Abstract
Background: Pneumoperitoneum (P) created to facilitate laparoscopy (L) is associated with splanchnic perfusion, ischemia/reperfusion (I/R) injury, and oxidative stress. In this randomized controlled experimental study with blind outcome assessment, we evaluated the effect of preconditioning (PRE) on L-induced I/R injury. Methods: The subjects were 40 Sprague-Dawley male rats. P was created in all except controls, using carbondioxide (CO2) insufflation under a pressure of 15 mmHg. PRE consisted of 10 min of P, followed by 10 min of deflation (D). The rats were randomized to the following groups: Group P was subjected to 60 min of P. Group P/D was subjected to 60 min of P, followed by 45 min of D. Group PRE/P was subjected to PRE, followed by 60 min of P. Group PRE/P/D was subjected to PRE, followed by 60 min of P and 45 min of D. Group C (control) was subjected to a sham operation, without P. Its anesthesia time was equal to that for group PRE/P/D. At the end of the experiments, the rats were killed; blood, liver, and kidney samples were then obtained and coded. Plasma alanine aminotransferase (ALT) and malondialdehyde (MDA), as well as homogenized tissue MDA levels and glutathione (GSH) activities, were measured; tissue samples were assessed for histopathological evidence of injury; all assessments were done by investigators blinded to the study design. The results were decoded and analyzed statistically with the Kruskal-Wallis and Mann Whitney tests. A p < 0.05 was considered significant. Results: Plasma ALT as well as plasma, liver, and kidney MDA levels and liver and kidney injury scores were increased, whereas liver and kidney GSH values were decreased in groups P and P/D, as compared to group C. Rats subjected to PRE before P had plasma ALT, kidney MDA, and kidney and liver GSH levels comparable to controls; their kidney and liver injury scores were higher than controls but significantly lower than nonpreconditioned animals. PRE enabled decreased plasma, kidney, and liver MDA as well as increased kidney GSH if applied before P; its efficacy on oxidative stress was limited to providing decreased kidney MDA and increased kidney GSH if applied before P/D. However, PRE significantly attenuated kidney and liver injury after P as well as P/D. Conclusion: PRE consisting of 10 min of P followed by 10 min of D decreases the oxidative stress induced by sustained P in the plasma, liver, and kidney. PRE significantly limits liver and kidney injury after prolonged P and P/D. After further studies to define its ideal timing, PRE before L incorporating P may have clinical relevance, especially for elderly patients or those with impaired hepatic and/or renal function or perfusion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Pneumoperitoneum (P) is often used to facilitate the realization of laparoscopy (L). The most common method of creating surgical P is the insufflation of carbon dioxide (CO2). However, L-related adverse functional and structural alterations have been noted in many organs and associated with the increased systemic CO2 load and intraabdominal pressure (IAP) that occurs during P [19, 24, 26].
Splanchnic organs have been recognized as being particularly vulnerable to the deleterious effects of P, owing to significant local as well as systemic hemodynamic changes [6, 12, 19, 21, 24]. Gas insufflation during P is associated with significant ischemia of splanchnic organs [6, 19, 24], followed by their sometimes paradoxically increased [6] reperfusion injury after deflation (D). Thus, P followed by D comprises the sequential stages of ischemia/reperfusion, respectively (I/R). It follows that L incorporating P has the potential to cause I/R injury, which is currently viewed as the most likely mechanism by which hypoxia damages cells and tissues [13].
Augmented production of reactive oxygen and nitrogen species and of other related and hazardous compounds not only during ischemia but also during reperfusion are considered to be crucial elements in the development of I/R-injury [13].
The liver and kidneys are among the splanchnic organs most severely affected by L incorporating P [6, 12, 21, 23, 24]. Indeed, P can depress the dual supply of liver perfusion, with loss of the buffering response of hepatic arterial flow to impaired portal venous flow seen in other settings of portal ischemia [21]. Impairment of liver perfusion secondary to L can have important clinical consequences, as implied by the increased blood levels of liver enzymes noted in animals [23] and humans [3] and by the spectrum of structural alterations, including liver necrosis, documented in animals after prolonged P [23].
The kidneys are also prone to impaired perfusion and I/R injury when exposed to P [24]; complications can include necrosis and failure [12, 23].
