Abstract
Background
This study aimed to characterize the clinical; features of intestinal malrotation in adults, and to compare the results for the open and laparoscopic Ladd procedures.
Methods
Between 1984 and 2003, 21 adult patients with a mean age of 36 years (range, 14–89 years) were surgically treated for intestinal malrotation. The clinical data collected included age, gender, presenting symptoms, diagnostic tests, type of operation, operative time, narcotic requirement, time to oral intake, length of hospital stay, and outcome. The groups (open vs laparoscopic) were comparatively analyzed using two-sample t-tests and Wilcoxon rank sum tests.
Results
The two groups were similar in terms of age, clinical presentation, and diagnostic tests performed. The most common presenting symptoms were chronic abdominal pain, nausea, and repeated vomiting. Upper gastrointestinal barium studies (UGI/SBFT) were diagnostic for all patients with malrotation as compared with computed tomography (CT) scanning, which was falsely negative in 25% of patients. A total of 21 patients underwent the Ladd procedure, either open (n = 10) or laparoscopic (n = 11). Three laparoscopic procedures were converted to open. Overall, the laparoscopic group resumed oral intake earlier than the open group (1.8 vs 2.7 days; p = 0.092), had a shorter hospital stay (4.0 vs. 6.1 days; p = 0.050), and required less intravenous narcotics on postoperative day 1 (4.9 vs 48.5 mg; p = 0.002). The laparoscopic group underwent a longer operation (194 vs 143 min; p = 0.053). Sixteen of eighteen patients available for follow-up reported complete resolution of symptoms, 2 felt greatly improved. No patient required a second operation related to volvulus or recurrent symptoms.
Conclusions
The laparoscopic Ladd procedure is feasible, safe, and as effective as the standard open Ladd procedure for the treatment of adults who have intestinal malrotation without midgut volvulus. Patients also benefit from this minimally invasive approach, as manifested by an earlier oral intake, a decreased need for intravenous narcotics, and an earlier discharge from the hospital.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Malrotation of the midgut occurs when the normal embryologic rotation and fixation process of the intestine fails to take place [7]. Four potential anomalies may occur: nonrotation, malrotation, reverse rotation, and paraduodenal hernia, with malrotation of the midgut being the most common (Table 1). Anatomic variation is common in patients with intestinal malrotation and may include an abnormally high position of the cecum and a narrow mesenteric pedicle, which can lead to midgut volvulus and intestinal ischemia. In the absence of volvulus, congenital adhesive bands (Ladd bands) may compress the duodenum and cause chronic obstruction [10].
Anomalies of intestinal rotation that occur during fetal development often are discovered in infants and children, but rarely in adults [14]. Indeed, most adult patients are asymptomatic and incidentally are discovered later in life at surgery for other conditions [8, 16]. However, some adults may present acutely with midgut volvulus and intestinal ischemia or chronically with symptoms of intermittent bowel obstruction or vague abdominal complaints. The diagnosis for adult patients therefore relies on a high degree of clinical suspicion that may be confirmed by appropriate radiologic studies [17].
Operative management of intestinal malrotation, the Ladd procedure, includes counterclockwise detorsion of the midgut volvulus (if present), division of the abnormal coloduodenal Ladd bands tethering the midgut and causing extrinsic compression, widening of the mesenteric base to prevent further volvulus, and removal of the malpositioned appendix [11].
Recently, laparoscopic techniques for treating malrotation in both infants [2, 18, 20] and adults [6, 12, 13, 19] have been described. The laparoscopic experience with adults has consisted primarily of isolated case reports. This retrospective study aimed to better characterize the clinical features of this rare disease state in a larger group of adults, and to compare open and laparoscopic surgical techniques to assess whether patients treated laparoscopically benefit from a minimally invasive approach while achieving comparable outcomes.
