Abstract
Despite the high regenerative capacity of skeletal muscle, volumetric muscle loss (VML) is an irrecoverable injury. One therapeutic approach is the implantation of engineered biologic scaffolds enriched with stem cells. The objective of this study is to investigate the synergistic effect of high-intensity interval training (HIIT) and stem cell transplantation with an amniotic membrane scaffold on innervation, vascularization and muscle function after VML injury. A VML injury was surgically created in the tibialis anterior (TA) muscle in rats. The animals were randomly assigned to three groups: untreated negative control group (untreated), decellularized human amniotic membrane bio-scaffold group (dHAM) and dHAM seeded with adipose-derived stem cells, which differentiate into skeletal muscle cells (dHAM-ADSCs). Then, each group was divided into sedentary and HIIT subgroups. The exercise training protocol consisted of treadmill running for 8 weeks. The animals underwent in vivo functional muscle tests to evaluate maximal isometric contractile force. Regenerated TA muscles were harvested for molecular analyses and explanted tissues were analyzed with histological methods. The main finding was that HIIT promoted muscle regeneration, innervation and vascularization in regenerated areas in HIIT treatment subgroups, especially in the dHAM-ADSC subgroup. In parallel with innervation, maximal isometric force also increased in vivo. HIIT upregulated neurotrophic factor gene expression in skeletal muscle. The amniotic membrane bio-scaffold seeded with differentiated ADSC, in conjunction with exercise training, improved vascular perfusion and innervation and enhanced the functional and morphological healing process after VML injury. The implications of these findings are of potential importance for future efforts to develop engineered biological scaffolds and for the use of interval training programs in rehabilitation after VML injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Volumetric muscle loss (VML) is defined as the surgical or traumatic loss of a major part of a skeletal muscle, resulting in an irrecoverable injury. The replacement of myofibers with fibrotic tissue in the injured area impairs muscle structure and function (Liu et al. 2018; Wu et al. 2012). After injury, long-term dysfunction causes permanent disability and cosmetic handicaps. Existing therapies such as surgical repair with muscle flap transposition or autologous tissue transfer are limited to scar tissue debridement and provide some cosmetic improvement but these clinical methods are inefficient in improving function or morphological repair (Kesireddy 2016; Quarta et al. 2017).
Tissue engineering technologies and stem cell therapy have emerged as promising strategies for regenerative skeletal muscle repair (Pantelic and Larkin 2018). Stem cells are defined by their ability for division, self-renewal and differentiation into multiple cell types (Chagastelles and Nardi 2011).
Extracellular matrix (ECM) molecules within the basement membrane have a marked influence on the elasticity, stiffness, adhesion and growth of overlying cells (Niknejad et al. 2008). The ECM of skeletal muscle is organized into the endomysium, perimysium and epimysium layers, which contain collagen I and III. The basal and reticular lamina are composed mainly of collagen fibrils (types I, III, IV and VI), laminin and fibronectin in a proteoglycan-rich gel (Dunn et al. 2018). The amniotic membrane (AM) can act as a scaffold with a template of the ECM. Epithelial cells in the AM secrete collagen types III and IV and glycoproteins. Collagen types V and VI were found between interstitial collagen and the epithelial basement membrane and interstitial collagens include types I and III. The spongy layer on the stromal portion of the AM contains an abundance of hydrated proteoglycans and glycoproteins and also contains type III collagen (Niknejad et al. 2008). The human amniotic membrane (HAM) is a biodegradable scaffold richly supplied with collagen, elastin, fibronectin and laminin, which create a strong, elastic structure (Fouad et al. 2016). Biologic scaffolds collected from decellularized HAM have been shown to promote constructive remodeling in injured tissues such as burn wounds, damaged skin and soft tissues, among others (Gholipourmalekabadi et al. 2016). Bio-scaffolds based on HAM have also been reported to decrease inflammation, prevent scarring and favor wound healing. In addition, HAM is a suitable bio-scaffold for modulating angiogenesis and shows good adhesion to wounds in the wet microenvironment of the injured area (Fouad et al. 2016; Gholipourmalekabadi et al. 2016; Song et al. 2017). These characteristics make HAM an appropriate resource for muscle tissue-engineered scaffolds.
In the present study, we used adipose-derived stem cells (ADSCs) as an alternative cell source co-cultured with a decellularized human amniotic membrane (dHAM) scaffold for tissue-engineered skeletal muscle in an experimental model of VML injury repair. Previous studies have reported that ADSC have the potential to differentiate into myogenic and other lineages (Zuk et al. 2002). In addition, ADSC represent an abundant, easily expandable, pluripotent adult stem cell source that can be readily isolated from adipose tissue. This source of stem cells is easier to use than other mesenchymal stem cells in terms of ease of access (Kesireddy 2016).
VML injuries often involve not only the loss of myofibers but also concomitant damage to intramuscular nerve connections and blood vessel structures. Revascularization plays an important role in tissue repair or regeneration by providing circulating cells, nutrients and oxygen. Innervation also plays an important role in the development of the structural and functional capacities of skeletal muscle (VanDusen et al. 2014). However, skeletal muscle denervation can contribute to continued degeneration, leading to the failure of neuromuscular junctions (NMJs) and consequent atrophy and tissue necrosis (Hua et al. 2015). In addition, VML results in intense functional deficits. For example, it has been reported that when 20% of the tibialis anterior (TA) mass is defective, this muscle exhibits a functional deficit of 29% at 2 months post-injury and 31% at 4 months after injury (Corona et al. 2012; Wu et al. 2012). Therefore, patients with VML need an effective treatment plan to repair muscle structures and improve functional recovery.
Recent studies have used voluntary cage wheel running to investigate muscle rehabilitation programs and the recovery of functional muscle contractility after VML injury (Aurora et al. 2014; Nakayama et al. 2018; Quarta et al. 2017). However, some research has shown that involuntary exercise training with incremental intensity and duration was effective in improving histological and physiological aspects of muscle regeneration (Bazgir et al. 2017). High-intensity interval training (HIIT) is one beneficial treatment for muscle regeneration, because it influences functional outcomes (such as strength) and morphological properties of skeletal muscle by increasing the number of satellite cells and the muscle protein synthesis ratio and by modifying contractile properties (Bazgir et al. 2017; Nederveen et al. 2015; Pugh et al. 2015). In particular, HIIT triggers angiogenesis and vascularization and appears to be effective in reducing fibrotic tissues by increasing satellite cell activation and protein turnover (Cocks and Wagenmakers 2016; Hoier et al. 2013). Despite the different roles of endurance, resistance and voluntary exercise training in the innervation of damaged muscles (Messi et al. 2015; Nakayama et al. 2018; Quarta et al. 2017), little is known about the effect of HIIT on NMJ maturation and motor unit innervation. One relevant factor that affects innervation and nerve branch maturation is the release of neurotrophic factors from skeletal muscles during exercise training and their ability to stimulate neurogenesis in damaged muscle tissue (Domínguez-Sanchéz et al. 2018). In addition, HIIT affects neurotrophic factors and glial cell function (Domínguez-Sanchéz et al. 2018; Zoladz et al. 2014); however, the available evidence is scarce. Ultimately, muscle strength and force production must be supported by exercise training. As shown by previous studies, exercise training improves vascularization, innervation and force production in the process of muscle renewal in vivo.
