Abstract
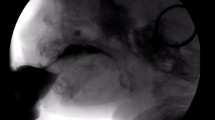
There is little reported evidence regarding the reliability of temporal and physiologic features of infant swallowing from videofluoroscopic swallowing studies (VFSS). The purpose of this retrospective study was to determine a reliable set of temporal and physiologic features from infant swallowing that can be measured from analysis of VFSS. Temporal and physiologic features for testing were determined from review of previously reported features of infant VFSS in the literature. Two novel analysts underwent three training sessions to learn and practice visual recognition of the proposed features. The two analysts then assessed 25 swallows from 10 total subjects’ VFSS. To establish inter- and intra-rater reliability, calculation of Pearson’s r was used for features that met criteria for parametric analysis and Spearman’s rank correlation coefficient was used for the non-continuous features. Percent agreement was used to report on the reliability of the dichotomous features due to insufficient variability for Spearman’s rho analyses. Fifteen of the 16 tested features were found to have acceptable inter- and intra-rater reliability measures, with each analyst achieving a correlation of 0.75 or higher. This project identifies 15 variables that can be reliably measured from infant VFSS. This information can be used to assist with determination of normal versus abnormal swallow features and in developing and testing therapeutic strategies for infants with dysphagia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The improved survival rate of infants and children with complex medical conditions has resulted in a significant increase in the prevalence of pediatric feeding and swallowing disorders. The prevalence of feeding disorders in pediatric populations with developmental disorders ranges from 33 to 80 % [1]. Dysphagia in infants and children may be the result of many underlying conditions including neurological disorders, prematurity and resulting sequelae, craniofacial anomalies, pulmonary disorders/diseases, and those conditions that affect suck/swallow/breath rhythmicity [1, 2]. Evaluation of infants and children suspected of oropharyngeal dysphagia typically includes instrumental assessment. Ultrasound, endoscopy, and videofluoroscopy techniques have all been described in the literature as useful technologies in the diagnosis of pediatric dysphagia [3–18]. Of all the available assessment techniques, the videofluoroscopic examination of swallowing remains the most commonly used tool for analyzing swallowing function in pediatric patients [4, 5, 7, 9, 11–13, 15, 18, 19].
Kramer and Eicher described the videofluoroscopic examination of swallowing as the “best procedure” for evaluating the dynamic process of swallowing in pediatric populations [20]. Many authors have used the videofluoroscopic examination to describe normal and abnormal swallowing function in a variety of pediatric populations ranging in age from infancy to adolescence [4, 5, 7, 9, 11–13, 15, 18]. Each individual report utilizes a different set of temporal and physiologic features to describe normal and abnormal swallowing features. As a result, it is not always possible to compare swallowing features from different populations across reports.
The ability to diagnose normal or abnormal swallowing function in any population, including pediatrics, depends on the establishment of reliable features that can be compared across videofluoroscopic swallowing studies. The purpose of this retrospective study was to determine a set of temporal and physiologic features of infant swallowing function that can be reliably measured with frame-by-frame analysis of videofluoroscopic swallowing studies.
Methods
Subject Selection
Subjects were identified from a retrospective review of the medical records of patients 1 week to 6 months of age who were also referred for a VFSS at Le Bonheur Children’s Hospital in Memphis, Tennessee before December 2010. The age range was restricted based on the established feeding development hierarchy. To avoid the possible developmental influence of spoon feeding, only those infants who had not yet started spoon feeding were included in the current study. The patient’s name, medical record number, and financial number were removed from all reviewable records, and each subject was assigned a number to ensure anonymity. For inclusion, the subjects were required to have a VFSS that identified dysphagia with score on the Penetration-Aspiration Scale of 2 or more on at least one swallow [19]. Based on the limited empirical evidence regarding normal swallowing in infants, airway compromise is not expected on videofluoroscopic imaging [7, 18]. Exclusion criteria included any infant with known neurologic impairment, any infant not at 38 weeks post-conceptual age, any infant with tracheotomy, and any infant with craniofacial anomaly.
