Abstract
REM sleep is characterized by rapid eye movements, desynchronized electroencephalographic activity, dreams and muscle paralysis that preclude the individual from acting out the action of dreams. REM sleep is generated and modulated by a complex and still poorly understood, neuronal network that involves multiple nuclei and neurotransmission systems. The key structures that generate REM sleep muscle paralysis are the subcoeruleus nucleus in the mesopontine tegmentum and the reticular formation of the ventral medial medulla. Using glutamatergic, GABAergic and glycinergic inputs, direct and indirect projections from these two areas inhibit the motoneurons of the spinal cord resulting in skeletal paralysis in REM sleep. Experimental studies in cats and rodents where the subcoeruleus nucleus and ventral medial medulla were impaired by electrolytic, pharmacological and genetic manipulations have repeatedly produced increased electromyography activity during REM sleep associated with abnormal motor behaviors (e.g., prominent twitching, attack-like behaviors). These animal models represent the pathophysiological substrate of REM sleep behavior disorder, a parasomnia in humans characterized by nightmares and abnormal vigorous behaviors (e.g., prominent jerking, shouting, kicking) linked to excessive phasic and/or tonic electromyographic activity in REM sleep. The extraordinary observation that a sleep disorder is often the first manifestation of a devastating neurodegenerative disease such as Parkinson disease carries important diagnostic implications and opens a window for neuroprotection. This review addresses the neuronal substrates of REM sleep generation and modulation and how its impairment may lead to REM sleep behavior disorder.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleep is a normal, recurring, and reversible state characterized by loss of consciousness, unresponsiveness to the environment and reduced bodily movement. Contrary to popular belief, sleep is not a passive state. Sleep involves dynamic changes in cellular functioning that are controlled by precise neural structures and networks. Functions of sleep are multiple and include regulation of gene expression, protein synthesis and clearance, cardiovascular and endocrine functions, thermoregulatory and energy conservation, maintenance of the immune system and memory consolidation. Sleep is divided in two different states, non-rapid eye movement (NREM) sleep and rapid eye movement (REM) sleep. Each state has different neuronal, metabolic and biochemical substrates (Irwin 2015; Mander et al. 2017; Scammel et al. 2017; Silber et al. 2004). REM sleep is characterized by rapid eye movements, desynchronized electroencephalographic activity, dreams, minimal phasic muscles twitches in distal limbs and complete muscle atonia in axial postural muscles that preclude the sleeper from physically acting out the action of dreams (Peever and Fuller 2017; Scammel et al. 2017).
Sleep may be affected by pathological processes resulting in sleep problems such as the parasomnias. Parasomnias are abnormal behaviors and experiences occurring during entry into sleep or arousal from sleep, within NREM sleep (e.g., sleepwalking, sleep terrors) or REM sleep. REM sleep parasomnias comprise recurrent sleep paralysis, recurrent nightmares and REM sleep behavior disorder (RBD) (American Academy of Sleep Medicine 2014). RBD is characterized by unpleasant dreams and vigorous behaviors (e.g., prominent jerking, punching, shouting) linked to excessive electromyographic (EMG) activity in REM sleep. RBD reflects damage of the neuronal structures that regulate REM sleep. RBD is not a mere parasomnia without neurological consequences. Follow-up of subjects with the idiopathic form of RBD (IRBD) showed that the vast majority are eventually diagnosed with a neurodegenerative disease, namely the synucleinopathies Parkinson disease (PD), dementia with Lewy bodies (DLB) and multiple system atrophy (MSA). The finding that a parasomnia may represent the initial manifestation of a synucleinopathy carries important implications (Högl et al. 2018; Iranzo et al. 2016). This article reviews the physiology of REM sleep and the pathophysiology and implications of RBD.
REM sleep generation and modulation
REM sleep was discovered in 1953 by Aserinsky and Kleitman (1953). It is also called paradoxical sleep (Luppi et al. 2011) and active sleep (Fung et al. 2011). REM sleep occurs in almost all species and is thought to be involved in cortical plasticity, restoration of receptor function, brain and sensorimotor development, memory consolidation, learning and preparing the individual for ensuing wakefulness (Arrigoni et al. 2016; Peever and Fuller 2017). The neural network that generates REM sleep is responsible for the parameters for REM sleep onset latency, percentage of REM sleep during the night, number of REM sleep periods and EMG atonia. A large number of anatomic structures are directly or indirectly implicated in the generation and maintenance of the sleep-wake cycle where REM sleep is one of the main components. These structures are mainly located in the lower brainstem, limbic system, thalamus, hypothalamus and cortex. Such a large number of different structures explain why many neurotransmitters have been implicated in REM sleep generation and modulation including glutamate, gamma-aminobutyric acid (GABA), glycine, hypocretin/orexin, melanin concentrating hormone (MCH), melatonin, histamine, acetylcholine, dopamine, serotonin and noradrenaline (Fraigne et al. 2015; Fuller et al. 2007, 2011; Luppi et al. 2011, 2013; Peever and Fuller 2017).
The critical structures for REM sleep generation and REM sleep muscle atonia are located in the mesopontine tegmentum and in the ventral medial medulla (VMM). In these regions, there exist a large number of nuclei that send projections inhibiting or activating nearby nuclei in the brainstem or other distant brain regions. For the basic researcher, working in such a tiny region is a challenge as some nuclei can be difficult to identify. When trying to damage a specific brainstem nucleus with a cytotoxic injection, the lesion may expand to surrounding nuclei or unintended neurons within the nucleus producing unexpected results. More clean and accurate results can be obtained using c-Fos labelling, retrograde and anterograde tracing, administration of neurotransmitters agonists and antagonists, selective electric stimulation, genetic manipulation with knockout animals of neurotransmitters and receptors, genetic inactivation using adeno-associated viruses and optogenetics. Experimental studies in animals have provided a great knowledge on the generation of REM sleep. However, results in animals may depend on the species studied (rats, mice, felines, dogs, non-human primates) because the location of some nuclei may be different.
For the clinician, REM sleep generation and RBD pathophysiology are very difficult to understand not only because of their complexity and the changing nature of the field but also because different terminology is used to label the same structures across species and across different group of investigators and anatomic atlas. For example, the subcoeruleus nucleus in humans is the equivalent to peri-locus coeruleus alpha nucleus (peri-LCa) in cats and to the sublaterodorsal tegmental nucleus (SLD) in rats and mice. The subcoeruleus nucleus in humans is located ventral and slightly rostral to the locus coeruleus (LC) and the SLD in rodents is ventral to the laterodorsal tegmental nucleus (LDT). The seemingly different location of the subcoeruleus and SLD is due to the fact that the LC in primates and humans and even in cats extends very rostrally. The subcoeruleus nucleus is also named pontine inhibitor area (PIA) dorsal nucleus pontis oralis (PnO), dorsal rostral pontine reticular nucleus and ventral laterodorsal tegmental nucleus depending on the investigators or the anatomic atlas (Fuller et al. 2007; Fung et al. 2011; Luppi et al. 2011; Reinoso-Suárez et al. 2001). This review will use the terms subcoeruleus nucleus and SLD. The cholinergic pedunculopontine tegmental nucleus (PPT) is also called pedunculopontine nucleus (PPN) and subpenducular tegmental nucleus. In the VMM, the ventral gigantocellular (GiV) nucleus in rodents corresponds to the nucleus magnocellularis in cats. The VMM contains medium and small size neurons as well and a complex large number of nuclei have been identified, namely the GiV, the nucleus raphe magnus (RMg), alpha-gigantocellular reticular nucleus (GiA), laterally adjacent paragigantocellular (LPGi) cell groups and dorsal paragigantocellular reticular nucleus (DPGi). In the VMM, the inferior olive is also called supraolivary medulla (SOM).
Although it was first thought that central mechanisms generating REM sleep were cholinergic and monoaminergic in nature, recent evidence indicate that the system responsible for REM sleep generation is more complex, involving critical GABAergic and glutamatergic neurotransmission in the brainstem (Boissard et al. 2002 and Boissard et al. 2003; Crochet and Sakai 2003; Lu et al. 2006; Luppi et al. 2007). Early pharmacological and electrophysiological experiments in the mesopontine tegmentum of animals showed that cholinergic administration promotes REM sleep whereas serotonin and noradrenaline application suppresses REM sleep. However, selective lesions of the mesopontine cholinergic nuclei (PPT and LDT), serotonergic nuclei (dorsal raphe nucleus (DRN)) and noradrenergic nuclei (LC) did not change the amount of REM sleep or had an effect on the muscular activity during REM sleep. This suggested that there were additional brain regions and neurotransmitter systems that are more critically involved in the generation of REM sleep (Luppi et al. 2011).
Studies in rodents revealed the presence of non-monoaminergic and non-cholinergic REM-on and REM-off structures in the mesopontine tegmentum that form the basis of a REM sleep generation model that is analogous to an electronic flip-flop switch. This flip-flop switch consists in a rapid and complete transition from REM sleep to NREM sleep and back. In this model, REM-on neurons inhibit REM-off neurons and vice versa. This mutually inhibitory relationship ensures fast transitions from one state to another (but not from and to wakefulness). REM-on neurons fire during REM sleep and enhance this sleep stage. During NREM sleep, REM-on neurons do not fire because they are inhibited by REM-off cells (Lu et al. 2006). REM-on neurons in rodents are GABAergic in nature and located in the dorsal part of the sublaterodorsal nucleus (SLD). It has been speculated that the REM-on neurons in the SLD that generate REM sleep are glutamatergic and not GABAergic (Clement et al. 2011). It is also possible that the glutamatergic caudal region of the LDT (cLDT) contains also REM-on neurons. REM-off cells are GABAergic and are located in the lateral pontine tegmentum (LPT, also called the deep mesencephalic nucleus (DpME)) and in the ventrolateral periaqueductal gray matter (vlPAG) (Lu et al. 2006).
The flip-flop model of REM sleep generation, however, is much more complex and involves a large number of other brain regions and neurotransmitter systems that act as modulators. Other structures and neurotransmitters modulate the REM-on cells of the SLD and also the REM-off cells of the LPT and vlPAG. These structures and their corresponding neurotransmitters have an important role in the modulation but not generation, of the flip-flop switch model. The following structures are thought to promote REM sleep either activating the REM-on neurons of the SLD or inhibiting the REM-off cells of the LPT and vlPAG: the GABAergic extended ventrolateral preoptic nucleus (eVLPO) in the hypothalamus, the MCH cells in the hypothalamus, the glutamatergic cells from the central nucleus of the amygdala, the cholinergic PPT and LDT in the mesopontine tegmentum, the glutamatergic cells from the periaqueductal gray matter (PAG) and caudal GABAergic projections from the DPGi and LPGi arising from the VMM (Lu et al. 2006; Weber et al. 2015). MCH neurons promote REM sleep and wakefulness inhibiting the LPT and vlPAG but also inhibiting the histaminergic neurons of the tuberomammillary nucleus (TMN) of the thalamus, the noradrenergic cells of the LC and the serotonergic neurons of the DRN (Fraigne et al. 2015). Conversely, the following structures activate the REM-off sleep neurons of the LPT and vlPAG: the hypocretinergic/orexinergic cells in the dorsolateral hypothalamus and several brainstem nuclei such as the serotonergic DRN, noradrenergic LC and dopaminergic ventral periaqueductal gray matter (vPAG) (Lu et al. 2006) (Fig. 1). The noradrenergic LC and serotonergic DR neurons inhibit REM sleep generation inactivating the SLD, PPT and LDT and activating the LPT and vlPAG (Arrigoni et al. 2016). The neurons in the core of the ventrolateral preoptic nucleus (VLPO) regulate NREM sleep while the dorsal and medial neurons (the eVLPO) are involved in REM sleep (Lu et al. 2006). Of note, the cholinergic PPT and LDT nuclei promote REM sleep through (1) activation of the inhibitory M2 and M4 receptors of the vlPAG and LPT and (2) activation of the excitatory M1 and M3 receptors of the SLD (Lu et al. 2006).
