Abstract
Type 1 diabetes mellitus (T1DM) is an autoimmune disease characterized by lack of insulin and irreversible destruction of islet β cells. In order to alleviate the symptoms, lifelong exogenous insulin administration has been the primary treatment of T1DM. In recent years, as a novel promising therapy, the transplantation of mesenchymal stem cells (MSCs) with or without pancreatic islets has achieved great therapeutic effects in animal models due to their multipotency along with their secretion of cytokines, angiogenic factors and immunomodulatory substances. There is plenty of evidence showing that MSCs can delay T1DM onset, reverse hyperglycemia after onset and increase insulin production. To date, the immunoregulation and immunosuppression of MSCs have been widely proved but the exact mechanisms are still not clear enough. Therefore, in this review, we mainly discuss the immunologic mechanism of MSCs in moderating the immune response of T1DM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
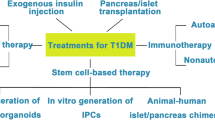
Type 1 diabetes mellitus (T1DM) is a chronic, multifactorial autoimmune disease characterized by the irreversible destruction of insulin-secreting β cells. T1DM is induced by the activation of the specific autoimmunity and ultimately results in the loss of insulin production and secretion (Figliuzzi 2014). The morbidity and mortality of T1DM have been increasing in recent these years (Group 2015). Lifelong exogenous insulin administration by insulin pump or multiple daily injections is nowadays the primary treatment of T1DM. But it is difficult to maintain physiological insulin levels and is therefore not very effective in reducing complications such as retinopathy, nephropathy and neuropathy. Much work has been carried out to search for a new effective treatment.
Islet transplantation emerges as a promising treatment to cure T1DM. However, the long-term outcome is still poor because of the shortage of transplant donors, immunological rejection, long-time immunosuppression and some other problems (Gruessner and Gruessner 2016; Jamiolkowski 2012). In recent years, mesenchymal stem cells (MSCs) have been highlighted as a novel regenerative therapy for their multipotency, self-renewal, low immunogenicity and high immunomodulatory properties. They can be derived from many different kinds of tissues and organs such as bone marrow, umbilical cord blood, placenta, cartilage and adipose tissue (Dominguez-Bendala 2012). Considering the abundant resource, there are no ethical problems in clinical trials such as with embryonic stem cells. MSCs are distinguished from other pluripotent stem cells for their great immunomodulatory functions, which makes them promising in treating T1DM. Several in vitro co-culture studies have shown that MSCs can inhibit the proliferation of splenocytes of T1DM mice (Abdi et al. 2015). And in vivo, the function of MSCs has also been demonstrated (Hu et al. 2015). They can delay the onset of T1DM and reduce hyperglycemia in diabetes mice (Hu et al. 2015). And it has also been demonstrated that MSCs combined with pancreatic islets are able, when injected, to affect both survival and function of pancreatic islets in T1DM models due to their immunosuppressive properties (American Diabetes 2013). MSCs also have the ability to regulate immune cells, especially T cells that play a significant role in T1DM.
Through a variety of research, we can infer that the therapeutic value of MSCs for T1DM have logical potential but that the exact mechanisms are still not clear enough for clinical application. Therefore, in this review, we mainly discuss the immunologic mechanism of MSCs in moderating the immune response of T1DM. The immunomodulatory function of MSCs to effector T cells, Tregs and APCs is examined in detail.
Pathogenesis of T1DM
A combination of environmental risk factors, genetic predisposition and autoimmune-mediated processes contribute to T1DM etiology. During the progression of T1DM, autoimmune reaction is the key step, in which T cells play an important role. T cells can be divided into at least three groups based on their function, including T helper cells (subsets Th1, Th2, and Th17 cells), cytotoxic T lymphocytes (CTLs) and regulatory T cells (Tregs). Under normal circumstances, these subsets of T cells interact with each other and maintain immune response homeostasis by cell-to-cell contact, cytokines and soluble molecules.
Initial CD4+T cells differentiate into Th1 cells in the presence of interleukin 12 (IL-12), IL-27 and interferon-γ (IFN-γ) (Hermann-Kleiter and Baier 2010), which secrete IFN-γ, tumor necrosis factor α (TNF-α), IL-2 and IL-1, mediating cellular immunity. When initial CD4+T cells are activated in the presence of IL-4, Th2 cells differentiate and secrete IL-4, IL-10 and IL-13, mediating the humoral immunity. Th17 cells are differentiated from the initial CD4+T cells by the influence of transforming growth factor-β (TGF-β) and IL-6, are defined by the dominant expression of IL-17A and also secrete IL-21, IL-22 and IL-17F (Awasthi and Kuchroo 2009). Th17 cells and Th1 cells are both pro-inflammatory phenotypes playing an important role in the inflammatory responses of the human body and have been shown to be involved in a variety of autoimmune diseases.
Tregs are named according to their functional subsets and their regulation function of the immune response. Depending on the different sources, CD4+Tregs are divided into two subgroups, natural regulatory T cells (nTregs) and induced regulatory T cells (iTregs). After the negative selection in the thymus, the nTregs mature, gain CD4+CD25+FOXP3+expression and secrete TGF-β and IL-10, while the iTregs are induced by the CD4+T cells outside the thymus and gain CD25+ expression. By intercellular contact, the Tregs produce soluble factors and make negative regulation of the major subtypes of Th cells mentioned above, while other immune cells also make immunosuppressive effects (Wan and Flavell 2009) and maintain homeostasis and tolerance to self-antigens.
