Abstract
Background: We compared the perioperative parameters and outcomes achieved with hand-assisted laparoscopic colectomy (HALC) vs open colectomy (OC) for the management of benign and malignant colorectal disease, including cancer patients treated with curative intent. Methods: Sixty eligible patients were randomized to either HALC (n = 30) or OC (n = 30) treatment groups. We used Pearson’s chi-square and two-sample t-tests to compare the differences in demographics and perioperative parameters. Results: There were no significant differences in age, gender distribution, disease pattern, operative procedure, comorbidity, or history of abdominal surgery. The HALC patients had significantly shorter hospital stays and incision lengths, faster recovery of gastrointestinal function, less analgesic use and blood loss, and lower pain scores on postoperative days 1, 3, and 14. There were no significant differences in operative time, complications, or time to return to normal activity. Conclusion: Hand-assisted laparoscopic colectomy (HALC) is safe and produces better therapeutic results in terms of perioperative parameters than OC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Although laparoscopically assisted colectomy was first applied for colon resection as early as 1990, the procedure has not been widely accepted by surgeons. The major limitations of the approach include lack of tactile feedback, loss of normal stereoscopic vision, and inadequate exposure. Further more, it entails the possibility of iatrogenic trauma to solid organs and the intestine caused by laparoscopic instruments. Several reports have demonstrated that the laparoscopic approach confers particular benefits that include decreases in postoperative pain, length of hospital stay, and time to gastrointestinal recovery, as well as reductions in stress and immunosuppression. However, legitimate concerns have been raised regarding the prolonged operative time, the steep learning curve, the cost-effectiveness of laparoscopic techniques, and the potential for port site recurrence after curative resection for colorectal cancer [1, 9, 11, 12]. To address these limitations and unresolved issues, surgeons and engineers developed the new technique of hand-assisted laparoscopic surgery (HALS) [7].
With HALS, the surgeon’s hand is inserted through the abdominal wall to facilitate dissection and retraction without disturbing the pneumoperitoneum. Thus, it can be used, as in an open procedure, to palpate intraabdominal organs or tumors, to deflect organs atraumatically, to identify vessels and control any bleeding by finger pressure, and to dissect bluntly along tissue planes. As an added advantage, this approach is more economical than the traditional laparoscopic approach because it reduces the number of trocars and instruments. Several authors have also claimed that it is easier to learn and requires shorter operative times than traditional laparoscopic surgery [2, 3, 4, 5, 6, 8, 10, 13, 14, 15, 16]. Furthermore, HALS has a lower rate of conversion to open surgery and facilitates the completion complex procedures [2, 3, 10, 14, 15].
We conducted a prospective randomized single-center trial to compare the perioperative parameters and outcomes of hand-assisted laparoscopic colectomy (HALC) vs open colectomy (OC) for the treatment of patients with benign and malignant colorectal diseases, including cancers managed with curative intent.
Materials and methods
Patients
Between January 2002 and December 2002, patients diagnosed with benign and malignant colorectal disease and scheduled for elective surgery at our hospital were evaluated via colon examination, abdominal CT scan, liver ultrasound, and chest radiography. Based on that information, eligible patients were asked to participate in the study. Eligible patients were those aged from 18 to 80 years with an American Society of Anesthesiologists (ASA) score of I–III who were candidates for elective colorectal resection. Emergency operations, pregnancy, severe medical problems, and advanced malignant disease were contraindications precluding participation in the study. After giving written informed consent, the enrolled patients were randomized into two treatment groups, either HALC or OC, according to a predetermined scheme using random numbers.
All patients underwent preoperative mechanical bowel preparation. The oncological principles for both types of surgery included adequate mucosal resection margins, wide en bloc mesenteric and vascular resection, and minimal intraoperative manipulation of the tumor masses. The mesenteric vessels were ligated and transected intracorporeally. All the anastomoses were performed extracorporeally, either by hand sutures or staples. The open colon and rectum resection was performed by standard procedure. In the HALC group of patients, port size and placement were dependent on the location of the pathology in each case, and the specimen was extracted through the largest incision. All of the operations were performed by the same surgeon (J.C.K).
