Abstract
Tongue strength is routinely evaluated in clinical swallowing evaluations since lingual weakness is an established contributor to dysphagia. Tongue strength may be clinically quantified by the maximum isometric tongue pressure (MIP) generated by the tongue against the palate; however, wide ranges in normal performance remain to be fully explained. Although orthodontic theory has long suggested a relation between lingual function and oral cavity dimensions, little attention has been given to the potential influence of oral and palatal structure(s) on healthy variance in MIP generation. Therefore, anterior and posterior tongue strength measures and oropalatal dimensions were obtained across 147 healthy adults (aged 18–88 years). Age was confirmed as a significant, independent predictor explaining approximately 10.2% of the variance in anterior tongue strength, but not a significant predictor of posterior tongue strength. However, oropalatal dimensions predicted anterior tongue strength with over three times the predictive power of age alone (p < .001). Significant models for anterior tongue strength (R 2 = .457) and posterior tongue strength (R 2 = .283) included a combination of demographic predictors (i.e., age and/or gender) and oropalatal dimensions. Palatal width, estimated tongue volume, and gender were significant predictors of posterior tongue strength (p < .001). Therefore, oropalatal dimensions may warrant consideration when accurately differentiating between pathological lingual weakness and healthy individual difference.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Reduced tongue strength is a promising target for swallowing rehabilitation as lingual weakness is a frequently cited contributor to the deleterious and potentially life-threatening condition of dysphagia [1,2,3]. Fortunately, lingual strengthening and skill training protocols have shown potential to improve swallowing function [4,5,6]. Determining candidacy for lingual interventions, however, has been muddled by the great variability in healthy “tongue strength”, represented by the measurement of maximum isometric tongue pressure generated against the palate [7,8,9,10,11,12,13,14,15,16,17]. Thus, a one-size-fits-all benchmark for lingual weakness has largely eluded researchers and clinicians. Currently, there is a need to differentially diagnose lingual weakness from normal variation to accurately identify persons most likely to benefit from lingual training protocols.
Numerous investigations have sought to delineate healthy ranges of tongue strength (i.e., maximum isometric tongue pressure; MIP) [7,8,9,10,11,12,13,14,15,16,17]. Across this literature, influential factors on MIP have emerged (e.g., age, gender, race/ethnicity, task feedback, and tongue region); however, wide ranges of individual performance, interactions among these factors, and equivocal reports of a gender effect remain to be fully explained [7, 11, 14, 17]. Measurement of MIP in the literature has been widely conducted by placing a sensor between the tongue and the palate, as the palate serves as a contact platform for generating lingual–palatal pressure. The tongue’s hydrostatic properties allow it to compress against the palate and to functionally adapt to the individual shape of the palate during pressure generation. Therefore, a potentially under-recognized contributor to normal variability may be the dimensions of the palate, that is, the potential “palatal” contribution to lingual–palatal pressure generation. Researchers collecting samples of normative lingual–palatal pressures, using sensor configurations based on either fixed distances or anatomically-defined sensor placements, have hypothesized that the wide variability in lingual pressure generation noted across individuals may be attributed to individual differences in oral and palatal morphology [11, 18].
Orthodontic theory also has a long history of interest in the harmonious relation among palatal morphology, oral structure, and lingual function [19, 20]. A seminal investigation by Kydd and Toda [19] reported the influence of palatal shape (i.e., “round”, “peaked or narrow”, or “flat”) on the magnitude of lingual–palatal swallowing pressures (LSPs). McGlone and Proffit [20] later identified weak, positive correlations between the size of the oral cavity in nine healthy children and LSPs. Researchers have also manipulated the vertical distance between the tongue and palate through the use of bite blocks and demonstrated that increments as small as 4–5 mm (mm) may influence lingual–palatal pressure generation in healthy adults [21, 22]. In the opposite direction, palatal augmentation prostheses (PAP) that lower the palate in increments as small as 2.8 mm have demonstrated significant changes in lingual function including total duration of lingual movement and duration of lingual–palatal contact [23, 24]. Palatal augmentation prostheses have also demonstrated potential for improved swallowing function (e.g., reduced phase durations, reduced aspiration, and/or improved bolus clearance) for persons post-glossectomy or stroke survivors [25, 26]. The central theme across such findings supports the theory that oropalatal dimensions influence lingual function, specifically the contact between the tongue and hard palate during swallowing.