The CD8+CTLs can recognize the major histocompatibility complex I (MHC-I) and antigenic peptides, then induce apoptosis of target cells via pro-apoptotic surface receptors or release of cytotoxic granules. CTLs can also release IFN-γ, TNF-α and TNF-β to inhibit viral replication and recruit macrophages to the infection site.
In the progression of T1DM, genetic predisposition combines with environmental factors and pancreatic β cell autoantigens are recognized by antigen-presenting cells (APCs), including dendritic cells (DCs) and macrophages, which are the first to infiltrate islets followed by CD4+ and CD8+T lymphocytes, natural killer (NK) cells and B cells (Waldron-Lynch and Herold 2011). The autoantigens are presented together with the MHC-II molecules on the surface of APCs to trigger autoimmune responses. Subsequently, Th1 cells secrete IL-2 and IFN-γ, which promote the cytotoxicity of CTLs, inhibit Th2 cells and weaken the protective effects of Th2 cells. Furthermore, Th17 cells also contribute to this process (Honkanen et al. 2010) via secreting IL-17 in response to β-cell autoantigens, which attract inflammatory cell infiltration and enhances neutrophil function (Glenn and Whartenby 2014), while macrophages are activated and then chemotaxis to the injury sites. Th1, Th17 and macrophages induce β-cell apoptosis by secreting cytokines (Arif et al. 2011). IL-17 can exacerbate the apoptosis induced by the combination of IL-1β and IFN-γ or TNF-α and IFN-γ (Arif et al. 2011; Yeung et al. 2012). CTLs, which are important T1DM-infiltrating cells, destroy pancreatic β cells by releasing perforin and cytotoxic granules as well as Fas-mediated apoptosis (Arif et al. 2011; Notkins 2002). Ultimately, T cell-mediated cell destruction is effected by the interplay between receptor-mediated interactions (e.g., Fas-Fas ligand, CD40-CD40 ligand and TNF-TNF receptor), secretion of pro-inflammatory cytokines and reactive oxygen species (ROS) and the release of granzymes and perforin from cytotoxic effector T cells (Chhabra and Brayman 2013) (Fig. 1). Autoantigens are also presented to B cells, which produce specific autoantibodies to the islet cell, insulin, GAD (GAD 65) and the tyrosine phosphatases IA-2 and IA-2β (American Diabetes 2013). These autoantibodies combining with NK cells contribute to the destruction of pancreatic β cells. The autoimmune process in T1D is also composed of regulatory components, such as Tregs. The reduction of Treg frequency could accelerate the onset of autoimmune diabetes in NOD mice (Salomon et al. 2000).
Main pathogenesis of T1DM. B cell autoantigens are presented by antigen-presenting cells (APCs) to active T cells, including Th1, Th17 and CTLs. Th1 secrete pro-inflammatory mediating autoimmune response; IFN-γ is a key cytokine. Activated CTLs destroy β cells by releasing perforin and cytotoxic granules as well as Fas-mediated apoptosis, while NK cells destroyed β cells directly. Th17 secreted pro-inflammatory cytokine IL-17, which exacerbated the apoptosis induced by the combination of IL-1β and IFN-γ or TNF-α and IFN-γ. These immune cells work together to trigger β cell destruction and reduce insulin levels
Immunomodulatory function of mesenchymal stem cells
MSCs are multipotential non-hematopoietic progenitor cells that can be isolated from a number of adult tissues, including bone marrow, umbilical cord blood, placenta, cartilage and adipose tissues. Though they are rare in these tissues, their great capacity for self-renewal allows for the efficient expansion of these cells in vitro. And they can differentiate in vitro into cells of the mesoderm lineage such as adipocytes, chondrocytes and osteocytes. Human MSCs are characteristic of low immunogenicity and immune tolerance (Majumdar et al. 2003) because they lack expression of major histocompatibility II (MHC-II) (Le Blanc et al. 2003) and co-stimulatory molecules CD80(B7-1), CD86 (B7-2), CD40 and CD40L (Hematti et a.l 2013; Wang et al. 2014) only express the MHC-I molecular itself. Thus, MSCs are able to induce peripheral tolerance and will not lead to proliferation of allogeneic and autoreactive lymphocytes. In addition, MSCs exhibit strong immune regulatory function. They have been shown to inhibit the proliferation and function of major immune cell populations such as T cells, B cells and NK cells, induce CD4+/CD8+ Foxp3+ Tregs and modulate the activities of DCs, by cell–cell contact and cytokine secretion both in vivo and in vitro (Abdi et al. 2008; Fiorina et al. 2011). Their low immunogenicity and immunomodulatory properties make them promising in transplantation both alone and in combination with islets.
Immunological mechanism of MSCs in T1DM therapy
T1DM is an autoimmune disease characterized by a lack of insulin and irreversible destruction of islet β cells. It has been widely proved that MSC administration can delay the onset of T1DM and reduce the hyperglycemia after onset. In some T1DM model mice experiments, administration of MSCs increased the level of insulin and reduced hyperglycemia (Hu et al. 2015; Jurewicz et al. 2010; Yaochite et al. 2015). The supernatant of MSCs also has an effect but was not as efficient as MSCs (Aali et al. 2014; Liu et al. 2012). The protection of MSCs to β cells is via cell-to-cell contact and soluble factors.
