Abstract
Purpose
Although the principles of the Ladd’s procedure for intestinal malrotation in children have remained unchanged since its first description, in the era of minimally invasive surgery it is controversial whether laparoscopy is advantageous over open surgery. The aim of our study was to determine whether the surgical approach for the treatment of malrotation had an impact on patient outcome.
Methods
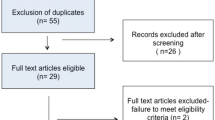
Using a defined strategy (PubMed, Cochrane, Embase and Web of Science MeSH headings), two investigators independently searched for studies comparing open versus laparoscopic Ladd’s procedure in children. Case reports and opinion articles were excluded. Outcome measures included age at operation, time to full enteral feeding, length of hospital stay, and post-operative complications. Maneuvers were compared using Fisher’s exact test and meta-analysis was conducted using RevMan 5.3. Data are expressed as mean ± SD.
Results
Of 308 abstracts screened, 49 full-text articles were analyzed and nine (all retrospective) met our search criteria. Selected articles included 1003 patients, of whom 744 (74 %) underwent open surgery and 259 (26 %) laparoscopy. Patients who had open surgery were younger (0.9 ± 1.2 years) than those who underwent laparoscopy (2.6 ± 3 years; p < 0.0001). Laparoscopy was converted to open Ladd’s in 25.3 % patients. Laparoscopy was associated with faster full enteral feeding (1.5 ± 0.3 days) in comparison to open surgery (4.6 ± 0.1 days, p < 0.0001). Length of hospital stay was shorter in the laparoscopic group (5.9 ± 4.3 days) than in the open group (11.2 ± 6.7 days; p < 0.0001). Open surgery was associated with higher overall post-operative complication rate (21 %) than laparoscopy (8 %; p < 0.0001). Although there was no difference in the prevalence of post-operative bowel obstruction (open, n = 10 %; laparoscopy, n = 0 % p = 0.07), post-operative volvulus was more frequent in the laparoscopy group (3.5 %) than in the open group (1.4 %, p = 0.04).
Conclusion
Comparative but non-randomized studies indicate that laparoscopic Ladd’s procedure is not commonly performed in young children. Although one third of laparoscopic procedures is converted to open surgery, laparoscopy is associated with shorter time to full enteral feeds and length of hospital stay. However, laparoscopic Ladd’s procedure seems to have higher incidence of post-operative volvulus. Prospective randomized studies with long follow-up are needed to confirm present outcome data and determine the safety and effectiveness of the laparoscopic approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intestinal malrotation is defined as the congenital abnormal positioning of the midgut, whereby the duodeno-jejunal flexure lies right of the midline and relatively close to the ileocecal valve [1–4]. This makes the dorsal mesenteric root narrow, and puts the bowel at risk of midgut volvulus. Intestinal malrotation is estimated to occur in between 1 in 200 and 1 in 500 live births [5–7].
All symptomatic patients with positive investigative findings should undergo surgical intervention [1, 8–10]. There is some controversy in the literature about the treatment of the asymptomatic or atypically symptomatic patients, in whom a rotational abnormality is found incidentally [11, 12].
The procedure to correct intestinal malrotation was first described by Ladd [13]. The principles of this surgery are the anticlockwise derotation of a volvulus if present, the division of the Ladd’s bands if present, the broadening of the mesenteric root and the positioning of the small bowel in the right quadrants of the abdomen and the large bowel in the left ones.
The laparoscopic approach for intestinal malrotation was first reported by van der Zee and Bax in 1995, and it has become more popular over the years [14]. The principles of this approach are the same of the open technique. Single institution retrospective studies indicated that the laparoscopic approach is safe for diagnosing and treating malrotation [15–20]. One of the reported advantages of laparoscopy is its potential to distinguish between true malrotation with a narrow mesenteric base, non-rotation and atypical malrotation with duodenal malposition [15]. Laparoscopy has been used mainly to repair malrotation in clinically stable patients, whereas the open approach has been preferred in patients with suspected midgut volvulus [21]. A systematic review from the American Pediatric Surgical Association reports that the laparoscopic approach to correct malrotation in children is feasible and safe (level 3–4 evidence, grade C recommendation), whereas there is minimal evidence to support the laparoscopic approach in neonates [12]. Moreover, in cases of known volvulus there have been no prospective studies to compare the open and laparoscopic approach to treat this condition.
The aim of our systematic review and meta-analysis was to determine whether the surgical approach, open or laparoscopic, had an impact on the outcome of infants and children with intestinal malrotation.