REM sleep flip-flop model. In this flip-flop model, the REM-on structures promote REM sleep inhibiting the REM-off structures, while the REM-off nuclei inhibit REM sleep through inhibition of the REM-on structures. REM-on structures are in blue and REM-off structures are in red. Dash line, inhibition; plus sign, activation; ACh, acetylcholine; cLDT, caudal lateral dorsal tegmentum; CNA, central nucleus of the amygdala; DA, dopamine; DPGi, dorsal paragigantocellular reticular nucleus; DRN, dorsal raphe nucleus; eVLPO, extended ventrolateral preoptic nucleus; GABA, gamma-aminobutyric acid; Glut, glutamate; Hypoth, hypothalamus; LC, locus coeruleus nucleus; LDT, lateral dorsal tegmentum; LPT, lateral pontine tegmentum; MCH, melanin concentrating hormone; NA, noradrenaline; PAG, periaqueductal gray matter; PPT, pedunculopontine tegmentum nucleus; SLD, sublaterodorsal nucleus; VlPAG, ventrolateral part of the periaqueductal gray matter; VMM, ventral medial medulla; VPAG, ventral part of the periaqueductal gray matter; 5-HT, serotonin
Neuronal activation during REM sleep is not only confined to the nuclei located in the brainstem. Functional neuroimaging studies in humans during REM sleep show activation of not only the pontine tegmentum but also the thalamus, basal forebrain, limbic areas (amygdala, hippocampus, anterior cingulate cortex) and temporo-occipital cortices. Functional neuroimaging during REM sleep also shows deactivation of the dorsolateral prefrontal cortex, inferior parietal cortex, precuneus and posterior cingulate gyrus (Dang-Vu et al. 2010).
The characteristic electroencephalographic activity of REM sleep is generated by ascending glutamatergic inputs from the dorsal part of the SLD (Krenzer et al. 2011; Peever and Fuller 2017). These inputs reach the precoeruleus area (PC, which is located in the pons rostral to the LC), the parabrachial nucleus (PB, which is located in the basal forebrain), the PPT and the LDT. Glutamatergic projections from the PB and PC and cholinergic projections from the PPT and LDT reach the intralaminar and reticular thalamic nuclei, lateral hypothalamus and basal forebrain, which in turn reach the cortex and hippocampus producing cortical activation (Fuller et al. 2011; Lu et al. 2006; Luppi et al. 2011; Peever and Fuller 2017). REM sleep cortical activation is also mediated by decreased noradrenergic activity in the LC, reduced serotonergic activity in the DRN, decreased histaminergic activity in the TMN of the thalamus and reduced hypocretinergic/orexinergic activity in the lateral hypothalamus (Peever and Fuller 2017). Neuroimaging and animals studies have shown that during REM sleep, the somatosensory cortex is deactivated while some structures of the limbic cortex are activated such as the anterior cingulate, retrospinal, entorhinal cortex and dentate gyrus (Luppi et al. 2017). These limbic structures receive inputs from the claustrum, medial septum and suprammamilary nucleus during REM sleep (Luppi et al. 2017).
The typical rapid eye extrinsic movements seen in REM sleep are mediated by brainstem structures involved in ocular motility such as the para-abducens nucleus and medial pontine reticular formation (Reinoso-Suárez et al. 2001).
REM sleep muscle paralysis
In humans and animals, the muscle paralysis seen in REM sleep is characterized by (1) continuous sustained absence of muscle tone (also known as “REM sleep atonia”) and (2) few intermittent bursts of muscular activity that can be associated with minimal muscle twitches resulting in brief and small distal movements of the limbs, ears, orofacial area, jaw and tail (also known as “REM sleep EMG phasic activity”). REM sleep muscle paralysis requires (1) sustained inhibition throughout the REM sleep period of the tonic EMG activity that underlies the postural tone and (2) disfacilitation of the phasic EMG activity that influences movements and locomotion. In other words, muscle tone in REM sleep is reduced by combined activation of inhibitory systems and inactivation of facilitatory systems. The final result is inhibition of the motoneurons located in the nuclei of the cranial nerves of the brainstem (e.g., hypoglossal, trigeminal, facial) and of the motoneurons of the spinal cord, both resulting in skeletal muscle atonia and minimal intermittent muscle twitches (Chase et al. 1989; Chase 2008).
The key structures that generate REM sleep paralysis are the ventral region of the SLD (vSLD) in the mesopontine tegmentum and several nuclei within the VMM including the RMg, GiA, GiV and LPGi (Arrigoni et al. 2016; Boissard et al. 2002, 2003; Fraigne et al. 2015; Krenzer et al. 2013; Lu et al. 2006; Peever et al. 2014). The neurons of the VMM that promote REM sleep paralysis are located at the level of the supraolivary medulla (SOM), which is the rostro-caudal segment of the gigantocellular reticular field and corresponds to the RMg, GiA, GiV and LPGi (Vetrivelan et al. 2009).
The SLD contains GABA, glutamate and cholinergic cells. The dorsal part of the SLD uses GABA transmission and through the flip-flop model regulates the transition from NREM sleep to REM sleep and induces cortical activation during REM sleep. Thus, the dorsal part of SLD regulates REM sleep onset and maintenance but not REM sleep paralysis. In contrast, the vSLD contains mainly glutamatergic cells and is implicated in the control of REM sleep muscle paralysis. The vSLD generates muscle paralysis by two different pathways (Fig. 2). There is a direct pathway of excitatory vSLD glutamatergic projections to the interneurons of the spinal cord, which in turn inhibit the ventral horn skeletal motoneurons with GABA/Glycinergic inputs (Lu et al. 2006). An indirect polysynaptic pathway consists of other descending glutamatergic vSLD neurons that send their projections to the VMM (Sakai et al. 1979), which in turn inhibits the motor neurons of the ventral horn of the spinal cord resulting in muscle paralysis. The neurons of the VMM release GABA/glycine to the ventral horn motoneurons (Chase 2008; Luppi et al. 2011) and glutamate (Brooks and Peever 2008; Vetrivelan et al. 2009) to the spinal cord GABA/glycinergic interneurons, which in turn inhibit the motoneurons of the ventral horn. The red nucleus in the midbrain activates the motoneurons in the spinal cord and produce muscular twitches during REM sleep. The VMM inhibits the activity of the red nucleus to reduce the production of phasic EMG activity that could be excessive to allow the release of movements (Blumberg and Plumeau 2016).
Schematic diagram of REM sleep muscle paralysis circuitry. The vSLD in the mesopontine tegmentum is the main structure that promotes REM sleep muscle paralysis. It inhibits the spinal cord motoneurons through a direct pathway and also through an indirect pathway that relies on the VMM. The direct pathway inhibits the tonic electromyographic activity. The indirect pathway defacilitates the phasic electromyographic activity as the red nucleus is inhibited by the VMM. Damage to the vSLD and VMM both result in REM sleep behavior disorder. Transgenic mice with deficient glycine and GABA receptors also result in REM sleep behavior disorder. Dash line, inhibition; plus sign, activation; GABA, gamma-aminobutyric acid; Gly, glycine; RN, red nucleus; VMM, ventral medial medulla; vSLD, ventral sublaterodorsal nucleus
The glutamatergic descending neurons from the vSLD that decrease REM sleep muscular activity are modulated by direct and indirect projections from the brainstem and from supratentorial structures (Fig. 3). They include inhibitory afferents from GABAergic neurons from the LPT, serotonergic neurons from the DRN, noradrenergic neurons from the LC and hypocretinergic/orexinergic neurons from the dorsolateral hypothalamus. The vSLD also receives excitatory glutamatergic projections from the primary motor area of the frontal cortex, supplementary somatosensory area, central nucleus of the amygdala, PAG, PPT and LDT (Boissard et al. 2003). The substantia nigra pars reticulata and the internal segment of the globus pallidum send GABAergic projections to the PPT, which in turn excite the neurons of the VMM with glutamatergic and cholinergic inputs (Rye 1997; Rye and Bliwise 2004).
Afferents of the ventral sublaterodorsal nucleus and ventral medial medulla in the control of REM sleep muscle paralysis. During REM sleep, (1) the vSLD is activated through excitatory inputs from the cortex, VMPJ, amygdala, PPT and LDT and (2) the VMM is activated through excitatory inputs from the VMPJ and PPT/MEA. The inhibitory activity of the hypocretinergic hypothalamus, serotonergic DRN and noradrenergic LC nuclei does not occur during REM sleep. Dash line, inhibition; plus sign, activation; ACh, acetylcholine; CNA, central nucleus of the amygdala; DRN, dorsal raphe nucleus; GABA, gamma-aminobutyric acid; Glu, glutamate; GPi, internal segment of the globus pallidus; Hypoth, hypothalamus; LC, locus coeruleus nucleus; LDT, lateral dorsal tegmentum; LPT, lateral pontine tegmentum; MEA, midbrain extrapyramidal area; NA, noradrenaline; PAG, periaqueductal gray matter; PPT, pedunculopontine tegmentum nucleus; SNr, substantia nigra pars reticulata; VMM, ventral medial medulla; VMPJ, ventral mesopontine junction; vSLD, ventral sublaterodorsal nucleus; 5-HT, serotonin
On the other hand, the ventral mesopontine junction (VMPJ) is a region that includes the substantia nigra pars reticulata, the caudal portion of the retrorubral nucleus and the ventral tegmental area. The VMPJ is also involved in the control of muscle tone since glutamatergic neurons from this region activate the vSLD and VMM promoting REM sleep muscle paralysis (Siegel 2009).
Pathophysiology of REM sleep behavior disorder
In humans, RBD is clinically characterized by unpleasant dream recall (e.g., being attacked and chased) and abnormal simple (e.g., prominent jerks) and elaborated (e.g., kicking, punching singing, talking, gesturing, jumping out of bed) behaviors during REM sleep. Polysomnographic recordings in humans show increased phasic EMG activity and/or sustained tonic EMG activity during REM sleep (Boeve 2013; Högl et al. 2018; Iranzo et al. 2016; Lapierre and Montplaisir 1992). In patients with RBD, other components of REM sleep are normal such as density of rapid eye movements, REM sleep onset latency, percentage of REM sleep across the night and number of REM sleep periods. In patients with IRBD, NREM sleep architecture and wakefulness are usually normal.
Basic science using experimental animals (e.g., cats and rodents) indicates that RBD is caused by dysfunction of the nuclei that generates REM sleep paralysis, namely the subcoeruleus nucleus and nuclei from the VMM. This is supported by postmortem and neuroimaging studies in patients with RBD (Ehrminger et al. 2016; Iranzo et al. 2013; Scherfler et al. 2011). This indicates that impairment of glutamatergic neurotransmission from the subcoeruleus nucleus and/or GABAergic and glycinergic neurotransmission from the VMM underlies the pathophysiology of RBD. Alternatively, it is plausible that RBD can also be caused by damage of the anatomical connections of the subcoeruleus nucleus and VMM with other structures such as the dorsolateral hypothalamus and the limbic system. Thus, other neurotransmitters systems (e.g., monoamines, acetylcholine and hypocretin/orexin) can also be involved in the pathophysiology of RBD. Our knowledge on the pathophysiology of RBD is based on (1) the existence of experimental animal models of RBD and (2) the occurrence of humans with RBD secondary to neurodegenerative diseases, narcolepsy, autoimmune diseases, focal structural lesions in the brain and the effect of some medications. This section of this review will address these two aspects.