Lingual structure may also influence maximum isometric pressure generation, particularly lingual volume. Increases in tongue strength in healthy adults may co-occur with small increases in lingual volume following lingual strengthening interventions, thus suggesting lingual mass relates to force generation [27]. Lingual volume may also be gender dependent with males demonstrating greater tongue dimensions than females [28]. Mean lingual volumes across 70 healthy young adults obtained via magnetic resonance imaging techniques demonstrated significant gender differences with an average of 89.9 cm3 (SD = 11.5) for males and 68.9 cm3 (SD = 7.0) for females [28]. Due to normal anatomical variation in tongue size and the hydrostatic properties of the tongue, exact geographical and functional lingual regions remain largely undefined, complicating the interpretation of lingual–palatal pressures.
To better understand whether and to what degree anatomical dimensions may explain individual variation in maximum isometric tongue pressure generation, the present study obtained measures of oropalatal dimensions and MIP measures across a wide age range of healthy adults. Investigators hypothesized that palatal dimensions and lingual volume would explain significant and additional variance in MIP when controlling for the factors of age and gender. Such knowledge may advance the clinical identification of pathological lingual weakness by contextualizing tongue strength within normal anatomical variation.
Method
The protocol for this study was approved by Florida State University’s Institutional Review Board and the University of Northern Iowa Institutional Review Board.
Participants
Out of a recruited and consented 152 participants, 147 participants (age 18–83; M age = 43.2 years, SD = 21.4 years; 74 males, 73 females) met the following inclusionary criteria: (1) normal oral structure and function assessed by an oral mechanism exam, (2) self-reported oral diet rated by a trained examiner as a level 7 on the functional oral intake scale (FOIS) [29], and (3) adequate natural or permanent, artificial dentition for the completion of an alginate dental impression. Participants with more than two missing maxillary teeth, or full/removable upper dentures were excluded as such lack of dentition would hinder the acquisition and measurement of a dental impression. Exclusionary criteria also included history of dysphagia, neurologic disease, stroke, heart attack, or oral surgeries beyond routine dental surgery, speech disorders beyond a remediated childhood articulation disorder, or a history of respiratory disorders beyond childhood asthma or medication-controlled asthma.
Instrumentation
Lingual–palatal pressures were obtained using the IOPI (Iowa Oral Performance Instrument; Model 2.1 or 2.2), a handheld, digital device with excellent reliability [15, 16] in measuring the peak pressure applied with the tongue to a connected air-filled silicone tongue bulb (approximately 3.5 × 4.5 cm in diameter) against the palate. Twenty participants repeated the protocol with the counterbalanced IOPI model (either 2.1 or 2.2). A Wilcoxon matched-pairs signed-rank test indicated models were equivalent in measurement of lingual–palatal pressures (p = .228). All IOPI tasks were completed with participants seated in a straight-backed chair with feet flat on the floor during IOPI tasks.
Experimental Tasks
Lingual–Palatal Pressures
Lingual–palatal pressures were obtained at both the anterior and posterior oral tongue. Anterior bulb placement was anatomically defined as the straight edge of the bulb directly behind the central incisors on the midline of the superior surface of the anterior tongue [11], and posterior tongue bulb placement was defined as midline on the superior surface of the tongue with the straight edge of the bulb in line with the anterior edge of the participant’s first lower molars. The anterior–posterior distance between the two tongue bulb placements was measured in millimeters (mm) and was significantly larger in men than women (for men M = 21.5, SD = 3.7; for women M = 19.0, SD = 3.0; (t(145) = 4.394, p < .001; Levene’s test p > .05)).