Materials and methods
Systematic review
A systematic review of the literature was made using a defined search strategy. Two investigators (VDC and GL) independently searched scientific databases (PubMed, Medline, Cochrane Collaboration, Embase and Web of Science) using a combination of keywords (Table 1). MeSH headings and terms used are “laparoscopic AND malrotation” and “laparoscopic AND Ladd”. Case reports and opinion articles were excluded from the review.
Only studies comparing open versus laparoscopic approach to treat intestinal malrotation in infants and children were included. Patients were divided into two groups according to the surgical approach (open or laparoscopic).
Outcome measures included patient demographics (gender, age and weight at surgery), indication to surgery, conversion rate, time to full feed, length of hospital stay, length of follow-up, post-operative complications including bowel obstruction, and post-operative volvulus. To reduce bias while assessing post-operative complications and post-operative volvulus, patients who initially underwent laparoscopic approach but required conversion to open Ladd’s procedure, were considered in the open group.
Meta-analysis
Data are expressed as mean ± SD. For the above mentioned outcomes, open and laparoscopic procedures were compared using RevMan 5.3. Incidence of presenting symptoms and post-operative complications were compared between the two groups using Fisher’s exact test. p < 0.05 was considered significant.
Results
Our search strategy yielded 309 studies. Forty-nine full-text articles were reviewed and nine of them met the inclusion criteria [19, 21–28] (Table 2). All included studies were published between 2000 and 2016. These nine articles included 1003 patients, of whom 744 (74 %) underwent open surgery and 259 (26 %) laparoscopic approach. The gender was reported in four studies (n = 575 patients), with a slight male preponderance (57 %, n = 327).
The age at surgery was reported for both groups in six studies (n = 690 patients) accounting for a population of 690 patients [19, 23–27]. In this population, we observed that patients who had open surgery were younger (0.9 ± 1.2 years) than those who underwent laparoscopic Ladd’s procedure (2.6 ± 3 years, p < 0.0001). This overall difference was confirmed when we analyzed the prevalence of open and laparoscopic Ladd’s procedure in neonates (<30 days), as reported in two studies (n = 105 patients). In fact, laparoscopy was less commonly performed in these patients (n = 9, 8.5 %), in comparison to open Ladd’s (n = 96, 91.5 %, p < 0.0001).
Data on the weight at surgery were specifically reported in three studies for an overall population on 466 patients [19, 23, 26]. The mean weight was greater in the laparoscopic group (21.3 ± 5.2 kg), than in the open group (8.4 ± 3 kg, p < 0.0001).
Four studies (open surgery n = 207, 66 %; laparoscopy n = 96, 34 %) reported information on patient clinical presentation [23, 24, 26, 27]. The proportion of asymptomatic patients in the open surgery group (n = 48, 23 %) was similar to that in the laparoscopic group (n = 14, 17 %).
In comparison to patients who underwent open Ladd’s procedure, those who had laparoscopy were more frequently suffering from aspecific symptoms such as feeding intolerance (34 versus 13 %, p = 0.012), and intermittent abdominal pain (32 versus 10 %, p = 0.004). Conversely, patients who had open Ladd’s were more likely to have a pre-operative suspected volvulus (n = 166, 77 %) compared to those who had a laparoscopic Ladd’s (n = 49, 23 %; p < 0.001) [24, 27].
The overall conversion rate was outlined in six studies (n = 760). Of the 190 patients, who had laparoscopic Ladd’s, the conversion rate to open surgery was 25 % (n = 48) [19, 21, 23, 24, 26, 27]. The most common indications for converting to open surgery were inadequate view (40 %), technical problems (10 %) and impossibility to reduce midgut volvulus (4 %) (Table 3). However, in 29 % (n = 14) of patients the indication to conversion was not reported.
The time to full enteral feed was reported in 322 patients (open surgery, n = 261, 81 %; laparoscopy, n = 61, 19 %) [19, 27]. Laparoscopy was associated with an earlier full enteral feed (1.5 ± 0.3 days) in comparison to open surgery (4.6 ± 0.1 days, p < 0.0001; Fig. 1a).
The length of hospital stay was compared in two studies (open surgery, n = 291, 79 %; laparoscopy, n = 76, 21 %) and it was shorter in the laparoscopic group (5.9 ± 4.3 days) than in the open group (11.2 ± 6.7 days; p < 0.0001; Fig. 1b) [19, 24]. Data on length of follow-up were available for comparison in three studies [19, 23, 27] (open = 284, 83.5 %; laparoscopy = 56, 16.5 %) and showed no difference between the open group (43.8 ± 28 months) and the laparoscopic group (29.5 ± 3.8; p = ns).