After administration, MSCs were able to polarize into two distinctly phenotypes depending on inflammatory milieu and changed the microenvironment and the proportion of immune cells, while the infiltration of inflammatory cells reduced. MSCs were detected in the pancreatic section (Aali et al. 2014). The regenerative role of MSCs can be mediated by protective effects on functional islet cells and also differentiation potency to insulin-producing cells in vivo and in vitro (Rahavi et al. 2015). A direct co-culture of MSCs and islets also showed that MSCs lost their fibroblastic-like morphology and differentiated into insulin-producing cells (Scuteri et al. 2014).The view that MSCs could migrate to the sites has been accepted but whether or not they can differentiate into insulin-producing cells is still controversial, some researchers showing that MSCs could differentiate into insulin-producing cells (Dong et al. 2008; Xie et al. 2009), while other studies obtained the opposite results (Dong et al. 2008; Wang et al. 2014).
Their immunomodulatory function has been proved in T1DM: both undifferentiated and differentiated MSCs can inhibit T cell proliferation in autologous and allogeneic lymphocyte reactions. To analyze the cytokines of DCs, the initial and activation of T cells and NK cells after co-culture indicated that MSCs could increase anti-inflammatory factors and increase the number of Treg (Le Blanc et al. 2004; Maccario et al. 2005). Studies have shown that MSCs influence the differentiation and maturation of dendritic cells from monocytes and interfere with their ability to activate T cells (Uccelli et al. 2006) and MSCs can shift from Th1 to Th2.
MSCs can inhibit the autoimmune reactions but the details of therapeutic mechanisms of MSCs are still unclear. In recent studies, MSCs pre-activated by immune cells (Shi et al. 2010) mediated immunosuppression through the secretion of prostaglandin E2 (PGE2), indoleamine-2,3-dioxygenase (IDO), nitric oxide (NO), transforming growth factor-beta (TGF-β) and human growth factor (HGF), which can widely inhibit the proliferation and activation of T cells (English et al. 2010; Ren et al. 2010; Yeung et al. 2012) (Fig. 2). Using antibodies to HGF, TGF-β or IL-6, either alone or in combination, T cell proliferation could not be inhibited by MSCs (Li et al. 2010). MSCs need not be retained in the damaged pancreas to exert their therapeutic function, which represents the importance of cytokine secretion in immunomodulation (Yaochite et al. 2015). In the following section, we will mainly discuss the specific function of cytokines to different types of cells.
The immunoregulatory function of MSCs on immune cells. MSCs could down-regulate the proliferation and function of DCs and subsequently inhibit their stimulation to Th1 and CTLs. In addition, MSCs increase Tregs. Tregs can inhibit the function of Th1, Th17, CTLs and NKs, while increase the protective Th2
The polarization of MSCs
MSCs are able to adopt two distinctly acting phenotypes depending on the inflammatory environment both in vitro and in vivo. Similar to macrophage polarization into the M1 or M2 phenotypes, MSCs may polarize into proinflammatory MSC1 and antinflammatory MSC2 (Waterman et al. 2010).
Under the stimulation of proinflammatory cytokines IFN-γ, TNF, IFN-α and IL-1β, MSCs are able to regulate expression of a subset of TLRs that are expressed on the surface of MSCs, thus switching toward MSC1 and increasing its sensitivity to the inflammatory sites (Raicevic et al. 2010). In the absence of an inflammatory environment (low levels of TNF-α and IFN-γ), MSCs may adopt a proinflammatory phenotype (MSC1) and enhance T cell responses by secreting chemokines (e.g., MIP-1α and MIP-1β, RANTES, CXCL9 and CXCL10), which hinder lymphocytes at inflammatory sites, while in the presence of an inflammatory environment (high levels of TNF-α and IFN-γ). MSCs become activated and adopt an immune-suppressive phenotype (MSC2) by secreting high levels of soluble factors [e.g., IDO, PGE2, NO, TGF-β, HGF and hemoxygenase (HO)] that suppress T cell proliferation (Li et al. 2012; Ren et al. 2008).
There are many studies about the switch between MSC1 and MSC2. The basis is research exploring the regulatory mechanism of Toll-like receptors (TLRs), since MSC1 and MSC2 phenotypes were polarized by downstream TLR signaling (Nemeth et al. 2010; Tomchuck et al. 2008). The research of Waterman et al. (2010) indicated that hMSCs express several TLRs (e.g., TLR3 and TLR4) and the immunological characteristics of them are drastically affected by specific TLR-agonist engagement. TLR4-primed MSCs (MSC2) mostly elaborate pro-inflammatory mediators, while TLR3-primed MSCs (MSC2) express mostly immunosuppressive ones. Mounayar et al. (2015) found that overexpression of human STAT1 or of a constitutively active PI3Ka mutant shifted MSCs into a MSC2-like phenotype i.e., it strongly potentiated IFNγ-mediated IDO production in vitro. And in the case of STAT1 overexpression, T-cell suppression was also enhanced by MSCs (Mounayar et al. 2015). This research suggests that the phenotypic regulatory switching between MSC1 and MSC2 may be one of the mechanisms enhancing the immunosuppressive function of MSC for the treatment of various inflammatory disorders, including type 1 diabetes.
