Abstract
Dysphagia is common in older adults and associated with increased socioeconomic burdens. Recently, sarcopenia is considered to be a possible contributor for dysphagia. The purpose of this study is to investigate the association of dysphagia with sarcopenia in a geriatric population in Korea. This is a cross-sectional study using data from the Korean Longitudinal Study on Health and Aging (KLoSHA). Community-dwelling men and women aged 65 years and older without common causes of dysphagia in Seongnam City, Korea were included (N = 236). Dysphagia was screened using Standardized Swallowing Assessment. Appendicular skeletal muscle mass was calculated by dual-energy X-ray absorptiometry. Grip strength and long-distance corridor walk were assessed. Of 236 subjects, 54 (22.9%) showed dysphagia and 38 (16.1%) showed sarcopenia. Fourteen (5.9%) participants were diagnosed with sarcopenic dysphagia. In multiple logistic regression analysis for dysphagia, sarcopenia was the only significant variable with odds ratio of 2.738 (95% confidence interval 1.160–6.466). Sarcopenia was associated with increased risk of dysphagia in community-dwelling older adults having no common causes of dysphagia even after adjusting for possible confounders. A prospective study with a larger sample size is needed to reveal their causal relationship in the future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dysphagia is one of the common symptoms among older adults. Overall prevalence of dysphagia in community-dwelling older adults is about 15%, ranging from 5 to 72% [1]. Dysphagia increases the risk of aspiration pneumonia and choking that can lead to hospital admission or even death. It increases socioeconomic burdens and reduces quality of life of patients substantially [2, 3]. Therefore, timely diagnosis and treatment including swallowing rehabilitation and diet modification are important. Although common causes of dysphagia in older adults include neurological diseases (such as stroke, Parkinson’s disease, and Alzheimer disease) and chronic illnesses such as chronic obstructive lung disease [4, 5], the exact causes of dysphagia are unclear in many cases [6].
In recent years, it has been suggested that sarcopenia may be closely associated with dysphagia in the elderly population [7, 8]. Sarcopenia is characterized by progressive and generalized loss of skeletal muscles. It is recognized as an independent condition with an ICD-10-CM code [9]. Sarcopenia is diagnosed when low skeletal muscle mass with either muscle weakness or poor physical performance is apparent [10]. Kuroda et al. [11] used the term ‘sarcopenic dysphagia’ first. Since then, several Japanese studies have suggested that dysphagia is significantly associated with sarcopenia in older adults [12,13,14]. However, these studies included older adults staying in hospital or other facilities which might increase the risk of selection bias. In addition, subjects with cognitive dysfunction or chronic illnesses related to dysphagia were also included, making it difficult to define pure sarcopenic dysphagia. Therefore, the objective of this study was to investigate the association of sarcopenia with dysphagia in community-dwelling older adults without common causes of dysphagia using data from the Korean Longitudinal Study on Health and Aging (KLoSHA).
Methods
Study Population
This study was a part of the KLoSHA, a population-based, prospective cohort study on health status and common geriatric disease in elderly Koreans [15]. At baseline, 992 participants living in Seongnam City were enrolled from September 2005 to September 2006. At the first follow-up period from May 2010 to March 2012, 165 participants died while 303 participants did not respond or agree to the invitation for follow-up assessment. Of the remaining 524 participants, 130 participants who were not assessed by standardized Swallowing Assessment (SSA) or corridor walk test were excluded. Participants with history of diseases (stroke, n = 44; Parkinson’s disease, n = 13; chronic obstructive pulmonary disease, n = 5; temporomandibular joint disorder, n = 3; cognitive impairment, n = 93) that could cause dysphagia were excluded. Thus, 236 participants were included for analysis in this study (Fig. 1). Mini Mental Status Examination (MMSE) was used for global cognition measurement [16]. Cognitive impairment was defined as MMSE score of less than 23 which was corrected according to education level. No patient had a history of head and neck cancer.