Oxidative stress represents loss of the normal balance between the oxidants and antioxidants of the body [27]; it is not only an indicator of, but also a contributor to, the development of organ damage, including that of the liver [14, 25] and kidney [10, 28]. Despite its potential to promote I/R injury, data consistent in showing that L incorporating P is accompanied by tissue oxidative stress remain very limited. P-associated oxidative stress in splanchnic organs was described initially by Eleftheriadis et al. [7] as relevant changes in the liver, spleen, and intestines of rats; we reported further evidence of intestinal oxidative stress [30] and were the first to demonstrate renal oxidative stress complicating P [1]. Glantzounis et al. [8] reported changes in the serum markers of oxidative stress following laparoscopic cholecystectomy in humans, thereby showing that the P-associated I/R injury of splanchnic organs could have systemic effects.
Increasing recognition of the adverse effects of P, has led to a search for alternative approaches, such as gasless L. However, since P facilitates better visualization and manipulation during L, a safer method of applying it would have clinical value.
Ischemic preconditioning (PRE) is an injury-limiting mechanism initially described as the attenuation of cardiac damage due to a severe I/R insult by previous short I/R cycles [16]. The liver [20] and kidney [5, 17] have also been shown to benefit from PRE prior to mechanical interruption of their circulation. Arguing that a PRE approach could also help to limit L-related I/R injury, we recently showed, for the first time, that a system comprising brief and sequential periods of P followed by D was effective in decreasing oxidative stress in the intestines of rats exposed to P [30]. This randomized, controlled, experimental study with blind outcome assessment was designed to investigate whether short-term P followed by D could also serve as a protective PRE mechanism against L-associated adverse changes in the liver and kidneys. We also evaluated whether there were any changes in organ function and/or structure after P, with or without PRE, that were related to a possible modification of P-associated I/R injury by PRE, blood, and tissue markers of oxidative stress.
Materials and methods
The study protocol was designed in accordance with the 1996 revised edition of The Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health and approved by the university ethical committee. All of the procedures and experiments were performed in rats while they were under the effect of anesthesia.
After overnight fasting with free access to tap water, 40 male, 4-month-old Sprague-Dawley rats weighing 280 ± 15 g were anesthetized with an intraperitoneal injection of pentobarbital (50 mg per kg body weight). A 1-cm-long midline laparotomy incision was made below the umbilicus and a catheter was placed into the peritoneum as the vehicle of P, which was created in all animals except controls. P was obtained by connecting the other side of the tube to a CO2 insufflator (model no. 3-315-00, Nortech, Elgin, IL, USA). The pressure of the CO2 insufflator was fixed at 15 mmHg. The system used to obtain P enabled simultaneous CO2 insufflation into multiple rats under the same pressure. Prior to insufflation, the incision was closed with a tight purse-string suture to prevent leakage.
For the purpose of this study, PRE was defined as 10 min of P followed immediately by 10 min of D. The rats were randomly assigned to one of the following groups (n = 8 for each): Group P was subjected to 60 min of P. Group P/D was subjected to 60 min of P, followed by 45 min of D. Group PRE/P was subjected to PRE, followed by 60 min of P. Group PRE/P/D was subjected to PRE, followed by 60 min of P and then 45 min of D. Group C (control) was subjected to a sham operation, without P. The anesthesia duration of group C was equal to that of group PRE/P/D (125 min).
On completion of the experiments, laparotomy incisions were opened and extended; P catheters were removed and the kidneys and livers of the rats were removed. Their blood samples were taken by intraaortic cannulation. They were then killed with an intracardiac potassium injection.
One-half of each kidney and one lobe of each liver was washed with ice-cold lactated Ringer’s solution and stored at –20°C until analysis. At that time, it was initially homogenized (Ultra Turrax Homogenizer, T18 Basic; IKA, Wilmington, NC, USA) in 0.1 M ice-cold phosphate buffer with a pH of 7.4 and then centrifuged at 10000 rpm and +4°C for 10 min. Finally, its supernatant was removed to measure tissue markers of oxidative stress. The other kidney halves and liver lobe were immersed in 10% formaldehyde for later histopathological examination. Each tissue sample was assigned a code number by the principal investigator and referred to the biochemists and pathologist participating in the study, who were blinded to the differences between specific groups and animals. All results were reported under then respective sample code numbers.
