Abstract
Oropharyngeal dysphagia has features of geriatric syndromes and is strongly associated with sarcopenia. In this cross-sectional study, we aimed to evaluate the association between dysphagia and sarcopenia, in a practical way, accompanied by comprehensive geriatric assessment. Dysphagia and sarcopenia were defined by the EAT-10 and SARC-F questionnaires, respectively. Cognition and mood, was evaluated by the Mini-mental State Examination (MMSE) and Geriatric Depression Scale (GDS), respectively. Physical performance was assessed by the Timed up and Go Test (TUG) and muscle strength was determined by Hand Grip Strength (HGS). Functionality was stated by Katz and Lawton Indexes. Serum levels of hemoglobin, triglyceride, albumin, and total cholesterol were recorded. A total of 512 (151 male/361 female) patients age 60 and older were included in the study. Prevalences of dysphagia and sarcopenia were 23% and 40.6%, respectively. In multivariate analysis sarcopenia (OR:2.596, p = 0.008), depressive symptoms (OR:1.115, p < 0.001), and lower KATZ scores (OR:0.810, p = 0.036) were independently related with dysphagia. Dysphagic patients with sarcopenia had lower scores on the Katz and Lawton scales (p < 0.001, rpb = 0.380 and p < 0.001, rpb = 0.447 respectively) and TUG performances were worse (p = 0.009, rpb = − 0.254). Serum hemoglobin and albumin levels were significantly low in dysphagic patients with sarcopenia (p < 0.001, rpb = 0.345, p = 0.008, rpb = 0.243). Dysphagia is independently associated with sarcopenia, depressive symptoms, and functionality. Dysphagia coexist with sarcopenia is associated with worse clinical consequences than without sarcopenia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
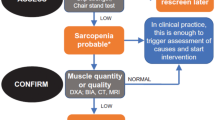
Dysphagia is defined as symptom of difficulty in swallowing function and is observed in 13–35% of the geriatric population [1]. In recent years, it has been recognized that oropharyngeal dysphagia has the features of geriatric syndromes, as it is highly prevalent in the geriatric population and it has common risk factors with other geriatric syndromes like multimorbidity and polypharmacy [2]. Additionally it is related with poor outcomes such as aspiration pneumonia, malnutrition, institutionalization, and mortality [2]. Dysphagia is often associated with underlying diseases such as Parkinson’s disease, dementia, and stroke but the exact causes of dysphagia are unclear in many cases [3, 4]. Dysphagia may also be associated with other geriatric syndromes like sarcopenia and may cause worse outcomes when accompanied by sarcopenia [5]. Sarcopenia is characterized by a decrease in muscle strength, muscle function, and muscle mass. The prevalence of sarcopenia in the geriatric population varies between 1 and 33% and the prevalence of such a wide range is due to differences in sarcopenia measurement techniques and cut off values [6]. Dual energy X-ray absorptiometry (DEXA) and Bio impedance analysis (BIA) are widely used to measure skeletal muscle mass in research but are not practical to apply during clinical evaluation in outpatient clinics. The SARC-F, recommended for screening of sarcopenia in the EWGSOP2 is an easy questionnaire and has high specificity [7, 8]. Its validity and reliability has been achieved in many institutions and countries [9].
Loss of muscle strength and mass observed in sarcopenia is systematic [10]. Influence of respiratory muscles due to sarcopenia may affect respiratory function, and pharyngeal muscles may cause dysphagia [11]. A new term introduced in recent years is sarcopenic dysphagia [10, 12]. In 2013, in addition to the confirmation of dysphagia and sarcopenia according to the criteria defined in 5 items, the confirmation of decreased oropharyngeal muscle mass by imaging was added to the criteria [13, 14]. At present, the real prevalence of sarcopenic dysphagia is unknown, due to the difficulty of technical methods, but the inevitable association of sarcopenia and dysphagia is a fact. Screening tests, bedside swallowing evaluation tests, and advanced video fluoroscopic imaging can be performed to determine dysphagia [15,16,17]. Functional tests are the gold standard but are not practical for population studies, because they require swallowing specialists and technical equipment. The Eating Assessment Tool (EAT-10) is an easy and applicable test that can be used for screening of dysphagia in ambulatory patients [15].
The coexistence of sarcopenia and dysphagia has been shown in previous studies with a wide variety of methods. Here we aimed to investigate the relationship between sarcopenia and dysphagia, in a practical way by applying the SARC-F and EAT -10 questionnaires respectively, in the context of comprehensive geriatric evaluation and compare related clinical consequences in dysphagic patients with and without sarcopenia.