The purpose of the present study is to compare the simultaneous and separate effects of HIIT and biologic scaffolds enriched with stem cells on the structural and functional regeneration of skeletal muscle after VML injury. We used a biologic scaffold and exercise training in a rat model of VML injury to increase revascularization and muscle reinnervation and determined whether HIIT with the use of dHAM+ADSC had positive effects on innervation, vascularization, neurotrophic factors and isometric contraction of the TA muscle renewal tissues after ablation. In addition, we investigated the expression of genes for three neurotrophic factors: brain-derived neurotrophic factor (BDNF), nerve growth factor (NGF) and neurotrophin-3 (NT3).
Material and methods
Animals model
Thirty-six adult male Wistar rats (225–250 g, 6–7 weeks old) from the animal laboratory of Shahid Chamran University of Ahvaz were maintained under controlled room temperature conditions (22 ± 1 °C at 60 ± 5% relative humidity), exposed to a 12-h light/dark cycle and fed with commercial standard pellets with free access to tap water. All procedures in this study were performed in accordance with the National Research Council (US) Committee Guide for the Care and Use of Laboratory Animals, 8th edition and the guidelines provided by the Experimental Animal Care and Ethics Committee of Shahid Chamran University of Ahvaz (Ethical approval number: EE/97.24.370024/scu.ac.ir). All applicable international, national and/or institutional guidelines for the care and use of animals were followed.
Experimental design
During surgery and the recovery period, 6 animals were excluded from further study. Three of the animals died and 3 others had movement defects in their operated leg. A VML injury was surgically created in the TA muscle of the left hindlimb in 30 animals. The rats were randomly assigned to three groups of 10 rats each: untreated negative control group (untreated; surgical creation of the VML injury and debridement were performed but no bio-scaffolds were transplanted), dHAM, or decellularized amniotic membrane scaffold co-cultured with adipose-derived stem cells that differentiated into skeletal muscle (dHAM-ADSC). Two weeks post-injury, each of the three groups was further divided into two subgroups: sedentary and HIIT. Then, the exercise training protocol began on a treadmill for 8 weeks. The animals underwent in vivo functional muscle tests to evaluate maximal isometric contractile force. At the end of the exercise period, the rats were killed in a rodent euthanasia chamber using carbon dioxide (CO2) and the TA muscles were removed for molecular analyses.
In vitro studies
Bio-scaffold preparation
Human amniotic membranes were decellularized according to the protocol described by Shi et al. (2015). The membranes were obtained from mothers who completed an informed consent form after their cesarean delivery. The use of the human amniotic membranes was approved by the Ethics Committee of Shahid Chamran University of Ahvaz. At the time of tissue collection, serological testing was used to screen the donors for human syphilis, HIV and hepatitis virus types B and C. Amniotic membranes were mechanically separated from the placenta and washed three times in phosphate-buffered saline (PBS). The fresh HAM was sterilized in 75% alcohol/water for 10 s and then washed with shaking in PBS containing penicillin–streptomycin (200 U/mL) for 1 day; the solution was changed every 12 h. For the process of decellularization, HAM was treated sequentially with 1% Triton X-100 for 14 h, 2000 U/L lipase PBS for 10 h at 37 °C, and 2000 U/L DNAase PBS for 3 h at 37 °C. Each step was followed by PBS rinsing. Finally, the dHAM was cut into slices about 2.0 × 2.0 cm and stored at 4 °C.
Characterization of dHAM
Amniotic membrane decellularization was confirmed by hematoxylin and eosin (H&E) staining. Samples were then fixed in 10% neutral-buffered formalin, dehydrated with a graded series of ethanol, embedded in paraffin wax and sectioned at 5 μm on a microtome. Samples were checked with a Nikon E-200 microscope (Nikon, Tokyo, Japan) after staining with H&E.
Isolation, preparation and culture of adipose tissue-derived stem cells
ADSCs were collected according to the protocol reported by Zuk et al. (2002). Briefly, adipose tissue was isolated from the inguinal or subcutaneous regions of donor rats and then minced and washed extensively in sterile PBS and low-glucose Dulbecco’s modified Eagle’s medium (LG-DMEM; (Gibco, Invitrogen Corporation, Carlsbad, CA, USA) supplemented with 1% antibiotic/antimycotic solution. The adipose tissue was then subjected to collagenase II enzymatic digestion with 0.2% collagenase type I in DMEM at 37 °C for 1 h with constant shaking. After digestion, the tissue was neutralized with medium consisting of DMEM containing 10% FBS (fetal bovine serum; Gibco BRL, Thermo Fisher Scientific, Waltham, MA, USA) and 1% antibiotic/antimycotic solution and centrifuged for 10 min at low speed to separate the fatty top layer from the cell pellet that contained ADSC. The cell pellet was resuspended and filtered through a 100-µm cell strainer. The filtrate was plated onto conventional tissue culture plates. The cells were seeded into cell culture flasks and incubated at 37 °C in a humidified atmosphere with 5% CO2 in air. Cell passages were carried out when the cells reached 80–90% confluency.
Characterization of ADSC by flow cytometry
Surface markers on adipose tissue were identified with a FACSCalibur Flow Cytometer (BD biosciences, San Jose, CA, USA). Cells were trypsinized with 0.05% trypsin/ethylenediaminetetracetic acid (EDTA) (Gibco) and resuspended in PBS. The monoclonal antibodies used were CD45-FITC, CD34 PE, CD44 PE and CD90 PE. The cells were immunolabeled with antibodies for 1 h at 4 °C and immunoglobulin G staining was used as a negative control. After washing, the cells were stained with a fluorescein isothiocyanate (FITC)- or phycoerythrin (PE)-labeled goat anti-mouse secondary antibody for 30 min and analyzed with BD FACSComp™ software.
ADSC co-culture on dHAM and multipotent differentiation
Bio-scaffolds were created in vitro by co-culture of ADSC on dHAM. The ADSC were seeded on the dHAM at about 5 × 104 cells per cm2 in single-well plates. Two types of scaffold were prepared: one with and one without ADSC. In the dHAM group (without stem cells), the culture medium contained DMEM with 10% FBS and 1% penicillin/streptomycin and culture lasted for 5 days. In the dHAM-ADSC group, myogenic differentiation was induced by a cell culture medium with 10 µM 5-azacytidine (Sigma-Aldrich, St. Louis, MO, USA) plus LG-DMEM, 10% FBS and 5% horse serum (Gibco) for 14 days.
