Abstract
Background: Elective laparoscopically assisted sigmoid colectomy for diverticular disease and ileocolic resection for terminal ileal Crohn’s disease are safe and beneficial procedures in many patients. However, few data exist regarding the laparoscopic management of enteric fistulas from diverticular and Crohn’s disease. Methods: We completed a retrospective chart review of patients who underwent laparoscopic treatment of enteric fistulas complicating diverticular and Crohn’s disease. Results: During an 8-year period (1994–2002), 72 patients underwent 73 laparoscopically assisted bowel resections for enteric fistulas by one surgeon at the Mount Sinai Medical Center. Ninety percent of patients had Crohn’s disease, the average age was 39, and the male/female ratio was 38/34. Patients had a history of prior abdominal surgery in 39.7% of cases. Multiple fistulas were present in 30% of patients and 12.3% underwent multiple resections at the time of operation. Mean operating time was 199 min, and the conversion rate was 4.1%. Average length of stay was 5.2 days. There were no mortalities in the series. Overall morbidity was 11%. Conclusions: Laparoscopic management of enteric fistula disease is safe and effective. Low morbidity and short hospital stay demonstrate the safety and benefit of the minimally invasive approach for even complicated fistula disease in patients with history of prior abdominal surgery and multiple fistulas, or in patients requiring multiple resections for fistulas from diverticular and Crohn’s disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Enteric fistulas are a frequent and challenging complication of diverticular and Crohn’s disease [8, 9]. A history of previous surgery, a significant inflammatory reaction/mass, and the use of steroids and immunosuppressants in patients with Crohn’s disease all complicate the surgical management of these patients. Surgical treatment in these cases usually involves resection of the involved segment and primary anastamosis in the elective setting. Fistula involvement of other segments of bowel or other organs, such as bladder, can often be treated with local repair as long as the segment does not have disease or inflammatory involvement.
Laparoscopic management of patients with diverticular and Crohn’s disease has become more common at centers for advanced laparoscopy [1, 13]. Elective laparoscopically assisted sigmoid colectomy for diverticular disease and ileocolic resection for terminal ileal Crohn’s disease have been shown to be safe and beneficial procedures in most patients [3, 4, 10]. However, the presence of enteric fistulas and an inflammatory mass has been associated with a higher conversion rate to open procedure and has been a relative contraindication to a laparoscopic approach in Crohn’s disease [2]. Given these findings, as well as the relatively few data that exist regarding the laparoscopic management of enteric fistula disease, we reviewed our series of patients with enteric fistulas complicating diverticular and Crohn’s disease.
Methods
We completed a retrospective chart review of patients who underwent laparoscopically assisted bowel resections for enteric fistulas from diverticular and Crohn’s disease. All operations were performed by one laparoscopic surgeon at the Mount Sinai Medical Center in New York. Data collected included patient demographics, prior medical history (presenting signs and symptoms, prior abdominal surgery, and medications), details of the operative procedure (operative time, type of fistula, type of procedure, and conversion rate), and postoperative course (length of stay, morbidity, and mortality). Institutional review board approval was obtained prior to data collection.
Results
We identified 72 patients who had undergone 73 laparoscopically assisted bowel resections for management of enteric fistulas in diverticular and Crohn’s disease by one minimally invasive surgeon between January 1994 and July 2002. Ten percent of patients had a history of diverticulitis and 90% of patients had Crohn’s disease. Thirty-eight of the patients were male, 34 were female, and the mean age was 39. Past medical and surgical history were significant for prior abdominal surgery in 40% of patients and 50% of patients were taking steroids and/or immunosuppressive agents at the time of operation. Obstructive symptoms including abdominal pain, distention, and nausea/vomiting were the most common presentation. A list of additional presenting symptoms is shown in Table 1.