Biochemical analysis
Blood and tissue samples were used for biochemical analysis. After procurement, blood samples were centrifuged at 3000 rpm and +4°C for 10 min to allow separation of plasma, which was removed and kept at –20°C until analysis. Alanine aminotransferase (ALT) levels were determined in plasma samples with an autoanalyzer (Hitachi automatic analyzer 911; Hitachi, Mannheim, Germany). Plasma malondialdehyde (MDA) was measured as an indicator of lipid oxidation, using the thiobarbituric acid method of Ohkawa et al. [18].
Two markers of oxidative stress were measured in supernatants of homogenized liver and kidney tissue samples. MDA was measured to assess the degree of tissue lipid oxidation [18]. Reduced glutathione (GSH) levels were measured as an indicator of tissue antioxidant capacity using the method of Beutler et al. [4]. MDA levels were expressed as nmol/mg protein. GSH levels were expressed as pmol/mg protein for kidney tissue and nmol/mg protein for liver tissue.
Histopathological analysis
Liver and kidney samples preserved in 10% formaldehyde were embedded in paraffin, cut into 3-µm–thick sections, and stained with hematoxylin-eosin. The section of each sample with the largest surface area was selected and analyzed by the pathologist. Ten high-power fields (hpf) of each section were examined via light microscopy for tissue injury using the semiquantitative scale described by Hauet et al. [9] (Table 1). Parameters evaluated in kidney samples were proximal tubular cell vacuolization, tubular dilatation, congestion, interstitial mononuclear inflammatory cell infiltration, and interstitial edema. Each parameter was graded with a score between 1 to 5 according to its severity and frequency in 10 hpf of the kidney section selected; this was followed by the calculation of the sum of scores assigned to all five parameters, with the possibility of a maximum total score of 25. The same approach was used to assess liver samples. Parameters evaluated in liver sections were single cell necrosis, cellular edema, congestion, focal hemorrhage, and portal and sinusoidal mononuclear inflammatory cell infiltration.
Statistical analysis
The results were decoded after being reported and expressed as the mean ± standard error of the mean (SEM). Statistical analysis of the data was done with the Kruskal-Wallis and Mann–Whitney U tests. A p value of <0.05 was considered significant.
Results
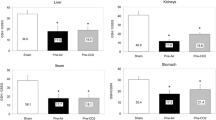
The results are summarized in Tables 2 and 3 and presented graphically in Figs. 1, 2, 3. Plasma ALT levels were significantly increased in the P and P/D groups compared to the control group (88.00 ± 6.02 and 83.62 ± 6.39 vs 58.00 ± 7.07 U/L, respectively; p = 0.001 for P vs C and p = 0.017 for P/D vs C). Plasma MDA levels were also significantly increased in the P and P/D groups compared to the control group (5.30 ± 0.41 and 4.11 ± 0.43 vs 2.66 ± 0.30 µmol/L, respectively; p = 0.011 for P vs C and p = 0.027 for P/D vs C). Kidney MDA values were higher in the P and P/D groups than the control group (75.23 ± 1.34 and 77.90 ± 1.29 vs 61.07 ± 1.58 nmol/mg protein, respectively; p = 0.007 for P vs C and for P/D vs C). Liver MDA values were also higher in the P and P/D groups than the control group (57.20 ± 3.01 and 53.11 ± 1.47 vs 37.67 ± 2.09 nmol/mg protein, respectively; p = 0.007 for P vs C and for P/D vs C). Kidney and liver GSH were decreased, whereas kidney and liver injury scores were increased in the P and P/D groups compared to the control group; all differences had statistical relevance (p = 0.007 for P vs C and for P/D vs C with respect to kidney GSH; p = 0.006 for P vs C and p = 0.008 for P/D vs C with respect to liver GSH; p = 0.006 for P vs C and p = 0.005 for P/D vs C with respect to both injury scores).
Plasma ALT and MDA values of the groups (n = 8 in each). For plasma ALT, p = 0.001 for P vs C, p = 0.017 for P/D vs C, p > 0.05 for all other comparisons. For plasma MDA, p = 0.011 for P vs C, p = 0.027 for P/D vs C, p = 0.017 for PRE/P/D vs C; p = 0.03 for P vs PRE/P; p > 0.05 for all other relevant comparisons.
Liver tissue MDA and GSH values of the groups (n = 8 in each). For liver MDA, p = 0.007 for P vs C and for P/D vs C; p = 0.007 for PRE/P vs C and for PRE/P/D vs C; p = 0.012 for P vs PRE/P; p > 0.05 for all other relevant comparisons. For liver GSH, p = 0.006 for P vs C and p = 0.008 for P/D vs C; p > 0.05 for all other relevant comparisons but p values close to statistical relevance for P vs PRE/P (0.052) and for P/D vs PRE/P/D (0.059).