The regulation function of MSCs to T cells
There are a variety of immune cells participating in the pathogenesis of T1DM in which the T cells are one of the major groups, including T helper cells (Th) such as Th1, Th2, Th17, regulatory T cells (Treg) and cytotoxic T cells (CTLs), which are mediated by immune regulation factors. Under normal circumstances, through the secretion of cytokines and other signaling molecules, T cells restrain and cooperate with each other, maintaining the balance of the body’s immune response. In this section, we try to discuss the function of MSCs to different T cell phenotypes.
The regulation function of MSCs to effector T cells
Th1 cells are the crucial immunity effectors against intracellular bacteria and protozoa. In the progression of T1DM, Th1 cells are the main effector T cells contributing to β cells destruction. They are triggered by IL-2 and IL-12 and activated in the presence of IFN-γ, IL-1, IL-2 and TNF-α. The effector functions of Th1 cells include activation and recruitment of macrophages CD8+T cells, IgG-secreting B cells and IFN-γ CD4+T cells. IFN-γ can activate macrophages to phagocytose and activate nitric oxide synthase to produce NOx free radicals to kill β cells, which is a vital pro-inflammatory cytokine.
In contrast to Th1 cells, Th2 cells are protective cells in the process of the onset of T1DM. MSCs can ameliorate T1DM by the secretion of IL-4, alter the ratio of Th1/Th2 in vivo with a Th1 to Th2 shift and promote the maturity of naive T cells tending to Th2 phenotype (Li et al. 2010). In addition, in the co-culture system of diabetic peripheral blood mononuclear cells (PBMCs) with human bone marrow, IL-4 in the supernate was significantly higher than the control group (Favaro et al. 2014; Zanone et al. 2010). In addition, MSCs can promote the secretion of IL-4 and the T cell phenotype shift to the anti-inflammatory Th2 cells (Zanone et al. 2010).
It has been demonstrated that MSCs have the capacity to modulate immune reaction in vitro and in vivo where they polarize the pro-inflammatory state to the anti-inflammatory state, reduce IFN-γ and increase IL-4. This is mediated by a shift in the Th1/Th2 cells balance or by inhibition of Th17 differentiation and IL17- production (Rahavi et al. 2015).
Th17 cells contribute to the progress of T1DM with a higher IL-17 production in patients. Inhibition of Th17 cell-mediated inflammation and autoimmunity by MSC administration has been reported in models of T1DM. In the NOD mice model, the blockade of IL-17 is protective (Emamaullee et al. 2009). MSCs can inhibit Th17 cells development through various ways including inhibition of PGE2, IL-10 and PD-1/PD-L1 ligation (Ghannam et al. 2010; Luz-Crawford et al. 2012). Ghannam et al. (2010) also found that human MSCs could yield regulatory effects on Th17 cells in an inflammatory environment by down-regulating the Th17 cell-specific transcription factor retinoid-acid receptor-related orphan receptor gamma t (RORγ t) and up-regulating FOXP3. In addition, human MSCs-derived microvisicles (MVs) may play a big role during the modulation compared with the evident reduction of Th17 cells in the control group (Favaro et al. 2014). MVs significantly decreased IFN-γ spots and levels in glutamic-acid-decarboxylase (GAD) 65-stimulated PBMCs, and significantly increased TGF-β, IL-10, IL-6 and PGE2 levels (Favaro et al. 2014). Furthermore, MVs decreased the number of Th17 cells and the levels of IL-17 and increased FOXP3+ regulatory T cells in GAD65-stimulated PBMCs (Favaro et al. 2014). And in the co-culture model, MSCs mainly suppressed immature Th17 cells while there was no evident suppression of mature Th17 cells (Ait-Oufella et al. 2006).
CTLs mediate β cell apoptosis in the process of T1DM. Despite the expression of MHC I on the MSCs surface, MSCs were still resistant to CTLs (Rasmusson et al. 2007). The administration of MSCs has the potential to reduce CTLs function via direct effects on CTLs as well as through inhibition of Th cells responses. In addition, the incapacity of MSCs to induce CTLs to secrete pro-inflammatory cytokines or CD25 is another reason why MSCs could survive (Rasmusson et al. 2007). Li et al. (2010) transplanted islets to T1DM mice and found that the CTL1/CTL2 ratio was altered with a CTL1 to CTL2 shift and that the latter is protective. As CTLs are the most important immune cells for eliminating abnormal cells, inhibition of CTLs may increase the risk of cancer (Han et al. 2012; Patel et al. 2010). MSCs enhanced Tregs numbers and Th2 cell-related cytokines as well as inhibited proliferation and release of granzyme B by CTLs, all of which result in the protection of cancer cells from immune-mediated lysis (Patel et al. 2010) (Table 1). What is more, the suppressive effects of MSCs were observed not only in memory CD4+ and memory CD8+T cells but also in naive CD4+T and naive CD8+T cells (Li et al. 2010). The suppressive effects of memory CD8+T cells were more profound. MSCs can secret large amounts of C-X-C motif ligand12 (CXCL12), a chemokine that promotes the homing of memory CD8+T cells (Mazo et al. 2005). In conclusion, MSCs can modulate effector T cells from pro-inflammatory to anti-inflammatory, reducing β cell destruction.