Lingual–palatal pressures were measured at anterior and posterior bulb placements during both maximal isometric and swallowing tasks in counterbalanced order. Results of the swallowing trials are not reported within the scope of this manuscript since maximum pressure generation is the primary clinical metric for determining lingual weakness. MIP was defined as the greatest pressure (kPa) obtained across three encouraged trials in which the participant compressed the tongue bulb with maximum effort with either the anteromedian (MIPA) or posteromedian (MIPP) tongue against the palate. Participants were provided visual biofeedback of the digital pressure reading on the IOPI screen during MIP trials.
Palatal Dimensions
Dental impressions of the upper alveolar ridge and palate were obtained using Cavex CA37 Fast Set Alginate. Impressions were trimmed posteriorly at the posterior border of the second molars, and anteriorly and laterally along the lingual surfaces of the upper teeth. The following palatal measurements were obtained from the impression using digital calipers (mm): (1) incisive palatal height (IH) was defined as the height of the mold at the posterior edge of the lateral incisors, (2) molar palatal height (MH) was defined as the height of the mold at the anterior edge of the first molars, (3) incisive palatal width (IW) was defined as the distance between the midpoints of the lingual surfaces of the left and right lateral incisors, (4) molar palatal width (MW) was defined as the distance between the midpoints of the lingual surfaces of the left and right first molars, and (5) palatal length (PL) was defined as the distance between the junction of the central incisors to the midpoint of the posterior border of the second molars. Measures are illustrated in Fig. 1.
Estimated Tongue Volume (ETV)
Tongue volume was estimated as per equation [28] using the factors of gender and participant weight as measured on a digital scale during study intake procedures (ETV (cm3) = 43 + 12.8 (gender) + .435 (kg); with male = 1 and female = 0).
Analysis
All analyses were conducted in SPSS 22.0 with the level of significance set at p < .05, unless otherwise noted. Paired t-tests were conducted to compare MIPA to MIPP across the total sample. Independent t-tests were conducted to explore differences in palatal dimensions by gender (significance set at p < .01 with Bonferroni correction).
To investigate relations among MIP and the seven factors of: age, estimated tongue volume, and palatal dimensions (i.e., IH, MH, IW, MW, and PL), Pearson correlation coefficients (r) were calculated. Two multiple linear regressions were conducted to respectively predict MIPA and MIPP based upon the independent variables that demonstrated significant correlations with MIP generation.
Reliability
Each palatal measurement was repeated three times per individual dental impression. Intra-rater reliability for each of the five palatal measurements was high across the entire sample with Cronbach’s alpha coefficients greater than .991. Palatal measurements were repeated by a second trained investigator for 25 dental impressions and Wilcoxon matched-pairs signed-rank tests indicated no significant difference between raters for all palatal measures (p > .05). Dental impressions were repeated for 24 participants and Wilcoxon matched-pairs signed-rank tests indicated that replicated dental impressions did not significantly differ from original impressions across all palatal measurements (p > .05).
Results
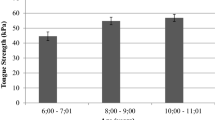
Anteromedian and Posteromedian MIP
Descriptive statistics for anterior and posterior MIP are reported in Table 1 for the total sample and by gender groups. Overall, anteromedian MIP (M = 62.1 kPa, SD = 12.4) was significantly greater than posteromedian MIP (M = 56.7 kPa, SD = 12.6; t(146) = 6.178, p < .001) across the total sample, as well as for males (t(73) = 6.998, p < .001) and females (t(72) = 2.066, p = .042).
Oropalatal Dimensions
Descriptive statistics for oropalatal dimensions are reported for the total sample and by gender in Table 2. Men exhibited significantly larger oropalatal dimensions than women for all measurements (p < .003). Correlations among MIP, individual oropalatal dimensions, ETV, and age are reported in Table 3.
MIPA Regression
All oropalatal measures, excluding incisive palatal height (IH), demonstrated a significant correlation with MIPA and were included in the model along with the factors of age and gender. Exploration of regression assumptions confirmed independence of observations (i.e., Durbin-Watson of 1.918) and low multicollinearity with all tolerance values above .286, averaged variance inflation factor (VIF) of 1.95, and all VIF values less than 3.501. No significant outliers were of concern, with eight (5.4%) of 147 cases falling outside of two standard deviations from the mean, as expected, since approximately 5% of cases have standardized residuals outside of this limit, and all eight cases were within 2.56 standard deviations. Residuals also demonstrated normal distribution per visual analysis of a histogram and demonstrated lack of homoscedasticity when plotted against predicted values.