No statistically relevant difference was found between the P and P/D groups.
The PRE/P and PRE/P/D groups had results similar to those of the control group, with the exception of increased plasma MDA in group PRE/P/D (p = 0.017 vs C); liver MDA increased in both groups (p = 0.007 for PRE/P vs C and for PRE/P/D vs C) and both had higher kidney and liver injury scores (p = 0.005 for PRE/P vs C and p = 0.004 for PRE/P/D vs C, in relation to both scores).
As compared to group P, group PRE/P had decreased plasma (p = 0.03), kidney (p = 0.001), and liver (p = 0.012) MDA; it also had increased kidney GSH (p = 0.001) and decreased kidney and liver injury (p = 0.037 and p = 0.04, respectively). Liver GSH was also increased in group PRE/P, in contrast to group P; the difference approached but did not reach statistical value (p = 0.052). No significant difference was seen between the plasma ALT of groups P and PRE/P.
In comparison to group P/D, group PRE/P/D had decreased kidney MDA (p = 0.001) and increased kidney GSH (p = 0.001) levels; it also had lower scores for kidney (p = 0.005) and liver (p = 0.045) injury.
Histopathological evidence of moderate degree liver and kidney injury was found in all study groups as compared to the control group, but groups PRE/P and PRE/P/D had the least severe lesions. In contrast, groups P and P/D had the most impressing evidence of organ injury, with severe tubular vacuolization and dilatation, congestion, and interstitial inflammatory cell infiltration in their kidneys accompanied by particularly prominent cellular necrosis, edema, and mononuclear cell infiltration in their livers. PRE resulted in lower kidney and liver injury scores than P without PRE.
Discussion
P is often used during L, but it has serious disadvantages, including its ischemic potential. On the other hand, D of P is associated with organ reperfusion. In effect, P/D amounts to I/R, and L carries the risk of being complicated by I/R injury of affected organs. Evidence of oxidative stress can be used to assess the degree of I/R injury after L. However, the true weight of oxidative stress resides in the fact that it is not only an indicator of ischemic damage in the liver [25] and kidney [28], but also a causal factor in their chronic and progressive functional and structural deterioration within the context of a wide spectrum of diseases [10, 14]. The presence of oxidative stress in splanchnic organs after L implies the possibility of continuing damage in organs subjected to I/R injury during P/D. Eleftheriadis et al. [7] were the first to document oxidative stress in the liver following P. We were the first to show the presence of P-related significant oxidative stress in renal tissue, independent from and additive to the effect of warm ischemia in a rat model of laparoscopic donor nephrectomy [1].
Notwithstanding these findings and despite the development of alternative approaches, P does make organ manipulation easier for the surgeon. Therefore, a method that curtailed its risk would be valuable. Indeed, increasing recognition of the adverse effects of P on splanchnic organ perfusion led Richter et al. [21] to suggest that “a selective setting, including low-pressure pneumoperitoneum with intermittent deflation at distinct time points may be recommended for safe laparoscopic interventions in critically ill patients.” Our recent study [30] and current data show that D of P, not in an intermittent manner but as a PRE approach, can protect against I/R injury related to L, similar to the beneficial effects of PRE mechanisms in other I/R injury models.
Ischemic PRE was initially described in relation to the heart as an endogenous protective mechanism by which short periods of I/R cycles attenuate the organ injury secondary to a subsequent and more severe I/R insult [16]. Shortly thereafter, the liver [20] and kidney [5, 17] were also shown to benefit from PRE prior to mechanical interruption of their circulation. Inspired by the positive results of PRE in other models of I/R injury, we recently reported the results of the first study concerning the effect of PRE on P-induced tissue injury [30]. By demonstrating the protective effect of a short period of P followed by a similar period of D against I/R injury in the intestines of rats exposed to P [30], we were able to define a PRE system relevant to L for the first time. The same PRE system was utilized in this study, in which we observed that PRE consisting of 10 min of P followed by 10 min of D is effective in attenuating P-induced oxidative stress in the plasma, kidney, and liver, as indicated by the decreased plasma, kidney, and liver MDA and the increased kidney GSH values of rats exposed to P after PRE as compared to those exposed to P without PRE. Rats exposed to P/D after PRE also had lower kidney MDA and higher kidney GSH than those exposed directly to P/D.