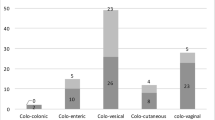
In terms of the operative procedure, the mean operative time was 199 min with a range of 62–400 min. The conversion rate was 4.1% with all conversions to open performed because of significant adhesions and inflammation. Multiple resections were performed in 12.3% of cases, and ileocolic resection was the most commonly performed procedure (70.7%). The types of resection completed are shown in Table 2. Multiple fistulas were found in 30% of cases, and enterocolic fistulas were the most common (34%). The distribution of fistulas is listed in Table 3. The surgical procedure performed was dependent on the judgment of the primary surgeon. Fistulas between two limbs of small bowel or between the terminal ileum and cecum usually required a single bowel resection and primary anastamosis, depending on the length of bowel between the fistula openings. Fistulas involving other organs, such as bladder, were treated with bowel resection of the involved segment and repair of the other involved organ. Fistulas between the small bowel and the sigmoid colon were treated by small bowel resection and stapling of the fistula opening in the sigmoid colon, as long as the surrounding colon was not involved with active inflammation. If colonic inflammation was encountered, an additional sigmoid resection and primary anastamosis were performed.
The mean length of stay was 5.2 days with a range of 2–14 days. There were no mortalities, and overall morbidity was 11%. Two patients required reoperation, the first for urgent laparotomy on postoperative day 1 for mesenteric bleeding and the second for cholecystectomy to treat acalculous cholecystitis. One patient with a colovesical fistula from diverticulitis underwent a sigmoid colectomy and developed an anastamotic bleed that was managed conservatively. However, this patient did go on to have a recurrent fistula approximately 5 months postoperatively. Additional postoperative complications are detailed in Table 4.
Discussion
Laparoscopic bowel resection for benign disease has become more common since it was first performed in the early 1990s [6]. The reported advantages include decreased pain, faster return of bowel function and resumption of diet, shorter length of stay, faster return to normal activity, and improved cosmesis. Laparoscopically assisted sigmoid colectomy for diverticular disease and ileocolic resection for Crohn’s disease are becoming more routine at many centers. However, conversion to open and traditional open procedures have been more common when a significant inflammatory reaction with accompanying abscess or fistula occurs.
Only a few small series exist in the literature regarding laparoscopy in the management of enteric fistula disease in diverticulitis and Crohn’s [5, 7, 11, 12]. Poulin et al. [11] looked at their experience with 13 patients with diverticular or Crohn’s fistulas undergoing laparoscopic bowel resection, and matched them with 13 patients undergoing open operations. There was no difference in outcome between the laparoscopic and open groups, and one of 13 patients required conversion to an open procedure. Watanabe et al. [12] also reported a small series of 20 patients undergoing 25 laparoscopic operations for fistula disease from Crohn’s. Complications were minimal at 16%, and conversion to open occurred in four patients (16%).
We report our experience with 72 patients undergoing 73 laparoscopic operations for fistulous disease complicating diverticular and Crohn’s disease. We were able to complete laparoscopically assisted bowel resections with a low conversion rate (4.1%), length of stay (5.2 days), and overall complication rate (11%). Operative time was significant at 199 min, but the procedures were complex with prior abdominal surgeries in 40%, multiple fistulas in 30%, and multiple resections completed in 12%.
Despite its retrospective design, we believe this study demonstrates that laparoscopically assisted procedures for enteric fistula disease are safe and feasible in experienced hands. In addition to the benefits of faster recovery and shorter hospital stay, laparoscopy clearly leads to decreased adhesion formation. This is of significant benefit in the Crohn’s population, which may require additional future surgical explorations and resections.
It is important to remember that these operations are advanced laparoscopic procedures that involve advanced laparoscopic skills and a steep learning curve. Certainly the results of this series are related to the significant laparoscopic experience of the team involved. Additional issues do remain unresolved, including cost analysis and evaluation using prospective and randomized data for comparison with open procedures. However, we do believe that laparoscopy will continue to evolve as a treatment option in patients with complicated fistula disease from diverticulitis and Crohn’s.