A significant model emerged for MIPA (F(7, 139) = 16.742, p < .001). Beta and p values are reported in Table 4. Significant predictors included age (p < .001), ETV (p = .022), and palatal width at the lateral incisors (p = .007) and at the first molars (p < .001); gender, molar palatal height, and palatal length were not significant predictors. The overall model explained 45.7% of the variance in anterior tongue strength (R 2 = .457; adjusted R 2 = .430), which is a R 2 change of .33 compared to the correlation between age and MIPA (R 2 = .1).
MIPP Regression
Only measures of incisive height, incisive width, molar width, palatal length, and ETV along with gender demonstrated a significant correlation with MIPP and were included in the model. Exploration of regression assumptions confirmed independence of observations (i.e., Durbin–Watson of 1.836), and low multicollinearity with all tolerance values above .297, averaged VIF of 1.943, and with all VIF values less than 3.359. No significant outliers were of concern with six (4.1%) of 147 cases failing outside of two standard deviations of the mean, and all cases were within 2.56 standard deviations. Residuals also demonstrated normal distribution per visual analysis of histogram with superimposed normal curve and demonstrated lack of homoscedasticity when plotted against predicted values.
A significant model emerged for MIPp (F(6, 140) = 9.210, p < .001). Beta and p values are reported in Table 5. Significant predictors included gender (p = .020), ETV (p = .013), and palatal width at the incisors (p < .001) and at the first molars (p = .002); however, age, molar palatal height, and palatal length were not significant predictors. The overall model explained 28.3% of the variance in posterior tongue strength (R 2 = .283; adjusted R 2 = .252).
Discussion
The purpose of this study was to improve our understanding of how anatomical variation in oral and palatal structure may contribute to normal variability in tongue strength (i.e., maximum isometric pressure generation) in addition to the established influential factors of age and gender. We hypothesized that palatal dimensions and lingual volume would explain significant and additional variance in MIP when controlling for the factors of age and gender. Based on the results of the current study, individual differences in oropalatal structure do in fact contribute to the variation in maximum isometric lingual–palatal pressure (MIP) generation in healthy adults. In combination, age, gender, and oropalatal dimensions may account for approximately 43% of the variance in anterior tongue strength and 25% of variance in posterior tongue strength in healthy adult populations. Of interest to note is that different combinations of the above factors that best predicted tongue strength differed between the anterior and posterior tongue regions.
Age is a well-established, influential factor on maximum isometric tongue pressure generation [3, 7,8,9,10,11,12,13,14,15,16,17]. Surprisingly, in the present study oropalatal dimensions (R 2 change = .33) explained greater than three times the variance in anterior tongue strength as age alone; however, age was not a significant predictor of posterior tongue strength when controlling for gender and oropalatal differences. Such differential effects of aging on pressure generation of the anterior tongue compared to the posterior region may be attributed to functional and anatomical differences between lingual regions. Specifically, the anterior tongue houses higher concentrations of connective tissue as well as a predominance of type IIA fast-twitch muscle fibers compared to the posterior tongue [30, 31]. Differences in myoarchitecture may render the anterior tongue particularly vulnerable to age-related changes in contractile function including selective loss or transition of fast-twitch fibers and a reduction in motor unit density [32, 33].
Gender did not manifest as a significant predictor of anterior tongue strength; however, a small, yet significant gender effect potentially could be concealed within the variables of oropalatal dimensions (i.e., males exhibited larger oropalatal dimensions than females and estimated tongue volume was differentially calculated by gender as per equation). Nevertheless, gender remained a significant factor for predicting posterior tongue strength beyond oropalatal dimensions. A significant gender effect unique to posterior lingual–palatal pressure generation may reflect differences in body composition or lingual muscular tissue concentrations with respect to the ratio of muscle, adipose, and connective tissue [30, 34]. For example, males generally exhibit greater concentrations of muscular tissue than females, and such concentrations are higher in the posterior compared to the anterior lingual regions [30]. An alternative explanation may also relate to sampling effects in regard to individual variation in bone mineral density. Females generally have lower bone mineral density compared to males and preliminary evidence suggests a positive correlation between anterior tongue strength and bone mineral density in healthy, young athletes [34].