Cell/dHAM morphology
Cell sheet samples from the two groups were examined by scanning electron microscopy (SEM). The samples were washed in PBS and specimens were fixed in 2.5% glutaraldehyde (Alfa Aesar, Haverhill, MA, USA) for 12 h. After washing with PBS, the cells were dehydrated in a graded series of ethanol. After critical-point drying, the specimens were sputter-coated with gold and examined in a digital scanning electron microscope (Zeiss Leo 1450 VP; Tokyo, Japan).
Immunocytochemical staining
The cells were fixed with 4% paraformaldehyde (Sigma-Aldrich), washed in PBS, and incubated in 0.3% H2O2 in the dark for 20 min to suppress endogenous peroxidase activity. They were then incubated in blocking solution containing PBS + 5% normal goat serum for 20 min at room temperature. They were stained with primary antibodies for myogenin, PDM 158, Myod1, DBS and PDM120-s-1 (Diagnostic Biosystems, Pleasanton, CA, USA) for 1 h. A super-enhancer (DAKO, BioGenex, Fremont, CA, USA) was then added to the cells for 15 min and they were incubated with labelled polymer HRP (EnVision, Dako, Glostrup, Denmark) for 30 min. Then, freshly prepared 3,3′-diaminobenzidine (DAB) (Dako) chromogen and H2O2 solution were added to the samples for 3 min and the cells were washed in distilled water and then counterstained with hematoxylin.
In vivo studies
VML injury model
Ibuprofen (Children’s Motrin®, Soha Pharmaceutical, Tehran, Iran) 20 mg/kg was administered as an analgesic by oral gavage 1 h before surgery. All rats (n = 36) were anesthetized with intraperitoneal ketamine (5 mg/kg) and xylazine (2 mg/kg) and core temperature was maintained at 36.5–37.5 °C with a temperature-controlled platform. The surgical VML injury in the TA muscle was created as previously reported (Wu et al. 2012). Briefly, a longitudinal incision was made along the lateral aspect of the shin and a surgical defect was created in the middle third of the TA muscle. For expression analysis, the muscle was separated from the extensor digitorum longus muscles and tibia with blunt dissection. In the TA muscle, two horizontal incisions (7 mm wide) and two longitudinal incisions (10 mm long) were made to a depth of 3 mm with a sterile scalpel (size 11). The amount of tissue excised was approximately 20% of the TA muscle mass.
Bio-scaffold transplantation
In the dHAM and dHAM-ADSC groups, the bio-scaffolds were transplanted immediately after the creation of the muscle defect. Each bio-scaffold was carefully cut and trimmed to fit the defect and a layer of scaffold was inserted in the wound area with the same technique. The top layer of the scaffold contained stem cells co-cultured with dHAM. In all rats, the fascia and skin were then closed with prolene suture (0–6) and the rats were allowed to recover from anesthesia. In the negative control (untreated) group, surgical creation of the VML injury and debridement were performed but no bio-scaffolds were transplanted.
Recovery period
After VML surgery, a 2-week recovery period was allowed. Ibuprofen 20 mg/kg was administered as an analgesic by oral gavage every 6 h during the first 24 h post-surgery and every 12 h thereafter. All rats received systemic antibiotic treatment with enrofloxacin (Shahid Ghazi Pharmaceutical, Tabriz, Iran) 10–20 mg/kg every 24 h via drinking water for 10 days.
Exercise training program
During the 2-week recovery period, animals in the experimental groups were familiarized with the motorized treadmill (Danesh Salar Iranian model, Tehran, Iran) 3 days per week at a slow pace (5 m/min) for 10 min/day. At the end of the recovery period, all three groups of animals were randomly divided into sedentary untreated and HIIT subgroups. Thereafter, exercise training was used 5 days per week for 8 weeks and each session consisted of three sets of HIIT that included:
Warm up: running for 5 min at 30–40% of VO2max.
Main training: 32-min interval running (8 intervals). Each interval consisted of 3 min of running at 85–90% of VO2max and 2 min at 30–35% of VO2max for active recovery.
Cool down: 5 min at 30–40% of VO2max.
Estimates of the intensity of training for each week were adjusted based on previous studies that demonstrated a strong relationship between running speed and VO2max in rats (Kraljevic et al. 2013). Therefore, training intensity was increased by 0.02 m/s every week.
Functional analysis
The isometric contraction force of the TA muscle was measured in vivo in anesthetized rats (n = 30) as previously described and body temperature was maintained at 36–37 °C. The hindlimb was stabilized and secured on the platform with pins and bars at right angles to the ankle and knee joint. For in vivo measurements, the TA was isolated by tenotomizing the agonist dorsiflexor muscles. Maximal isometric contraction force was determined by stimulating the peroneal nerve and using the average value from three contractions. Muscle force signals were recorded at approximately 150 Hz with a pulse width (duration) 0.1 ms over a range of voltages (2–8 V) with a PowerLab converter (ADInstruments, Nagoya, Japan). P values more than 0.05 were considered nonsignificant.
Immunohistochemical staining of regenerating muscle
Immunohistochemical studies were done in samples from tissues cut to a thickness of 4 µm on charged adhesion slides (Citoglass, Nanjing, China) (n = 5 rats per group) and incubated at 37 °C to obtain tissue adherence to the slides. Tissues that were embedded in paraffin were deparaffinized and antigens were immediately retrieved with antigen retrieval buffer (100 × citrate buffer, pH 6.0), then endogenous peroxidase was blocked by adding one part 30% H2O2 for 10 min. Primary antibodies (myosin heavy chain-monoclonal mouse antibody to myosin, skeletal (fast)) (DBS, Mob 207 concentrated), CD31 antibody (CD31: ab119339, secondary: ab6785), mouse anti-neurofilament monoclonal antibody (PDM012-S) and FLEX anti-synaptophysin (Code IR660) were added to the slides, which were then incubated with the antibodies and treated with the Mouse/Rabbit PolyDetector HRP/DAB Detection System kit (Diagnostic Biosystems) for 30 min. DAB was added to the slides, which were then incubated for 5 min and examined for nuclear and/or cytoplasmic staining, which indicated positivity for the protein of interest.
For immunofluorescence staining, the slides were deparaffinized in xylene, rehydrated in ethanol and rinsed in distilled water. The slides were permeabilized with 0.5% Triton X-100 (Sigma, UK) for 10 min and blocked with 10% goat serum in PBS for 20 min. The sections were incubated with 1:100 dilutions of primary anti-CD31 FITC (abcam, UK) in the dark overnight at 2–8 °C. In the next step, the samples washed with PBS 3 times for 15 min each and the slides were incubated with the secondary antibody at a 1:150 dilution according to the manufacturer’s instructions. Then, the slides were washed with PBS and counterstained with DAPI (Sigma, UK), washed with PBS and examined with a fluorescence microscope (Olympus, BX51, Japan). P values more than 0.05 were considered nonsignificant. In 5 animals in each group, 3 images were obtained from each animal and 3 fields were obtained from each image.