Methods
Participants
We conducted a cross sectional study and data was evaluated retrospectively. Patients at age 60 years and older, admitted to the geriatric outpatient clinic of a tertiary center between the dates of Nov 2018 and August 2019 were included in the study. The data of the patients’ first admission was evaluated. Patients with missing data, restricted mobility, severe dementia, head and neck cancer, or acute diseases with clinical deterioration were not included in the study. Comorbidities and number of medications were recorded and the Charlson comorbidity index (CCI) was calculated [18]. Anthropometric measures of the patients were taken. At time of first admission, fasting laboratory values including serum albumin, hemoglobin, triglycerides, and total cholesterol were recorded.
Dysphagia and Sarcopenia
Dysphagia was evaluated by the EAT-10 questionnaire [14]. EAT-10 consists of 10 items and each item is scored from 0 (no problem) to 4 (severe problem) with total score ranges between 0 and 40, while scores of 3 or more are defined as dysphagia. Sarcopenia was assessed by the SARC-F screening questionnaire [8]. This is a 5-item questionnaire with a total score of 10. Four or higher scores are assigned as sarcopenia.
Comprehensive Geriatric Assessment
The Katz and Lawton scales were applied to patients in order to evaluate dependency in activities of daily living (ADL) and instrumental activities of daily living (IADL), respectively [19, 20]. Higher scores in both scales represent functional independency. Mood was evaluated by the Geriatric depression scale (GDS). Higher scores indicate more depressive symptoms. Fourteen points and higher were defined as depression [21]. Cognition was assessed by the mini-mental state examination (MMSE), in which scores lower than 24 points state dementia [22]. Patients with MMSE scores lower than 9, representing severe dementia were not included in the study. Nutritional status was evaluated by the mini nutritional assessment-short form (MNA-SF) [23]. Hand grip strength (HGS) and the Timed up and go (TUG) test were performed for evaluation of muscle strength and muscle performance, respectively. A jamar hand dynamometer was used for measuring HGS. Three consecutive measurements with 30 s of rest after each measurements were taken from the dominant hand. Maximum grip strength values were taken for analysis. The TUG test was performed as patients sat on a standard armchair. At the directive of “go”, patients were instructed to stand up from the chair, walk to the line marked on the floor using a usual pace, turn around, walk back to the chair, and sit down again [24].
Approval of the study was obtained from the Local Ethics Committee. Informed consents were received from all patients.
Statistical Analysis
A descriptive analysis was performed based on Dysphagia status. Histogram and q–q plots were examined to assess the data normality. A two-sided independent samples t test and Mann Whitnay U test were conducted to compare the differences between continuous variables; while the Pearson Chi square test or Fisher exact test were used to compare differences between categorical variables. Phi correlation test was used to compare between categorical and continuous variables. Univariate and multiple binary logistic regression analysis were used to identify the risk factors of Dysphagia. Odds ratios (OR) were calculated with 95% confidence intervals (CI). Significant variables with potential for causal effect on Dysphagia at p < 0.250 on univariate analysis were taken into multiple models and backward stepwise selection was performed using likelihood ratio statistic at p < 0.10 stringency level. The calibration of the model was assessed using the Hosmer–Lemeshow goodness of fit test. p < 0.05 was considered as statistically significant. Point biserial and Phi correlation coefficients were calculated to determine effect size of variables in dysphagic patients with sarcopenia. Spearman’s rank correlation coefficients were calculated to check for multicollinearity. Analyses were conducted using SPSS version 22 and TURCOSA (Turcosa Analytics Ltd. Co., Turkey) statistical softwares. (https://turcosa.com.tr/).
Results
A total of 512 (151 male/361 female) patients were included in the study. The mean + standard deviation (range) age of the study population was 72.1 ± 7.3 (60–98). Patients with the diagnosis of diabetes mellitus (DM), hypertension, cerebrovascular diseases, chronic obstructive pulmonary diseases (COPD), Alzheimer’s, and Parkinson’s disease were 236 (46.1%), 336 (65.6%), 26 (5.1%), 32 (6.3%), 63 (12.3%), and 16 (3.1%), respectively. Prevalence of dysphagia and sarcopenia was 23% and 40.6%, respectively. Number of patients with both dysphagia and sarcopenia was 83 (16.6%). Patients with dysphagia were older (p = 0.011), more dependent in ADL and IADL (p < 0.001, p < 0.001), had more depressive symptoms (p < 0.001), and had lower MMSE scores (p = 0.038). Demographic characteristics of the patients and relation with dysphagia are represented in Table 1. In multivariate analysis, sarcopenia (OR:2.596, p = 0.008), depressive symptoms (OR:1.115, p < 0.001), and lower KATZ scores (OR:0.810, p = 0.036) were independently related with dysphagia (Table 2). Effect size of each significant variable in dysphagic patients in case of sarcopenia was pointed out by rpb and phi values. Dysphagic patients with sarcopenia had lower scores on ADL (p < 0.001, rpb = 0.380) and IADL (p < 0.001, rpb = 0.447). HGS was lower (p < 0.001, rpb = 0.434 and p = 0.038, rpb = 0.244 in male and female respectively) and TUG performances (p = 0.009, rpb = − 0.254) were worse. Serum levels of hemoglobin (p < 0.001, rpb = 0.345) and albumin (p = 0.008, rpb = 0.243) were significantly low in dysphagic patients with sarcopenia. However, triglyceride and total cholesterol level did not differ between the two groups. Comparison of variables between dysphagic patients with and without sarcopenia are shown in Table 3.