The two groups were compared with respect to perioperative parameters that included operative time, estimated blood loss, any complications, and incision length. Postoperatively, all patients were given patient-controlled analgesia (PCA) and oral analgesia for pain control. A clear-liquid diet was started when bowel sounds were heard or when flatus or stools were passed. The diet was advanced to full liquids and a soft diet as tolerated by each patient. Patients were discharged when the wound looked normal, when they could tolerate a regular diet, and when adequate oral pain control was possible. Questionnaires were completed by nurses on postoperative days 1, 3, 14, and 30 to evaluate recovery for each patient. Parameters included a pain score on a visual analogue scale (VAS) (range, 0–100), use of analgesia, gastrointestinal function recovery, oral intake, length of hospitalization, and any adverse events.
Statistical analysis
Data were analyzed using the SPSS10.0 software package (SPSS., Chicago, IL, USA). We compared the HALS with the OC group using chi-square tests for categorical variables and Student t-tests for continuous variables. Differences in the observed results were considered significant when p ≤ 0.05.
Surgical technique for HALC
After achieving general anesthesia, patients were placed in a modified lithotomy position, and a nasogastric tube and urinary catheter were inserted. HALC was performed in a manner similar to the standard laparoscopic procedure and involved the intracorporeal ligature of vascular pedicles and mobilization of the mesocolon of the affected area.
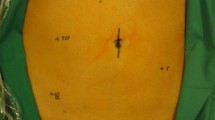
A pneumoperitoneum was induced using a Veress needle and maintained at 12–15 mmHg using an automatic carbon dioxide insufflator. A 10-mm 00 laparoscope was inserted through a supraumbilical port. Patients in the HALC group underwent exploratory laparoscopy to determine the appropriate place for the incision. This incision was later used for specimen retrieval and performance of the anastomosis. A 6–8-cm transverse incision was made in the left or right iliac fossa or in the suprapubic region, depending on the area of the colon and rectum affected, and the hand port device was inserted.
We used the HandPort device (Smith & Nephew, Andover, MA, USA). The surgeon’s dominant or nondominant hand was inserted into the hand port device, depending on the surgeon’s preference. Pneumoperitoneum was reestablished and the operative procedure carried out with hand assistance. Only one or two 10-mm trocars were inserted, at varying locations depending on the resection site. The colon and rectum were mobilized from peritoneal and retroperitoneal attachments using a 10-mm LCS Harmonic Scalpel (Ethicon Endo-Surgery, Cincinnati, OH, USA). The mesentery with its vascular stalk was ligated and divided intracorporeally using the Harmonic Scalpel. The mobilized bowel segment was brought through the hand port for transaction and retrieval of the specimen. An end-to-end anastomosis was performed extracorporeally, either hand-sutured or stapled. Finally, a suction drain was inserted into the pelvis, and the abdominal wall wounds were closed layer by layer.
Results
Sixty eligible patients with colorectal disease were enrolled in the study. Overall, five specific colorectal operations were performed using either hand-assisted l aparoscopic surgery or open colectomy procedures, including right hemicolectomy (n = 8), left hemicolectomy (n = 11), anterior resection (n = 20), low anterior resection (n = 10), and total abdominal colectomy (n = 11). Thirty patients were randomized to HALC and. 30 to open OC. None of the patients in the HALC group were converted to the OC procedure. There were no significant differences between the groups in terms of age, sex distribution, disease pattern, operative procedure, comorbidity, or previous abdominal surgery (Table 1).