Animal models of REM sleep behavior disorder
Experimental studies in cats and rodents impairing the SLD or the VMM produce REM sleep with excessive EMG activity associated with abnormal behaviors during unequivocal REM sleep. These abnormal behaviors may range from prominent twitches and jerks to goal-directed behaviors such as hunting-like movements. The severity of the behaviors depends on the region in the brain that is damaged and its extent. Interestingly, selective damage of these brainstem regions does not affect wakefulness and NREM sleep and REM sleep amount is usually not changed. Selective impairment of the vSLD produces REM sleep without atonia preserving the amount of REM sleep. When the lesion of the vSLD extends to surrounding areas such as the cholinergic caudal LDT, the REM sleep time is then reduced (Krenzer et al. 2013). The animal models of RBD have been induced by electrolytic and neurochemical lesions and by pharmacological and genetic manipulation of glutamate, GABA and glycinergic neurotransmission (Luppi et al. 2013).
Animal models involving the subcoeruleus/SLD nucleus
Jouvet and Delrome showed in 1965 that electrolytic lesions of the subcoeruleus region in cats resulted in REM sleep without atonia associated with simple and complex motor behaviors such as orienting, walking and attacking (Jouvet and Delrome 1965). This observation was confirmed by many other investigators (Hendricks and Morrison 1981; Hendricks et al. 1982; Morrison et al. 1981; Shouse and Siegel 1992). It was shown that the site and extent of the lesions in the pontine tegmentum determine the severity of the behaviors that the cat releases, ranging from prominent limb jerks to locomotion and attack behaviors (Hendricks et al. 1982). Asymmetrical or unilateral electrolytic lesions in the subcoerulus region or caudally projecting fibers resulted in minimal release of proximal limb movements and rocking head and neck movements. Orienting and searching movements of the eyes and head were associated with damage of pontine afferents to the superior colliculus, a midbrain visual center controlling eye movements during wakefulness that plays a critical role in the ability to direct behaviors toward specific moving objects and generating spatially directed head turns and arm-reaching movements. Cats with larger lesions extending rostrally and ventrally in the pons showed more elaborate behaviors including raising the head, searching and walking. Some of the cats that showed violent attacking behaviors had damage to the pathway arising from the central nucleus of the amygdala (Hendricks et al. 1982). In a different study with rats, small unilateral lesions in the subcoeruleus region were sufficient to remove the atonia of REM sleep but larger and bilateral lesions were needed to release abnormal behaviors (Sandford et al. 2001). In another study in cats, REM sleep atonia was intact after selective electrolytic or radio frequency lesions of the cholinergic PPT and LDT and of the noradrenergic LC. In contrast, lesions confined to the subcoeruleus nucleus eliminated atonia during REM sleep. These findings indicate that selective cholinergic and noradrenergic damage does not play a major role in the pathogenesis of RBD (Shouse and Siegel 1992). In rodents, selective damage of the glutamatergic neurons of the vSLD produces REM sleep with increased muscular activity associated with prominent jerks, walking and running (Lu et al. 2006).
Pharmacological studies within the SLD also provided animal models of RBD. Application of kynurenic acid (a glutamate antagonist) in the SLD produces REM sleep without atonia in rodents (Boissard et al. 2002). In rats, ibotenic acid (a GABAA agonist of the glutamate NMDA receptor) lesions in the vSLD cause loss of REM sleep atonia associated with jerks and complex movements such as walking (Lu et al. 2006).
Genetic manipulation within the SLD has also provided elegant and selective models of RBD using transgenic animals. In contrast to cytotoxic lesions and pharmacological experiments, genetic studies allow to inactivate a specific population of neurons (e.g., glutamatergic, GABAergic). In rats, genetic inactivation of the glutamatergic transmission in the SLD (infusing adeno-associated viral vectors that impair the vesicular glutamate transporter) resulted in excessive EMG activity in the nuchal muscles during REM sleep linked to jerks in the head, fore and hind limbs, nose and tail. Occasionally the rats displayed goal oriented behaviors (e.g., seeking for food, trying to run) during REM sleep. The eyes were closed while the rats moved during REM sleep (Valencia Garcia et al. 2017). In one study using transgenic mice (vGlut2 flox/flox), genetic elimination of glutamate neurotransmission from the SLD neurons produced a RBD-like phenotype where animals showed increased EMG activity during REM sleep linked to simple movements (e.g., body twitches and jerking) and occasionally locomotion (Krenzer et al. 2011). A genetic approach using optogenetics in rodents showed that switching off glutamate subcoeruleus cells can prevent REM sleep EMG paralysis (McKenna and Peever 2017). In rodents, increased EMG activity in REM sleep can be obtained after knockout of the vesicular glutamate transporter 2 gene in the SLD and in the VMM (Lu et al. 2006). This study suggests that decreased glutamate release from both SLD and VMM to the spinal cord is also a model of RBD and that not only the SLD but also the VMM are highly implicated in the pathophysiology of RBD.
Animal models involving the ventral media medulla reticular formation
The VMM is a complex anatomical region that contains several nuclei including the RMg, GiA, GiV, DLPGi and LPGi. GABA and glycine coexist in these VMM neurons and some cells also contain glutamate. Neurons from the DLPGi and LPGi help to promote REM sleep generation inhibiting (by GABA transmission) the vlPAG/LPT, LC and red nucleus (Weber et al. 2015). The RMg, GiV and GiA are involved in the REM sleep muscle paralysis pathway. These neurons induce REM sleep paralysis by three mechanisms (1) sending inhibitory GABA/Glycinergic inputs to the motoneurons of the spinal cord, (2) sending excitatory glutamatergic projections to the interneurons in the spinal cord, which in turn inhibit the motoneurons and (3) reducing the activity of the red nucleus (and therefore reducing the amount of phasic EMG activity and twitches). The VMM contains different types of glutamate receptors (AMPA and NMDA) that have different roles. Injection in the VMM of an AMPA receptor agonist produces normal REM sleep with paralysis, whereas injection of a NMDA receptor agonist produces REM sleep with increased EMG activity. Accumulative data indicated that selective experimental dysfunction in the VMM results in an animal model of RBD characterized by REM sleep with excessive phasic EMG activity associated with abnormal behaviors.
In cats, cytotoxic glutamate-induced lesions of the VMM that included the nucleus magnocellularis, the caudal nucleus gigantocellularis and the rostral nucleus paramedianus (which are analogous of RMg, GiV and GiA in rodents) resulted in REM sleep without atonia associated with a variety of behaviors such as lifting the head, slow lateral movements of the head to both sides, chewing-like movements, pawing at the air, extension and altered movements of all limbs but not locomotion. In this experiment, REM sleep without atonia and abnormal movements in REM sleep were not observed after acetylcholine-induced lesions in the VMM (Schenckel and Siegel 1989). Cytotoxic lesions in the GiV and GiA do not decrease the amount of REM sleep (Holmes and Jones 1994). Restricted glutamatergic lesions in the GiV of rodents produce increased tonic and phasic muscular activity linked to whole body movements during REM sleep (Vetrivelan et al. 2009). In rats, selective loss of glutamate release from the GiV but not GABA/glycine release from the GiV, produces increased phasic EMG activity and movements in REM sleep that are similar to those observed after restricted glutamatergic GiV lesions. This supported the observations that glutamatergic neurons in the GiV also excite GABA/Glycinergic interneurons in the spinal cord, which in turn inhibit the motoneurons (Vetrivelan et al. 2009).
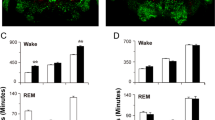
Genetic experiments in the VMM have also produced an animal model of RBD in rodents. A study showed that transgenic mice with deficient glycine receptor α1 and GABAA receptor resulted in a model of RBD characterized by increased phasic EMG activity in REM sleep (linked to chewing, grooming, jerking and running), normal absence of tonic EMG activity in REM sleep, jerking in no-REM sleep, sleep fragmentation, subtle EEG slowing in the spectral analysis and normal REM sleep percentage. The increased phasic EMG activity was recorded in the masseter, neck and limbs. Interestingly, clonazepam and melatonin, the two drugs of choice in human RBD, decreased the phasic EMG activity and the abnormal behaviors seen in REM sleep. This study provided a genetic model of RBD and indicated that GABAergic and glycinergic impairment underlies RBD (Brooks and Peever 2011). In another study, selective genetic inactivation of the GABA/glycinergic transmission in the VVM (infusing adeno-associated viral vectors that impair the vesicular GABA/glycine transporter) resulted in excessive EMG activity in the nuchal muscles during REM sleep linked to jerks in the hind limbs, whiskers and tail. Occasionally, the rats displayed goal-oriented behaviors (e.g., seeking for food, trying to run) during REM sleep. The eyes were closed while the rats moved during REM sleep (Valencia Garcia et al. 2018). Another genetic RBD model in rats occurs when the impairment affects the more rostral area of the GiV and GiA (at the level at the inferior olive/supraolivary medulla that contains GABA/glycinergic cells) and not when the lesion only damages the caudal part of these nuclei (which mainly contain glutamate cells) (Chen et al. 2017). The rodents of this experiment had preserved EMG atonia and increased phasic EMG activity associated with prominent jerking and twitches but not complex behaviors.
Animal models involving the ventral mesopontine junction
In one study, neurotoxic lesions in the caudal VMPJ of cats produced increased tonic and phasic EMG activity in the neck and limbs and RBD-like behaviors such as jerking, kicking, raising and moving the head and lifting of the body. These behaviors were not significantly correlated with the number of dopaminergic loss at the VMPJ. The authors speculated that impairment of the glutamatergic projections from the VMPJ to the SLD and to the VMM could explain the occurrence of an animal model of RBD caused by damage of the VMPJ (Lai et al. 2008).
Animal models involving the limbic system
The limbic system is a set of brain structures including the amygdala, hippocampus, cingulate gyrus, mammillary bodies and nucleus accumbens that modulate a variety of functions including emotions, behaviors, reward, long-term memory and autonomic function. In particular, the amygdala regulates intense emotions (pleasure and fear) during wakefulness (Davis 2000). In RBD, the characteristic emotional component of the dream-enacting behaviors and vocalizations (e.g., punching, screaming, groaning) and the common occurrence of nightmares (e.g., being attacked, arguing) have led to the hypothesis that the limbic system and particularly the amygdala, is involved in the pathogenesis of this parasomnia. In fact, the central nucleus of the amygdala promotes REM sleep sending direct excitatory glutamatergic projections to the subcoeruleus nucleus. In one study, cats with unilateral damage to the central nucleus of the amygdala (preceded by bilateral pontine lesions) exhibited attack behaviors associated with increased EMG activity during REM sleep (Zagrodzka et al. 1998). In another study with cats, pontine lesions damaging the pathway arising from the central nucleus of the amygdala resulted in violent attacking behaviors during REM sleep (Hendricks et al. 1982). These observations are in line with the observation that RBD occurs in humans affected by a limbic encephalitis associated with LGI1 antibodies. This disorder apparently spares the brainstem and impairs the amygdala and the hippocampus damage resulting in RBD, memory problems, confusion and seizures (Iranzo et al. 2006). In this condition, the origin of RBD may be explained by primary damage to the limbic system leading to functional dysregulation of the key brainstem structures that regulate REM sleep muscle paralysis.
Animal models involving the spinal cord
The spinal cord may be another site implicated in the pathogenesis of RBD. Local application of strychnine (glycine receptor antagonist) decreases motoneuron hyperpolarization, indicating that motoneurons are inhibited by glycine during REM sleep (Chase et al. 1989). Pharmacological studies in the trigeminal nucleus (which can be considered functionally as analogous to the spinal cord) show that simultaneously antagonizing the receptors GABAB with phaclophen, GABAA with bicuculline and glycine with strychnine prevents REM sleep muscle atonia in the masseter musculature (Brooks and Peever 2012). In one study, genetic disruption of GABA/glycinergic neurotransmission in the interneurons of the anterior horn of the cervical spinal resulted in twitching and jerky movements in the upper extremities (and occasionally in the lower extremities and tail) during REM sleep (Krenzer et al. 2011).