Concerning palatal dimensions, palatal width was a significant predictor of both anterior and posterior MIP generation, and significant, positive correlations between measures of palatal width and tongue strength existed. Molar palatal width was a significant and stronger predictor of anterior MIP than incisive width, and incisive palatal width was a significant and stronger predictor of posterior MIP than molar width. Perhaps greater palatal width at the divergent lingual region provided a superior platform to generate greater counter or stabilizing tongue pressure toward the opposing lingual region. Neither palatal height nor palatal length was a significant predictor of maximum isometric tongue pressure generation. This finding seems surprising in light of previous investigations demonstrating that the vertical distance between the tongue and the hard palate through the use of bite blocks or palatal augmentation influences lingual–palatal contact [21,22,23]. The lack of significant contribution of palatal height in the present study may be attributed to the small variation in palatal height across healthy adults (less than 2.8 mm standard deviation). Substantial adjustments in palatal height or vertical dimensions that significantly influence MIP may be more similar in magnitude to increments seen with pathological conditions, postsurgical changes, or prosthetics more than those based upon general anatomical variation. Therefore, instrumental pressure sensors used to capture lingual–palatal pressures may need to account more for individual variability in palatal width compared to height and length or consider anatomically customized sensor positions.
The finding of a relation between lingual volume and lingual–palatal pressure generation is somewhat intuitive as increased tongue volume may reflect greater muscle mass and subsequently, increased force generation. This result concurs with previous reports of increased lingual volume (an average of 5.1%) with concurrent gains in tongue strength for healthy older adults following an 8-week lingual strengthening protocol [27]. Thus, it is not surprising that greater estimated lingual volume was related to higher maximum isometric tongue pressures at both the anterior and posterior lingual regions when controlling for both age and gender.
It is interesting that estimated tongue volume demonstrated significant yet small, positive correlations with the majority of palatal measures, especially at the molar region. These relations support the theory that lingual volume may influence the growth and expansion of the midface, particularly in the vertical and transverse directions [35]. Nevertheless, controversy persists to whether the tongue physically shapes its surrounding structures or adapts to existing oral structure and dimensions [35]. Further research into the relation between lingual and palatal morphology may better elucidate their functional relationships for speech production and swallowing.
Overall, predictive equations for lingual–palatal pressure generation provide a foundation for contextualizing maximum isometric pressure generation within healthy individual variation and suggest that that a “one-size fits-all” benchmark-approach to identify lingual weakness may not be the most sensitive metric. Yet, the predictive equation proposed for both anterior and posterior tongue strength still exhibit 57–75% of unexplained variance; suggesting that additional predictors exist (i.e., lingual concentrations of adipose, connective, and muscular tissue; pharyngeal dimensions; body composition; or bone mineral density). Further research regarding additional predictors and the validity of estimating lingual volume across genders and a wide age range may advance our understanding of the considerable variability in healthy tongue strength.
Limitations of the study include the exclusion of healthy adults without adequate dentition for a dental impression, particularly those with upper dentures; and the estimation of tongue volume based on an equation established only in young, healthy adults. However, these findings are the first to substantiate the relation of lingual function in the context of surrounding anatomical parameters, thus, offer a framework for future investigation. Additionally, the benefit of taking direct measurement of palatal width and estimating tongue volume by equation demonstrates greater clinical feasibility than obtaining such measures through imaging of oropalatal structure.
Conclusions
Oropalatal dimensions along with participant age and gender help to explain the wide variation in healthy tongue strength across individuals and may contribute to differentiating pathological weakness from individual difference when included in a predictive equation. Clinical implications of this finding include the ability to better predict healthy tongue strength for comparison to baseline measures at initial clinical evaluations. Equations may also be used to determine optimal treatment targets during lingual strengthening programs for individuals with tongue weakness and dysphagia. However, the use of equations to predict healthy tongue strength is in its infancy and it remains unknown if and to what extent deviation from the predicted pressure relates to clinically significant reductions in swallowing safety or efficiency. Overall, oropalatal dimensions, particularly palatal width and lingual volume, may warrant consideration along with the factors of age and gender when MIP generation is used as a clinical metric to assess tongue strength.