The regulation function of MSCs to Tregs
Tregs that are considered a member of the immune regulatory family play an important role in indirect immunosuppression of MSCs. A variety of evidence has shown, both in vitro and in vivo, that MSCs increased Tregs (Bassi et al. 2012b; Ghannam et al. 2010). For instance, in NOD mice, an increase of Tregs was found in the islets after the administration of MSCs, while, in vitro, MSCs have been proved to be a promoter of the expansion of Tregs through a cell-to-cell contact-dependent manner mediated by PD-L1. Then, CTLA 4, a ligand–protein molecular on the surface of the Tregs can combine with CD80/CD86 on the surface of the DCs and lead to the excitation of IDO in DCs, catalyzing tryptophan into the urea and reducing the amount of free tryptophan with a lower level of T cell activation (Meisel et al. 2004).
MSCs are able to enhance Tregs proliferation, which can secrete IL-10 and TGF-β, mediating the inflammatory reaction of Th1 and Th17 and reduce the cytotoxicity of CTLs, thus inducing immune tolerance (Luz-Crawford et al. 2013). MSCs can generate significantly higher numbers of Tregs compared to the control group both in vitro and in vivo by expressing TNF-α-stimulated gene 6 (TSG-6), a kind of anti-inflammatory protein (Kota et al. 2013). In addition, MSCs can induce CD4+T cells differentiating into Tregs. Tregs inhibiting the proliferation, activation and differentiation of Th1 and Th17 cells has become a novel therapy target (Ait-Oufella et al. 2006). MSCs-derived MVs can recover the balance between Th1 and Th2 cells and protect Tregs, increasing the amount of moderating factor IL-10, which is also an anti-inflammatory molecular (Rasmusson et al. 2007). In some graft rejection, allergy and immunological disease models, the protective effects of MSCs administration was reverted after the depletion of Tregs, which meant that up-moderating of Tregs is one of the main mechanisms of MSCs-mediated immunosuppression (English et al. 2010; Ge et al. 2010; Kavanagh and Mahon 2011).
The regulation function of MSCs to APCs
Besides up-regulation of Tregs, down-regulation of APCs is another mechanism of immunosuppression. DCs are the most important among all the APCs. They bridge the innate and adoptive immune systems. MSCs can directly inhibit both the maturation of monocytes and CD34+ precursor cells into DCs and the direct activation of DCs via the secretion of PGE2, IL-6, TSG-6, M-CSF and Jagged-2-mediated signaling (Y. Liu et al. 2014; Ramasamy et al. 2007; Su et al. 2011) and inhibition of up-regulation of CD40, CD86 and CD83 suppressed DC maturation. Furthermore, endocytosis of DCs and production of IL-12 and TNF-α were alleviated. IL-12 is not only a key cytokine in Th1 activation but also important in regulating the maturation and function of DCs. Reduction of IL-12 would interfere with antigen-presenting (Glenn and Whartenby 2014). In T1DM mice with combined transplantation of pancreatic islets and MSCs, the expression of CD11c (monocyte-derived DCs phenotype) and CD83 (mature DCs phenotype) was markedly reduced (Li et al. 2010). Down-regulation of MHC II antigen I-Ab and co-stimulatory molecule CD86 was also observed. Impaired antigen-presenting ability subsequently inhibits the downstream immune response (Li et al. 2010).
Macrophages play more as inflammatory cells rather than APCs in T1DM. There are two types of macrophages: M1 produce pro-inflammatory cytokines, while M2 produce anti-inflammatory cytokines. MSCs have the ability to modulate the phenotype of macrophages by inducing a shift from M1 to M2, thereby accelerating the recovery process (Bernardo and Fibbe 2013). MSCs can reduce the expression of CD86 and MHC II on macrophages that diminished their stimulatory potency (Glenn and Whartenby 2014). MSCs have also been reported to directly induce an M2 phenotype. This directed maturation is partially regulated via direct cell contact but also by MSCs secretion of PGE2, IL-6 and GM-CSF (Le Blanc and Davies 2015).
Conclusions and future directions
MSCs can be readily isolated from plentiful sources without ethical problems. The properties of weak immunogenicity and strong immunoregulation make them promising in treating autoimmune diseases including T1DM. Through many animal and clinical trials, MSCs have been demonstrated to have the ability to modulate immune cells and delay the onset of T1DM mice (Kota et al. 2013) and to reduce hyperglycemia after onset with or without islets transplantation (Bassi et al. 2012a; Li et al. 2010). The protective efficiency of MSCs in T1DM requires a long period to reduce blood glucose depending on its dose (Yaochite et al. 2015). The study of the interaction between MSCs and T lymphocytes could build a theoretical base for clinical application, give prophylactic therapy to high-risk groups and reduce morbidity. Those findings may also be useful in other auto-immune diseases, such as systemic lupus erythematous, rheumatoid arthritis and allergic encephalomyelitis, in which MSCs also show great therapeutic effects.
However, MSCs generally lack homing molecules, hindering their spreading migration and colonization in an inflammatory milieu following intravenous or intra-arterial administration and the entrapment of the cells mainly colonizes in the lungs, which could decrease the number of MSCs migrating to target areas for treatment (Eggenhofer et al. 2012; Plock et al. 2013). Enforced hematopoietic cell E- and L-selectin ligand (HCELL) expression primes transendothelial migration of both murine MSC and human MSC and reverses hyperglycemia of autoimmune diabetes in NOD mice (Abdi et al. 2015; Thankamony and Sackstein 2011). Abdiet al. (2015) found that administration of HCELL + MSCs resulted in durable reversal of hyperglycemia, whereas only temporary reversal was observed following administration of HCELL − MSCs. A better effect could be obtained through local injection rather than systemic administration and intrasplenic injection reverted hyperglycemia in a higher proportion in diabetic-treated mice compared with the intrapancreatic injection route. Based on the above-mentioned result, we think that it supports the idea that immunoregulation properties play a more important role than the regenerative and repairing properties of MSCs in T1DM, because the spleen is an immune organ (Yaochite et al. 2015). Though MSCs have low immunogenicity, allogeneic MSCs can still be recognized and removed by the receptor’s immune system (Fiorina et al. 2009). Though MSCs are effective when administrated either locally or systematically (Longoni et al. 2010), appropriate local administration may improve the therapeutic function of MSCs and reduce side effects.