Intact and regenerating fibers were identified in H&E-stained slides (Thermo Fisher Scientific) and the areas of fibrous connective tissue and myofibers were identified with Masson’s trichrome staining. Briefly, the tissues were sliced, embedded in paraffin and cut into 5-μm-thick sections. The sections were visualized with a Nikon E-200 microscope and digital camera and the areas of interest were quantified with Image J software (NIH, Bethesda, MD, USA) using a color deconvolution plugin. Fibrous connective tissue areas were visualized with Masson’s trichrome staining and recorded as the percentage of the area within 500 µm of the scaffold periphery. Colored images were processed with ImageJ and Matlab software (The MathWorks Inc., Natick, MA, USA) to produce maps showing only blue-stained areas.
For immunohistochemical staining without the primary antibody, as a negative control, sections were counterstained with hematoxylin, which stains nuclei blue with a weakly alkaline solution, in contrast to the brown staining by HRP-DAB. In the present study, the control slides were stained separately from the same experimental samples. Therefore, differences in background staining were due to technical variations, e.g., in the duration of exposure of the stained slides to alcohol and xylene during the dehydration stage.
Calculation of percent positive DAB staining nuclei
To calculate the number of DAB-positive-staining nuclei referred to the total number of nuclei (DAB+, DAB−), we used ImageJ software. The images were converted to 8 bits, which showed only the DAB+ nucleus. To count both stained and unstained nuclei with precision, the cell counter plugin tool was used. The plugin automatically counts the number of clicks and provides the total number of type 1 (DAB+) and type 2 cells (DAB−). The algorithm used by the software then determines the percentage of positively-stained cells. In 5 animals in each group, 3 images were obtained from each animal and 3 fields were obtained from each image.
Quantification of centrally located nuclei
To assess myofiber regeneration in the injured area after the exercise training intervention, the density of centrally located nuclei was examined. Sections of TA were stained with H&E to quantify fiber diameters and centrally located nuclei. Images were captured with a Nikon E-200 microscope and digital camera. The percentage of the total number of centrally located nuclei was counted within 500 µm of the scaffold periphery and normalized to the total number of fibers per image in each field. In 5 animals in each group, 3 images were obtained from each animal and 3 fields were obtained from each image. P values larger than 0.05 were considered nonsignificant.
Quantitative reverse transcription PCR
Total RNA was extracted from frozen TA muscle tissue specimens of each group (n = 5) that contained approximately 50–100 mg of the regenerating area, using TRIzol according to the manufacturer’s protocol for reverse transcription to obtain cDNA. Then, 2 μL cDNA was combined with SYBR Green Ex Taq II (Tli RNaseH Plus, Bio-Rad, Hercules, CA, USA) and 200 nM forward/reverse primers using a Rotor-Gene Q 5plex System (Qiagen, Hilden, Germany). Glyceraldehyde 3-phosphate dehydrogenase (GAPDH) expression (housekeeping gene) was used as an internal control to determine the change in cycle threshold (Ct) value. Expression levels for mRNA were determined with the 2−ΔΔCt method by normalizing each treatment group to the untreated sedentary group. Primer pairs were synthesized with the DNA Oligos design tool (Sigma-Aldrich) (Table 1). P values larger than 0.05 were considered nonsignificant.
Statistical analysis
GraphPad PRISM 8.0 software was used for statistical analysis and graph generation and all figures show the results as the mean ± standard deviation. Unpaired t tests were used for between-group comparisons. Where appropriate, one-way ANOVA was done with post hoc Tukey’s pairwise comparison of adjusted means. Significance was set at conventional levels as P ≤ 0.05 (*), P ≤ 0.01 (**), P ≤ 0.001 (***), and P ≤ 0.0001 (****).
Results
Cell and tissue morphology and characterization of the VML model
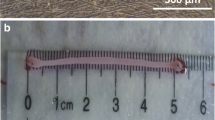
Fresh dHAM scaffolds stained with H&E are shown in Fig. 1(a,b). Cells were successfully removed from the HAM tissue. Attachment of the ADSC to the dHAM scaffold was verified by SEM observation (Fig. 1). In plates where ADSC differentiated into skeletal muscle cells, parts of the structure of muscle cells and their components were visible, which is an indication of the differentiation process (Fig. 1d). To characterize the muscle defect, we compared the ablated TA muscle with the same uninjured muscle in the opposite hindlimb. Our ablation surgery model was consistent with the standard method reported by Wu et al. (Fig. 1e, f). In each surgically created defect, approximately 30% of the TA muscle mass was lost (Wu et al. 2012).
Cell and tissue morphology in our rat model of VML. a H&E staining of fresh HAM and b successful decellularization of the HAM tissue. The photos were taken at two magnification of 1500 and 400 with a Nikon Plan Fluor × 40 oil immersion and × 10 objective. c SEM shows ADSCs were well attached and expanded on the dHAM. d ADSCs differentiated into skeletal muscle cells. The arrows indicate myoblasts and their components. e A complete view of the TA muscle. f Standard VML model ablation at × 25 magnification that was taken 1 day after the creation of VML. The image (e and f) was taken from the anterolateral orientation of tibialis anterior muscle bulk in a cross-section incision
Morphology and characterization of ADSC
Differentiation of ADSC into skeletal muscle cells was verified in different groups by immunocytochemical staining, which showed a heterogeneous population of progenitor cells according to the percentage of DAB+ nuclei (MyoD 27.3 ± 3%) and differentiation-committed cells (myogenin 23.4 ± 2%). The results showed that the ADSC could also differentiate into myogenic cells (Fig. 2a, b).
Immunocytochemical testing for ADSC differentiation into skeletal muscle cells and FACS identification of rat ADSCs in culture. Expression of myoD1 (a) and myogenin (b) at the protein level was assessed in different groups with immunecytochemical staining. The percentage of MyoD1 and myogenin proteins showed significant increases (P = 0.02 and P = 0.001, respectively). Also, negative control images are shown in the supplement section (Fig. 2). c–f Percentage of CD44 (c), CD90 (d), CD45 (e) and CD34 (f) cells by FACS analysis. Flow cytometry analyses showed that the ADSCs expressed CD44 and CD90 but the expression of CD34 and CD45 was negligible. The morphology of ADSC is spindle-shaped and specific for mesenchymal stem cells (g). Scale bar, 100 μm
Inverted microscopy examination showed that ADSC acquired a spindle-shaped morphology after 3 passages (Fig. 2). ADSC isolated from donor rats (passage 3) were characterized by the presence of standard positive and negative markers in FACS analysis (Fig. 2). It was evident from FACS analysis that ADSC expressed surface markers CD44 and CD90 but did not express CD34 or CD45, confirming the relative purity of isolated ADSC. With FACS analysis, the percentage of CD44 and CD90 cells was estimated as 99.8% and 94.2%, respectively. Figure 2 shows the average percentages of cells with CD44 and CD90 expression from separate experiments.