Materials and methods
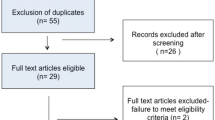
A retrospective analysis, approved by the Mayo Foundation Institutional Review Board, was performed for all adult patients (age, >13 years) who underwent a Ladd procedure for intestinal malrotation (with our without volvulus) at the Mayo Clinic between 1950 and 2003. A total of 48 patients were identified. To make a better comparison between the laparoscopic and open approaches, we elected to limit our analysis only to the adult patients treated between 1984 and 2003, the period during which we began using laparoscopy for the Ladd procedure. Moreover, we believed that routine postoperative care and hospital stays for open cases in the 1950s through 1970s would be too different from the laparoscopic cases from the more recent era.
For the period 1984 to 2003, 21 adult patients with a mean age of 36 years (range, 14–89 years) were identified. The patients were divided into two groups: those who had received a laparoscopic Ladd procedure (n = 11), and those who had undergone conventional open Ladd procedure via a midline or subcostal abdominal incision (n = 10). Whether a laparoscopic or open approach was used or not was left to the discretion of the operating surgeon. Laparoscopic procedures were performed through a 10-mm infraumbilical port and two or three 5-mm working ports as necessary. The operative times listed are for the entire duration of the operation, including surgical procedures performed in addition to the Ladd procedure. Data collected through chart review and telephone questionnaire included patient’s age, gender, clinical symptoms, diagnostic tests, operative time, type of operation, intravenous narcotic requirement on postoperative day 1, time to oral intake, length of hospital stay, and outcome.
In an effort to assess long-term outcome, telephone interviews focused on postoperative relief of symptoms and the need for further surgical intervention or dietary modifications. Exclusion criteria specified abdominal reoperations for patients who previously had undergone a Ladd procedure and patients with malrotation who did not receive a Ladd procedure. Three patients in the laparoscopic group underwent conversion to an open procedure, but were analyzed in the laparoscopic group for intent-to-treat purposes.
Statistical analysis
Summary statistics are presented as mean ± standard derivation. Comparison between the study cohorts used two-sample t-tests when the data were approximately Gaussian, and Wilcoxon rank sum tests when the data were not sufficiently Gaussian. All statistical tests were two-sided, and the threshold of statistical significance was set at an alpha of 0.05. All analyses were conducted using SAS version 8.2 (SAS Institute Cary, NC, USA).
Results
The male to female ratio and the mean age, were similar in the two groups (Table 2). The most common presenting symptoms in both groups were chronic abdominal pain, nausea, and repeated vomiting. Acute abdominal pain was experienced by all five patients who presented with midgut volvulus. Other symptoms such as chronic diarrhea, constipation, early satiety, bloating, and gastroesophageal reflux disease (GERD) were uncommon (Table 3).
Upper gastrointestinal barium studies were diagnostic for all 16 patients in whom it was performed. Computed tomography scanning of the abdomen was positive for intestinal malrotation in 9 of 12 patients, but falsely negative in 3 of 12 patients. Other tests, such as barium enema, abdominal ultrasound, colonoscopy, esophagogastroduodenoscopy, and plain radiographs were of limited clinical value (Table 4). Diagnostic laparoscopy was not performed for any patient in our series.
All the patients who presented with midgut volvulus underwent an open Ladd procedure. The mean operative times were similar in the laparoscopic (194 min) and open (143 min) groups (p = 0.053) (Table 5). The laparoscopic group experienced a shorter time to oral intake (1.8 days vs 2.7 days; p = 0.092), a shorter hospital stay (4 vs 6 days; p = 0. 050), and less intravenous narcotic use on postoperative day 1 (4.9 vs. 48.5 mg; p = 0.002). Conversion from laparoscopic to open technique was necessary in three patients for technically difficult dissection (n = 1), inability to visualize structure clearly (n = 1), and intraoperative findings necessitating a change in the planned operative procedure (n = 1).
The follow-up period ranged from 2 weeks to 97 months (mean, 42 months) and was complete for 18 (86%) of 21 patients. Of the 21 patients, 16 commented that they had complete resolution of their symptoms after the operation and had not required any dietary modifications. The remaining two patients (one laparoscopic and one open) rated their symptoms as “greatly improved,” but required some modifications to their diet. No patients required a repeat operation for symptoms or volvulus. The 30-day mortality was zero for both groups.