In recent studies, most researchers used MSCs from healthy people or animals to study their therapeutic function. Though there are data from diabetes mice-derived MSCs (Fiorina et al. 2009), the data of human MSCs from patients themselves to treatT1DM are lacking. Investigations of clinical trials using hMSCs as a part of treatment to explore the clinical effect of MSCs are ongoing.
As the studies go deeper, there is a safety problem emerging that administration of MSCs may increase the risk of tumor induction, either through spontaneous malignant transformation of MSCs themselves (Miura et al. 2006; Rubio et al. 2005; Tolar et al. 2007) or by the promotion of tumor development and growth (Djouad et al. 2003). Although spontaneous transformation has not so far been noted in clinical trials using human MSCs, it has been demonstrated that long-term in vitro expansion of MSCs increases the risk of accumulating mutations and consequently enhancing their potential for tumor development in vivo (Miura et al. 2006; Tolar et al. 2007). There is evidence showing that use of autologous MSCs induces tumors while use of allogeneic MSCs does not, due to the recognition of allogeneic MSCs by the host immunosurveillance (Fiorina et al. 2009). This safety problem should be highlighted and avoided.
To conclude, the therapeutic function of MSCs, either allogeneic or isogenic, in T1DM has been proven both in vivo and in vitro. Great immune-regulatory functions and promotion of β cell regeneration have been shown but we still have a long way to go before clinical application. The administration of MSCs is a promising cellular treatment deserving deeper investigation. Compared with traditional systemic delivery, local injection has shown better therapeutic effects and fewer side effects and the therapeutic is dose-dependent. We should minimize the injury of repeating injections as well as obtain an effective therapeutic dose to find a balance. And when we use the immunosuppression peculiarity of MSCs, we need to avoid the risk of cancer. What is more, though there are many common denominators among different kinds of MSCs, they also have their own personalities and thus have different effects on different diseases.
References
Aali E, Mirzamohammadi S, Ghaznavi H, Madjd Z, Larijani B, Rayegan S, Sharifi AM (2014) A comparative study of mesenchymal stem cell transplantation with its paracrine effect on control of hyperglycemia in type 1 diabetic rats. J Diabetes Metab Disord 13(1):76. doi:10.1186/2251-6581-13-76
Abdi R, Fiorina P, Adra CN, Atkinson M, Sayegh MH (2008) Immunomodulation by mesenchymal stem cells: a potential therapeutic strategy for type 1 diabetes. Diabetes 57(7):1759–1767. doi:10.2337/db08-0180
Abdi R, Moore R, Sakai S, Donnelly CB, Mounayar M, Sackstein R (2015) HCELL Expression on Murine MSC Licenses Pancreatotropism and Confers Durable Reversal of Autoimmune Diabetes in NOD Mice. Stem Cells 33(5):1523–1531. doi:10.1002/stem.1948
Ait-Oufella H, Salomon BL, Potteaux S, Robertson AK, Gourdy P, Zoll J, Mallat Z (2006) Natural regulatory T cells control the development of atherosclerosis in mice. Nat Med 12(2):178–180. doi:10.1038/nm1343
American Diabetes, Association (2013) Diagnosis and classification of diabetes mellitus. Diabetes Care 36 Suppl 1:S67-74 doi: 10.2337/dc13-S067
Arif S, Moore F, Marks K, Bouckenooghe T, Dayan CM, Planas R, Peakman M (2011) Peripheral and islet interleukin-17 pathway activation characterizes human autoimmune diabetes and promotes cytokine-mediated beta-cell death. Diabetes 60(8):2112–2119. doi:10.2337/db10-1643
Awasthi A, Kuchroo VK (2009) Th17 cells: from precursors to players in inflammation and infection. Int Immunol 21(5):489–498. doi:10.1093/intimm/dxp021
Bassi EJ, Moraes-Vieira PMM, Moreira-Sa CSR, Almeida DC, Vieira LM, Cunha CS, Camara NOS (2012a) Immune Regulatory Properties of Allogeneic Adipose-Derived Mesenchymal Stem Cells in the Treatment of Experimental Autoimmune Diabetes. Diabetes 61(10):2534–2545. doi:10.2337/db11-0844
Bassi EJ, Moraes-Vieira PM, Moreira-Sa CS, Almeida DC, Vieira LM, Cunha CS, Camara NO (2012b) Immune regulatory properties of allogeneic adipose-derived mesenchymal stem cells in the treatment of experimental autoimmune diabetes. Diabetes 61(10):2534–2545. doi:10.2337/db11-0844