Correlations between all relevant variables with dysphagia yielded low to moderate relationship (r < 0.7) (Table 4). Distribution of EAT-10 and SARC-F scores of study population are shown in Fig. 1.
Discussion
We have observed the prevalence of dysphagia and sarcopenia as 23% and 40.6%, respectively. 16.6% of all participants and 72.2% of dysphagic patients had both sarcopenia and dysphagia. The term sarcopenic dysphagia should include sarcopenia in swallowing muscles alongside the dysphagia and the generalized sarcopenia [10, 25]. Though we did not show the sarcopenia in muscles working in swallowing function, we do not claim that our results define the entity of sarcopenic dysphagia. However, our findings promote the strong relationship between sarcopenia and dysphagia. The prevalence of sarcopenic dysphagia has been reported in a wide range, from 26% to 42.3% [10, 26, 27]. Actually, the assessment methods of sarcopenia and dysphagia were different throughout these studies, but the final conclusions were common, emphasizing the strong association between dysphagia and sarcopenia [6]. One of the possible underlying mechanisms of sarcopenic dysphagia is that, sarcopenia affects Type II fibers more than type I fibers and the swallowing muscles are heavily composed of type II fibers [6, 28]. Dysphagia associated with sarcopenia appears to be more severe than other types of dysphagia [5]. In our study, the total EAT-10 scores were significantly higher in dysphagic patients with sarcopenia. Dysphagic patients with sarcopenia had lower HGS. Laboratory results including serum Hb and albumin levels were lower in dysphagic patients with sarcopenia than without. However serum albumin levels did not differ between patients with and without dysphagia. Similarly, Wakabayahi et al. reported that sarcopenic dysphagia was associated with lower HGS, calf circumference, and serum albumin levels [5]. Functionality revealing dependency in ADL and IADL measured by performing Katz and Lawton scales yielded poor scores in dysphagic patients with sarcopenia with higher effect sizes than other variables (rpb = 0.380 rpb = 0.447). In addition, lower scores on the Katz scale were independently related with dysphagia. Basic functional impairment seems to be one of the high risk factors for dysphagia, as well as being one of the poor outcomes of sarcopenia [10]. Furthermore, dysphagia was independently associated with depressive symptoms besides sarcopenia and functionality in our results. Prevalence of depression among dysphagic patients was 63.6%. Hence, the data in literature is insufficient. Mood disorders, especially depression, are highly prevalent in patients with dysphagia and prevalence of depression in patients with dysphagia has been reported as 32.6 and 62.2% in ambulatory and hospitalized patients, respectively [29, 30]. There are many triggering factors for dysphagia in Parkinson’s disease, such as the stage and severity of disease. Indeed an independent relationship between depression and dysphagia has been shown in this patient group as well [31].
Essentially, in our study the MMSE scores were lower in patients with dysphagia, though cognitive status was not independently related with dysphagia. In agreement, Tagliaferri et al. observed a significant and negative correlation between EAT-10 scores and cognitive status but the relevance was not independent [32]. Recently, Özsürekçi et al. evaluated dysphagia in Alzheimer disease and observed the association of dysphagia with sarcopenia and cognitive impairment even in early stages of the disease [33]. We observed significantly lower MMSE scores in dysphagic patients with sarcopenia than without.
Parkinson’s disease, Alzheimer’s disease, and COPD all have high risk of dysphagia [4]. Albeit, these patient groups have been excluded from some studies to preclude the misleading interference of the results, we did not excluded patients with the above diagnosis and significant relation between dysphagia and sarcopenia continued after adjusting for these diseases.