REM sleep behavior disorder in humans
The first formal description of RBD in humans was made in 1986 by Schenck et al. who described four men and one woman aged 60 to 72 years presenting to a sleep clinic with a chronic history of nightmares associated with yelling, gesturing, punching and leaping out of bed during sleep. Nocturnal polysomnography with synchronized video recording demonstrated that these behaviors occurred during REM sleep where EMG activity was abnormally increased (Schenck et al. 1986). The following year, the same authors reported an expanded series of ten patients with the same clinical and video-polysomnographic findings and gave its name as a new category of sleep disorder (Schenck et al. 1987). In humans, the diagnosis of RBD requires polysomnographic confirmation of excessive amounts of EMG activity in REM sleep. RBD may be idiopathic (IRBD) or secondary to a neurological condition or the introduction of a medication. IRBD is diagnosed when a patient with video-polysomnographic confirmation of RBD has no evidence of a neurological disease or other possible causes. In patients with IRBD, however, neuroimaging studies show evidence of neuronal dysfunction in the mesopontine structures known to regulate REM sleep atonia including the subcoeruleus nucleus, PPT, LC, and PAG (Ehrmingeret al. 2016; Scherfler et al. 2011). The postmortem study of a patient who died with the diagnosis of RBD plus mild cognitive impairment showed neurodegeneration (neuronal loss plus Lewy body pathology) in the subcoeruleus nucleus, GiV, LC, DNR, PPT, PAG and amygdala (Iranzo et al. 2014). The same postmortem pathological pattern is found in patients with IRBD that were eventually diagnosed in life with PD and DLB (Iranzo et al. 2013). Indeed, RBD is a common clinical feature in the setting of living patients already diagnosed with PD, DLB and MSA (Iranzo et al. 2016), probably because these conditions are commonly associated with neurodegeneration of the core structures that regulate REM sleep muscular paralysis. In contrast, RBD is rare in neurodegenerative disease without marked brainstem cell loss such as Alzheimer’s disease.
Longitudinal follow-up of IRBD patients shows the frequent development of the classical motor and cognitive symptoms of the synucleinopathies PD, DLB and MSA (Iranzo et al. 2013; Postuma et al. 2015; Schenck et al. 1996). Patients with IRBD have no cognitive or motor complaints but show many abnormalities (e.g., loss of smell, constipation, depression, subtle electroencephalographic slowing, asymptomatic cognitive dysfunction disclosed by neuropsychological tests and functional neuroimaging demonstration of decreased content of dopamine in the nigrostriatal pathway, microglial activation in the substantia nigra and cortical hypoperfusion) that reflect a widespread process in the brain. These abnormalities are neither the cause nor the consequence of RBD. They are epiphenomena that reflect damage of brain areas that are not associated with the regulation of REM sleep like the olfactory system and the nigrostriatal system. These clinical and neuroimaging abnormalities are typically seen in living subjects already diagnosed with PD, DLB and MSA. Patients with IRBD show aggregates of synuclein (the main component of the Lewy bodies that are the pathological hallmark of PD, DLB and MSA) in organs innervated by the peripheral autonomic system such as the colon, all salivary glands and skin (Antelmi et al. 2017; Doppler et al. 2017; Sprenger et al. 2015; Vilas et al. 2016).
RBD also occurs in patients with narcolepsy, an autoimmune disorder characterized by intrusion of REM sleep into wakefulness leading to hypersomnia and cataplexy (Schenck and Mahowald 1992). Narcolepsy is caused by selective loss of hypocretin/orexin-producing neurons in the dorsolateral hypothalamus. The occurrence of RBD in narcolepsy may be explained by hypocretin/orexin deficiency since hypocretinergic/orexinergic neurons have wide projections to several nuclei that regulate REM sleep atonia (e.g., subcoeruleus nucleus) and the emotional content of dreams (e.g., central nucleus of the amygdala).
RBD has been described in subjects with anti-IgLON5 disease, a neurological condition associated with autoantibodies against the neuronal protein IgLON5. The neuropathological pattern of this disease is characterized by cell loss and tau deposits in the brainstem and hypothalamus impairing, among other regions, some nuclei that regulate sleep (Gelpi et al. 2016; Sabater et al. 2014). RBD can be detected in most of the patients with anti-IgLON5 disease and consists in increased EMG activity in the mentalis and in the four limbs during REM sleep linked to body and limb jerks. Aggressive behaviors such as punching and shouting are rare in RBD linked to anti-IgLON5 disease. In this condition, damage of the magnocellular nucleus in the medulla may explain the occurrence of RBD in view of the preservation of the subcoeruleus nucleus, as disclosed by neuropathology studies.
RBD has been reported in patients with focal structural lesions in the brain mainly confined to the mesopontine tegmentum and much less frequently to the medulla or the limbic system (for review, see Iranzo and Aparicio 2009). The nature of lesions can be infarctions, hemorrhages from vascular malformations, tumors, inflammatory processes and demyelinating plaques. These RBD patients had nightmares suggesting the occurrence of functional dysregulation of those supratentorial structures that modulate intense emotions and that are anatomically connected with the mesopontine tegmentum such as the limbic system.
Some medications have been described to unmask latent RBD, mainly antidepressants. They include sertraline, fluoxetine, venlafaxine, clomipramine, paroxetine, escitalopram, citalopram and mirtazapine (for review, see Aurora et al. 2010; Gagnon et al. 2006). Antidepressants increase serotonin and noradrenergic activity and decrease cholinergic activity. Bisoprolol, a lipophilic beta blocker, may also induce RBD. Melatonin and clonazepam both activate GABAA receptors (Kunz and Bes 1999; Schenck and Mahowald 2002; Wu et al. 1999) and improve RBD symptomatology. They are the treatment of choice in human RBD to minimize the risk of injuries. The effect of clonazepam and melatonin on EMG activity during REM sleep has not been well studied to date.
Open questions in RBD pathophysiology
Are the experimental animal models of RBD equivalent to human RBD?
Overall, animal experiments have provided a large amount of knowledge on the normal REM sleep control and on the pathophysiology of RBD. However, one should question if these animal models of increased EMG activity in REM sleep are the exact paradigm of the pathophysiology of human RBD. The human brain is not exactly the same as the brain of animals. Size, localization and role of some nuclei vary across species. Animal studies on RBD have been performed mainly in cats and rodents that also have different anatomy. Vocalizations are another issue that may distinguish RBD patients from experimental animals with RBD.
Published articles on animal models of RBD have some limitations. Most studies did not distinguish tonic from phasic EMG activity and only used the term “REM sleep without atonia” to reflect excessive muscular activity. In some studies, video-analysis was not used and subsequently we had no information if the excessive EMG activity was sufficient to cause movements or not and what type of movements were displayed.
In humans with RBD, the mentalis, the flexor digitorum superficialis in the upper limbs and the extensor digitorum brevis in the lower limbs are the muscles where the increased phasic EMG activity is more prominent (Frauscher et al. 2008). Simultaneous EMG recording of these three muscles detects 95% of the motor and vocal manifestations occurring in patients with RBD (Iranzo et al. 2011). Thus, to better characterize the EMG pattern in subjects with RBD is necessary to evaluate the mentalis muscle plus the four limbs. However, in most of the studies reported on animal models of RBD, the EMG activity was only evaluated in the nuchal muscle (the analogous of the mentalis muscle in humans) and not in the extremities, where the manifestations of human RBD are characteristic and very prominent. Only few works in animals have evaluated the EMG activity in the limbs (Brooks and Peever 2011; Hsieh et al. 2013).
Available animal models of RBD explained elegantly some of the anatomic and biochemical mechanisms involved in this sleep disorder. However, these experiments did not assess how the neural substrate of a widespread neurodegenerative disease such as PD (where alpha-synuclein is the specific pathological hallmark) may evolve from a single brainstem disorder such as RBD. One study showed that inoculation of pathological alpha-synuclein into the substantia nigra or striatum of mice and monkeys resulted in progressive nigrostriatal neurodegeneration starting at striatal dopaminergic terminals. Exogenous human alpha-synuclein was internalized within host nigral neurons and extended to brain regions distant to the injection site (Recasens et al. 2014). It remains to be determined if injection of pathological alpha-synuclein into the key structures of REM sleep muscle paralysis (e.g., subcoeruleus nucleus, VMM) results in clinical RBD and spreads rostrally into the substantia nigra producing parkinsonism. This would be an animal model of PD starting from RBD. However, there is preliminary evidence that the injection of a recombinant adeno-associated virus expressing human alpha-synuclein into the REM sleep circuit in mice causes pathological aggregation of Lewy-like pathology in REM sleep-generating cells. These pathogenic changes led to elevated levels of phasic motor activity during REM sleep and abnormal behaviors providing a new model of RBD based on alpha-synuclein deposition (McKenna and Peever 2017). Such finding indicates that alpha-synuclein pathology in REM sleep circuitry can lead to a RBD-like motor phenotype.
What is the origin and clinical significance of increased tonic and phasic EMG activity in REM sleep?
In patients with RBD, EMG evaluation during REM sleep shows increased tonic EMG activity and/or excessive phasic EMG activity. In RBD, tonic EMG activity may be sustained or intermittent and is usually seen in the mentalis muscle or in other cranially innervated muscles (e.g., sternocleidomastoid). From a clinical point of view, tonic EMG activity results in incremented postural tone while increased phasic EMG activity is associated with movements (e.g., jerks, punching, kicking, gesturing, jumping out of bed). The excessive phasic EMG activity is observed in the mentalis and in the limbs. The mentalis of patients with RBD may contain only tonic EMG activity, only phasic EMG activity, or combined tonic and phasic EMG activity. The limbs usually exhibit only phasic EMG activity (Frauscher et al. 2008). Some RBD patients have both increased tonic and phasic EMG activity in the mentalis and limb muscles. Another group of RBD patients exhibits only increased phasic EMG activity in the limbs and normal atonia in the mentalis. In few RBD cases, the increased phasic EMG activity may only involve the upper or only the lower limbs. Another group of RBD patients has only increased EMG tonic activity in the mentalis and not excessive phasic EMG activity in the limbs (this is possibly a subclinical form of RBD that may later evolve to clinical RBD if phasic EMG activity appears with time) (Figs. 4, 5, 6, and 7). These different presentations of muscle activity in RBD may underlie different degrees and extent of dysfunction in the brainstem structures that modulate REM sleep tonic and phasic EMG activity.