References
Clark HM, Henson PA, Barber WD, Stierwalt JAG, Sherrill M. Relationships among subjective and objective measures of tongue strength and oral phase swallowing impairments. Am J Speech Lang Pathol. 2003;12(1):40–50.
Lazarus CL, Logemann JA, Pauloski BR, Rademaker AW, Larson CR, Mittal BB, et al. Swallowing and tongue function following treatment for oral and oropharyngeal cancer. J Speech Lang Hear Res. 2000;43(4):1011–23.
Stierwalt JAG, Youmans SR. Tongue measures in individuals with normal and impaired swallowing. Am J Speech Lang Pathol. 2007;16(2):148–56.
Rogus-Pulia N, Rusche N, Hind JA, Zielinski J, Gangnon R, Safdar N, et al. Effects of device-facilitated isometric progressive resistance oropharyngeal therapy on swallowing and health-related outcomes in older adults with dysphagia. J Am Geriatr Soc. 2016;64(2):417–24.
Robbins J, Kays SA, Gangnon RE, Hind JA, Hewitt AL, Gentry LR, et al. The effects of lingual exercise in stroke patients with dysphagia. Arch Phys Med Rehab. 2007;88(2):150–8.
Yeates EM, Molfenter SM, Steele CM. Improvements in tongue strength and pressure-generation precision following a tongue-pressure training protocol in older individuals with dysphagia: three case reports. Clin Interv Aging. 2008;3(4):735–47.
Adams V, Mathisen B, Baines S, Lazarus C, Callister R. A systematic review and meta-analysis of measurements of tongue and hand strength and endurance using the Iowa Oral Performance Instrument (IOPI). Dysphagia. 2013;28(3):350–69.
Clark HM, Solomon NP. Age and sex difference in orofacial strength. Dysphagia. 2012;27(1):2–9.
Crow HC, Ship JA. Tongue strength and endurance in different aged individuals. J Gerontol A Biol Sci Med Sci. 1996;51(5):247–50.
Fei T, Polacco RC, Hori SE, Molfenter SM, Peladeau-Pigeon M, Tsang C, et al. Age-related differences in tongue-palate pressures for strength and swallowing tasks. Dysphagia. 2013;28(4):575–81.
Gingrich LL, Stierwalt JAG, Hageman CF, LaPointe LL. Lingual propulsive pressures across consistencies generated by the anteromedian and posteromedian tongue by healthy young adults. J Speech Lang Hear Res. 2012;55(3):960–72.
Nicosia MA, Hind JA, Roecker EB, Garnes M, Doyle J, Dengel GA, et al. Age effects on the temporal evolution of isometric and swallowing pressure. J Gerontol A Biol Sci Med Sci. 2000;55(11):M634–40.
Robbins J, Levine R, Wood J, Roecker EB, Luschei E. Age effects on lingual pressure generation as a risk factor for dysphagia. J Gerontol A Biol Sci Med Sci. 1995;50(5):257–62.
Utanohara Y, Hayashi R, Yoshikawa M, Yoshida M, Tsuga K, Akagawa Y. Standard values of maximum tongue pressure taken using newly developed disposable tongue pressure measurement device. Dysphagia. 2008;23(3):286–90.
Youmans SR, Stierwalt JAG. Measures of tongue function related to normal swallowing. Dysphagia. 2006;21(1):61–5.
Youmans SR, Youmans GL, Stierwalt JAG. Differences in tongue strength across age and gender: is there a diminished strength reserve? Dysphagia. 2009;24(1):57–65.
Vanderwegen J, Guns C, Van Nuffelen G, Elen R, De Bodt M. The influence of age, sex, bulb position, visual feedback and the order of testing on maximum anterior and posterior tongue strength and endurance in healthy Belgian adults. Dysphagia. 2013;28(2):159–66.