Sarcopenia and dysphagia are both geriatric syndromes, which have attracted attention in recent years and have a significant impact on older individuals, resulting in poor outcomes. They are in a vicious cycle of mutual cause and effect with each other and geriatric syndromes such as malnutrition and depression [32, 34]. The elderly population needs to be screened for these geriatric syndromes. Fast, easy, and practical screening methods are needed to reach large audiences. In this case, questionnaires with high specificity like SARC-F and EAT-10 seem to be advantageous. In addition, patients who are positive in EAT-10 screening can be candidates for instrumental evaluation of swallowing and be directed.
This study has some limitations. First, we evaluated both sarcopenia and dysphagia with questionnaires. Determining skeletal muscle mass and defining sarcopenia according to the EWGSOP may yield more objective results with respect to sarcopenia. In addition, dynamic evaluation of swallowing function, though not easily applicable and practical is the gold standard for the diagnosis of dysphagia. Secondly, due to the cross sectional design of this study, we cannot argue for the causal relationship between dysphagia and sarcopenia.
In conclusion, while managing patients with dysphagia, a detailed geriatric evaluation is needed including sarcopenia, depression, and functionality. Our results support a comprehensive treatment approach while managing dysphagia that covers psychological interventions as well as rehabilitation, exercise, and nutritional support [29, 35].
References
Chen PH, Golub JS, Hapner ER, Johns MM. Prevalence of perceived dysphagia and quality-of-life impairment in a geriatric population. Dysphagia. 2009;24(1):1–6.
Baijens LW, Clavé P, Cras P, Ekberg O, Forster A, Kolb GF, Leners JC, Masiero S, Mateos-Nozal J, Ortega O, Smithard DG, Speyer R, Walshe M. European Society for Swallowing Disorders–European Union Geriatric Medicine Society white paper: oropharyngeal dysphagia as a geriatric syndrome. Clin Interv Aging. 2016;11:1403–28.
Yeom J, Song YS, Lee WK, Oh BM, Han TR, Seo HG. Diagnosis and clinical course of unexplained dysphagia. Ann Rehabil Med. 2016;40(1):95–101.
Cha S, Kim WS, Kim KW, Han JW, Jang HC, Lim S, Paik NJ. Sarcopenia is an independent risk factor for dysphagia in community-dwelling older adults. Dysphagia. 2019;34(5):692–7.
Wakabayashi H, Takahashi R, Murakami T. The Prevalence and prognosis of sarcopenic dysphagia in patients who require dysphagia rehabilitation. J Nutr Health Aging. 2019;23(1):84–8.
Zhao WT, Yang M, Wu HM, Yang L, Zhang XM, Huang Y. Systematic review and meta-analysis of the association between sarcopenia and dysphagia. J Nutr Health Aging. 2018;22(8):1003–9.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, Cooper C, Landi F, Rolland Y, Sayer AA, Schneider SM, Sieber CC, Topinkova E, Vandewoude M, Visser M, Zamboni M, Writing Group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), Extended Group for EWGSOP2. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48(1):16–31.
Malmstrom TK, Miller DK, Simonsick EM, Ferrucci L, Morley JE. SARC-F: a symptom score to predict persons with sarcopenia at risk for poor functional outcomes. J Cachexia Sarcopenia Muscle. 2016;7(1):28–36.
Bahat G, Yilmaz O, Kılıç C, Oren MM, Karan MA. Performance of SARC-F in regard to sarcopenia definitions, muscle mass and functional measures. J Nutr Health Aging. 2018;22(8):898–903.
Maeda K, Akagi J. Sarcopenia is an independent risk factor of dysphagia in hospitalized older people. Geriatrics Gerontol Int. 2015;16(4):515–21.
Cesari M, Pedone C, Chiurco D, Cortese L, Conte ME, Scarlata S, Incalzi RA. Physical performance, sarcopenia and respiratory function in older patients with chronic obstructive pulmonary disease. Age Ageing. 2012;41:237–41.
Kuroda Y, Kuroda R. Relationship between thinness and swallowing function in japanese older adults: implications for sarcopenic dysphagia. J Am Geriatr Soc. 2012;60(9):1785–6.
Wakabayashi H. Presbyphagia and sarcopenic dysphagia: association between aging, sarcopenia, and deglutition disorders. J Frailty Aging. 2014;3:97–103.
Mori T, Fujishima I, Wakabayashi H et al (2017) Development, reliability, and validity of a diagnostic algorithm for sarcopenic dysphagia. JCSM clinical reports vol 2(2). https://jcsm-clinical-reports.info/index.php/jcsm-cr/article/view/17. Accessed 5 Nov 2018.