Polysomnography of normal REM sleep in a healthy human. This figure represents 30 s of a normal human during REM sleep undergoing polysomnography. The recording shows physiological muscle atonia in the mentalis and isolated bursts of phasic electromyographic activity only in the limbs (red arrows). Abd, abdominal movements; EKG, electrocardiogram; EOG, electrooculogram; F3,F4,C3,C4,O1 and O2, electroencephalographic electrode positions (frontal, central and occipital of each side) according to the 10/20 International system referenced to combined ears; LFDS, left flexor digitorum superficialis muscle in the upper limb; LTA, left tibialis anterior muscle in the lower limb; MEN, mentalis muscle; Nasal, nasal airflow; Oral, oral airflow; RFDS, right flexor digitorum superficialis muscle in the upper limb; RTA, right tibialis anterior muscle in the lower limb; Thor, thoracic movements
Polysomnographic representation in REM sleep of increased tonic and phasic EMG activity in the mentalis in a patient with idiopathic REM sleep behavior disorder. This figure represents 30 s showing increased sustained (tonic) and phasic EMG activity in the mentalis (blue arrows) and minimal phasic EMG activity in the limbs (red arrows) where the patient did not move during this epoch. Abd, abdominal movements; EKG, electrocardiogram; EOG, electrooculogram; F3,F4,C3,C4,O1 and O2, electroencephalographic electrode positions (frontal, central and occipital of each side) according to the 10/20 International system referenced to combined ears; LFDS, left flexor digitorum superficialis muscle in the upper limb; LTA, left tibialis anterior muscle in the lower limb; MEN, mentalis muscle; Nasal, nasal airflow; Oral, oral airflow; RFDS, right flexor digitorum superficialis muscle in the upper limb; RTA, right tibialis anterior muscle in the lower limb; Thor, thoracic movements
Polysomnographic representation in REM sleep of increased phasic EMG activity in the limbs and normal muscular atonia in the mentalis in a patient with idiopathic REM sleep behavior disorder. This figure represents 30 s showing normal muscle atonia in the mentalis (blue arrow) but excessive phasic electromyographic activity in the upper and lower limb muscles (red arrows) that was clinically associated with prominent jerks in the limbs. Abd, abdominal movements; EKG, electrocardiogram; EOG, electrooculogram; F3,F4,C3,C4, O1 and O2, electroencephalographic electrode positions (frontal, central and occipital of each side) according to the 10/20 International system referenced to combined ears; LFDS, left flexor digitorum superficialis muscle in the upper limb; LTA, left tibialis anterior muscle in the lower limb; MEN, mentalis muscle; Nasal, nasal airflow; Oral, oral airflow; RFDS, right flexor digitorum superficialis muscle in the upper limb; RTA, right tibialis anterior muscle in the lower limb; Thor, thoracic movements
Polysomnographic representation in REM sleep of increased tonic EMG activity in the mentalis and phasic EMG activity in the limbs in a patient with idiopathic REM sleep behavior disorder. This figure represents 30 s showing increased sustained (tonic) EMG activity in the mentalis (blue arrows) and prominent phasic EMG activity in the limbs (red arrows) where the patient displayed prominent jerks in the limbs. Abd, abdominal movements; EKG, electrocardiogram; EOG, electrooculogram; F3,F4,C3,C4, O1 and O2 electroencephalographic electrode positions (frontal, central and occipital of each side) according to the 10/20 International system referenced to combined ears; LFDS, left flexor digitorum superficialis muscle in the upper limb; LTA, left tibialis anterior muscle in the lower limb; MEN, mentalis muscle; Nasal, nasal airflow; Oral, oral airflow; RFDS, right flexor digitorum superficialis muscle in the upper limb; RTA, right tibialis anterior muscle in the lower limb; Thor, thoracic movements
In normal REM sleep, neural inhibition of the generators of tonic and phasic muscular components are believed to be different. It is thought that the direct pathway that reaches the ventral horn from the vSLD is responsible for inhibiting the tonic muscular activity, whereas the indirect pathway (that involves both vSLD and VMM components) is responsible for disfacilitating the phasic muscular activity resulting in minimal twitches in the face and extremities (Fraigne et al. 2015; Lu et al. 2006; Luppi et al. 2013; Peever et al. 2014; Ramaligam et al. 2013; Stefani et al. 2015; Vetrivelan et al. 2009).
Sustained EMG atonia is thought to be mediated by the SLD. The REM sleep atonia circuit arises from the glutamatergic vSLD that activates the spinal cord interneurons in the spinal cord, which in turn inhibits the anterior horn motoneurons through GABA/glycinergic transmission (Fig. 2). This direct pathway bypasses the VMM. Selective lesions confined to the SLD in rats produce loss of atonia in the neck and have no effect on phasic EMG activity of the jaw (Anaclet et al. 2010).
Phasic EMG activity is mediated by an additional circuit where the VMM and the red nucleus play an important role. During normal REM sleep, the glutamatergic neurons of the red nucleus activate the motoneurons of the spinal cord resulting in phasic EMG activity, twitches and small movements (Li and Peever 2015). This activity is not prominent in normal REM sleep because the VMM inhibits both the red nucleus and the spinal cord motoneurons (Tiriac et al. 2012, 2014). This circuit is probably more complex since cholinergic transmission from the LDT and PPT also produces phasic EMG activity. Thus, it is possible that motor behaviors in RBD could be caused by an abnormal overactivation of the red nucleus and these other nuclei. Pharmacological blockade of GABA and glycine inhibitory drives to the spinal cord motoneurons increases phasic EMG activity in REM sleep (Brooks and Peever 2008, 2012). Experimental damage of the VMM produces increased phasic EMG activity in REM sleep.
What is the origin of motor behaviors in RBD?
Experimental animals and patients with RBD display two types of motor behaviors during REM sleep (Manni et al. 2009):
-
1.
Simple motor behaviors. They are primitive jerky movements of the head, face, ears, whiskers, limbs, tail, or even the whole body. They are exaggerated expressions of those small movements and jerks seen in normal people and animals (e.g., dogs, cats) during normal REM sleep linked to bursts of phasic EMG activity.
-
2.
Complex motor behaviors. These are more elaborated movements that represent goal directed movements that can be violent (punching, kicking, biting, pulling hair) or non-violent (mimicking eating, drinking, kissing, dancing, smoking, clapping, spitting, pointing, searching for something). They resemble very much the movements that are displayed during wakefulness in normal people, with the exception that RBD patients have their eyes closed (Oudiette et al. 2009).
In human IRBD, simple motor behaviors (69%) are more frequent than complex motor behaviors (31%) (Frauscher et al. 2008; Manni et al. 2009). Both types of movements are usually displayed by the same person. Simple motor behaviors may occur while the patient mutters, groans, moans, or shouts. Complex behaviors can be associated with shouts, swearing, singing, or giving long instructions or speeches.
There is a strong debate on the origin of movements in RBD. Two different hypotheses have been proposed on the origin of the simple and complex behaviors seen in RBD (Figs. 8 and 9). The “cortical hypothesis” states that the motor cortex is primarily responsible for both simple and complex movements (Luppi et al. 2013; Peever et al. 2014). During normal REM sleep, the subcoeruleus nucleus and VMM inhibit the motor neurons of the spinal cord that prevent pyramidal neurons in the motor cortex from producing movement. In this model, all RBD behaviors result from activation of the neocortex that reaches directly the spinal cord because the inhibitory influences from the brainstem are lost in REM sleep. Accordingly, patients with RBD are “acting out the dreams” with movements that are generated in the cortex. This is supported by the fact that the pyramidal neurons from the cortex are active during REM sleep and that the electroencephalographic pattern of the cortex during normal REM sleep is similar to that observed during the performance of a voluntary movement during wakefulness (De Carli et al. 2016; Evarts 1964). This hypothesis does not explain why the nature of the dreams is usually violent and consequently the released behaviors are aggressive. It is likely that the cortical limbic system is implicated generating unpleasant dreams and exciting the motor cortex glutamatergic pyramidal neurons, which in turn excite the motoneurons of the spinal cord.
Origin of the motor behaviors in RBD according to the “cortical hypothesis.” a During normal REM, the sleep muscular paralysis is produced because the ventral medial medulla (VMM) inhibits the motor neurons of the spinal cord (thick red arrows) and the pyramidal tract from the motor cortex is then prevented to produce movements (dashed blue arrow) because of intense hyperpolarization of the spinal cord. b In RBD, there is direct or indirect damage of the VMM that does not inhibit the motor neurons of the spinal cord. This allows the pyramidal tract from the cortex (thick blue arrow) to reach the spinal cord and produce movements according to what the individual is dreaming
Origin of the motor behaviors in RBD according to the “brainstem hypothesis.” The red nucleus (RN) in the brainstem stimulates the motoneurons of the spinal cord producing twitches and movements. a In normal REM sleep, the RN is inhibited by the ventral medial medulla (VMM) (thick red arrow) that also inhibits the motor neurons of the spinal cord with direct projections (thick red arrow). This results in muscular paralysis and occasional twitches because the blockade of the RN is not complete from the VMM. b In RBD, there is direct or indirect damage of the VMM. Accordingly, the VMM cannot inhibit the RN. Thus, the RN is free to generate excessive twitching resulting in simple and complex behaviors. These behaviors produce an increase sensory feedback to the cortex (thick blue arrow) that then generates a dream according to how the subject is moving
Alternatively, the challenging “brainstem hypothesis” proposes that the red nucleus and other brainstem nuclei (e.g., superior colliculus) play a major role in exciting spinal motoneurons during REM sleep independently from the cortex. In normal REM sleep, the red nucleus activates the motoneurons in the spinal cord resulting in twitching but this motor activity is not prominent because the VMM inhibits the red nucleus during REM sleep. If in RBD the VMM is impaired then the red nucleus is free to produce massive twitches and complex movements originated in the brainstem. These behaviors produce an increased sensory feedback to the sensorimotor cortex that generates a dream (an unpleasant dream, in fact). Therefore, this model proposes that external stimuli (“massive twitching and movements”) are incorporated into dreams and that subsequently patients with RBD are “dreaming about their actions” (Blumberg and Plumeau 2016). The assumption that in RBD the motor cortex is not necessary to produce complex behaviors is supported by the fact that stimulation in animals of some brainstem structures (e.g., PAG, superior colliculus) can result in escape responses and violent behaviors similar to those seen in patients with RBD (Dean et al. 1989). Interestingly, none of these two hypotheses involved the limbic system. In RBD, the limbic system is probably impaired because the content of the dreams is usually unpleasant and typically the released behaviors are violent (e.g., kicking, punching).
It seems possible that the complex, elaborated and purposeful motor behaviors indicate the participation of motor neocortical areas. There are no reports of RBD linked to cortical lesions (e.g., stroke, tumors) or neurodegenerative diseases selectively damaging the cortex (e.g., pure Alzheimer disease without Lewy body pathology). Bilateral lesions of the parieto-occipital cortex can prevent dreaming but REM sleep is still characterized by muscle atonia (Bischof and Bassetti 2004). Thus, it can be speculated that complex behaviors in RBD are mediated by abnormal activation of sensorial and motor cortical areas rather than their damage. This is in line with reports on ictal functional neuroimaging that showed activation of the supplementary motor area during a RBD episode in subjects with RBD (Dauvilliers et al. 2011; Mayer et al. 2015). The supplementary area is implicated in the planning of motor actions. In normal conditions, the supplementary motor area is anatomically connected with the SLD (Boissard et al. 2002) and promotes REM sleep. Therefore, it is possible that in RBD the activation of the supplementary motor area reaches directly the spinal cord, bypassing a damaged brainstem, resulting in elaborated dream-enacting behaviors. This speculation is in agreement with the observations that during RBD episodes PD and MSA patients show purposeful movements that are faster, stronger and smoother than during wakefulness (De Cock et al. 2007; De Cock et al. 2011). The authors of these studies in PD and MSA proposed the following hypothesis to explain the restoration of normal motor control seen in patients during RBD: the complex movements are generated by the motor areas and follow the pyramidal tract bypassing the basal ganglia that is damaged by the disease. The inputs from the cortex are transmitted directly to lower motor neurons resulting in dream-enacting behaviors since the brainstem structures that produce REM sleep atonia are impaired by the disease. Thus, in this model, the motoneurons of the spinal cord during REM sleep are not submitted to the influence of the brainstem structures that regulate REM sleep and to the basal ganglia, resulting in dream-enacting behaviors without parkinsonian features.
What is the origin of vocalizations in RBD?
Vocalizations are not obvious in experimental RBD rats (Valencia Garcia et al. 2017). In patients with RBD, vocalizations are common although they are much less frequent than motor behaviors (Iranzo et al. 2011). There are two types of vocalizations displayed by RBD patients.
-
1.
Simple vocalizations. These elementary and primitive vocalizations include groaning, muttering, catcall, moaning, shouts, swearing, crying and laughing. They are primitive, brief and usually include an emotional component.
-
2.
Complex vocalizations. They are much less common than simple vocalizations. They include singing, whistling, arguing, complaining and giving short or long speeches. They can be intelligible or have normal prosody. They are linked to a negative emotional component (arguing) and less frequently to a pleasant component (singing). Few patients may use foreign languages or combine two different mother-tongue languages like Spanish and Catalán.