Ono T, Hori K, Nokubi T. Pattern of tongue pressure on hard palate during swallowing. Dysphagia. 2004;19:259–64.
Kydd WL, Toda JM. Tongue pressures exerted on the hard palate during swallowing. J Am Dent Assoc. 1962;65:319–30.
McGlone RE, Prroffit WR. Correlation between functional lingual pressure and oral cavity size. Cleft palate J. 1972;9(3):229–35.
Nagao K, Kitaoki N, Kawano F, Komoda J, Ichikawa T. Influence of changes in occlusal vertical dimension on tongue pressure to palate during swallowing. Prosthodont Res Pract. 2002;1(1):16–23.
Solomon NP, Munson B. The effect of jaw position on measures of tongue strength and endurance. J Speech Lang Hear Res. 2004;47(3):584–94.
Okayama H, Tamura F, Kikutani T, Kayanaka H, Katagiri H, Nishiwaki K. Effects of a palatal augmentation prosthesis on lingual swallowing function in postoperative patients with oral cancer: coronal section analysis by ultrasonography. Odontology. 2008;96(1):26–31.
Toyoshita Y, Koshino H, Hirai T, Matsumi T. Effect of wearing a palatal plate on swallowing function. J Prosthet Orthot Res. 2009;53(4):172–5.
Light J, Edelman SB, Alba A. The dental prosthesis used for intraoral muscle therapy in the rehabilitation of the stroke patient: a preliminary research study. NY State Dent J. 2001;67:22–7.
Marunick M, Tselios N. The efficacy of palatal augmentation prostheses for speech and swallowing in patients undergoing glossectomy: a review of the literature. J Prosthet Dent. 2002;91:67–74.
Robbins J, Gangnon RE, Theis SM, Kays SA, Hewitt AL, Hind JA. The effects of lingual exercise on swallowing in older adults. J Am Geriatr Soc. 2005;53:1483–9.
Liégeois F, Albert A, Limme M. Comparison between tongue volume from magnetic resonance images and tongue area from profile cephalograms. J Orthod. 2009;32:381–6.
Crary MA, Mann GD, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005;86(8):1516–20.
Miller JL, Watkin KL, Chen MF. Muscle, adipose, and connective tissue variations in intrinsic musculature of the adult human tongue. J Speech Lang Hear Res. 2002;45:51–65.
Stäl P, Marklund S, Thornell L, De Paul R, Eriksson P. Fibre composition of human intrinsic tongue muscles. Cell Tissues Organs. 2003;173:147–61.
Saboisky JP, Stashuk DW, Hamilton-Wright A, Trinder J, Nandedkar S, Malhotra A. Effects of aging on genioglossus motor units in humans. PLoS ONE. 2014;9:e104572.
Lexell J. Human aging, muscle mass, and fiber type composition. J Gerontol A Biol Sci Med Sci. 1995;50:11–6.
VanRaenhorst-Bell H, Coufal K, Pinkston J, Patterson J. Tongue muscle performance in relation to measure of body composition and bone mineral density. Paper presented at American Speech-Language and Hearing Association Convention; 2016, Philadelphia, Pennsylvania.
Liu Z, Shcherbatyy V, Gu G, Perkins J. Effects of tongue volume reduction on craniofacial growth: a longitudinal study on orofacial skeletons and dental arches. Arch Oral Biol. 2008;53:991–1001.
Acknowledgements
We gratefully acknowledge Justine Rinehart, Margaret Way, Anne Delaney, Erica Murrell, Caiti Boyack, Carolyn Pellegrino, Amy Happ, Apryl Bailey, Nicole Tryon, and Grant Leacox who contributed to the success of this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
No conflicts of interest or financial support to be declared.
Additional information
Research completed at the Florida State University and the University of Northern Iowa.
Rights and permissions
About this article
Cite this article
Pitts, L.L., Stierwalt, J.A.G., Hageman, C.F. et al. The Influence of Oropalatal Dimensions on the Measurement of Tongue Strength. Dysphagia 32, 759–766 (2017). https://doi.org/10.1007/s00455-017-9820-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-017-9820-4