Six studies reported post-operative complications in 690 patients (open n = 502, 73 %; laparoscopy n = 188, 27 %) [19, 23–27]. Open surgery was associated with higher overall post-operative complication rate (n = 109, 22 %) in comparison to laparoscopy (n = 13, 7 %; p < 0.0001) (Fig. 2a). Moreover, surgical wound infection was described only in patients treated with the open approach (n = 14, 3 %; p = 0.015). The rate of hospital readmission was higher for patients who underwent open Ladd’s procedure (n = 33, 6.5 %), compared to those who had laparoscopy (n = 4, 2 %, p = 0.021).
Six studies reported data about post-operative adhesive small bowel obstruction (n = 367, open surgery n = 207, 79 %; laparoscopy n = 96, 21 %) [23, 24, 26, 27]. Post-operative bowel obstruction was developed by 22 patients (10 %), who had open Ladd’s, and not reported for patients who had laparoscopic Ladd’s (0 %; p = 0.07).
Conversely, the incidence of post-operative volvulus, reported in five studies (open n = 482, 74 %; laparoscopy n = 170, 26 %) was higher in the laparoscopy group (n = 5, 3.5 %) than in the open group n = 7, 1.4 %, p = 0.04) [19, 23–26] (Fig. 2b).
Discussion
The present study shows that there is a lack of evidence in the literature to support either open or laparoscopic Ladd’s procedure in infants and children with intestinal malrotation. In fact, according to our research, there is a paucity of comparative studies, none of which was prospective. This could be explained partially by the relatively recent introduction and popularization of laparoscopy for this condition, and partially by the heterogeneity of patient presentation. The higher post-operative volvulus in the laparoscopic group is worrisome and requires further prospective evaluation.
The laparoscopic Ladd’s procedure has gained more interest in the last years thanks to its feasibility, fast post-operative course and low rate of long-term morbidity [1, 17, 18]. However, our study shows that the open technique is still more commonly employed to correct intestinal malrotation in infants and children. This could be due to the fact that a big proportion of cases of intestinal malrotation are diagnosed in neonates, where there are still controversies with regards to the safety of the laparoscopic approach [12, 16, 28]. In fact, patients who had open surgery were younger and smaller than those who underwent laparoscopy. The preponderance of open Ladd’s in neonates and children is not only because of the size of the patient but also because of the higher rate of suspected volvulus in these patients.
In our study, 20 % of patients were asymptomatic at the time of surgery, with an incidental radiological diagnosis of intestinal malrotation [23, 24, 26, 27]. We did not find a difference between the two groups of patients. Laparoscopy has the advantage to confirm the presence of intestinal malrotation, the mobility of the colon and the width of the mesentery in a less invasive manner [12]. Therefore, it could be adopted as first line treatment in these children with equivocal diagnosis.
Among the symptomatic patients, without a volvulus, those who suffer from aspecific symptoms were more commonly treated with laparoscopy. This is in line with the tendency of using laparoscopy in older children who more commonly present feeding intolerance and recurrent abdominal pain secondary to intestinal malrotation.
Midgut volvulus is the most feared consequence of intestinal malrotation as it may result in intestinal obstruction and ischemia with a potential for necrosis of the entire midgut [1, 2, 29]. In our review, the indication for surgery was suspected volvulus in more than half of the cases, and only a few of them were primarily approached by laparoscopy. The use of laparoscopy in infants and children with an acute abdomen or acute volvulus is controversial. On the one hand some case reports and small case series reported that the laparoscopic treatment of intestinal malrotation with volvulus is feasible and recommended that this should be performed where expertise and equipment are available [9, 16, 30]. On the other hand, other studies advocated against laparoscopy in patients with acute abdomen and evidence of volvulus [21, 31]. Hsiao and Langer proposed to avoid laparoscopic Ladd’s in neonates with suspected volvulus and to restrict this approach to older children regardless the presence of a volvulus [21].
The conversion rate of the laparoscopic technique to open surgery was found in a quarter of cases and in neonates it was as high as 50 % [21]. The majority of converted cases were recorded during the first years of experience in laparoscopy, which may indicate a surgical learning curve for the laparoscopic treatment of intestinal malrotation [19, 24].
According to our analysis, laparoscopy has advantages over open surgery as it was associated with shorter time to full enteral feeding and faster length of hospital stay. These two outcomes have been also recognized in infants and children treated by laparoscopy with other conditions [32, 33]. However, these results could be biased by the fact that patients in the open surgery group are more often symptomatic neonates with volvulus and/or with an increased risk of associated co-morbidities which may negatively affect the post-operative results.