An elementary model of normal vocal control during wakefulness, based mainly on research in the squirrel monkey, consists of two different pathways (Jürgens 2002, 2009).
-
1.
In the first pathway, the anterior cingulate gyrus and the supplementary motor area project to the PAG in the midbrain and the PAG projects to an extensive area in the reticular formation of the pons and medulla that includes the retroambiguus nucleus and the gigantocellularis nucleus. Finally, these lower brainstem nuclei project bilaterally to the phonatory motoneurons of the nucleus ambiguus and hypoglossal nucleus. The anterior cingulate cortex, supplementary motor area and PAG are responsible for voluntary initiation of vocal behavior. In this same pathway, the pontine and medullar nuclei of the reticular formation modulate innate vocal reactions such as non-verbal emotional vocal utterances (crying, laughing, screaming). Electrical stimulation of the anterior cingulate gyrus, PAG and reticular formation in the lower brainstem induces vocalizations such as screaming and laughing. PAG stimulation with glutamate, with acetylcholine and with GABA antagonists also results in vocalizations. Lesions in the anterior cyngulate gyrus, supplementary motor area and PAG cause mutism.
-
2.
The second pathway runs from the primary motor cortex via the reticular formation in the pons and medulla to the phonatory motoneurons. This pathway is modulated by basal ganglia and cerebellar inputs. It is responsible for the production of a learned vocal pattern. Lesions of the primary motor cortex produce mutism and lack of singing but patients are still able to moan, cry and laugh.
This anatomic model of vocalizations should be inactive during sleep, particularly during REM sleep. It is tempting to speculate that in RBD simple vocalizations arise from abnormal activation of the first pathway at the level of the brainstem nuclei including the PAG, whereas complex vocalizations may result from abnormal activation of the primary motor cortex and cortical language areas.
The speech of patients with PD and MSA is more intelligible, louder and better articulated during RBD episodes than during wakefulness (De Cock et al. 2007; De Cock et al. 2011). This may be explained by impairment of the basal ganglia and cerebellum by the disease that does not inhibit the activity of motor and cortical language areas to reproduce learned vocal patterns during REM sleep.
Does nigrostriatal dopaminergic deficiency play a central role in RBD?
It can be speculated that dysfunction of the dopaminergic nigrostriatal system plays an important role in the pathogenesis of RBD because this parasomnia frequently occurs in PD, MSA and DLB, three neurodegenerative diseases where substantia nigra neuronal loss and dopaminergic deficit are prominent. In about 50% of patients with IRBD, functional neuroimaging of the nigrostriatal dopaminergic system using FP-CIT-SPECT shows reduced striatal dopamine transporters (Iranzo et al. 2017). This observation represents a comorbid finding and not the primary pathogenic determinant of RBD, as subjects with IRBD frequently develop a neurodegenerative disorder associated with substantia nigra cell loss (e.g., PD, MSA and DLB) (Högl et al. 2018; Iranzo et al. 2016). In PD, parkinsonism only manifests when the substantia nigra pars compacta reaches 50–60% of cell loss. Thus, it is possible that FP-CIT-SPECT in IRBD is detecting subjects close to 50–60% substantia nigra neuronal loss at a high risk for developing parkinsonism, rather than explaining the pathophysiology of RBD (Iranzo et al. 2017). Moreover, dopamine transporter FP-CIT-SPECT is abnormal in idiopathic PD regardless of the presence or absence of RBD.
There are several lines of evidence suggesting that dopaminergic deficiency is not directly responsible for RBD pathogenesis:
-
1.
RBD does not occur in about half of the PD patients (Gagnon et al. 2002).
-
2.
In some PD patients with RBD, the parasomnia onset clearly antedates the onset of parkinsonism (Iranzo et al. 2005).
-
3.
In PD patients with RBD, total levodopa equivalent dose is not associated with measures of RBD severity, such as tonic EMG activity in the mentalis, phasic EMG activity in the mentalis and limbs, self-reported severity of the RBD symptoms and severity of the behaviors detected on video-polysomnography (Iranzo et al. 2005).
-
4.
The use of dopaminergic agents does not improve RBD symptomatology in subjects with PD (Kumru et al. 2008).
-
5.
In PD, surgical techniques (e.g., deep brain subthalamic stimulation) do not ameliorate RBD while provide effective control of the parkinsonian dopaminergic motor symptoms (Iranzo et al. 2002).
-
6.
In RBD cases secondary to structural brainstem lesions (stroke, tumors), the substantia nigra is habitually spared.
-
7.
Although not systematically studied, there are neither published reports of RBD precipitated by antipsychotic drugs blocking dopaminergic receptors nor descriptions of RBD occurring in subjects with drug-induced parkinsonism.
-
8.
Animal studies in monkeys, rats and cats with impairments of substantia nigra dopaminergic and GABAergic cells did not show REM sleep without atonia (Gerashchenko et al. 2006; Lai et al. 2008; Rye and Bliwise 2004). In contrast, one study showed that marmoset monkeys treated with MPTP (the non-human primate model for PD characterized by toxic nigrostriatal dopaminergic deficit) show increased tonic but not phasic, EMG activity in the chin and neck muscles without abnormal motor behaviors (Verhave et al. 2011). It should be noted that the MPTP model not only impairs dopaminergic activity but also noradrenergic and serotonergic cells. Thus, it is possible that noradrenergic and serotonergic deficits (and not dopaminergic impairment) are responsible for increased tonic EMG activity in this animal model of PD.
Does the Braak et al. ascending hypothesis for Parkinson’s disease fit with the time of appearance of RBD?
In a seminal work by Braak et al. (2003), it was reported that in sporadic PD, Lewy pathology (Lewy bodies and Lewy neurites containing alpha-synuclein aggregates) begins in the anterior olfactory nucleus and the dorsal motor nucleus of the vagus nerve in the medulla (stage 1). From the medulla, the neuropathological process advances rostrally until the VMM and the subcoeruleus-coeruleus complex (stage 2), the substantia nigra, the PPT and the amygdala (stage 3), the temporal mesocortex (stage 4) and finally reaches the neocortex (stages 5 and 6). This hypothesis is supported by the demonstration that misfolded alpha-synuclein can be propagated from an already affected neuron to a nearby neuron in a prion-like fashion (for review, see Tamgüney and Korczyn 2017). This staging model of pathology proposes that in PD the neurodegenerative process starts in the peripheral autonomic nervous system, medulla, or olfactory bulb (Braak et al. 2000; Braak and Del Tredici 2017; Del Tredici et al. 2002). Braak et al. postulated that stages 1 and 2 correspond to a premotor state of PD, stages 3 and 4 to the development of parkinsonism and stages 5 and 6 to parkinsonism associated with cognitive impairment. Accordingly, sufficient damage of the structures involved may correlate with a predictable sequence of symptoms where constipation and hyposmia (stage 1, involving the dorsal motor nucleus of the vagus nerve and olfactory system) precede depression and RBD (stage 2, involving DRN, VMM and subcoeruleus nucleus) before the onset of parkinsonism (stage 3, involving the substantia nigra pars compacta). This temporal sequence of Lewy pathology may account for the finding that in some PD patients, RBD (stage 2) antedates the clinical onset of parkinsonism (stage 3) (Iranzo et al. 2013; Postuma et al. 2015; Schenck et al. 1996). Moreover, living IRBD patients show alpha-synuclein in the peripheral autonomic nervous system in organs such as the colon and the submandibular glands (Sprenger et al. 2015; Vilas et al. 2016) before the onset of parkinsonism (Fig. 10). Taken together, the common observation that RBD precedes the onset of parkinsonism in PD fits with the caudo-rostral topographical sequence described by Braak et al.
Alpha-synuclein deposits in the submandibular gland in a patient with idiopathic REM sleep behavior disorder. Immunohistochemical stain for phosphorylated alpha-synuclein (pAS) on Ser129 in a punch biopsy of the submandibular gland in a study subject with idiopathic RBD reveals abnormal pAS aggregates (brown signal) within nerve fibers embedded in connective tissue and around a centrally located vessel (original magnification ×200). Courtesy of Ellen Gelpi
In one study, 44 IRBD patients without parkinsonism were asked to report on the presence and perceived onset of hyposmia, constipation and depression (Aguirre-Mardones et al. 2015). The first symptom perceived was (1) RBD in 17 (38.6%) patients, (2) RBD manifesting at the same time span as other symptoms in nine (22.7%) patients, (3) hyposmia in seven (15.9%), (4) constipation in five (11.4%), (5) depression in three (6.8%) and (6) hyposmia at the same timespan as constipation in one (2.4%) patient. In patients with hyposmia, smell loss preceded RBD onset in 28.6% of the cases, occurred simultaneously in 35.7% and appeared after RBD in 35.7%. In patients with constipation, this symptom antedated RBD onset in 43.5% of them, occurred simultaneously in 8.7% and appeared after RBD in 47.8%. In patients with depression, depressive symptomatology occurred before RBD onset in 24.0%, simultaneously in 36.0% and after RBD in 40.0%. Seven (15.9%) IRBD patients had no hyposmia, depression, or constipation. Eleven (25.0%) perceived hyposmia and constipation but no depression. Four (9.1%) noticed hyposmia, constipation and depression. Patients reported 23 different temporal sequences, with the most frequent being (1) RBD followed by hyposmia, (2) hyposmia followed by RBD and (3) hyposmia followed by both RBD and constipation occurring at the same time span. This study was in agreement with the Braak et al. hypothesis showing that patients with IRBD were commonly affected by hyposmia depression and constipation before the onset of parkinsonism. However, there was a highly variable chronological emergence of RBD, hyposmia, constipation and depression with 23 different temporal presentations. The above observations in subjects with IRBD do not reflect a predictable temporal sequence of symptoms before the onset of parkinsonism. In IRBD, the variable and heterogeneous emergence of clinical features suggests the existence of a wide variety of clinical phenotypes, with different patterns of disease development that does not strictly follow a single time course. The heterogeneity on symptomatology may reflect different degrees of pathological burden (e.g., cell loss) in the nuclei that are responsible for the development of a specific function and symptoms. This is in line with the observations that some PD patients do not develop RBD (Gagnon et al. 2002) and that parkinsonism may precede RBD onset in most PD subjects (Iranzo et al. 2005). One possible explanation is that in these situations the severity of neuronal dysfunction in the brainstem structures generating REM sleep does not reach a critical threshold for the clinical expression of RBD.