Discussion
Intestinal malrotation is diagnosed in the first month after birth for the great majority of patients. The incidence of malrotation in adulthood is 0.2% [6, 13]. Unlike the pediatric population, most adult patients with malrotation lack other congenital anomalies and are free of symptoms related to their malrotated bowel. The adult minority that does have symptoms typically present with a prolonged history of abdominal complaints suggestive of obstruction. The most common symptoms found in our patients were chronic abdominal pain, nausea, repeated vomiting, and early satiety, all suggestive of an obstructive intestinal process. The diagnosis often is delayed, which leads clinicians and patients to attribute symptoms to the wrong diagnosis. All too often, such patients undergo numerous investigational tests and carry diagnostic labels such as irritable bowel syndrome, peptic ulcer disease, or psychogenic disorder.
Our patients were no different in this regard and had undergone a myriad of tests before the diagnosis was secured. In our hands, the most accurate diagnostic test to confirm malrotation was the upper gastrointestinal study with small bowel followthrough (UGI/SBFT), which may demonstrate a dilated duodenum, a right-sided duodenojejunal junction, and a duodenum failing to cross the midline or ascend to the level of the pylorus (Fig. 1). An unusual UGI/SBFT finding in one of our patients was the presence of a “cocoon deformity,” in which the small bowel was encased in a filmy peritoneal sac (Fig. 2), resulting in a chronic low-grade obstruction.
Several papers in the literature have reported that computed tomography (CT) scanning for patients with intestinal malrotation can be helpful to identify an abnormally positioned superior mesenteric vein lying anterior to or to the left of the superior mesenteric artery [3, 5, 9, 15]. For a patient with midgut volvulus, a characteristic “whirlpool sign” is seen on CT scan indicating mesenteric rotation around a narrow-based pedicle [21] (Fig. 3). In our series of patients who underwent CT scans, 25% were falsely negative.
For adult patients, the Ladd procedure is the standard of care for resolving symptoms and preventing future complications. For our patients, the Ladd procedure was highly efficacious in that it led to complete resolution of symptoms for 16 of the 18 patients available for follow-up and near complete resolution for the remaining 2 patients. We, like others, believe that the incidental discovery of malrotation in the adult patient is an indication for surgery because no reliable means exists to predict which asymptomatic patient will later experience complications [1].
Laparoscopy is now used for many surgical conditions. In some instances, such as laparoscopic cholecystectomy, it has become the standard of care replacing the conventional open approach. Our study, the largest series reported for adults, confirms that the laparoscopic Ladd procedure is safe, feasible, and effective for the management of adults with intestinal malrotation. Moreover, the benefits of minimally invasive surgery seen in our patients were early oral intake, less narcotic use, and a shortened hospital stay. We did not question our patients about the cosmetic results, but clearly, young patients will find this an added benefit [4].
Laparoscopy also may be helpful when the diagnosis of intestinal malrotation is uncertain. A method has been developed by Mazziotti et al. [13] to determine whether intraoperative Ladd procedure is feasible. According to these authors, if the length between the duodenojejunal junction and the ileocecal valve is less than half the transverse diameter of the peritoneal cavity, a formal laparoscopic Ladd procedure should be performed to prevent volvulus.
In summary, our data indicate that the laparoscopic Ladd procedure used for adults with intestinal malrotation is feasible, safe, and as effective as the open procedure for relief of symptoms and prevention of the catastrophic consequences associated with acute midgut volvulus. Moreover, additional benefits expected for a minimally invasive approach were observed.