Dysphagia Assessment
Swallowing was assessed using the Standardized Swallowing Assessment (SSA) [17]. The Korean version of SSA was used. It has been validated in nursing home setting [18]. The SSA consists of three sections. In the first section, levels of alertness, responsiveness, and availability of upright position with head control were evaluated. In the second section, voluntary cough, salivary management, ability to lick top and bottom lips, respiratory function, and vocal quality were assessed. If all items in sections 1 and 2 were passed, the participant underwent examination for section 3. A spoon of water (5 ml) was tried three consecutive times followed by a trial of a half glass of water (about 120 ml). Coughing, choking, breathlessness during swallowing, and wet voice after swallowing were considered as abnormal findings. An overall judgment of swallowing safety was made by a trained occupational therapist. Participants who showed any abnormalities in these three sections were categorized to the dysphagia group.
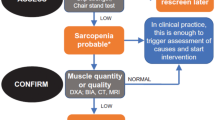
Sarcopenia Assessment
Sarcopenia was defined by low skeletal muscle mass, low hand grip strength, and low physical performance based on the European Working Group on Sarcopenia in Older People (EWGSOP) guidelines [10]. Cut-off values were determined according to the Asian Working Group for Sarcopenia diagnostic criteria [19]. Muscle mass was measured with a dual-energy X-ray absorptiometry (Lunar Corporation, Madison, WI, USA). Muscle mass of the four extremities was defined as appendicular skeletal muscle mass (ASM). Skeletal muscle mass index (SMI) was defined as ASM/height2 (kg/m2). Cut-off values of SMI for men and women were 7.0 kg/m2 and 5.4 kg/m2, respectively.
Handgrip strength of the dominant hand was measured using a digital grip strength dynamometer (Sammons Preston, Bolingbrook, IL, USA). Two consecutive attempts with 1-min interval were performed in a neutral position of the arm, forearm, and wrist. The Asian Working Group for Sarcopenia cut-off values for handgrip strength were < 26 kg for men and < 18 kg for women.
Physical performance was assessed by long-distance corridor walk. Participants were instructed to walk 400 m in a hall way without running at a pace they could maintain. The cut-off value of 362 s was used according to the study of Newman et al. [20]. If participants failed to complete the test or took more than 362 s, they were classified as having low physical performance.
Other Variables
As functional assessment tools, the Korean ADL (K-ADL) scale for basic activities and the Korean Instrumental ADL (K-IADL) scale for instrumental activities were used [21]. K-ADL consisted of seven domains (dressing, washing face and hands, bathing, eating, performing transfers, toileting, and continence) while K-IADL consisted of ten domains (grooming, doing housework, preparing meals, doing laundry, taking a short trip, using transportation, shopping, managing money, using a telephone, and taking medicine). K-ADL and K-IADL ranged from 7 to 21 points and 10 to 37 points, respectively, with lower score indicating more independent state. Participants answered questionnaires with the aid of trained nurses.
The geriatric quality of life scale (G-QOL) [22] was used to assess quality of life. It consisted of 25 items assessing physical and psychological health, independence, relationship, environment, religions, and global quality of life. Each item was scored from 1 (not satisfactory) to 4 (fully satisfactory). Total score ranged from 25 (no quality of life) to 100 (perfect quality of life).
Smoking and alcohol history were assessed using self-reported questionnaires. Subjects who were currently smoking (those who answered “Yes” to the question “Are you currently smoking?”) were defined as smokers. Alcohol intake was calculated by adding total number of standard drinking units (one bottle of beer, one glass of wine, or one unit of Soju (a clear distilled liquor that is popular in Korea), approximately equivalent to 10 g of ethanol) per month.
Calcium, albumin, total cholesterol, and low-density lipoprotein cholesterol levels were measured enzymatically using an autoanalyzer (Hitachi 747; Hitachi, Ltd, Tokyo, Japan). Serum total 25[OH]D concentration was measured using Diels–Alder derivatization and ultrahigh performance liquid chromatography-tandem mass spectrometry (Waters, Milford, MA, USA).