Clinical Standards for VFSS
Established clinical standards at Le Bonheur Children’s Hospital dictate that infants undergoing VFSS study were seated, semi-upright, in a Tumbleform chair and were viewed in the lateral projection. Each subject was initially presented with Varibar Thin Liquid Barium (Bracco Diagnostics Inc, Monroe Township, NJ) (target viscosity of 4 centipoise, viscosity range <15 centipoise). The thin liquid barium required reconstitution from powder and clinicians followed manufacturer’s instructions for standard preparation. For the current project, reliability of chosen features was determined from analysis of swallows with the thin liquid barium from Similac (Abbott Laboratories, Abbott Park, IL) disposable volu-feeder bottles with standard Similac, disposable one-hole nipples. The videos were all recorded and reviewed at 30 frames per second.
The subject characteristics are presented in Table 1.
Swallowing Variables for Reliability
Sixteen different swallowing variables were chosen for review based on previous videofluoroscopic analyses of infant swallowing function [7, 18, 21]. The included parameters for reliability analysis are presented in Table 2 along with the instructions given to raters during training.
Reliability Training
Both analysts underwent a series of three, 90 min, training sessions. During the training sessions, the analysts were given the instructions for how to collect all of the intended measures and practiced collecting the target measures with an independent expert analyst. Practice began with collecting the above measures from adult videofluoroscopic swallowing studies on commercially available training packages and then transitioned to practice collecting measures on pediatric VFSS [23, 24]. Videos were reviewed utilizing QuickTime software version 7 (Apple, Cupertino, CA). QuickTime software provides a timer to the hundredths of a second and that was visible for all timing measures. Videos were reviewed with frame-by-frame analysis as many times as necessary for analysts to feel confident in their ratings. In addition to training sessions, analysts reinforced learned concepts by completing independent practice between training sessions. Independent practice was reviewed with the expert analyst at the follow-up training session. They were also able to access the expert analyst for questions and feedback at any time during the training window.
Graduate student volunteers were utilized to fill analysts’ roles as they had no previous experience with pediatric dysphagia, and therefore, did not introduce any clinical bias into their ratings. The expert analyst was an individual with the clinical distinction of board certified specialist in swallowing and swallowing disorders with more than 5 years of clinical experience in the field of pediatric dysphagia diagnosis and management. The expert analyst had previously reviewed other infant VFSS videos and established intra-rater reliability before providing instruction and training to novice analysts.
After completing training, the two novel analysts assessed a total of 25 swallows contributed from 10 different subjects with the established measures on two different occasions at least 2 weeks apart. Individual analysts were blinded to the ratings of the other analysts. The expert analyst independently assessed 10 of the original 25 swallows from four of the subjects to provide a measure of validity for the two volunteer analysts. Correlations of 0.75 or higher were deemed acceptable for labeling of reliable and/or valid for each of the individual features.
Statistical Analyses
Calculation of the Pearson’s r was used to establish inter- and intra-rater reliability for the two volunteer analysts for the 10 variables that met criteria for parametric analysis (number of sucks per swallow, suck time, oral transit time, initiation of velar movement, pharyngeal transit time, duration of cricopharyngeal opening, duration of pharyngeal constriction, time to laryngeal closure, duration of laryngeal closure, and score on the penetration-aspiration scale). Pearson’s r provides a measure of the strength of the correlation between two variables; in this case, the variables are the analyses provided by the two student analysts and one expert analyst for measures providing interval or ratio level data [25].