MDA arises from the breakdown of lipid peroxyl radicals and oxidizes protein molecules [18]; thus, it is a result as well as a cause of oxidative stress, while GSH is an important antioxidant [15].
Consistent with the place of oxidative stress as a marker and contributory factor in organ injury, our current data demonstrates attenuated oxidative stress, as well as injury to the kidney and liver, when PRE is employed before P or P/D.
The differences between the oxidative stress markers of groups P and P/D compared to groups PRE/P and PRE/P/D suggest the possibility that PRE may be less protective after P/D as opposed to its impressive efficacy after P. This can be explained by the unfavorable effect of prolonged D itself, as a cause of reperfusion [6] injury. Indeed, group PRE/P/D had higher plasma ALT and plasma, kidney, and liver MDA levels than group PRE/P; although the differences were not of sufficient magnitude to reach statistical relevance, they can be interpreted as reflecting aggravated systemic and tissue oxidative stress after prolonged cycles of P followed by prolonged D and relative resistance to PRE secondary to prolonged D. Furthermore, we did not observe any decrease in kidney and liver injury in group P/D as compared to group P. Our data indicate that the effects of prolonged D may be even more deleterious to the liver. Taking into consideration the study of Islam et al. [11], who showed that four repeated 15-min I/R cycles of renal artery clamping/release had no protective effect on later renal ischemia, recurrent periods of D alternating with periods of P throughout L procedures, as recommended by Richter et al. [21], are probably best avoided.
The PRE/P and PRE/P/D groups had results similar to those of the control group, with the exception of increased plasma MDA in group PRE/P/D as well as increased liver MDA, kidney, and liver injury scores in both PRE groups. However, since both PRE groups had significantly lower kidney and liver injury scores than the non-preconditioned groups, PRE proved effective in limiting kidney and liver injury secondary to P or P/D.
P-induced splanchnic ischemia and related adverse alterations in splanchnic organs may have particular relevance for elderly patients whose organs often have limited functional capacity. Moreover, elderly patients suffer increased hepatic ischemia after L [22] and renal antioxidant activity decreases with aging [2].
We conclude that a PRE approach may exert a beneficial effect prior to L incorporating P, particularly for elderly patients and/or those with existing impairment of hepatic and/or renal function or perfusion, especially if their operations last for extended periods. However, our experimental protocol of PRE is too lengthy to be recommended for direct use in humans. We are currently in the process of refining it through studies focused on the ideal time required for an optimum PRE effect. Despite pharmaceutical approaches that simulate its action, ischemic PRE has still not found a definite place in clinical practice, even with respect to its original site of discovery, the heart [29]. We agree with Yellon and Dana that more work on its adaptation to clinical settings is required for PRE to become anything more than a tool for the scientist [29]. At present, avoiding long and repeated periods of P as well as D and initiating L with very short sequences of P/D before the definitive P period should be considered for the elderly and other patients with increased risk of kidney or liver dysfunction.