Statistical Analyses
Demographic data are reported as mean ± standard deviation (SD) or number (percentages). Differences were analyzed using Welch’s t test for continuous variables and χ2 test for categorical variables. Multivariate logistic regression analysis was performed to determine variables that were independently associated with the presence of dysphagia. Variables with p < 0.25 in univariate analysis as well as age and gender were entered into the regression model for multivariate analysis. Effect sizes were expressed as odds ratios (ORs) with 95% confidence intervals (CIs). Two-sided p values < 0.05 were deemed to be statistically significant. All analyses were performed using IBM SPSS Statistics V21.0 (Armonk, NY, USA).
Results
Baseline characteristics of study subjects are presented in Table 1. Mean age of subjects was 76.6 years. Of 236 subjects, 114 (48.3%) were males. Fifty-four (22.9%) participants showed dysphagia and 38 (16.1%) participants were diagnosed with sarcopenia. Fourteen (5.9%) subjects had sarcopenia and dysphagia simultaneously (or sarcopenic dysphagia). Subjects with dysphagia showed more sarcopenia than subjects without dysphagia (25.9% vs. 13.2%). G-QOL of participants with dysphagia was lower than that of participants without dysphagia (57.0 vs. 60.5), although the difference between the two was not statistically significant. In forced entry logistic regression analysis, sarcopenia was the only significant risk factor for dysphagia, with an odds ratio of 2.738 (95% confidence interval 1.160–6.466) (Table 2).
Discussion
This study showed that sarcopenia was an independent risk factor for dysphagia in Korean older adults living in the community without common causes of dysphagia. The risk for dysphagia was 2.7 times higher in participants with sarcopenia compared to that in those without sarcopenia (Table 2). The prevalence of dysphagia was 22.9% and that of sarcopenic dysphagia was 5.9%. The total number of subjects with dysphagia regardless of underlying diseases was 131. Of these subjects, only 77 (58.8%) had related etiologies (25 with stroke, 6 with Parkinson’s disease, 2 with COPD, 3 with temporomandibular joint disorder, and 41 with cognitive impairment). This suggests that the chance to meet elderly patients with dysphagia without common etiology is relatively high in geriatric care and the need to evaluate sarcopenia in this population.
Few studies have investigated the underlying mechanism of sarcopenic dysphagia. Maeda et al. [23] have suggested that generalized sarcopenia may cause impaired swallowing function by decreased tongue pressure. In addition, changes of musculature associated with swallowing mechanism accompanied by aging including decreased muscle mass of masseter and tongue, increased fatty infiltration, and atrophied type I fiber have been suggested as possible pathophysiology of dysphagia in older adults [7, 24]. When these changes of swallowing related musculature are combined with physical inactivity, chronic illness, or malnutrition (aggravating factors for sarcopenic dysphagia) which is common in older adults, the chance of dysphagia occurrence could increase [8].
Considering possible mechanisms of sarcopenic dysphagia, strategies to improve the strength and function of swallowing related musculature including tongue resistance exercise program, Shaker exercise, and chin tuck resistance exercise could be provided as treatment options [25, 26]. To overcome the effect of aggravating factors on sarcopenic dysphagia such as physical inactivity and malnutrition, interventions to increase skeletal muscle mass including resistance training and essential amino acid supplementation could be recommended [27]. Oral care and food modification should also be taken into account to reduce adverse events associated with sarcopenic dysphagia such as aspiration pneumonia [28]. If all these treatments are offered comprehensively, sarcopenic dysphagia could improve and its related complication could decrease. Although Maeda et al. [29] have reported that sarcopenic dysphagia could be improved with comprehensive rehabilitation approach including nutritional support, clinical trials are needed to prove the efficacy of possible suggested interventions for sarcopenic dysphagia.