Spearman’s rank correlation coefficient provided a measure of the strength of the correlation between two variables for ordinal data [25]. Spearman’s rank correlation coefficient was used to establish inter- and intra-rater reliability for the two volunteer analysts for five of the non-continuous variables (location of bolus before the swallow, location of bolus at initiation of laryngeal closure, presence of residue after the swallow, location of residue if present, and jaw position at various times). These five non-continuous variables all represent ordinal data that can be ranked by their scores. Location variables were all ranked in order of appearance along the upper aerodigestive tract with lower location rankings representing material located closer to the oral cavity and higher location rankings representing material located closer to the hypopharynx and larynx. The presence of residue is dichotomous in nature (either yes it was present or no it was not present), but scores can be ranked with 1 (no residue) being more desirable than scores of 2 (residue). Jaw position was ranked as 1 (neutral) being more desirable than scores of 2 (closing) or 3 (opening).
For the dichotomous variables of the presence of epiglottic tilting during the swallow and nasopharyngeal backflow during the swallow, there was insufficient variability among the student analysts and the expert analyst to complete the Spearman’s rho analysis. There was 100 % agreement between the two novel analysts and one expert analyst for those two dichotomous variables.
Results
Descriptive Information
The aim of this study was to provide information on the reliability of a set of proposed swallowing variables for review of infant VFSSs. The results of the individual parameters for the subjects reviewed for the reliability analyses are provided below in a series of Tables 3 and 4.
Reliability
The two novel analysts achieved a correlation of 0.75 or higher for all statistical analyses except for Spearman’s rank correlation coefficients for the feature of jaw position at predetermined times. Each analyst’s scores were also compared to the scores of the expert independent analyst with the Pearson’s r and the Spearman’s rank correlation coefficient, respectively. Tables 5 and 6 provide the individual scores for each of the reliability measures for both intra- and inter-rater reliability. In total, 15 different features were found to be reliable for the analysis of infant VFSS.
Discussion
The VFSS is the most common imaging exam for providing information on all stages of swallowing for infants, and it can be used as part of a complete assessment for oropharyngeal dysphagia [21, 26]. The need for standardization of the VFSS has been established for adult populations [27]. A first step in standardizing criteria for the infant VFSS is establishing a set of oropharyngeal swallowing features than can be reliably analyzed across swallows. To our knowledge, the inter- and intra-rater reliability of a select set of oropharyngeal swallowing features has not been definitively established in the literature.
There are two studies in the literature that previously reported on normal infant swallowing features from review of VFSS and barium esophagram [7, 18]. Each of the studies on normal infant swallowing features utilized a unique set of oropharyngeal swallowing features and provided different liquids for swallowing. Weckmueller et al. provided the subjects with formula or breast milk mixed with barium sulfate powder, while Newman et al. provided subjects with a liquid barium suspension of barium sulfate powder and sterile water [7, 18]. Weckmueller et al. did not report on the reliability of the reported swallowing features used in their study [18]. Newman et al. reported good interobserver reliability with intraclass coefficient correlations (0.79 to 0.99, p < 0.0001) for number of sucks per swallow, suck time, oral transit time, and pharyngeal transit time [7]. Similarly, this study found good interobserver reliability with calculation of the Pearson’s r statistic for inter-rater reliability for the same features. The non-parametric variables recorded in both research projects included collection of material before the swallow, nasopharyngeal reflux, and residue after the swallow. Newman et al. and the current study found interobserver reliability ranging from fair to good for these non-parametric swallowing features [7].
Comparisons, regarding the values of the measures studied here to determine reliability to previously reported normal infant swallowing parameter values, are difficult due to methodological variations. Both the Newman et al. and Weckmueller et al. research studies reported swallowing parameter values for infants without dysphagia. The subjects in this research study were all identified as having dysphagia. The subjects in the Newman et al. and the Weckmueller et al. study had a mean age of 50 days and 2.2 months, respectively, while the mean age of the infants in this study was 3.35 months [7, 18]. Additionally, as the goal of this study was to determine the reliability of the proposed set of parameters for analysis of infant VFSSs, the subject pool was not tightly controlled to allow for generalizability of parameter findings to specific diagnostic groups. However, it may be of interest to compare our limited results to previous results for similar measures; therefore, those comparisons are presented in Table 7.