Histological characterization
Histological analysis 70 days after VML creation demonstrated thin myofiber growth within the scaffold. VML injury repair with bio-scaffolds containing stem cells co-cultured on dHAM exhibited renewal tissue formation, e.g., myoblast fusion, differentiated elongated fiber formation and smaller mature striated myofibers on the scaffold (Fig. 3). Within 500 µm of the scaffold periphery, the degree of fibrosis did not differ significantly between the dHAM and dHAM-ADSC groups regardless of exercise training (P = 0.18). The HIIT dHAM-ADSC subgroup (b) had significantly less fibrosis compared to the untreated sedentary subgroup (e) (P = 0.001) (Fig. 3).
Fiber formation on the scaffold part of the engineered muscle in VML injuries repaired with stem cells co-cultured on dHAM scaffolds, as shown by Masson’s trichrome staining. Black indicates nuclei, blue indicates collagen and red indicates muscle. a The interface of native tissue and muscle repaired with the bio-scaffold. b Fibrosis area of the dHAM-ADSCs group combined with HIIT. The yellow dotted line marks the demarcation between newly repaired thin myofibers and the native tissue. c, d Magnified view of the engineered scaffold. c Black arrows indicate infiltration of myofibers in dHAM and fusion of differentiated ADSCs to form new muscle fibers. d Red brackets indicate myofibers and black arrows indicate myoblasts. e Fibrosis area of the untreated sedentary group. The yellow dotted line marks the demarcation between scaffold and the native tissue. f Percentage of fibrosis area. Values are mean ± SD. Scale bar, 100× = 200 μm, 200× = 100 μm, 400× = 50 μm, 1500× = 10 μm. Statistically significant comparisons: *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001
In the muscle regeneration process, MHC is expressed relatively late in the differentiation program. Immunohistochemical analysis showed MHC proteins in the cytoplasm of newly formed fibers and demonstrated positivity for structural protein at the interface between the bio-scaffold and native tissue (Fig. 4).
Immunohistochemical staining for myosin heavy chain (MHC) shows the structure of new myofibers at the interface with native tissue. a At the interface between native and fibrotic tissue, we found no myofibers in untreated groups 70 days after VML creation. b Thin, short myofibers are shown with arrows in the sedentary dHAM-ADSCs group. c Tissues from the dHAM group showed no myofibers. d Staining for MHC showing new myofibers on the scaffold in the HIIT dHAM-ADSCs. New myofibrils are narrower and more irregular than native muscle tissue. The yellow dotted line marks the demarcation between scaffold and the native tissue. Negative control images are shown in the supplement section (Fig. 3). Scale bar, 200× = 100 μm, 400× = 50 μm
Anti-neurofilament and anti-synaptophysin staining showed evidence of innervation in the regenerating area with myofibers containing a central nucleus (Fig. 5). However, nerve formation was not detected in the groups without transplanted ADSC either with or without exercise training. In the three subgroups without exercise training, there were no mature nerves. In contrast, newly formed nerve branches were numerous in the region of the grafted scaffold with ADSC in the HIIT subgroup. Quantification of the total numbers of nerves in the whole regenerating area showed a significant between-group difference (P < 0.05) (Fig. 5).
Immunohistochemical staining for anti-neurofilaments and anti-synaptophysin showing innervation in the regenerating area. a Anti-neurofilament staining in the sedentary group shown by black arrows. b Anti-neurofilament staining in the HIIT dHAM-ADSC group shown by black arrows. c Anti-synaptophysin staining in the HIIT group shown by black arrows. d Anti-synaptophysin staining in the sedentary group (no staining was detected). Scale bar, 50 μm. Total number of nerves and mature nerves was calculated within 1000 µm of the scaffold periphery. Negative control images are shown in the supplement section (Fig. 4). e, f Number of nerves and mature nerve in the regenerating area (per mm2). Values are mean ± SD. Statistically significant comparisons: *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001
Positive staining for CD31 showed evidence of vascularization in the regenerating area with myofibers containing a central nucleus (Fig. 6). Quantification of the number of blood vessels in whole regenerating areas showed a significant difference in all exercise training subgroups compared to all sedentary subgroups. In the groups that received a bio-scaffold with ADSC the number of blood vessels in the regenerating area was significantly greater in both the HIIT and sedentary subgroups compared to untreated groups (no bio-scaffold implantation). (Fig. 6). In the HIIT subgroups, the vascular network appeared to be denser than in the other groups (Fig. 6).
Revascularization in sedentary and HIIT groups with different types of scaffolds in the ablated muscle. Positive CD31 staining in vascular structures was quantified in the regenerating area in (a, a',a'') sedentary untreated, (b, b', b'') sedentary dHAM, (c, c',c'') sedentary dHAM-ADSC and (d, d',d'') HIIT dHAM-ADSC groups. Scale bar, 50 μm. (e) Number of blood vessels in the regenerating area (per mm2). Maximal isometric force in vivo (N) (f). Expression of neurotrophic factor genes in the regenerating TA muscle defect of the dHAM-ADSC group (g, h, i) and dHAM group (j, k, l). Specimens of the defect area in sedentary and HIIT groups were compared for (g, j) BDNF, (h, k) NT3 and (i, l) NGF expression. Values are mean ± SD. Statistically significant comparisons: *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001
Measurements of force production in vivo showed that the HIIT protocol, after implantation of dHAM seeded with ADSCs, resulted in larger increases in force production and force transmission in regenerating muscle tissue after VML compared to implantation of a dHAM scaffold without stem cells (P = 0.01) and the untreated group (P = 0.0001) in the absence of exercise (Fig. 6).
Levels of neurotropic factor gene expression were compared in the sedentary and HIIT subgroups of the dHAM-ADSC and dHAM groups. In the dHAM-ADSC group, independent sample t tests for mRNA expression/GAPDH ratio (normalized in each group to the untreated sedentary subgroup) in the two subgroups showed that regardless of the type of scaffold, the dHAM-ADSC group that received HIIT had significantly higher mRNA levels for BDNF (P = 0.004) and NT3 (P = 0.0008) compared to the subgroup without HIIT, whereas mRNA levels for NGF did not differ significantly (P = 0.5) (Fig. 6). In the dHAM group, the results showed that regardless of the type of scaffold, the dHAM subgroup that received HIIT had significantly higher mRNA levels for BDNF (P = 0.001) compared to the group without HIIT, whereas mRNA levels for NGF (P = 0.12) and NT-3 (P = 0.085) did not differ significantly (Fig. 6).