References
Aguirre-Mardones C, Iranzo A, Vilas D, Serradell M, Gaig C, Santamaría J, Tolosa E (2015) Prevalence and timeline of nonmotor symptoms in idiopathic rapid eye movement sleep behavior disorder. J Neurol 262:1568–1578
American Academy of Sleep Medicine (2014) International classification of sleep disorders, 3rd edn. American Academy of Sleep Medicine, Darien
Anaclet C, Pedersen NP, Fuller PM, Lu J (2010) Brain circuitry regulating phasic activity in the trigeminal motor nucleus (Mo5) during REM sleep. PLoS One 5:e878
Antelmi E, Donadio V, Incensi A, Plazzi G, Liguori R (2017) Skin nerve phosphorylated α-synuclein deposits in idiopathic REM sleep behavior disorder. Neurology 88:2128–2131
Arrigoni E, Chen MC, Fuller PM (2016) The anatomical, cellular and synaptic basis of motor atonia during rapid eye movement sleep. J Physiol 594:5391–5414
Aserinsky E, Kleitman N (1953) Regularly occurring periods of eye motility and concomitant phenomena during sleep. Science 118:273–274
Aurora RN, Zak RS, Maganti RK, Auerbach SH, Casey KR, Chowdhuri S, Karippot A, Ramar K, Kristo DA, Morgenthaler TI, Standards of Practice Committee; American Academy of Sleep Medicine (2010) Best practice guide for the treatment of REM sleep behavior disorder (RBD). J Clin Sleep Med 6:85–95
Bischof M, Bassetti CL (2004) Total dream loss: a distinct neuropsychological dysfunction after bilateral PCA stroke. Ann Neurol 56:583–586
Blumberg MS, Plumeau AM (2016) A new view of “dream enactment” in REM sleep behavior disorder. Sleep Med Rev 30:34–42
Boeve BF (2013) Idiopathic REM sleep behavior disorder in the development of Parkinson’s disease. Lancet Neurol 12:469–482
Boissard R, Gervasoni D, Scmidt MH, Barbagli B, Fort P, Luppi PH (2002) The rat ponto-medullary network responsible for paradoxical sleep onset and maintenance: a combined microinjection and functional neuroanatomical study. Eur J Neurosci 16:1959–1973
Boissard R, Fort P, Gervasoni D, Barbagli B, Luppi PH (2003) Localization of the GABAergic and non-GABAergic neurons projecting to the sublaterodorsal nucleus and potentially gating of paradoxical sleep. Eur J Neurosci 18:1627–1639
Braak H, Del Tredici K (2017) Neuropathological staging of brain pathology in sporadic Parkinson’s disease: separating the wheat from the chaff. J Parkinsons Dis 7(Suppl 1):S73–S87
Braak H, Rub U, Sandmann-Keil D, Gai WP, de Vos RA, Jansen Steur EN, Arai K, Braak E (2000) Parkinson’s disease: affection of brain stem nuclei controlling premotor and motor neurons of the somatomotor system. Acta Neuropathol 99:489–495
Braak H, Del Tredici K, Rüb U, de Vos RA, Jansen Steur EN, Braak E (2003) Staging of brain pathology related to sporadic Parkinson's disease. Neurobiol Aging 24:197–211
Brooks PL, Peever JH (2008) Glycinercic and GABAA-mediated inhibition of somatic motoneurons does not mediate rapid eye movement sleep motor atonia. J Neurosci 28:3535–3545
Brooks PL, Peever JH (2011) Impaired GABA and glycine transmission triggers cardinal features of rapid eye movement sleep disorder in mice. J Neurosci 31:7111–7121
Brooks PL, Peever JH (2012) Identification of the transmitter and receptor mechanisms responsible for REM sleep paralysis. J Neurosci 32:9785–9795
Chase MH (2008) Confirmation of the consensus that glycinergic postsynaptic inhibition is responsible for the atonia of REM sleep. Sleep 31:1487–1491
Chase MH, Soja PJ, Morales FR (1989) Evidence that glycine mediates the post-synaptic potentials that inhibit lumbar motoneurons during the atonia of active sleep. J Neurosci 9:743–751
Chen MC, Vetrivelan R, Guo CN, Chang C, Fuller PM, Lu J (2017) Ventral medullary control of rapid eye movement sleep and atonia. Exp Neurol 290:53–62
Clement O, Sapin E, Bérod A, Fort P, Luppi PH (2011) Evidence that neurons of the sublaterodorsal tegmental nucleus triggering paradoxical (REM) sleep are glutamatergic. Sleep 34:419–423
Crochet S, Sakai K (2003) Dopaminergic modulation of behavioral states in meso-pontine tegmentum: a reverse microdialysis study in freely moving cats. Sleep 26:801–806
Dang-Vu TT, Schabaus M, Desseilles M, Sterpenich V, Bonjean M, Maquet P (2010) Functional neuroimaging insights into the physiology of human sleep. Sleep 33:1589–1603
Dauvilliers Y, Boudousq V, Lopez R, De Cock VC (2011) Increased perfusion in supplementary area during a REM sleep behaviour episode. Sleep Med 12:531–532
Davis M (2000) The role of the amygdala in conditioned and unconditioned fear and anxiety. In: Aggleton JP (ed) The amygdala. Oxford University Press, New York, pp 213–288
De Carli F, Proserpio P, Morrone E, Sartori I, Ferrara M, Gibbs SA, De Gennaro L, Lo Russo G, Nobili L (2016) Activation of the motor cortex during phasic rapid eye movement sleep. Ann Neurol 79:326–330
De Cock VC, Vidailhet M, Leu S, Texeira A, Apartis E, Elbaz A, Roze E, Willer JC, Derenne JP, Agid Y, Arnulf I (2007) Restoration of motor control in Parkinson’s disease during REM sleep. Brain 130:450–456
De Cock VC, Debs R, Oudiette D, Leu S, Radji F, Tiberge M, Yu H, Bayard S, Roze E, Vidailhet M, Dauvilliers Y, Rascol O, Arnulf I (2011) The improvement of movement and speech during rapid eye movement sleep behaviour disorder in multiple system atrophy. Brain 134:856–862
Dean P, Redgrave P, Westby G (1989) Event or emergency? Two response systems in the mammalian superior colliculus. Trends Neurosci 12:137e47
Del Tredici K, Rub U, de Vos RA, Bohl JR, Braak H (2002) Where does Parkinson disease pathology begin in the brain? J Neuropathol Exp Neurol 61:413–426
Doppler K, Jentschke HM, Schulmeyer L, Vadasz D, Janzen A, Luster M, Höffken H, Mayer G, Brumberg J, Booij J, Musacchio T, Klebe S, Sittig-Wiegand E, Volkmann J, Sommer C, Oertel WH (2017) Dermal phospho-alpha-synuclein deposits confirm REM sleep behaviour disorder as prodromal Parkinson's disease. Acta Neuropathol 133:535–545
Ehrminger M, Latimier A, Pyatigorskaya N, Garcia-Lorenzo D, Leu-Semenescu S, Vidailhet M, Lehericy S, Arnulf I (2016) The coeruleus/subcoeruleus complex in idiopathic rapid eye movement sleep behaviour disorder. Brain 139:1180–1188
Evarts EV (1964) Temporal patterns of discharge of pyramidal tract neurons during sleep and waking in the monkey. J Neurophysiol 27:152–171
Fraigne JJ, Torontali ZA, Snow MB, Peever JH (2015) REM sleep at its core—circuits, neurotransmitters, and pathophysiology. Front Neurol 29:123. https://doi.org/10.3389/fneur.2015.00123
Frauscher B, Iranzo A, Högl B, Casanova-Molla J, Salamero M, Gschliesser V, Tolosa E, Poewe W, Santamaria J, SINBAR (Sleep Innsbruck Barcelona group) (2008) Quantification of electromyographic activity during REM sleep in multiple muscles in REM sleep behaviour disorder. Sleep 31:724–731
Fuller PM, Saper CB, Lu J (2007) The pontine REM switch: past and present. J Physiol 584-3:735–741
Fuller P, Sherman D, Pedersen N, Saper CB, Lu J (2011) Reassessment of the structural basis of the ascending arousal system. J Comp Neurol 519:933–956
Fung SJ, Xi M, Zhang J, Torterolo P, Sampogna S, Morales FR, Chase MH (2011) Projection neurons from the central nucleus of the amygdala to the nucleus pontis oralis. J Neurosci Res 89:429–436
Gagnon JF, Bédard MA, Fantini ML, Petit D, Panisset M, Rompré S, Carrier J, Montplaisir J (2002) REM sleep behavior disorder and REM sleep without atonia in Parkinson’s disease. Neurology 59:585–589
Gagnon JF, Postuma RB, Montplaisir J (2006) Update on the pharmacology of REM sleep behavior disorder. Neurology 67:742–747
Gelpi E, Höftberger R, Graus F et al (2016) Neuropathological criteria of anti-IgLON5-related tauopathy. Acta Neuropathol 132:531–543
Gerashchenko D, Blanco-Centurion CA, Miller JD, Shiromani PJ (2006) Insomnia following hypocretin2-saporin lesions of the substantia nigra. Neuroscience 137:29–36
Hendricks JC, Morrison AR (1981) Normal and abnormal sleep in animals. JAVMA 178:121–126
Hendricks JC, Morrison AR, Mann GL (1982) Different behaviors during paradoxical sleep without atonia depend on pontine lesion site. Brain Res 239:81–105
Högl B, Stefani A, Videnovic A (2018) Idiopathic REM sleep behaviour disorder and neurodegeneration—an update. Nat Rev Neurol 14:40–55
Holmes CJ, Jones BE (1994) Importance of cholinergic, GABAergic, serotonergic and other neurons in the medial medullary reticular formation for sleep-wake states studied by cytotoxic lesions in the cat. Neuroscience 62:1179–1200
Hsieh KC, Nguyen D, Siegel JM, Lai YY (2013) New pathways and data on rapid eye movement sleep behaviour disorder in a rat model. Sleep Med 14:719–728
Iranzo A, Aparicio J (2009) A lesson from anatomy: focal brain lesions causing REM sleep behavior disorder. Sleep Med 10:9–12
Iranzo A, Valldeoriola F, Santamaría J, Rumiá J, Tolosa E (2002) Sleep symptoms and polysomnographic architecture in advanced Parkinson’s disease after chronic bilateral subthalamic stimulation. J Neurol Neurosurg Psychiatry 72:661–664
Iranzo A, Santamaria J, Rye DB, Valldeoriola F, Marti MJ, Muñoz E, Vilaseca I, Tolosa E (2005) Characteristics of idiopathic REM sleep behavior disorder and that associated with MSA and PD. Neurology 65:247–252
Iranzo A, Graus F, Clover L, Morera J, Bruna J, Vilar C, Martínez-Rodriguez JE, Vincent A, Santamaría J (2006) Rapid eye movement sleep behavior disorder and potassium channel antibody-associated limbic encephalitis. Ann Neurol 59:178–182
Iranzo A, Frauscher B, Santos H, Gschliesser V, Ratti L, Falkenstetter T, Stürner C, Salamero M, Tolosa E, Poewe W, Santamaria J, Högl B, SINBAR (Sleep Innsbruck Barcelona) Group (2011) Usefulness of the SINBAR electromyographic montage to detect the motor and vocal manifestations occurring in REM sleep behaviour disorder. Sleep Med 12:284–288
Iranzo A, Tolosa E, Gelpi E, Molinuevo JL, Valldeoriola F, Serradell M, Sanchez-Valle R, Vilaseca I, Lomeña F, Vilas D, Lladó A, Gaig C, Santamaria J (2013) Neurodegenerative status and postmortem pathology in idiopathic rapid-eye-movement behavior disorder: an observational cohort study. Lancet Neurol 12:443–453
Iranzo A, Gelpi E, Tolosa E, Molinuevo JL, Serradell M, Gaig C, Santamaria J (2014) Neuropathology of prodromal Lewy body disease. Mov Disord 29:410–415
Iranzo A, Santamaria J, Tolosa E (2016) Idiopathic rapid eye movement sleep behaviour disorder: diagnosis, management, and the need for neuroprotective interventions. Lancet Neurol 15:405–419
Iranzo A, Santamaría J, Valldeoriola F, Monica S, Salamero M, Carles G, Niñerola-Baizán A, Sánchez-Valle R, Lladó A, De Marzi R, Stefani A, Seppi K, Pavia J, Högl B, Poewe W, Tolosa E, Lomeña F (2017) Dopamine transporter imaging deficit predicts early transition to synucleinopathy in idiopathic rapid eye movement sleep behavior disorder. Ann Neurol 82:419–428