Study Limitations
This study has several limitations. First, dysphagia was evaluated by one screening tool, SSA. Although test such as video fluoroscopic swallowing study makes it possible to diagnose dysphagia more accurately, it has disadvantages of high cost, time, and radiation. SSA evaluates both symptoms and signs of dysphagia. It has been validated as a good screening tool for dysphagia [30]. Second, the prevalence of sarcopenic dysphagia in this study (5.9%) was lower than that reported in the previous studies (ranging from 26 to 42.3%) [14, 23, 31]. This higher prevalence of sarcopenic dysphagia in previous studies could be due to different study population (institutionalized older adults). It is well known that the prevalence of dysphagia is much higher in hospitalized or nursing homes [32]. In contrast, only community-dwelling older adults without common causes of dysphagia were included in this study. Subjects in this study showed independent activity with near normal ADL and IADL scores (Table 1). Considering that the prevalence of dysphagia in community-dwelling elderly was about 15% [1], the prevalence of sarcopenic dysphagia at about 6% in our study might be appropriate for community-dwelling independent older adults. Third, since this study was cross-sectional, the causal relationship between sarcopenia and dysphagia could not be evaluated.
Conclusion
Among 236 community-dwelling older adults without common causes of dysphagia, 23% showed dysphagia and 6% showed sarcopenic dysphagia. Sarcopenia was associated with increased risk of dysphagia in these subjects. Due to the cross-sectional nature and small sample size of this study, a prospective cohort study with a larger sample size is needed to reveal their causal relationship. An interventional study is also needed to improve dysphagia in such sarcopenic dysphagia population in the future.
References
Madhavan A, Lagorio LA, Crary MA, Dahl WJ, Carnaby GD. Prevalence of and risk factors for dysphagia in the community dwelling elderly: a systematic review. J Nutr Health Aging. 2016;20(8):806–15.
Cabré M, Serra-Prat M, Force L, Almirall J, Palomera E, Clavé P. Oropharyngeal dysphagia is a risk factor for readmission for pneumonia in the very elderly persons: observational prospective study. J Gerontol. 2014;69(3):330–7.
Ekberg O, Hamdy S, Woisard V, Wuttge-Hannig A, Ortega P. Social and psychological burden of dysphaiga: its impact on diagnosis and treatment. Dysphagia. 2002;17(2):139–46.
Roy N, Stemple J, Merrill RM, Thomas L. Dysphagia in the elderly: preliminary evidence of prevalence, risk factors, and socioemotional effects. Ann Otol Rhinol Laryngol. 2007;116(11):858–65.
Suh MK, Kim H, Na DL. Dysphagia in patients with dementia: alzheimer versus vascular. Alzheimer Dis Assoc Disord. 2009;23(2):178–84.
Yeom J, Song YS, Lee WK, Oh BM, Han TR, Seo HG. Diagnosis and clinical course of unexplained dysphagia. Ann Rehabil Med. 2016;40(1):95–101.
Wakabayashi H. Presbyphagia and sarcopenic dysphagia: association between aging, sarcopenia, and deglutition disorders. J Frailty Aging. 2014;3(2):97–103.
Sakai K, Sakuma K. Sarcopenic dysphagia as a new concept. Frailty sarcopenia—onset, dev clin challenges. London: IntechOpen; 2017. https://doi.org/10.5772/intechopen.68791.
Anker SD, Morley JE, von Haehling S. Welcome to the ICD-10 code for sarcopenia. J Cachexia Sarcopenia Muscle. 2016;7(5):512–4.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: european consensus on definition and diagnosis. Age Ageing. 2010;39(4):412–23.
Kuroda Y, Kuroda R. Relationship between thinness and swallowing function in japanese older adults: implications for sarcopenic dysphagia. J Am Geriatr Soc. 2012;60(9):1785–6.
Shiozu H, Higashijima M, Koga T. Association of sarcopenia with swallowing problems, related to nutrition and activities of daily living of elderly individuals. J Phys Ther Sci. 2015;27(2):393–6.
Wakabayashi H, Matsushima M, Uwano R, Watanabe N, Oritsu H, Shimizu Y. Skeletal muscle mass is associated with severe dysphagia in cancer patients. J Cachexia Sarcopenia Muscle. 2015;6(4):351–7.
Maeda K, Akagi J. Sarcopenia is an independent risk factor of dysphagia in hospitalized older people. Geriatr Gerontol Int. 2016;16(4):515–21.
