further biliary symptoms after their ERCP at a median time of 17 months (IQR, 12.25-23.75 months); 22% (18/81) of the patients had died from biliary independent causes at a median time of 9 months (IQR, 3-12 months) after the ERCP. These data are summarized in Table 1.
The Mann-Whitney U test indicated that the time at presentation of further biliary symptoms (4.5 months) is significantly earlier (p < 0.01) than the median time at the end of the study when 61% of the patients are still alive with no further biliary symptoms (17 months). Similarly, those who died of biliary independent causes did so at a significantly earlier time (9 months) than those who were still alive without further biliary symptoms (17 months; p < 0.01) (Fig. 2).
In total, 83% (49/81 + 18/81) of the patients did not re-present with further biliary symptoms after their ERCP (Fig. 3).
Discussion
Our data demonstrated that 83% of the patients did not re-present with biliary symptoms after their ERCP. This indicates therefore that patients over 80 years can be managed expectantly after ERCP for bile duct stones. This conclusion was also reached in a prospective study by Arthur et al. [1]. They concluded that ERCP for the management of choledocholithiasis in patients over the age of 80 years might be the only intervention that is necessary in order to achieve an asymptomatic state.
While recommending expectant treatment, however, it is important to realize that three of the nine patients who experienced further biliary symptoms died as a result of their biliary disease. It could be argued that these deaths may have been avoided if cholecystectomy had been performed, particularly in the cases of the patient with cholangitis and the patient who developed a perforated gallbladder. Allied to the fact that there was only one late complication after five cholecystectomies, one could argue that surgical treatment should be given serious consideration. Hazan et al. have demonstrated that cholecystectomy is safe in octogenarians [4]. Clearly, however, the associated comorbidity of the patient needs to be assessed carefully if surgical treatment is to be pursued.
We noted that patients who re-presented with biliary symptoms did so at a median time of 4.5 months (IQR 2.25-8.5 months) after their ERCP. They presented at a significantly earlier time than those patients who were still alive and free of biliary symptoms at the end of the study (17 months). Similarly, those who died of biliary independent causes did so at a median of 9 months (IQR, 3-12 months), which also was significantly earlier than those who were still alive without further biliary symptoms (17 months).
If a course of expectant treatment is to be followed, then a pragmatic approach may be to keep these patients under clinical review for 12 months. After this period it appears likely, from our data, that the patients will be in the category of those who are still alive with no further biliary symptoms.
Conclusion
Patients over the age of 80 years who have had an ERCP for bile duct stones can be managed expectantly. However, we would recommend clinical review for 12 months prior to discharge.
References
JDR Arthur PR Edward LS Chagla (2003) ArticleTitleManagement of gallstone disease in the elderly Ann R Coll Surg Engl 85 91–96 Occurrence Handle10.1308/003588403321219849 Occurrence Handle1:STN:280:DC%2BD3s3htlOisg%3D%3D Occurrence Handle12648337
D Boerma EAJ Rauws YCA Keulemans IMC Janssen CJM Bolwerk R Timmer EJ Boerma H Obertop K Huibregtse DJ Gouma (2002) ArticleTitleWait and see policy or laparoscopic cholecystectomy after endoscopic sphincterotomy for bile duct stones: a randomised trial Lancet 360 761–765 Occurrence Handle10.1016/S0140-6736(02)09896-3 Occurrence Handle12241833
LE Hammarstrom T Holmin H Stridbeck (1996) ArticleTitleEndoscopic treatment of bile duct calculi in patients with gallbladder in situ: long term outcome and factors predictive for recurrent symptoms Scand J Gastroenterol 31 294–301 Occurrence Handle1:STN:280:BymH3s%2Fitlc%3D Occurrence Handle8833361
D Hazzan N Geron D Golijanin P Reissman E Shiloni (2003) ArticleTitleLaparoscopic cholecystectomy in octogenarians Surg Endosc 17 773–776 Occurrence Handle10.1007/s00464-002-8529-z Occurrence Handle1:STN:280:DC%2BD3s3hsFGlsw%3D%3D Occurrence Handle12616388
KH Lai LF Lin GH Lo (1999) ArticleTitleDoes cholecystectomy after endoscopic sphincterotomy prevent the recurrence of biliary complications? GI Endosc 49 483–487 Occurrence Handle1:STN:280:DyaK1M3hvVWhug%3D%3D
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pring, C.M., Skelding-Millar, L. & Goodall, R.J.R. Expectant treatment or cholecystectomy after endoscopic retrograde cholangiopancreatography for choledocholithiasis in patients over 80 years old?. Surg Endosc 19, 357–360 (2005). https://doi.org/10.1007/s00464-004-9089-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-004-9089-1