References
M Aleali JW Milsom (2001) ArticleTitle Laparoscopic surgery in Crohn’s disease. Surg Clin North Am 81 217–230 Occurrence Handle1:STN:280:DC%2BD3M7jsFGlsw%3D%3D Occurrence Handle11218166
JJ Bauer MT Harris NM Grumbach SR Gorfine (1996) ArticleTitleLaparoscopic-assisted intestinal resection for Crohn’s disease. J Clin Gastroenterol 23 44–46 Occurrence Handle10.1097/00004836-199607000-00012 Occurrence Handle1:STN:280:BymH3s3oslU%3D Occurrence Handle8835899
JL Bouillot JC Berthou G Champault C Meyer JP Arnaud G Samama D Collet P Brasslav A Gainant B Delaitre (2002) ArticleTitleElective laparoscopic colonic resection for diverticular disease. Results of a multicenter study in 179 patients. Surg Endosc 16 1320–1323
J Canin-Endres B Salky F Gattorno M Edye (1999) ArticleTitleLaparoscopically assisted intestinal resection in 88 patients with Crohn’s disease. Surg Endosc 13 595–599 Occurrence Handle10.1007/s004649901049 Occurrence Handle1:STN:280:DyaK1M3nvVGntw%3D%3D Occurrence Handle10347299
PJ Hewett R Stitz (1995) ArticleTitleThe treatment of internal fistulae that complicate diverticular disease of the sigmoid colon by laparoscopically assisted colectomy. Surg Endosc 9 411–413
M Jacobs JC Verdeja HS Goldstein (1991) ArticleTitleMinimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc 1 144–150 Occurrence Handle1:STN:280:ByuD1c%2FkslA%3D
JS Joo F Agachan SD Wexner (1997) ArticleTitleLaparoscopic surgery for lower gastrointestinal fistulas. Surg Endosc 11 116–118
JC Lavery (1996) ArticleTitleColonic fistulas. Surg Clin North Am 76 1183–1190 Occurrence Handle1:STN:280:BymH3sbgtlM%3D Occurrence Handle8841372
F Michelassi M Stella T Balestracci F Giuliante P Marogna GE Block (1993) ArticleTitleIncidence, diagnosis, and treatment of enteric and colorectal fistulae in patients with Crohn’s disease. Ann Surg 218 660–666 Occurrence Handle1:STN:280:ByuD2MfjvVw%3D Occurrence Handle8239781
JW Milsom KA Hammerhofer B Böhm P Mancelle P Elson VW Fazio (2001) ArticleTitleProspective, randomized trial comparing laparoscopic vs. conventional surgery for refractory ileocolic Crohn’s disease. Dis Colon Rectum 44 1–9 Occurrence Handle1:STN:280:DC%2BD38%2FnvVGjtg%3D%3D Occurrence Handle11805557
EC Poulin CM Schlachta J Mamazza PA Seshadri (2000) ArticleTitleShould enteric fistulas from Crohn’s disease or diverticulitis be treated laparoscopically or by open surgery? A matched cohort study. Dis Colon Rectum 43 621–627 Occurrence Handle1:STN:280:DC%2BD3c3osVKmtg%3D%3D Occurrence Handle10826421
M Watanabe H Hasegawa S Yamamoto T Hibi M Kitajima (2002) ArticleTitleSuccessful application of laparoscopic surgery to the treatment of Crohn’s disease with fistulas. Dis Colon Rectum 45 1057–1061 Occurrence Handle12195190
SD Wexner ID Moscovitz (2000) ArticleTitleLaparoscopic colectomy in diverticular and Crohn’s disease. Surg Clin North Am 80 1299–1319 Occurrence Handle1:STN:280:DC%2BD3cvmtVOitQ%3D%3D Occurrence Handle10987037
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Regan, J., Salky, B. Laparoscopic treatment of enteric fistulas. Surg Endosc 18, 252–254 (2004). https://doi.org/10.1007/s00464-003-8904-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-003-8904-4