The number of centrally located nuclei in new myofibers after exercise training in the HIIT dHAM-ADSC subgroup was significantly greater than in the sedentary dHAM-ADSC subgroup (P = 0.01) (Fig. 7).
Number and presence of centrally located nuclei in the two groups after 8 week HIIT. a Quantification of centrally located nuclei in the HIIT dHAM-ADSC group. Nuclei were indicated by white arrows. b Quantification of centrally located nuclei in the sedentary dHAM-ADSC group. Nuclei are indicated by black arrows (scale bar = 100 μm). Inset images are high magnification (scale bar = 50 μm). c Presence of centrally located nuclei in the injured muscle. Values are mean ± SD. Statistically significant comparisons: *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001
Discussion
This study examined the effects of combining exercise training and tissue engineering with the use of differentiated stem cells on recovery from a VML injury in a rat model. We report the first use, to our knowledge, of decellularized human amniotic membrane (dHAM) seeded with differentiated stem cells to repair a VML injury. The advantages of using this biologic scaffold, compared to other scaffolds, are its natural origin, abundance and permanent accessibility. Another innovation in the present study is the use of HIIT to aid functional rehabilitation after VML injury.
Although prior evidence suggested that soluble factors secreted by myogenic cells are effective in promoting the expression of muscle-specific proteins (Di Rocco et al. 2006; Mizuno 2010), recent studies found that transplanted stem cells may have a greater therapeutic effect than endogenous cells (Aurora and Olson 2014; Bazgir et al. 2017; Kesireddy 2016). In consonance with this mechanism, we observed greater structural and functional recovery after VML injury in animals that were treated with dHAM-ADSC bio-scaffolds than with scaffolds containing only dHAM without ADSC. Some earlier work reported that histological analysis of decellularized bio-scaffolds without donor cells disclosed large acellular regions and minimal scaffold remodeling or regeneration (Machingal et al. 2011), whereas other research showed that a decellular scaffold alone may have beneficial effects by recruiting satellite stem cells and other factors that facilitate skeletal muscle regeneration (Turner and Badylak 2012). Our results showed that regardless of whether exercise training was used or not, vascularization was significantly increased in the dHAM groups compared to the untreated group (P < 0.05).
Centrally located nuclei are an important histological marker for the fusion-mediated muscle regeneration process (Wang et al. 2014). In the present study, HIIT led to significantly larger numbers of centrally located nuclei in the HIIT dHAM-ADSC subgroup compared to the sedentary dHAM-ADSC subgroup after 8 weeks. In the regeneration process after injury, myoblasts can fuse at the site of damaged muscle, adding their nuclei to the fibers, which promotes their regeneration (Wang et al. 2014). Other studies have also reported that exercise training was associated with increased numbers of centrally located nuclei in the myofibers of new tissues (Aurora et al. 2014; Nakayama et al. 2018).
We hypothesize that exercise training increases muscle strength and generative muscle force by improving innervation. Our measurements of force production in vivo showed that the HIIT protocol after implantation of a dHAM-ADSC bio-scaffold resulted in greater force production and improved force transmission in regenerated muscle after VML compared to dHAM implantation + HIIT (P = 0.01) or sham surgical treatment + HIIT (P = 0.0001). In addition, dHAM implantation (without stem cells) in the area of VML injury, when combined with HIIT, may also favor optimal transmission of force generated by the remaining muscle tissue. In relation to the rapid functional adaptations seen in HIIT, no studies to date have attempted to clarify the neural contributions of exercising, although previous work showed that HIIT elicited different neuromuscular adaptations such as increased power output in the motor unit. These adaptations have been attributed to load intensity, volume training and other types of mechanical signaling (Burgomaster et al. 2005).
Different staining techniques showed nascent striated muscle fiber formation in the engineered side of dHAM scaffolds, indicating that repair was mediated by HIIT and differentiated ADSC. Immunohistochemical methods were used here to quantify the number of nerves and mature nerves within 1000 µm of the scaffold periphery and we conclude that HIIT increased the number of nerves approximately threefold compared to the untreated sedentary subgroup (Fig. 5). Neuromuscular junctions in regenerating areas appeared only when mature myofibers had formed. Anti-neurofilament staining detected nerve-like structures containing small myofibers or connective tissue. Anti-synaptophysin staining disclosed maturing nerves and NMJs, given that this protein is expressed in the last stages of nerve formation (Sortwell et al. 1998). Innervation is the last step in the skeletal muscle regeneration process and affects myofiber maturation and functional recovery (Quarta et al. 2017). In this study, all HIIT subgroups tended to have larger numbers of nerve components compared to sedentary subgroups. One study found that it took around 3 months for complete innervation and the maturation of nerves and NMJs (Larkin et al. 2003) and another study reported that NMJs were formed within 8 weeks, although muscle function was not complete after 12 weeks (Kang et al. 2012). The present findings showed that exercise training can reduce this time. Therefore, our results probably reflect the effective role of HIIT in the post-traumatic recovery of neuromuscular function.
One of the main findings of the present study was related to the expression of genes for neurotrophic factors. Our results showed that there were no changes in the levels of the gene expression except in the subgroups with HIIT and the differences were significant only in the training groups. Previous studies have reported that neurotrophic factors have direct and indirect influences on skeletal muscle regeneration (Lavasani et al. 2006; Sakuma and Yamaguchi 2011). These factors also promote survival, growth and differentiation of new neurons in regenerating areas (Huang and Reichardt 2001). Our results showed that in the dHAM-ADSC group that received HIIT, BDNF and NT3 mRNA levels were significantly elevated compared to untreated groups, whereas NGF mRNA levels showed no differences. Also, in the dHAM subgroup that received HIIT, BDNF mRNA levels were significantly elevated compared to the non-HIIT subgroup, whereas NT-3 and NGF mRNA levels showed no differences. The effect of the HIIT protocol on neurotrophic factor expression in the damaged skeletal muscle was, however, limited, so the HIIT intervention tested here is probably more effective in elevating BDNF and NT3 levels. However, BDNF and NT3 are more active than NGF in traumatic conditions, whereas NGF is more active in pathological conditions (Sakuma and Yamaguchi 2011). Perhaps the lack of statistical significance for the differences in NGF expression in the present study can be attributed to this issue. When comparing the expression of the BDNF gene in the dHAM-ADSC and dHAM groups, we found that in the dHAM group that did not receive stem cells, BDNF gene expression was similar to the group that received the stem cells. It may thus be concluded that HIIT training is more effective than stem cells in enhancing the expression of the BDNF gene. The mechanism of neurotrophin response to different exercise protocols is currently unclear (Domínguez-Sanchéz et al. 2018). We assume that skeletal muscle contractions during HIIT probably triggered a biochemical signaling cascade that led to increased BDNF levels in the brain or increased secretion from skeletal muscles (Domínguez-Sanchéz et al. 2018).