In our study, we observed a significantly higher rate of overall post-operative complications in the open Ladd’s group [19, 23–27]. This is in line with other non-comparative studies that reported a complication rate of the Ladd’s procedure as high as 35 % in patients treated by open surgery and as high as 24 % in those treated by laparoscopy [16, 18, 20, 24, 30, 31]. However, again, these results should be interpreted with caution as open surgery patient were significantly younger than laparoscopic ones and both groups could be not completely comparable in terms of size and clinical presentation.
In our systematic review there was no statistical difference in the prevalence of post-operative bowel obstruction, even if no cases were observed in the laparoscopic group [23, 24, 26, 27]. Non-comparative studies report a rate of adhesive small bowel obstruction following open Ladd’s procedure between 2 and 15 % [8, 20]. However, this outcome is influenced by the length of follow-up that is variable in the analyzed studies.
In our meta-analysis the rate of post-operative volvulus was significantly higher in the laparoscopic group than in the open group. On the one hand, our meta-analysis shows that the five articles included in this forest plot have no degree of heterogeneity (I2 = 0 %), so that we can confidently state that the effect of the intervention being tested is accurate and can be trusted. On the other hand, we acknowledge that this outcome could be biased by the lack of patient information that would be important for a proper evaluation of risk stratification. In fact, not all authors reported details about their intra-operative findings (e.g intestinal necrosis), surgical maneuvers (e.g. enterotomy), and/or time to volvulus post-Ladd’s procedure. The cause for a higher incidence of post-operative volvulus in infants who undergo laparoscopic Ladd’s procedure may be an incomplete intestinal derotation and splaying of the mesentery [9, 16, 21, 26, 27, 31]. Some surgeons believe that post-operative adhesions are important to keep the small bowel in the non-rotation orientation to prevent future volvulus [27]. Therefore, the potential advantage of the laparoscopic approach in reducing post-operative adhesions and consequent small bowel obstruction could be neutralized by an increased risk of long-term post-operative volvulus.
We acknowledge that our literature analysis is limited by the absence of high-quality studies (i.e., prospective and/or randomized trials) and the heterogeneity of the patients included in both groups with regards to the age at surgery and the clinical indications.
In conclusion, the present systematic review shows that the current surgical management of infants and children with intestinal malrotation is not based on substantial evidence. The laparoscopic approach is more common in older patients and it is associated with earlier full enteral feeding, shortened length of hospital stay, and decreased risk of post-operative complications. However, this review highlights the higher incidence of post-operative volvulus after laparoscopic Ladd’s procedure questioning the efficacy of the laparoscopic approach. To validate the use of laparoscopy in this population of patients, high-quality prospective long-term trials are needed.
References
Zani A, Pierro A (2017) Intestinal malrotation. In: Puri P (ed) Newborn surgery, 4th edn. CRC Press, Boca Raton, FL (in press)
Zellos A, Zarganis D, Ypsiladis S et al (2012) Malrotation of the intestine and chronic volvulus as a cause of protein-losing enteropathy in infancy. Pediatrics 129(2):e515–e518
Millar AJ, Rode H, Cywes S (2003) Malrotation and volvulus in infancy and childhood. Semin Pediatr Surg 12(4):229–236
Yousefzadeh DK (2009) The position of the duodenojejunal junction: the wrong horse to bet on in diagnosing or excluding malrotation. Pediatr Radiol 39(Suppl 2):S172–S177
Warner B (1997) Malrotation. In: Oldham KT, Colombani PM, Foglia RP (eds) Surgery of infants and children: scientific principles and practice. Lippincott Williams & Wilkins, Philadelphia, pp 12–29
Torres AM, Ziegler MM (1993) Malrotation of the intestine. World J Surg 17(3):326–331
McVay MR, Kokoska ER, Jackson RJ et al (2007) Jack Barney Award. The changing spectrum of intestinal malrotation: diagnosis and management. Am J Surg 194(6):712–717 (discussion 718–719)
Lin JN, Lou CC, Wang KL (1995) Intestinal malrotation and midgut volvulus: a 15-year review. J Formos Med Assoc Taiwan yi zhi 94(4):178–181