The operative time was slightly, but not significantly, shorter in the HALC group than in the OC group (Table 2). The length of the surgical incision was significantly shorter in the HALC group than in the OC group, and the estimated blood loss was significantly lower in the HALC group. In the postoperative period, patients in the HALC group experienced earlier resumption of oral intake, faster recovery of gastrointestinal functions, less need for analgesia, and an overall shorter hospital stay.
Postoperative pain scores were recorded on postoperative days 1, 3, 14, and 30 (Table 3). Patients in the HALC group reported lower pain scores on postoperative days 1, 3, and 14 than patients in the OC group. On postoperative day 30, there was no significant difference in pain score between the groups. No significant differences between the groups were found for the day of returning to normal activity or the development of complications.
Discussion
Hand-assisted laparoscopic surgery (HALS) is a newly developed endoscopic technique that was first described in 1994 [13]. Various operations have been performed with this technique, including colorectal resection, living-related donor nephrectomy, splenectomy, aortic surgery, vertical banded gastroplasty, and liver resection [2, 5, 6, 16]. HALS is a safe and efficient approach that makes it possible to combine the established convenience and safety of open surgery with the advantages of traditional laparoscopic surgery. In addition, HALS can simplify technically complex operations and can be used to initiate nonskilled surgeons in the performance of more advanced laparoscopic surgery [2, 3, 4, 5, 6, 8, 10, 13, 14, 15, 16].
To our knowledge, no prospective randomized trial comparing HALC and OC has been published to date. Only randomized and nonrandomized trials comparing HALC and traditional laparoscopic colectomy have been reported [2, 3, 13, 14, 15]. With respect to patient selection, we included curative cancer cases in our study, a group that had been omitted in the report by the HALS Study Group [3]. That report raised legitimate concerns regarding the potential of port site recurrence after the curative resection of colorectal cancers. However, the role of HALS in the management of cancer is still controversial. Targarona et al. conducted a prospective randomized study of HALS vs traditional laparoscopic surgery for the management of colorectal disease and included cancer patients in their study. They reported that there were no cases in either group where malignant cells could be found in the intraoperative lavage [15]. Several authors have suggested that use of the hand port device might offer protection of the wound site and prevent contamination of the wound by malignant cells or bacteria [4, 6, 8].
In our study, patients in the HALC group received the benefits and advantages of traditional laparoscopic surgery, including early recovery of gastrointestinal functions, less pain and less use of analgesic drugs, shorter hospital stay, and better cosmetic results than those in the OC group. In each group, the disease processes, complications, and operations performed were similar. Patients in the HALC group had fewer complications than those in the OC group, but this finding was not statistically significant. Although there were four complications in the HALC group, none of the patients, required repeat operations. Similarly, in a randomized study of hand-assisted laparoscopic vs open surgical live donor nephrectomy, Wolf et al. reported that laparoscopic donor nephrectomy is associated with a briefer, less intense, and more complete convalescence than the open surgical approach [16].
With regard to the operative time, there was no statistically significant difference between the two groups, which is surprising. This finding may be a reflection of more extensive surgical experience and better instruments. In addition, left colon and splenic flexures were more easily mobilized and dissected using Harmonic Scalpel dissection in the HALC patients. Shortening the operative time is also a significant advantage, especially for the procedure of living-related donor nephrectomy, because it minimizes the warm ischemia time [5].
In traditional laparoscopic colectomy, the rate of conversion to open surgery varies from 17% to 42% [1, 9, 11, 12]. The most common reasons for conversion are diverticular inflammation, intraabdominal adhesions, and the need for distal rectal resection. In comparison with traditional laparoscopic surgery, the reported conversion rate of HALS varies from 0% to 22%, and the most common reason for conversion is difficulty in maintaining a satisfactory pneumoperitoneum [2, 3, 10, 14, 15]. In our study, patients in the HALC group had prior abdominal surgery with mild adhesion (n = 7), colon cancer (n = 11), rectal cancer (n = 4), and diverticulitis (n = 5), but no conversions to the open procedure were needed. Retrospectively, we took >30 min to set up the device and to maintain the pneumoperitoneum during the operation in the first 10 cases, but this problem was resolved with more experience.