References
G Akbulut M Serteser C Polat T Köken F Aktepe S Yilmaz Ç Gökçe Ö Gökçe (2002) ArticleTitleChanges in tissue oxidative stress markers in an experimental model of laparoscopic donor nephrectomy. Transplantation 74 1768–1772 Occurrence Handle10.1097/00007890-200212270-00022 Occurrence Handle1:CAS:528:DC%2BD38Xpslaku7w%3D Occurrence Handle12499896
Z Akçetin G Erdemli HJ Bromme (2000) ArticleTitleExperimental study showing a diminished cytosolic antioxidative capacity in kidneys of aged rats. Urol Int 64 70–73 Occurrence Handle1:CAS:528:DC%2BD3cXktlGktb4%3D Occurrence Handle10810267
VE Andrei M Schein M Margolis JC Rucinski L Wise (1998) ArticleTitleLiver enzymes are commonly elevated following laparoscopic cholecystectomy: is elevated intra-abdominal pressure the cause? Dig Surg 15 256–259 Occurrence Handle10.1159/000018624 Occurrence Handle1:STN:280:DyaK1M%2Fmt1WgsA%3D%3D Occurrence Handle9845595
E Beutler (1970) Red cell metabolism. E Beutler (Eds) A manual of biochemical methods. Grune & Stratton New York 66
JV Bonventre (2002) ArticleTitleKidney ischemic preconditioning. Curr Opin Nephrol Hypertens . 43–48 Occurrence Handle10.1097/00041552-200201000-00007
E Eleftheriadis K Kotzampassi D Botsios E Tzartinoglou H Farmakis J Dadoukis (1996) ArticleTitleSplanchnic ischaemia during laparoscopic cholecystectomy. Surg Endosc 10 324–326 Occurrence Handle10.1007/s004649910051 Occurrence Handle1:STN:280:BymB2s7mtlE%3D Occurrence Handle8779068
E Eleftheriadis K Kotzampassi K Papanotas N Heliadis K Sarris (1996) ArticleTitleGut ischaemia, oxidative stress and bacterial translocation in elevated abdominal pressure in rats. World J Surg 20 11–16 Occurrence Handle10.1007/s002689900002 Occurrence Handle1:STN:280:BymC2cfjsVE%3D Occurrence Handle8588401
GK Glantzounis AD Tselepis AP Tambuki TA Trikalinos AD Manataki DA Galaris EC Tsimoyiannis AM Kappas (2001) ArticleTitleLaparoscopic surgery-induced changes in oxidative stress markers in human plasma. . 15 1315–1319 Occurrence Handle1:STN:280:DC%2BD3MnotV2ksw%3D%3D
T Hauet D Mothes JM Goujon JL Caritez M Carretier L le Moyec M Eugene JP Tillement (1997) ArticleTitleTrimetazidine prevents renal injury in the isolated perfused pig kidney exposed to prolonged cold ischaemia. Transplantation 64 1082–1086 Occurrence Handle1:CAS:528:DyaK2sXntFSjsL4%3D Occurrence Handle9381535
E Haugen KA Nath (1999) ArticleTitleThe involvement of oxidative stress in the progression of renal injury. Blood Purif 17 58–65 Occurrence Handle10.1159/000014377 Occurrence Handle1:CAS:528:DyaK1MXlsF2gt7g%3D Occurrence Handle10449863
CF Islam RT Mathie MD Dinneen EA Kiely AM Peters PA Grace (1997) ArticleTitleIschaemia-reperfusion injury in the rat kidney: the effect of preconditioning. Br J Urol 79 842–847 Occurrence Handle10.1046/j.1464-410X.1997.00209.x Occurrence Handle1:STN:280:ByiA2cnht1M%3D Occurrence Handle9202547
AJ Kirsch TW Hensle DT Chang (1994) ArticleTitleRenal effects of CO2 insufflation: oliguria and acute renal dysfunction in a rat model. Urology 43 453–459 Occurrence Handle10.1016/0090-4295(94)90230-5 Occurrence Handle1:STN:280:ByuB3crhtlM%3D Occurrence Handle8154067
C Li RM Jackson (2002) ArticleTitleReactive species mechanisms of cellular hypoxia-reoxygenation injury. Am J Physiol Cell Physiol 282 C227–241 Occurrence Handle1:CAS:528:DC%2BD38XhtFGisLg%3D Occurrence Handle11788333
CS Lieber (1997) ArticleTitleRole of oxidative stress and antioxidant therapy in alcoholic and nonalcoholic liver diseases. Adv Pharmacol 38 601–628 Occurrence Handle1:CAS:528:DyaK2sXivVarsg%3D%3D Occurrence Handle8895826
A Meister (1994) ArticleTitleGlutathione-ascorbic acid antioxidant system in animals. J Biol Chem 269 9397–9400 Occurrence Handle1:CAS:528:DyaK2cXis1Kns7k%3D Occurrence Handle8144521