Bernardo ME, Fibbe WE (2013) Mesenchymal stromal cells: sensors and switchers of inflammation. Cell Stem Cell 13(4):392–402. doi:10.1016/j.stem.2013.09.006
Chhabra P, Brayman KL (2013) Stem cell therapy to cure type 1 diabetes: from hype to hope. Stem Cells Transl Med 2(5):328–336. doi:10.5966/sctm.2012-0116
Djouad F, Plence P, Bony C, Tropel P, Apparailly F, Sany J, Jorgensen C (2003) Immunosuppressive effect of mesenchymal stem cells favors tumor growth in allogeneic animals. Blood 102(10):3837–3844. doi:10.1182/blood-2003-04-1193
Dominguez-Bendala J, Lanzoni G, Inverardi L, Ricordi C (2012) Concise review: mesenchymal stem cells for diabetes. Stem Cells Transl Med 1(1):59–63. doi:10.5966/sctm.2011-0017
Dong QY, Chen L, Gao GQ, Wang L, Song J, Chen B, Sun L (2008) Allogeneic diabetic mesenchymal stem cells transplantation in streptozotocin-induced diabetic rat. Clin Invest Med 31(6):E328–E337
Eggenhofer E, Benseler V, Kroemer A, Popp FC, Geissler EK, Schlitt HJ, Hoogduijn, MJ (2012) Mesenchymal stem cells are short-lived and do not migrate beyond the lungs after intravenous infusion. Front Immunol 3:297. doi: 10.3389/fimmu.2012.00297
Emamaullee JA, Davis J, Merani S, Toso C, Elliott JF, Thiesen A, Shapiro AM (2009) Inhibition of Th17 cells regulates autoimmune diabetes in NOD mice. Diabetes 58(6):1302–1311. doi:10.2337/db08-1113
English K, French A, Wood KJ (2010) Mesenchymal stromal cells: facilitators of successful transplantation? Cell Stem Cell 7(4):431–442. doi:10.1016/j.stem.2010.09.009
Favaro E, Carpanetto A, Lamorte S, Fusco A, Caorsi C, Deregibus MC, Zanone MM (2014) Human mesenchymal stem cell-derived microvesicles modulate T cell response to islet antigen glutamic acid decarboxylase in patients with type 1 diabetes. Diabetologia 57(8):1664–1673. doi:10.1007/s00125-014-3262-4
Figliuzzi M, Bonandrini B, Silvani S, Remuzzi A (2014) Mesenchymal stem cells help pancreatic islet transplantation to control type 1 diabetes. World J Stem Cells 6(2):163–172. doi:10.4252/wjsc.v6.i2.163
Fiorina P, Jurewicz M, Augello A, Vergani A, Dada S, La Rosa S, Abdi R (2009) Immunomodulatory function of bone marrow-derived mesenchymal stem cells in experimental autoimmune type 1 diabetes. J Immunol 183(2):993–1004. doi:10.4049/jimmunol.0900803
Fiorina P, Voltarelli J, Zavazava N (2011) Immunological applications of stem cells in type 1 diabetes. Endocr Rev 32(6):725–754. doi:10.1210/er.2011-0008
Ge W, Jiang JF, Arp J, Liu WH, Garcia B, Wang H (2010) Regulatory T-Cell Generation and Kidney Allograft Tolerance Induced by Mesenchymal Stem Cells Associated With Indoleamine 2,3-Dioxygenase Expression. Transplantation 90(12):1312–1320. doi:10.1097/TP.0b013e3181fed001
Ghannam S, Pene J, Moquet-Torcy G, Jorgensen C, Yssel H (2010) Mesenchymal stem cells inhibit human Th17 cell differentiation and function and induce a T regulatory cell phenotype. J Immunol 185(1):302–312. doi:10.4049/jimmunol.0902007
Glenn JD, Whartenby KA (2014) Mesenchymal stem cells: Emerging mechanisms of immunomodulation and therapy. World J Stem Cells 6(5):526–539. doi:10.4252/wjsc.v6.i5.526
Group, I. D. F. Diabetes Atlas (2015) Update of mortality attributable to diabetes for the IDF Diabetes Atlas: Estimates for the year 2013. Diabetes Res Clin Pract 109(3):461–465. doi:10.1016/j.diabres.2015.05.037
Gruessner AC, Gruessner RW (2016) Long-term outcome after pancreas transplantation: a registry analysis. Curr Opin Organ Transplant 21(4):377–385. doi:10.1097/MOT.0000000000000331
Hall SR, Tsoyi K, Ith B, et al. (2013) Mesenchymal stromal cells improve survival during sepsis in the absence of heme oxygenase-1: the importance of neutrophils. Stem Cells 31(2):397–407
Han ZP, Jing Y. Y, Zhang S. S, Liu Y, Shi Y. F, & Wei L. X (2012) The role of immunosuppression of mesenchymal stem cells in tissue repair and tumor growth. Cell Biosci 2. doi: Artn 8 10.1186/2045-3701-2-8
Hematti P, Kim J, Stein AP, Kaufman D (2013) Potential role of mesenchymal stromal cells in pancreatic islet transplantation. Transplant Rev (Orlando) 27(1):21–29. doi:10.1016/j.trre.2012.11.003
Hermann-Kleiter N, Baier G (2010) NFAT pulls the strings during CD4+ T helper cell effector functions. Blood 115(15):2989–2997. doi:10.1182/blood-2009-10-233585
Honkanen J, Nieminen JK, Gao R, Luopajarvi K, Salo HM, Ilonen J, Vaarala O (2010) IL-17 immunity in human type 1 diabetes. J Immunol 185(3):1959–1967. doi:10.4049/jimmunol.1000788