During HALC, we used the HandPort device as a wound protector, and all the specimen extractions and bowel anastomoses were performed through this device. In our study, one patient in the HALC group and four in the OC group developed wound infections, but this finding was not statistically significant. The performance of the HandPort device has been evaluated by several groups [14, 15, 16]. To date, we have applied the device to numerous laparoscopic approaches, such as colectomy, nephrectomy, and splenectomy, with excellent results.
Our own experiences using the HandPort device have shown that the effort needed to maintain the pneumoperitoneum can cause wrist and forearm constriction, resulting in numbness and fatigue of the surgeon’s hand. These findings are related to the size of the skin and fascial incision, the duration of the operative procedure, and the location of the hand port site [2, 6]. The problem of hand fatigue can be prevented by careful choreography and planning of trocar and hand port placement [2]. In general, most surgeons prefer to place their nondominant hand in the abdomen, but the dominant hand can also be used. In our study, hand fatigue occurred in 10 procedures (four low anterior resections and six total abdominal colectomles). To complete the procedure, the surgeon had to rest the hand for a few minutes or switch to the other hand.
Several centers reporting results with traditional laparoscopic colectomy have found that 10–40 procedures need to be performed to develop adequate skills [1, 9, 11, 12]. Attempts to define the learning curve for the mastery of HALC revealed that it is mandatory to focus on the operating time required, the conversion rate, and the operative complications. In our HALC group, most of the complications (75%) developed in the first five cases; the operative time reached a low point between cases 5 and 10. In addition, there were no conversions to the open procedure. Because this report represents the interim analysis of a relatively small group of patients, we can draw no firm conclusions about the rate of learning for HALC. Nevertheless, we believe that HALC has a shorter learning curve than traditional laparoscopic colectomy .
In conclusion, this prospective randomized study indicates that patients treated by the HALC procedure benefited from the smaller incisions required, with less pain, earlier resumption of a normal diet, more rapid recovery of gastrointestinal function, and an overall shorter hospital stay than patients treated by OC. We believe that, if practiced more, this technique might provide an effective bridge between traditional laparoscopic surgery and conventional open procedures. However, to address the role of HALC in the curative management of colorectal malignancies, long-term follow-up is warranted.
References
PM Falk RW Beart SD Wexner AG Thorson DG Jagelman IC Lavery OB Johansen RJ Fitzgibbons (1993) ArticleTitleLaparoscopic colectomy: a critical appraisal. Dis Colon Rectum 36 28–34 Occurrence Handle1:STN:280:ByyC3crntlw%3D Occurrence Handle8416776
InstitutionalAuthorNameHALS Study Group (2000) ArticleTitleHand-assisted laparoscopic surgery (HALS) with the HandPort system: initial experience with 68 patients. Ann Surg 231 715–723 Occurrence Handle1:STN:280:DC%2BD3c3jtFCksQ%3D%3D Occurrence Handle10767793
InstitutionalAuthorNameHALS Study GroupHALS Study Group (2000) ArticleTitleHand-assisted laparoscopic surgery vs standard laparoscopic surgery for colorectal disease. Surg Endosc 14 896–901 Occurrence Handle10.1007/s004640000324 Occurrence Handle11080399