Another hypothesis this study aimed to test was that vascularization and vascular infiltration in dHAM and renewal tissues would be better in rats that received the dHAM-ADSC bio-scaffold with and without the HIIT protocol (Fig. 6). Accordingly, we examined the average number of blood vessels in the graft region; the results showed that this number was approximately threefold as high as in the sedentary subgroup. In addition, the density and diameter of the vessels differed: vessels in the exercise training subgroup were thicker than in the control group. Previous research showed that transplantation of a dHAM scaffold alone increased blood vessel numbers and was associated with progression in angiogenesis (Shi et al. 2015; Song et al. 2017). Moreover, HIIT reportedly triggered angiogenesis and vascularization (Cocks and Wagenmakers 2016; Hoier et al. 2013). Exercise training has also been shown to increase capillary density based on the detection of vascular endothelial growth factor (VEGF) and the presence of endothelial progenitor cells (Amaral et al. 2001). One possible mechanism by which HIIT may enhance vascularization is the increased blood flow through capillaries and upregulation of endothelial nitric oxide synthase (eNOS) and NOX2 levels (Cocks et al. 2013). In this connection, HIIT led to increased mRNA expression of proteins involved in angiogenesis and was also reported to provide a stimulus for VEGF secretion and endothelial cell proliferation (Cocks et al. 2013; Cocks and Wagenmakers 2016; Hoier et al. 2013).
Enhancing myogensis and inhibiting fibrosis are two concerns in any approach to treatment for VML injuries. A notable finding in the present study is that HIIT resulted in less fibrosis only in the dHAM-ADSC group. A major component of the dHAM scaffold is collagen. Because decellularized scaffolds are predominantly composed of collagen I, no reduction in fibrosis levels would be expected (Fig. 4) with the dHAM interventions.
A potential limitation of this study is that the decellularized scaffolds used were xenogenic and not derived from skeletal muscle. Another limitation was the lack of testing in larger animal models, which should be undertaken in future research aimed at clinical translation.
In future studies, a multilayer amniotic membrane scaffold may be an effective way to fill the site of muscle ablation. We suggest that future studies should test the combination of dHAM scaffolds with electrospun fibers or nanofiber coatings. Another line of research worth investigating is satellite cell activation—a necessary mechanism of muscle regeneration after VML injury. Earlier work reported an increase in satellite cell populations after HIIT (Bazgir et al. 2017; Joanisse et al. 2013). Therefore, future studies could focus on the role of satellite cells in combination with biologic scaffolds in the repair of muscle injuries. Although tissue engineered scaffold technology is being investigated to treat VML injuries in large muscles, it could also potentially be used to treat congenital problems such as cleft lip or small muscle defects.
In conclusion, our study shows that a dHAM scaffold seeded with differentiated ADSC, when combined with high-intensity interval training, can enhance muscle regeneration and improve the remodeling of functional tissue after volumetric muscle loss injury in rats. The putative mechanism underlying regeneration is the induction of revascularization and re-innervation. High-intensity interval training may amplify some physiological processes in injured muscles by increasing the expression of neurotrophic factors. The implications of these findings are of potential importance for future efforts to develop engineered biological scaffolds and for the use of interval training programs in rehabilitation after traumatic muscle loss.
References
Amaral SL, Papanek PE, Greene AS (2001) Angiotensin II and VEGF are involved in angiogenesis induced by short-term exercise training. American Journal of Physiology-Heart and Circulatory Physiology 281:H1163–H1169
Aurora A, Garg K, Corona BT, Walters TJ (2014) Physical rehabilitation improves muscle function following volumetric muscle loss injury. BMC Sports Science, Medicine and Rehabilitation 6:41
Aurora AB, Olson EN (2014) Immune modulation of stem cells and regeneration. Cell Stem Cell 15:14–25
Bazgir B, Fathi R, Valojerdi MR, Mozdziak P, Asgari A (2017) Satellite cells contribution to exercise mediated muscle hypertrophy and repair. Cell J 18(4):473–484. https://doi.org/10.22074/cellj.2016.4714
Burgomaster KA, Hughes SC, Heigenhauser GJ, Bradwell SN, Gibala MJ (2005) Six sessions of sprint interval training increases muscle oxidative potential and cycle endurance capacity in humans. J Appl Physiol 98:1985–1990
Chagastelles PC, Nardi NB (2011) Biology of stem cells: an overview. Kidney International Supplements 1:63–67. https://doi.org/10.1155/2011/201696
Cocks M et al (2013) Sprint interval and endurance training are equally effective in increasing muscle microvascular density and eNOS content in sedentary males. The Journal of Physiology 591:641–656
Cocks M, Wagenmakers AJ (2016) The effect of different training modes on skeletal muscle microvascular density and endothelial enzymes controlling NO availability. The Journal of Physiology 594:2245–2257
Corona BT et al (2012) Further development of a tissue engineered muscle repair construct in vitro for enhanced functional recovery following implantation in vivo in a murine model of volumetric muscle loss injury. Tissue Eng Part A 18:1213–1228
Di Rocco G et al (2006) Myogenic potential of adipose-tissue-derived cells. J Cell Sci 119:2945–2952
Domínguez-Sanchéz MA et al (2018) (2018) Acute effects of high intensity, resistance, or combined protocol on the increase of level of neurotrophic factors in physically inactive overweight adults: The Brainfit Study. Front Physiol 9:741
Dunn A, Marcinczyk M, Talovic M, Patel K, Haas G, Garg K (2018) Role of stem cells and extracellular matrix in the regeneration of skeletal muscle. Muscle Cell and Tissue - Current Status of Research Field. https://doi.org/10.5772/intechopen.75828
Fouad H, Sabry D, Elsetohy K, Fathy N (2016) Therapeutic efficacy of amniotic membrane stem cells and adipose tissue stem cells in rats with chemically induced ovarian failure. Journal of Advanced Research 7:233–241
Gholipourmalekabadi M, Sameni M, Radenkovic D, Mozafari M, Mossahebi-Mohammadi M, Seifalian A (2016) Decellularized human amniotic membrane: how viable is it as a delivery system for human adipose tissue-derived stromal cells? Cell Prolif 49:115–121
Hoier B, Passos M, Bangsbo J, Hellsten Y (2013) Intense intermittent exercise provides weak stimulus for vascular endothelial growth factor secretion and capillary growth in skeletal muscle. Exp Physiol 98:585–597