Lampl B, Levin TL, Berdon WE et al (2009) Malrotation and midgut volvulus: a historical review and current controversies in diagnosis and management. Pediatr Radiol 39(4):359–366
Ford EG, Senac MO Jr, Srikanth MS et al (1992) Malrotation of the intestine in children. Ann Surg 215(2):172–178
Malek MM, Burd RS (2006) The optimal management of malrotation diagnosed after infancy: a decision analysis. Am J Surg 191(1):45–51
Graziano K, Islam S, Dasgupta R et al (2015) Asymptomatic malrotation: diagnosis and surgical management: an American Pediatric Surgical Association outcomes and evidence based practice committee systematic review. J Pediatr Surg 50(10):1783–1790
Ladd WE (1936) Surgical diseases of the alimentary tract in infants. N Engl J Med 215:705–708
van der Zee DC, Bax NM (1995) Laparoscopic repair of acute volvulus in a neonate with malrotation. Surg Endosc 9(10):1123–1124
Hsiao M, Langer JC (2011) Value of laparoscopy in children with a suspected rotation abnormality on imaging. J Pediatr Surg 46(7):1347–1352
Hagendoorn J, Vieira-Travassos D, van der Zee D (2011) Laparoscopic treatment of intestinal malrotation in neonates and infants: retrospective study. Surg Endosc 25(1):217–220
Bass KD, Rothenberg SS, Chang JH (1998) Laparoscopic Ladd’s procedure in infants with malrotation. J Pediatr Surg 33(2):279–281
Bax NM, van der Zee DC (1998) Laparoscopic treatment of intestinal malrotation in children. Surg Endosc 12(11):1314–1316
Fraser JD, Aguayo P, Sharp SW et al (2009) The role of laparoscopy in the management of malrotation. J Surg Res 156(1):80–82
Palanivelu C, Rangarajan M, Shetty AR et al (2007) Intestinal malrotation with midgut volvulus presenting as acute abdomen in children: value of diagnostic and therapeutic laparoscopy. J Laparoendosc Adv Surg Tech Part A 17(4):490–492
Hsiao M, Langer JC (2012) Surgery for suspected rotation abnormality: selection of open vs laparoscopic surgery using a rational approach. J Pediatr Surg 47(5):904–910
Kozlov YA, Novozhilov VA, Rasputin AA et al (2016) Endoscopic treatment of intestinal malrotation in newborns and infants. Khirurgiia 4:34–39
Miyano G, Fukuzawa H, Morita K et al (2015) Laparoscopic repair of malrotation: what are the indications in neonates and children? J Laparoendosc Adv Surg Tech Part A 25(2):155–158
Ooms N, Matthyssens LE, Draaisma JM et al (2016) Laparoscopic treatment of intestinal malrotation in children. Eur J Pediatr Surg 26(4):376–381
Pearson EG FS, Blinman TA (2013) Laparoscopic Ladd’s procedure is a safe and effective treatment for intestinal malrotation in children with and without volvulus. Paper presented at the American Academy of Pediatrics National Conference, Orlando FL
Stanfill AB, Pearl RH, Kalvakuri K et al (2010) Laparoscopic Ladd’s procedure: treatment of choice for midgut malrotation in infants and children. J Laparoendosc Adv Surg Techn Part A 20(4):369–372
Chen LE, Minkes RK, Langer JC (2003) Laparoscopic versus open surgery for malrotation without volvulus. Pediatr Endosurg Innov Techniques 7(4):433–438
Prasil P, Flageole H, Shaw KS et al (2000) Should malrotation in children be treated differently according to age? J Pediatr Surg 35(5):756–758
Lee HC, Pickard SS, Sridhar S et al (2012) Intestinal malrotation and catastrophic volvulus in infancy. J Emerg Med 43(1):e49–e51
Draus JM Jr, Foley DS, Bond SJ (2007) Laparoscopic Ladd procedure: a minimally invasive approach to malrotation without midgut volvulus. Am Surg 73(7):693–696
Kalfa N, Zamfir C, Lopez M et al (2004) Conditions required for laparoscopic repair of subacute volvulus of the midgut in neonates with intestinal malrotation: 5 cases. Surg Endosc 18(12):1815–1817
Durkin ET, Shaaban AF (2008) Recent advances and controversies in pediatric laparoscopic surgery. Surg Clin N Am 88 (5):1101–1119, viii
Hall NJ, Pacilli M, Eaton S et al (2009) Recovery after open versus laparoscopic pyloromyotomy for pyloric stenosis: a double-blind multicentre randomised controlled trial. Lancet 373(9661):390–398
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Catania, V.D., Lauriti, G., Pierro, A. et al. Open versus laparoscopic approach for intestinal malrotation in infants and children: a systematic review and meta-analysis. Pediatr Surg Int 32, 1157–1164 (2016). https://doi.org/10.1007/s00383-016-3974-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-016-3974-2