JJ Jakimowicz (2000) ArticleTitleWill advanced laparoscopic surgery go hand-assisted? Surg Endosc 14 881–882 Occurrence Handle10.1007/s004640000354 Occurrence Handle11080396
K Kercher D Dahl R Harland R Blute K Gallagher D Litwin (2001) ArticleTitleHand-assisted laparoscopic donor nephrectomy minimizes warm ischemia. Urology. 58 152–156 Occurrence Handle10.1016/S0090-4295(01)01194-3 Occurrence Handle1:STN:280:DC%2BD3MvksVeksw%3D%3D Occurrence Handle11489685
MS Kurian E Patterson VE Andrei MB Edye (2001) ArticleTitleHand-assisted laparoscopic surgery: an emerging technique. . 15 1277–1281 Occurrence Handle1:STN:280:DC%2BD3MnotV2lsA%3D%3D
DW Meijer JJG Bannenberg PF Leahy PJK Klopper (1994) ArticleTitleA helping hand for the laparoscopic sigmoid resection [Abstract]. Min Invas Ther 3 43
DW Meijer JJG Bannenberg JJ Jakimowicz (2000) ArticleTitleHand-assisted laparoscopic surgery: an overview. Surg Endosc 14 891–895 Occurrence Handle1:STN:280:DC%2BD3M7gvFOrsA%3D%3D Occurrence Handle11080398
AE Ortega RW Beart GD Steele DP Winchester FL Greene (1995) ArticleTitleLaparoscopic bowel surgery registry: preliminary results. Dis Colon Rectum 38 681–686 Occurrence Handle1:STN:280:ByqA3s7gslA%3D Occurrence Handle7607025
A Pietrabissa C Moretto A Carobbi U Boggi M Ghilli F Mosca (2002) ArticleTitleHand-assisted laparoscopic low anterior resection: initial experience with a new procedure. Surg Endosc 16 431–435 Occurrence Handle10.1007/s00464-001-9084-8 Occurrence Handle1:STN:280:DC%2BD387psFSiug%3D%3D Occurrence Handle11928022
JM Ramos RW Beart R Goes AE Ortega RT Schlinkert (1995) ArticleTitleRole of laparoscopy in colorectal surgery: a prospective evaluation of 200 cases. Dis Colon Rectum 38 494–501 Occurrence Handle1:STN:280:ByqB2MvpslY%3D Occurrence Handle7736880
AJ Senagore MA Luchtefeld JM Mackeigan WP Mazier (1993) ArticleTitleOpen colectomy versus laparoscopic colectomy: are there differences? Am Surg 59 549–553 Occurrence Handle1:STN:280:ByyA3s3jtFU%3D Occurrence Handle8338287
W Sjoerdsma DW Meijer A Jansen KT den Boer CA Grimbergen (2000) ArticleTitleComparison of effiencies of three techniques for colon surgery. J Laparoendosc Adv Surg Tech A 10 47–53 Occurrence Handle1:STN:280:DC%2BD3c7mvVyhsg%3D%3D Occurrence Handle10706303
InstitutionalAuthorNameHALS Study GroupHALS Study GroupSouthern Surgeons Club Study Group (1999) ArticleTitleHandoscopic surgery: a prospective multicenter trial of a minimally invasive technique for complex abdominal surgery. Arch Surg 134 477–486
EM Targarona E Gracia J Garriga C Martínez-Bru M Cortés R Boluda L Lerma M Trías (2002) ArticleTitleProspective randomized trial comparing conventional laparoscopic colectomy with hand-assisted laparoscopic colectomy. Surg Endosc 16 234–239 Occurrence Handle10.1007/s00464-001-8168-9 Occurrence Handle1:STN:280:DC%2BD383jtVWrtg%3D%3D Occurrence Handle11967670
JS Wolf RM Merion AB Leichtman DA Campbell JC Magee JD Punch JG Turcotte JW Konnak (2001) ArticleTitleRandomized controlled trial of hand-assisted laparoscopic versus open surgical live donor nephrectomy. Transplantation 72 284–290 Occurrence Handle1:STN:280:DC%2BD3MvktFWisQ%3D%3D Occurrence Handle11477354
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kang, JC., Chung, MH., Chao, PC. et al. Hand-assisted laparoscopic colectomy vs open colectomy: a prospective randomized study. Surg Endosc 18, 577–581 (2004). https://doi.org/10.1007/s00464-003-8148-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-003-8148-3