References
Anonymous (1990) The presentation of malrotation of the intestine in adults. Ann R Coll Surg Engl 72: 412
Bass KD, Rothenberg SS, Chang JH (1998) Laparoscopic Ladd’s procedure in infants with Malrotation. J Pediatr Surg 33: 279–281
Berdon WE (1995) The diagnosis of malrotation and volvulus in the older child and adult: a trap for radiologists. Pediatr Radiol 25: 101–103
Dunker MS, Bemelman WA, Slors JF, van Duijvendijk P, Gouma DJ (2001) Functional outcome, quality of life, body image, and cosmesis in patients after laparoscopic-assisted and conventional restorative proctocolectomy. Dis Colon Rectum 44: 1800–1807
Fisher JK (1981) Computed tomographic diagnosis of volvulus in intestinal malrotation. Radiology 140: 145–146
Frantzides CT, Cziperle DJ, Soergel K, Stewart E (1996) Laparoscopic Ladd procedure and cecopexy in the treatment of malrotation beyond the neonatal period. Laparosc Endosc Percutan Tech 6: 73–75
Frazer TE, et al (1915) On the factors concerned in causing rotation of the intestine in man. J Anat Physiol 50: 75
Fukuya T, Brown BP, Lu CC (1993) Midgut volvulus as a complication of intestinal malrotation in adults. Dig Dis Sci 38: 438–444
Gaines PA, Saunders AJ, Drake D (1987) Midgut malrotation diagnosed by ultrasound. Clin Radiol 38: 51
Ladd WE (1932) Congenital obstruction of the duodenum in children. N Engl J Med 206: 273–283
Ladd WE (1936) Surgical diseases of the alimentary tract in infants. N Engl J Med 215: 705
Matzke GM, Moir CR, Dozois EJ (2003) Laparoscopic Ladd procedure for adult malrotation of the midgut with cocoon deformity. J Laparoendosco Adv Surg Tech 13: 327–329
Mazziotti MV, Strassberg SM, Langer JC (1997) August. Intestinal rotation abnormalities without volvulus: the role of laparoscopy. J Am Coll Surg 185: 172–176
Powell DM, Othersen H, Smith CD (1989) Malrotation of the intestines in children: the effect of Age on presentation and therapy. J Pediatr Surg 24: 777–780
Shatzkes D, Gordon DH, Haller JO, Kantor A, De Silva R (1990) Malrotation of the bowel: malalignment of the superior mesenteric artery–vein complex shown by CT and MR. J. Comput Assist Tomogr 14: 93
Spigland N, Brandt ML, Yazbeck S (1990) Malrotation presenting beyond the neonatal period. J. Pediatr Surg 25:1139–1142
von Flue M, Herzog U, Ackermann C, Tondelli P, Harder F (1994) Acute and chronic presentation of intestinal nonrotation in adults. Dis Colon Rectum 37: 192–198
Waldhausen JH, Sawin RS (1996) Laparoscopic Ladd’s Procedure and assessment of malrotation. J Laparoendosc Surg 6(Suppl 1): S103–S105
Yahata H, Uchida K, Haruta N, Oshita A, Takiguchi T, Tanji H, Shinozaki K, Okimoto T, Marubayashi S, Asahara T, Fukada Y, Dohi K (1997) A case report of midgut nonrotation treated by laparoscopic Ladd procedure. Surg Laparosc Endosc Precutan Tech 7:177–178
Yamashita H, Kato H, Uyama S, Kanata T, Nishizawa F, Kotegawa H, Watanabe T, Kuhara T (1999) Laparoscopic repair of intestinal malrotation complicated by midgut volvulus. Surg Endosc. 13: 1160–1162
Yeh WC, Wang HP, Chen C, Wang HH, Wu MS, Lin JT (1999) Preoperative sonographic diagnosis of midgut malrotation with volvulus in adults: the “whirlpool sign”. J Clin Ultrasound 27: 279–283
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Matzke, G.M., Dozois, E.J., Larson, D.W. et al. Surgical management of intestinal malrotation in adults: comparative results for open and laparoscopic Ladd procedures. Surg Endosc 19, 1416–1419 (2005). https://doi.org/10.1007/s00464-004-8249-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-004-8249-7