Park JH, Lim J. An overview of the Korean Longitudinal Study on health and aging. Mov Disord. 2007;4(2):84.
Lee DY, Lee KU, Lee JH, Kim KW, Jhoo JH, Kim SY, et al. A normative study of the CERAD neuropsychological assessment battery in the Korean elderly. J Int Neuropsychol Soc. 2004;10(1):72–81.
Perry L. Screening swallowing function of patients with acute stroke. Part two: detailed evaluation of the tool used by nurses. J Clin Nurs. 2001;10(4):474–81.
Park YH, Han HR, Oh S, Chang H. Validation of the Korean version of the standardized swallowing assessment among nursing home residents. J Gerontol Nurs. 2014;40(2):26–35.
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, et al. Sarcopenia in Asia: consensus report of the Asian working group for sarcopenia. J Am Med Dir Assoc. 2014;15(2):95–101.
Newman AB, Simonsick EM, Naydeck BL, Boudreau RM, Kritchevsky SB, Nevitt MC, et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. J Am Med Assoc. 2006;295(17):2018–26.
Kang S, Choi S, Lee B, Kwon J. The reliability and validity of the Korean Instrumental Activities of Daily Living (K-IADL). J Korean Neurol Assoc. 2002;20(1):8–14.
Lee HS, Kim DK, Ko HJ, Ku HM, Kwon EJ, Kim JH. The standardization of “Geriatric Quality of Life scale”. Korean J Clin Psychol. 2003;22(4):859–81.
Maeda K, Akagi J. Decreased tongue pressure is associated with sarcopenia and sarcopenic dysphagia in the elderly. Dysphagia. 2015;30(1):80–7.
Humbert IA, Robbins JA. Dysphagia in the elderly. Phys Med Rehabil Clin N Am. 2008;19(4):853–66.
Yoon WL, Khoo JKP, Liow SJR. Chin tuck against resistance (CTAR): new method for enhancing suprahyoid muscle activity using a shaker-type exercise. Dysphagia. 2014;29(2):243–8.
Robbins J, Gangnon RE, Theis SM, Kays SA, Hewitt AL, Hind JA. The effects of lingual exercise on swallowing in older adults. J Am Geriatr Soc. 2005;53(9):1483–9.
Cruz-Jentoft AJ, Landi F, Schneider SM, Zúñiga C, Arai H, Boirie Y, et al. Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing. 2014;43(6):748–59.
Marik PE, Kaplan D. Aspiration pneumonia and dysphagia in the elderly. Chest. 2003;124(1):328–36.
Maeda K, Akagi J. Treatment of sarcopenic dysphagia with rehabilitation and nutritional support: a comprehensive approach. J Acad Nutr Diet. 2016;116(4):573–7.
Park YH, Bang HL, Han HR, Chang HK. Dysphagia screening measures for use in nursing homes: a systematic review. J Korean Acad Nurs. 2015;45(1):1–13.
Maeda K, Takaki M, Akagi J. Decreased skeletal muscle mass and risk factors of sarcopenic dysphagia: a prospective observational cohort study. J Gerontol. 2017;72(9):1290–4.
Clavé P, Shaker R. Dysphagia: current reality and scope of the problem. Nat Rev Gastroenterol Hepatol. 2015;12(5):259–70.
Acknowledgements
Ki Woong Kim received a Grant from the Korean Health Technology R&D project funded by the Ministry of Health and Welfare, Republic of Korea (Grant No. HI09C1379 [A092077]). Nam-Jong Paik received a grant from the Seoul National University Bundang Hospital (Grant No. 12-2013-007).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no other conflict of interest except for the grants mentioned above.
Informed Consent
Written informed consent was obtained from all study volunteers.
Rights and permissions
About this article
Cite this article
Cha, S., Kim, WS., Kim, K.W. et al. Sarcopenia is an Independent Risk Factor for Dysphagia in Community-Dwelling Older Adults. Dysphagia 34, 692–697 (2019). https://doi.org/10.1007/s00455-018-09973-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-018-09973-6