Irwin MR (2015) Why sleep is important for health: a psychoneuroimmunology perspective. Annu Rev Psychol 66:143–172
Jouvet M, Delrome F (1965) Locus coeruleus et sommeil paradoxal. C R Soc Biol 159:895–899
Jürgens U (2002) Neural pathways underlying vocal control. Neurosci Biobehav Reviews 26:235–258
Jürgens U (2009) The neural control of vocalization in mammals: a review. J Voice 23:1–10
Krenzer M, Anaclet C, Vetrivelan R, Wang N, Vong L, Lowell BB, Fulller PM, Lu J (2011) Brainstem and spinal cord circuitry regulating REM sleep and muscle atonia. PLoS One 6(10):e24998
Krenzer M, Lu J, Mayer G, Oertel W (2013) From bench to bed: putative animal models of REM sleep behavior disorder (RBD). J Neural Transm 120:683–688
Kumru H, Iranzo A, Carrasco E, Valldeoriola F, Marti MJ, Santamaria J, Tolosa E (2008) Lack of effects of pramipexole on REM sleep behavior disorder in Parkinson’s disease. Sleep 31:1418–1421
Kunz D, Bes F (1999) Melatonin as a therapy in REM sleep behavior disorder patients: an open-labeled pilot study on the possible influence of melatonin on REM-sleep regulation. Mov Disord 14:507–511
Lai YY, Hsieh KC, Nguyen D, Peever J, Siegel JM (2008) Neurotoxic lesions at the ventral mesopontine junction change sleep time and muscle activity during sleep: an animal model of motor disorders in sleep. Neuroscience 154:431–443
Lapierre O, Montplaisir J (1992) Polysomnographic features of REM sleep behavior disorder: development of a scoring method. Neurology 42:1371–1374
Li D, Peever J (2015) Pharmacogenetic stimulation of the red nucleus influences muscle tone during rapid eye movement (REM) sleep in mice. Sleep 37:A21
Lu J, Sherman D, Devor M, Saper CB (2006) A putative flip-flop switch for control of REM sleep. Nature 441:589–594
Luppi PH, Gervasono D, Verret L et al (2007) Paradoxical (REM) sleep genesis: the switch from an aminergic-cholinergic to a GABAergic-glutamatergic hypothesis. J Phsiol 100:271–283
Luppi PH, Clement O, Sapin E et al (2011) The neuronal network responsible for paradoxical sleep and its dysfunctions causing narcolepsy and rapid eye movement (REM) behavior disorder. Sleep Med Rev 15:153–163
Luppi PH, Clement O, Valencia Garcia S, Brischoux F, Fort P (2013) New aspects in the pathophysiology of rapid eye movement behavior disorder: the potential role of glutamate, gamma-aminobutyric acid, and glycine. Sleep Med 14:714–718
Luppi PH, Billwiller F, Fort P (2017) Selective activation of a few limbic structures during paradoxical (REM) sleep by the claustrum and the suprammamilary nucleus: evidence and function. Curr Opin Neurobiol 44:59–64
Mander BA, Winer JR, Walker MP (2017) Sleep and human aging. Neuron 94:19–36
Manni R, Terzaghi M, Glorioso M (2009) Motor-behavioral episodes in REM sleep behavior disorder and phasic events during sleep. Sleep 32:241–245
Mayer G, Bitterlich M, Kuwert T, Ritt P, Stefan H (2015) Ictal SPECT in patients with rapid eye movement sleep behaviour disorder. Brain 138:1263–1270
McKenna D, Peever J (2017) Degeneration of rapid eye movement sleep circuitry underlies rapid eye movement sleep behavior disorder. Mov Disord 32:636–644
Morrison AR, Mann GL, Hendrijks JC (1981) The relationship of excessive exploratory behavior in wakefulness to paradoxical sleep without atonia. Sleep 4:247–257
Oudiette D, De Cock VC, Lavault S, Leu S, Vidailhet M, Arnulf I (2009) Nonviolent elaborate behaviors may also occur in REM sleep behavior disorder. Neurology 72:551–557
Peever J, Fuller PM (2017) The biology of REM sleep. Curr Biol 27:R1237–R1248
Peever L, Luppi H, Montplaisir J (2014) Breakdown in REM sleep circuitry underlies REM sleep behavior disorder. Trends Neurosci 37:279–288
Postuma RB, Gagnon JF, Bertrand JA, Génier Marchand D, Montplaisir JY (2015) Parkinson risk in idiopathic REM sleep behavior disorder: preparing for neuroprotective trials. Neurology 84:1104–1113
Ramaligam V, Chen MC, Saper CB, Lu J (2013) Perspectives on the rapid eye movement sleep switch in rapid eye movement sleep behavior disorder. Sleep Med 14:707–7013
Recasens A, Dehay B, Bove J, Carballo-Carbajal I, Dovero S, Perez-Villalba A, Fernagut PO, Blesa J, Parent A, Perier C, Fariñas I, Obeso JA, Bezard E, Vila M (2014) Lewy body extracts from Parkinson disease brains trigger a-synuclein pathology and neurodegeneration in mice and monkeys. Ann Neurol 75:351–362
Reinoso-Suárez F, de Andrés I, Rodrigo-Angulo ML, Garzón M (2001) Brain structures and mechanisms involved in the generation of REM sleep. Sleep Med Rev 5:67–77
Rye DB (1997) Contributions of the pedunculopontine region to normal and altered REM sleep. Sleep 20:855–890
Rye DB, Bliwise DL (2004) Movement disorders specific to sleep and the nocturnal manifestations of waking movement disorders. In: Watts RL, Koller WC (eds) Movement disorders: neurologic principles and practice, 2nd edn. McGraw Hill, New York, pp 855–890
Sabater L, Gaig C, Gelpi E, Bataller L, Lewerenz J, Torres-Vega E, Contreras A, Giometto B, Compta Y, Embid C, Vilaseca I, Iranzo A, Santamaría J, Dalmau J, Graus F (2014) A novel non-rapid-eye movement and rapid-eye-movement parasomnia with sleep breathing disorder associated with antibodies to IgLON5: a case series, characterisation of the antigen, and post-mortem study. Lancet Neurol 13:575–586
Sakai K, Kanamori N, Jouvet M (1979) Neuronal activity specific to paradoxical sleep in the bulbar reticular formation in the unrestrained cat. C R Seances Acad Sci D 289:557–561
Sandford LD, Cheng CS, Sivestri AJ (2001) Sleep and behavior in rats with pontine lesions producing REM without atonia. Sleep Research Online 4:1–5
Scammel TE, Arrigoni E, Lipton JO (2017) Neural circuitry of wakefulness and sleep. Neuron 93:747–765
Schenck CH, Mahowald MW (1992) Motor dyscontrol in narcolepsy: rapid-eye-movement (REM) sleep without atonia and REM sleep behaviour disorder. Ann Neurol 32:3–10
Schenck CH, Mahowald MW (2002) REM sleep behavior disorder: clinical, developmental, and neuroscience perspectives 16 years after its formal identification in SLEEP. Sleep 25:120–138
Schenck CH, Bundlie SR, Ettinger MG, Mahowald MW (1986) Chronic behavioural disorders of human REM sleep: a new category of parasomnia. Sleep 9:293–308
Schenck CH, Bundlie SR, Patterson AL, Mahowald MW (1987) Rapid eye movement sleep behavior disorder. A treatable parasomnia affecting older adults. JAMA 257:1786–1789
Schenck CH, Bundlie SR, Mahowald MW (1996) Delayed emergence of a parkinsonian disorder in 38% of 29 older men initially diagnosed with idiopathic rapid eye movement sleep behavior disorder. Neurology 46:388–392
Schenckel E, Siegel JM (1989) REM sleep without atonia after lesions of the medial medulla. Neursci Lett 98:159–165
Scherfler C, Frauscher B, Schocke M, Iranzo A, Gschliesser V, Seppi K, Santamaria J, Tolosa E, Högl B, Poewe W, SINBAR (Sleep Innsbruck Barcelona) Group (2011) With and gray matter abnormalities in idiopathic rapid eye movement disorder: a diffusion-tensor imaging and voxel-based morphometry study. Ann Neurol 12:284–288
Shouse MN, Siegel JM (1992) Pontine regulation of REM sleep components in cats: integrity of the pedunculopontine tegmentum (PPT) is important for phasic events but unnecessary for atonia during REM sleep. Brain Res 571:50–63
Siegel J (2009) The neurobiology of sleep. Semin Neurol 29:277–296
Silber MH, Krahan LE, Morgenthaler T (2004) Physiological basis of sleep. In: Silber MH, Krahan LE, Morgenthaler T (eds) Sleep medicine in clinical practice. Taylor & Francis, London, pp 3–24
Sprenger FS, Stefanova N, Gelpi E, Seppi K, Navarro-Otano J, Offner F, Vilas D, Valldeoriola F, Pont-Sunyer C, Aldecoa I, Gaig C, Gines A, Cuatrecasas M, Högl B, Frauscher B, Iranzo A, Wenning GK, Vogel W, Tolosa E, Poewe W (2015) Enteric nervous system α-synuclein immunoreactivity in idiopathic REM sleep behavior disorder. Neurology 85:1761–1768
Stefani A, Gabelia D, Mitterling T, Poewe W, Högl B, Frauscher B (2015) A prospective video-polysomnographic analysis of movements during physiological sleep in 100 healthy sleepers. Sleep 38:1479–1487
Tamgüney G, Korczyn AD (2017) A critical review of the prion hypothesis of human synucleinopathies. Cell Tissue Res 8. https://doi.org/10.1007/s00441-017-2712-y
Tiriac A, Uitermarkt BD, Fanning AS, Sokoloff G, Blumberg MS (2012) Rapid whisker movements in sleep in new born rats. Curr Biol 22:2075–2080
Tiriac A, Del Rio-Bermudez C, Blumberg MS (2014) Self-generated movements with “unexpected” sensory consequences. Curr Biol 24:2136–2141
Valencia Garcia S, Libourel PA, Lazarus M, Grassi D, Luppi PH, Fort P (2017) Genetic inactivation of glutamate neurons in the rat sublaterodorsal tegmental nucleus recapitulates REM sleep behaviour disorder. Brain 140:414–428
Valencia Garcia S, Brischoux F, Clément O, Libourel PA, Arthaud S, Lazarus M, Luppi PH, Fort P (2018) Ventromedial medulla inhibitory neuron inactivation induces REM sleep without atonia and REM sleep behavior disorder. Nat Commun 9:504. https://doi.org/10.1038/s41467-017-02761-0
Verhave PS, Jongsma MJ, Van den Berg RM, Vis JC, Vanwersch RA, Smit AB, Van Someren EJ, Philippens IH (2011) REM sleep behaviour disorder in the marmoset MPTP model of early Parkinson disease. Sleep 34:119–1125
Vetrivelan R, Fuller PM, Tong Q, Lu J (2009) Medullary circuitry regulating rapid eye movement sleep and motor atonia. J Neurosci 29:9361–9369
Vilas D, Iranzo A, Tolosa E, Aldecoa I, Berenguer J, Vilaseca I, Martí C, Serradell M, Lomeña F, Alós L, Gaig C, Santamaria J, Gelpi E (2016) Assessment of α-synuclein in submandibular glands of patients with idiopathic rapid-eye-movement sleep behaviour disorder: a case-control study. Lancet Neurol 15:708–718
Weber F, Chung S, Beier KT, Xu M, Luo L, Dan Y (2015) Control of REM sleep by ventral medulla GABAergic neurons. Nature 526:435–438
Wu FS, Yang YC, Tsai JJ (1999) Melatonin potentiates the GABA(A) receptor-mediated current in cultured chick spinal cord neurons. Neurosci Lett 260:177–180
Zagrodzka J, Hedberg CE, Mann GL, Morrison AR (1998) Contrasting expressions of aggressive behavior related by lesions of the central nucleus of the amygdala during wakefulness and rapid eye movement sleep without atonia in cats. Behav Neurosci 112:589–602
Acknowledgments
I thank Dr. Ellen Gelpi for providing Fig. 10.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Iranzo, A. The REM sleep circuit and how its impairment leads to REM sleep behavior disorder. Cell Tissue Res 373, 245–266 (2018). https://doi.org/10.1007/s00441-018-2852-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-018-2852-8