Considering the division of the set of swallowing features in this research study into temporal measures and those that have the potential to report on the physiological aspects of the infant’s swallow, it will be of interest to investigate the correlation of each set with feeding outcomes. Temporal measures achieved acceptable inter- and intra-rater reliability in this preliminary study. Future analyses with these swallowing features could be used to investigate what, if any, relationship these features have with oropharyngeal dysphagia signs in infant populations such as laryngeal penetration and/or aspiration, respiratory complications, and poor growth/weight gain. Several of the features studied here for reliability can be used to provide comment on the physiological features of the infant swallow including the number of sucks/swallow, suck time, and time to initiate velar competency as a component of oral competency and efficiency; collection of bolus material prior to swallow initiation as a component of lingual–velar competency; the presence of nasopharyngeal backflow as a component of velum–posterior pharyngeal wall competency; and the presence of residue as a component of oral and pharyngeal strength/clearance. These types of correlations would require additional study and are only mentioned here as possibilities for future research.
This study utilized frame-by-frame analysis to obtain quantitative and qualitative data from retrospective review of infant VFSS. The analysts were pretrained to criterion normed features and established both intra- and inter-rater reliability for all features in this set of infant oropharyngeal swallowing parameters, except Jaw Position. This is an encouraging finding as it provides preliminary information on 15 oropharyngeal swallowing features that can be reliably measured during review of infant VFSS. An additional positive feature of this study is the use of novel clinicians in this study, as it points to the potential for generalizability of the reliability of these features, when used by more experienced clinicians.
This study has inherent limitations. It was completed with a small sample size (n = 10) that provided a total of 25 swallows for review. All of the subjects for this study were identified from a limited sample from the same institution, which might introduce institutional bias. If possible, studies should draw subjects from multiple institutions to avoid this bias. Future studies may be able to prevent this bias through prospective data collection from multiple institutions. This study relied on retrospective analysis of previously recorded VFSS. In order to control for common sources of bias from retrospective analysis, we randomly selected subjects from a qualified pool of subjects chosen against established inclusion and exclusion criteria. To control for observation bias, we collected new observations from the VFSS following training on a well-defined criterion referenced set of parameters. A final limitation to the current study comes from reliability training being completed with only one expert trainer. Future studies should examine the reliability of these parameters among experienced clinicians to further establish their validity.
Our results suggest that this set of 15 measures can be used reliably to report features of infant swallowing function. While results are preliminary and have not been validated by duplication in additional independent analyses, they are a first step in establishing possible criteria for standardization of infant VFSS interpretation. Additional work is necessary to determine the normal parameters of each of these features and to determine what, if any, impact these features have on long-term feeding outcomes in infants and children. Additionally, documentation of these features may allow for comparisons to be made between various populations of infants with dysphagia. This study represents the first comprehensive effort to define a set of infant oropharyngeal swallowing parameters and establish their reliability.
References
Lefton-Greif MA. Pediatric dysphagia. Phys Med and Rehabil Clin N Am. 2008;19(4):837–51.
Prasse JE, Kikano GE. An overview of pediatric dysphagia. Clin Pediatr. 2009;48(3):247–51.
Shawker TH, Sonies BC, Hall TE, et al. Ultrasound analysis of tongue, hyoid, and larynx activity during swallowing. Invest Radiol. 1984;19:82–6.
Griggs CA, Jones PM, Lee RE. Videofluoroscopic investigation of feeding disorders of children with multiple handicap. Dev Med Child Neurol. 1989;31(3):303–8.
Kramer SS. Radiologic examination of the swallowing impaired child. Dysphagia. 1989;3:117–25.
Bosma JF, Hepburn LG, Josell SD, et al. Ultrasound demonstration of tongue motions during suckle feeding. Dev Med Child Neurol. 1990;32:223–9.
Newman LA, Cleveland RH, Blickman JG, et al. Videofluoroscopic analysis of the infant swallow. Inves Radiol. 1991;26:870–3.
Bastian RW. Videoendoscopic evaluation of patients with dysphagia: an adjunct to the modified barium swallow. Otolaryngol Head Neck Surg. 1991;104:339–50.