Belafsky PC, Mouadeb DA, Rees CJ, Pryor JC, Postma GN, Allen J, Leonard RJ. Validity and reliability of the Eating Assessment Tool (EAT-10). Ann Otol Rhinol Laryngol. 2008;117:919–24.
Clavé P, Arreola V, Romea M. Accuracy of the volumeviscosity swallow test for clinical screening of oropharyngeal dysphagia and aspiration. Clin Nutr. 2008;27:806–15.
Azzolino D, Damanti S, Bertagnoli L, Lucchi T, Cesari M. Sarcopenia and swallowing disorders in older people. Aging Clin Exp Res. 2019;31(6):799–805.
Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47:1245–51.
Katz S, Akpom CA. 12. Index of ADL. Med Care. 1976;14:116–8.
Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–86.
Ertan T, Eker E. Reliability, validity, and factor structure of the geriatric depression scale in Turkish elderly: are there different factor structures for different cultures? Int Psychogeriatr. 2000;12:163–72.
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98.
Guigoz Y, Vellas B, Garry PJ. Assessing the nutritional status of the elderly: themini nutritional assessment as part of the geriatric evaluation. Nutr Rev. 1996;54:59–65.
Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–8.
Fujishima I, Fujiu-Kurachi M, Arai H, Hyodo M, Kagaya H, Maeda K, Mori T, Nishioka S, Oshima F, Ogawa S, Ueda K, Umezaki T, Wakabayashi H, Yamawaki M, Yoshimura Y. Sarcopenia and dysphagia: position paper by four professional organizations. Geriatr Gerontol Int. 2019;19(2):91–7.
Maeda K, Akagi J. Decreased tongue pressure is associated with sarcopenia and sarcopenic dysphagia in the elderly. Dysphagia. 2015;30(1):80–7.
Maeda K, Takaki M, Akagi J. Decreased skeletal muscle mass and risk factors of sarcopenic dysphagia: a prospective observational cohort study. J Gerontol. 2017;72(9):1290–4.
Ogawa N, Mori T, Fujishima I, Wakabayashi H, Itoda M, Kunieda K, Shigematsu T, Nishioka S, Tohara H, Yamada M, Ogawa S. Ultrasonography to measure swallowing muscle mass and quality in older patients with sarcopenic dysphagia. J Am Med Dir Assoc. 2018;19(6):516–22.
Kim JY, Lee YW, Kim HS, Lee EH. The mediating and moderating effects of meaning in life on the relationship between depression and quality of life in patients with dysphagia. J Clin Nurs. 2019;28(15–16):2782–9.
Verdonschot RJ, Baijens LW, Serroyen JL, Leue C, Kremer B. Symptoms of anxiety and depression assessed with the Hospital Anxiety and Depression Scale in patients with oropharyngeal dysphagia. J Psychosom Res. 2013;75(5):451–5.
Han M, Ohnishi H, Nonaka M, Yamauchi R, Hozuki T, Hayashi T, Saitoh M, Hisahara S, Imai T, Shimohama S, Mori M. Relationship between dysphagia and depressive states in patients with Parkinson’s disease. Parkinsonism Relat Disord. 2011;17(6):437–9.
Tagliaferri S, Lauretani F, Pelá G, Meschi T, Maggio M. The risk of dysphagia is associated with malnutrition and poor functional outcomes in a large population of outpatient older individuals. Clin Nutr. 2019;38(6):2684–9.
Özsürekci C, Arslan SS, Demir N, Çalışkan H, Şengül Ayçiçek G, Kılınç HE, Yaşaroğlu ÖF, Kızılarslanoğlu C, Doğrul TR, Balcı C, Sümer F, Karaduman A, Yavuz BB, Cankurtaran M, Halil MG. Timing of dysphagia screening in Alzheimer’s Dementia. JPEN J Parenter Enteral Nutr. 2019. https://doi.org/10.1002/jpen.1664(Epub ahead of print).
Wang H, Hai S, Liu Y, Cao L, Liu Y, Liu P, Zhou J, Yang Y, Dong B. Association between depressive symptoms and sarcopenia in older Chinese community-dwelling individuals. Clin Interv Aging. 2018;13:1605–11.
Yoshimura Y, Wakabayashi H, Bise T, Tanoue M. Prevalence of sarcopenia and its association with activities of daily living and dysphagia in convalescent rehabilitation ward inpatients. Clin Nutr. 2018;37(6 PT A):2022–8.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fırat Ozer, F., Akın, S., Soysal, T. et al. Relationship Between Dysphagia and Sarcopenia with Comprehensive Geriatric Evaluation. Dysphagia 36, 140–146 (2021). https://doi.org/10.1007/s00455-020-10120-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-020-10120-3