CE Murry RB Jenning KA Reimer (1986) ArticleTitlePreconditioning with ischaemia: a delay of lethal cell injury in ischemic myocardium. Circulation 74 1124–1136 Occurrence Handle3769170
T Ogawa Y Mimura N Hiki H Kanauchi M Kaminishi (2000) ArticleTitleIschaemic preconditioning ameliorates functional disturbance and impaired renal perfusion in rat ischaemia-reperfused kidneys. Clin Exp Pharmacol Physiol 27 997–1001 Occurrence Handle10.1046/j.1440-1681.2000.03378.x Occurrence Handle1:CAS:528:DC%2BD3cXovVWrur8%3D Occurrence Handle11117237
H Ohkawa N Ohishi K Yagi (1979) ArticleTitleAssay for lipid peroxidase in animal tissues by thiobarbituric acid reaction. Anal Biochem 95 351–358 Occurrence Handle1:CAS:528:DyaE1MXksFaisbk%3D Occurrence Handle36810
C O’Malley AJ Cunningham (2001) ArticleTitlePhysiologic changes during laparoscopy. Anesthesiol Clin North Am 19 1–19 Occurrence Handle1:STN:280:DC%2BD3MzgtF2mtA%3D%3D
C Peralta N Prats C Xaus E Gelpi J Rosello-Catafau (1999) ArticleTitleProtective effect of liver ischaemic preconditioning on liver and lung injury induced by hepatic ischaemia-reperfusion in the rat. Hepatology 30 1481–1489 Occurrence Handle1:STN:280:DC%2BD3c%2Fkt1ehtg%3D%3D Occurrence Handle10573528
S Richter A Olinger U Hildebrandt MD Menger B Vollmar (2001) ArticleTitleLoss of physiologic hepatic blood flow (“hepatic arterial buffer response”) during CO2-pneumoperitoneum in the rat. Anesth Analg 93 872–877 Occurrence Handle1:STN:280:DC%2BD3Mrisl2lsg%3D%3D Occurrence Handle11574348
K Sato T Kawamura R Wakusawa (2000) ArticleTitleHepatic blood flow and function in elderly patients undergoing laparoscopic cholecystectomy. Anesth Analg 90 1198–1202 Occurrence Handle1:STN:280:DC%2BD3c3ksFWgtQ%3D%3D Occurrence Handle10781479
A Schachtrupp Ch Toens J Hoer B Klosterhalfen AG Lawong V Schumpelick (2002) ArticleTitleA 24-h pneumoperitoneum leads to multiple organ impairment in a porcine model. J Surg Res 106 37–45 Occurrence Handle10.1006/jsre.2002.6421 Occurrence Handle1:STN:280:DC%2BD38zot1GltQ%3D%3D Occurrence Handle12127806
M Schafer H Sagesser J Reichen L Krahenbuhl (2001) ArticleTitleAlterations in hemodynamics and hepatic and splanchnic circulation during laparoscopy in rats. Surg Endosc 15 1197–1201 Occurrence Handle10.1007/s004640080159 Occurrence Handle1:STN:280:DC%2BD3MnotV2gsg%3D%3D Occurrence Handle11443454
F Serracino-Inglott NA Habib RT Mathie (2001) ArticleTitleHepatic ischaemia-reperfusion injury. Am J Surg 181 160–166 Occurrence Handle10.1016/S0002-9610(00)00573-0 Occurrence Handle1:CAS:528:DC%2BD3MXjtFGgtr8%3D Occurrence Handle11425059
KC Sharma G Kabinoff Y Ducheine J Tierney RD Brandstetter (1997) ArticleTitleLaparoscopic surgery and its potential for medical complications. Heart Lung 26 52–64 Occurrence Handle1:STN:280:ByiC28rks1Q%3D Occurrence Handle9013221
H Sies (1997) ArticleTitleOxidative stress: oxidants and antioxidants. Exp Physiol 82 291–295 Occurrence Handle1:CAS:528:DyaK2sXivFemtLc%3D Occurrence Handle9129943
LM Walker JL York SZ Imam SF Ali KL Muldrew PR Mayeux (2001) ArticleTitleOxidative stress and reactive oxygen species generation during renal ischaemia. Toxicol Sci 63 143–148 Occurrence Handle10.1093/toxsci/63.1.143 Occurrence Handle1:CAS:528:DC%2BD3MXmt12rs7k%3D Occurrence Handle11509754
DM Yellon A Dana (2000) ArticleTitleThe preconditioning phenomenon: a tool for the scientist or a clinical reality? Circ Res 87 543–550 Occurrence Handle11009558
S Yilmaz E Ateş C Polat T Köken Ç Tokyol G Akbulut Ö Gökçe (2003) ArticleTitleIschaemic preconditioning decreases laparoscopy-induced oxidative stress in small intestine. Hepatogastroenterology 50 .
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yilmaz, S., Koken, T., Tokyol, C. et al. Can preconditioning reduce laparoscopy-induced tissue injury? . Surg Endosc 17, 819–824 (2003). https://doi.org/10.1007/s00464-002-9096-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-002-9096-z