Abstract
Dysphagia in patients with lung cancer is usually due to direct invasion from bronchogenic carcinomas or nodal localizations, while metastases from distant lung neoplasms are considered rare. We report a case of a smooth esophageal narrowing secondary to intramural metastasis from pulmonary adenocarcinoma in a patient with no previous history of neoplasia. Since standard linear echoendoscope could not overpass the malignant stricture, we obtained a histological diagnosis by fine-needle aspiration biopsy using an echobronchoscope (EBUS), due to its lower diameter. The EBUS scope represents a valuable tool to obtain cytological specimens in patients with esophageal strictures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Clinical Conundrum
In May 2017, a 63-year-old Caucasian woman was admitted to our hospital because of a 3-month history of worsening dysphagia to solids. Her medical history was positive for type two diabetes and arterial hypertension and she declared cigarette consumption for 40 years. Endoscopic examination showed a smooth, not-occluding stricture of the mid-esophagus, with negative histology from biopsies of the overlying mucosa.
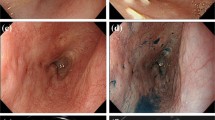
The patient underwent endoscopic ultrasonography (EUS) of the esophagus; since gastrointestinal echoendoscope failed to overpass the esophageal narrowing, EUS was performed using an echobronchoscope, in order to allow tissue sampling. EUS showed a 20-mm-long 9-mm-large hypo-echogenic thickening of the esophageal wall with loss of stratification of submucosal and muscular layers, and no extra-esophageal lesions (Fig. 1). Fine-needle aspiration (FNA) was conducted using a 22-gauge needle, and pathological evaluation of the obtained specimen was made (Fig. 2). A total body contrast-enhanced CT scan revealed a 30 mm mass of the inferior right pulmonary lobe, and an esophageal thickening (Fig. 3). No mediastinal lymphadenopathy or other distant metastases were seen. A 18-FDG positron emission tomography (PET) confirmed those findings showing a hypermetabolic lesion of the inferior right pulmonary lobe and hypermetabolic thickening of the esophageal wall (Fig. 4).
What is the Diagnosis?
Pathological examination from EUS-guided FNA showed mucin and epithelial cells with pleomorphic nuclei and clear cytoplasm mostly arranged in papillary and tubular structures; a fragment of muscularis propria was present and infiltrated by neoplastic cells, confirming that samples were obtained from the esophageal wall (Fig. 2). No lymphocytes were found. Immunohistochemistry, performed according to the peroxidase-antiperoxidase method, was positive for Napsin (Fig. 5), CK7 and TTF1, while CDX2 negative. The final diagnosis was pulmonary adenocarcinoma. Testing for exons 18, 19, 20, and 21 of Epidermal Growth Factor Receptor (EGFR) mutations were all negative. The patient received three chemotherapy cycles with cisplatin 75 mg/mq plus pemetrexed. At follow-up visit she reported improvement of dysphagia, with good tolerance of both semisolid and solid food. Three months of follow-up CT scan and esophagoscopy showed a reduction in primitive tumor size and a moderate improvement of the esophageal narrowing.
Discussion
Dysphagia in patients with lung cancer is usually secondary to direct invasion from bronchogenic carcinomas or nodal localizations, while metastases from distant lung neoplasms are considered rare [1]. Although autoptic studies report a high incidence of such entity [2], literature on en vivo cases is scarce, leading to a poor knowledge of its prognosis and no clear indications about optimal management. This case is peculiar because dysphagia was the presenting symptom of the disease, as the patient had not been diagnosed as any carcinoma previously, while in other reports patients usually develop esophageal metastases months or years after the primary diagnosis. This aspect, together with the normal look of esophageal mucosa, made the diagnosis challenging and echoendoscopic evaluation has been a key tool for the diagnosis.
Given the importance of endosonographic evaluation and fine-needle aspiration to obtain submucosal tissue samples, we aim to underline the potential role of echobronchoscope, in cases of not-occluding esophageal strictures. Indeed, one of the main technical limitations of linear echoendoscope is its large diameter (about 11 mm), while radial echoendoscope has a thinner diameter but it does not allow FNA. Echobronchoscopes do allow FNA performance, yet presenting a thin diameter (6 mm) [3, 4]. Thus, EBUS endoscope is a valid tool to perform endosonographic study of submucosal lesions of the esophagus when evaluation by standard echoendoscopes is limited.
References
Oka T, Ayabe H, Kawahara K, Tagawa Y, Hara S, Tsuji H, Kusano H, Nakano M, Tomita M. Esophagectomy for metastatic carcinoma of the esophagus from lung cancer. Cancer. 1993;71(10):2958–61.
Antler AS, Ough Y, Pitchumoni CS, Davidian M, Thelmo W. Gastrointestinal metastases from malignant tumors of the lung. Cancer. 1982;49:170–2.
Gupta K, Mallery S. Small-caliber endobronchial ultrasonic videoscope: successful transesophageal and transgastric FNA after failed passage of a standard ultrasonic endoscope. Gastrointest Endosc. 2007. https://doi.org/10.1016/j.gie.2007.02.025.
Buxbaum JL, Eloubeidi MA. Transgastric endoscopic ultrasound (EUS) guided fine needle aspiration (FNA) in patients with esophageal narrowing using the ultrasonic bronchovideoscope. Dis Esophagus. 2011;24:458–61. https://doi.org/10.1111/j.1442-2050.2011.01179.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Forti, E., Bonato, G., Dioscoridi, L. et al. A Smooth Esophageal Stricture Causing Dysphagia. Dysphagia 33, 399–402 (2018). https://doi.org/10.1007/s00455-018-9891-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-018-9891-x