Hua Y, Liu YH, Sahashi K, Rigo F, Bennett CF, Krainer AR (2015) Motor neuron cell-nonautonomous rescue of spinal muscular atrophy phenotypes in mild and severe transgenic mouse models. Genes Dev 29:288–297. https://doi.org/10.1101/gad.256644.114
Huang EJ, Reichardt LF (2001) Neurotrophins: roles in neuronal development and function. Annu Rev Neurosci 24:677–736
Joanisse S, Gillen JB, Bellamy LM, McKay BR, Tarnopolsky MA, Gibala MJ, Parise G (2013) Evidence for the contribution of muscle stem cells to nonhypertrophic skeletal muscle remodeling in humans. FASEB J 27:4596–4605
Kang S-B, Olson JL, Atala A, Yoo JJ (2012) Functional recovery of completely denervated muscle: implications for innervation of tissue-engineered muscle. Tissue Eng Part A 18:1912–1920
Kesireddy V (2016) Evaluation of adipose-derived stem cells for tissue-engineered muscle repair construct-mediated repair of a murine model of volumetric muscle loss injury. Int J Nanomed 11:1461
Kraljevic J, Marinovic J, Pravdic D, Zubin P, Dujic Z, Wisloff U, Ljubkovic M (2013) Aerobic interval training attenuates remodelling and mitochondrial dysfunction in the post-infarction failing rat heart. Cardiovasc Res 99:55–64
Larkin LM, Kuzon WM Jr, Halter JB (2003) Effects of age and nerve-repair grafts on reinnervation and fiber type distribution of rat medial gastrocnemius muscles. Mech Ageing Dev 124:653–661
Lavasani M, Lu A, Peng H, Cummins J, Huard J (2006) Nerve growth factor improves the muscle regeneration capacity of muscle stem cells in dystrophic muscle. Hum Gene Ther 17:180–192
Liu J, Saul D, Böker KO, Ernst J, Lehman W, Schilling AF (2018) Current Methods for Skeletal Muscle Tissue Repair and Regeneration. Biomed Res Int 2018:1984879
Machingal MA et al (2011) A tissue-engineered muscle repair construct for functional restoration of an irrecoverable muscle injury in a murine model. Tissue Eng Part A 17:2291–2303
Messi ML, Li T, Wang Z-M, Marsh AP, Nicklas B, Delbono O (2015) Resistance training enhances skeletal muscle innervation without modifying the number of satellite cells or their myofiber association in obese older adults. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences 71:1273–1280
Mizuno H (2010) The potential for treatment of skeletal muscle disorders with adipose-derived stem cells. Current Stem Cell Research & Therapy 5. 133–6. https://doi.org/10.2174/157488810791268573.
Nakayama KH et al (2018) Rehabilitative exercise and spatially patterned nanofibrillar scaffolds enhance vascularization and innervation following volumetric muscle loss. NPJ Regenerative medicine 3:16
Nederveen J, Joanisse S, Séguin C, Bell K, Baker S, Phillips S, Parise G (2015) The effect of exercise mode on the acute response of satellite cells in old men. Acta Physiol 215:177–190
Niknejad H, Peirovi H, Jorjani M, Ahmadiani A, Ghanavi J, Seifalian AM (2008) Properties of the amniotic membrane for potential use in tissue engineering. Eur Cells Mater 15:88–99
Pantelic MN, Larkin LM (2018) Stem cells for skeletal muscle tissue engineering. Tissue Engineering Part B: Reviews 24:373–391
Pugh JK, Faulkner SH, Jackson AP, King JA, Nimmo MA (2015) Acute molecular responses to concurrent resistance and high-intensity interval exercise in untrained skeletal muscle. Physiological Reports 3:e12364
Quarta M et al (2017) Bioengineered constructs combined with exercise enhance stem cell-mediated treatment of volumetric muscle loss. Nature Communications 8:15613
Sakuma K (2011) Yamaguchi A (2011) The recent understanding of the neurotrophin’s role in skeletal muscle adaptation. Journal of Biomedicine & Biotechnology 2011:201696
Shi P, Gao M, Shen Q, Hou L, Zhu Y, Wang J (2015) Biocompatible surgical meshes based on decellularized human amniotic membrane. Mater Sci Eng, C 54:112–119
Song M, Wang W, Ye Q, Bu S, Shen Z, Zhu Y (2017) The repairing of full-thickness skin deficiency and its biological mechanism using decellularized human amniotic membrane as the wound dressing. Mater Sci Eng, C 77:739–747
Sortwell CE et al (1998) Pattern of synaptophysin immunoreactivity within mesencephalic grafts following transplantation in a parkinsonian primate model. Brain Res 791:117–124
Turner NJ, Badylak SF (2012) Regeneration of skeletal muscle. Cell Tissue Res 347:759–774
VanDusen KW, Syverud BC, Williams ML, Lee JD, Larkin LM (2014) Engineered skeletal muscle units for repair of volumetric muscle loss in the tibialis anterior muscle of a rat. Tissue Eng Part A 20:2920–2930
Wang L, Cao L, Shansky J, Wang Z, Mooney D, Vandenburgh H (2014) Minimally invasive approach to the repair of injured skeletal muscle with a shape-memory scaffold. Mol Ther 22:1441–1449
Wu X, Corona BT, Chen X, Walters TJ (2012) A standardized rat model of volumetric muscle loss injury for the development of tissue engineering therapies. BioResearch Open Access 1:280–290
Zoladz J, Majerczak J, Zeligowska E, Mencel J, Jaskolski A, Jaskolska A, Marusiak J (2014) Moderate-intensity interval training increases serum brain-derived neurotrophic factor level and decreases inflammation in Parkinson’s disease patients. J Physiol Pharmacol 65:441–448
Zuk PA et al (2002) Human adipose tissue is a source of multipotent stem cells. Mol Biol Cell 13:4279–4295
Acknowledgements
We thank all the participants who donated amniotic membrane samples for this study. The authors thank Dr. Vahid Bayati, Cellular and Molecular Research Center, Ahvaz Jundishapur University of Medical Sciences, for fruitful comments during the preparation of this paper. This article is extracted from the Ph.D. thesis awarded to M.R.I. by the Department of Exercise Physiology, Faculty of Physical Education and Exercise Sciences, Shahid Chamran University of Ahvaz. We thank K. Shashok (AuthorAID in the Eastern Mediterranean) for editing the use of English in the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
Human amniotic membrane was obtained and used in accordance with the guidelines provided by the Experimental Animal Care and Ethics Committee of Shahid Chamran University of Ahvaz (Ethical approval number: EE/97.24.370024/scu.ac.ir). All applicable international, national and/or institutional guidelines for the care and use of animals were followed.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Izadi, M.R., Habibi, A., Khodabandeh, Z. et al. Synergistic effect of high-intensity interval training and stem cell transplantation with amniotic membrane scaffold on repair and rehabilitation after volumetric muscle loss injury. Cell Tissue Res 383, 765–779 (2021). https://doi.org/10.1007/s00441-020-03304-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-020-03304-8