Morton RE, Bonas R, Fourie B, et al. Videofluoroscopy in the assessment of feeding disorders of children with neurological problems. Dev Med Child Neurol. 1993;35(5):388–95.
Fanucci A, Cerro P, Ietto F, et al. Physiology of oral swallowing studied by ultrasonography. Dentomaxillofacial Radiol. 1994;23:221–5.
Mirrett PL, Riski JE, Glascott J, et al. Videofluoroscopic assessment of dysphagia in children with severe spastic cerebral palsy. Dysphagia. 1994;9:174–9.
Rogers B, Arvedson J, Buck G, et al. Characteristics of dysphagia in children with cerebral palsy. Dysphagia. 1994;9:69–73.
Wright RER, Wright FR, Carson CA. Videofluoroscopic assessment in children with severe cerebral palsy presenting with dysphagia. Pediatr Radiol. 1996;26:720–2.
Yang WT, Loveday EJ, Metreweli C, et al. Ultrasound assessment of swallowing in malnourished disabled children. Brit J Radiol. 1997;709:992–4.
Abraham SS, Wolf EL. Swallowing physiology of toddlers with long-term tracheostomies: a preliminary study. Dysphagia. 2000;15:206–12.
Willging JP, Thompson DM. Pediatric FEESST: fiberoptic endoscopic evaluation of swallowing with sensory testing. Current Gastroenterol Reports. 2005;7:240–3.
Miller JL, Kang SM. Preliminary ultrasound observation of lingual movement patterns during nutritive versus non-nutritive sucking in a premature infant. Dysphagia. 2007;22:150–60.
Weckmueller J, Easterling C, Arvedson J. Preliminary temporal measurement analysis of normal oropharyngeal swallowing in infants and young children. Dysphagia. 2011;26:135–43.
Fisher SE, Painter M, Milmoe G. Swallowing disorders in infancy. Pediatr Clin N Am. 1981;28(4):845–53.
Kramer SS, Eicher PM. The evaluation of pediatric feeding abnormalities. Dyspahgia. 1993;8:215–24.
Mercado-Deane MG, Burton EM, Harlow SA, et al. Swallowing dysfunction in infants less than 1 year of age. Pediatr Radiol. 2001;31(6):423–8.
Rosenbek JC, Robbins JA, Roecker EB, et al. A penetration-aspiration scale. Dysphagia. 1996;11(2):93–8.
Veteran’s Administration (2007) Understanding dysphagia [DVD].
Singular Publishing Group, Inc. Radiographic interpretation of swallowing disorders [CD-ROM]. San Diego, CA: Martin-Harris B, McConnel FMS, McMahon SJ; 1999.
Hinkle DE, Wiersma W, Jurs SG. Correlation: a measure of relationship. Applied statistics for the behavioral sciences. 5th ed. Boston/New York: Houghton Mifflin Company; 2003. p. 95–120.
Arvedson JC. Assessment of pediatric dysphagia and feeding disorders: clinical and instrumental approaches. Dev Disabil Res Rev. 2008;14:118–27.
Martin-Harris B, Brodsky MB, Michel Y, et al. MBS measurement tool for swallow impairment- MBSImp: establishing a standard. Dysphagia. 2008;23:392–405.
Acknowledgments
The authors wish to thank Drs. Corinna Ethington and Michael Cannito for their valuable assistance with this study. Recognition must also be given to the special project students who generously donated their time to this study at various stages. Thank you to Daniel Addess, Annie Cornell, Farra Durham, Molly Ellis, Katy Bills, Candace Thompson, and Alisa Gokhman.
Conflict of interest
The authors do not have any financial or non-financial conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gosa, M.M., Suiter, D.M. & Kahane, J.C. Reliability for Identification of a Select Set of Temporal and Physiologic Features of Infant Swallows. Dysphagia 30, 365–372 (2015). https://doi.org/10.1007/s00455-015-9610-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-015-9610-9