Hu J, Wang Y, Wang F, Wang L, Yu X, Sun R, Yan S (2015) Effect and mechanisms of human Wharton’s jelly-derived mesenchymal stem cells on type 1 diabetes in NOD model. Endocrine 48(1):124–134. doi:10.1007/s12020-014-0219-9
Jamiolkowski RM, Guo LY, Li YR, Shaffer SM, Naji A (2012) Islet transplantation in type I diabetes mellitus. Yale J Biol Med 85(1):37–43
Jurewicz M, Yang S, Augello A, Godwin JG, Moore RF, Azzi J, Abdi R (2010) Congenic mesenchymal stem cell therapy reverses hyperglycemia in experimental type 1 diabetes. Diabetes 59(12):3139–3147. doi:10.2337/db10-0542
Kavanagh H, Mahon BP (2011) Allogeneic mesenchymal stem cells prevent allergic airway inflammation by inducing murine regulatory T cells. Allergy 66(4):523–531. doi:10.1111/j.1398-9995.2010.02509.x
Kota DJ, Wiggins LL, Yoon N, Lee RH (2013) TSG-6 produced by hMSCs delays the onset of autoimmune diabetes by suppressing Th1 development and enhancing tolerogenicity. Diabetes 62(6):2048–2058. doi:10.2337/db12-0931
Le Blanc K, Davies LC (2015) Mesenchymal stromal cells and the innate immune response. Immunol Lett. doi:10.1016/j.imlet.2015.05.004
Le Blanc K, Tammik C, Rosendahl K, Zetterberg E, Ringden O (2003) HLA expression and immunologic properties of differentiated and undifferentiated mesenchymal stem cells. Exp Hematol 31(10):890–896
Le Blanc K, Rasmusson I, Gotherstrom C, Seidel C, Sundberg B, Sundin M, Ringden O (2004) Mesenchymal stem cells inhibit the expression of CD25 (interleukin-2 receptor) and CD38 on phytohaemagglutinin-activated lymphocytes. Scand J Immunol 60(3):307–315. doi:10.1111/j.0300-9475.2004.01483.x
Li FR, Wang XG, Deng CY, Qi H, Ren LL, Zhou HX (2010) Immune modulation of co-transplantation mesenchymal stem cells with islet on T and dendritic cells. Clin Exp Immunol 161(2):357–363. doi:10.1111/j.1365-2249.2010.04178.x
Li W, Ren G, Huang Y, Su J, Han Y, Li J, Shi Y (2012) Mesenchymal stem cells: a double-edged sword in regulating immune responses. Cell Death Differ 19(9):1505–1513. doi:10.1038/cdd.2012.26
Liu H, Lu K, MacAry PA, Wong KL, Heng A, Cao T, Kemeny DM (2012) Soluble molecules are key in maintaining the immunomodulatory activity of murine mesenchymal stromal cells. J Cell Sci 125(Pt 1):200–208. doi:10.1242/jcs.093070
Liu Y, Yin Z, Zhang R, Yan K, Chen L, Chen F, Jiang X (2014) MSCs inhibit bone marrow-derived DC maturation and function through the release of TSG-6. Biochem Biophys Res Commun 450(4):1409–1415. doi:10.1016/j.bbrc.2014.07.001
Longoni B, Szilagyi E, Quaranta P, Paoli GT, Tripodi S, Urbani S, Mosca F (2010) Mesenchymal Stem Cells Prevent Acute Rejection and Prolong Graft Function in Pancreatic Islet Transplantation. Diabetes Technol Ther 12(6):435–446. doi:10.1089/dia.2009.0154
Luz-Crawford P, Noel D, Fernandez X, Khoury M, Figueroa F, Carrion F, Djouad F (2012) Mesenchymal stem cells repress Th17 molecular program through the PD-1 pathway. PLoS ONE 7(9):e45272. doi:10.1371/journal.pone.0045272
Luz-Crawford P, Kurte M, Bravo-Alegria J, Contreras R, Nova-Lamperti E, Tejedor G, Carrion F (2013) Mesenchymal stem cells generate a CD4+CD25+Foxp3+ regulatory T cell population during the differentiation process of Th1 and Th17 cells. Stem Cell Res Ther 4(3):65. doi:10.1186/scrt216
Maccario R, Podesta M, Moretta A, Cometa A, Comoli P, Montagna D, Locatelli F (2005) Interaction of human mesenchymal stem cells with cells involved in alloantigen-specific immune response favors the differentiation of CD4+ T-cell subsets expressing a regulatory/suppressive phenotype. Haematologica 90(4):516–525
Majumdar MK, Keane-Moore M, Buyaner D, Hardy WB, Moorman MA, McIntosh KR, Mosca JD (2003) Characterization and functionality of cell surface molecules on human mesenchymal stem cells. J Biomed Sci 10(2):228–241
Mazo IB, Honczarenko M, Leung H, Cavanagh LL, Bonasio R, Weninger W, von Andrian UH (2005) Bone marrow is a major reservoir and site of recruitment for central memory CD8(+) T cells. Immunity 22(2):259–270. doi:10.1016/j.immuni.2005.01.008
Meisel R, Zibert A, Laryea M, Gobel U, Daubener W, Dilloo D (2004) Human bone marrow stromal cells inhibit allogeneic T-cell responses by indoleamine 2,3-dioxygenase-mediated tryptophan degradation. Blood 103(12):4619–4621. doi:10.1182/blood-2003-11-3909
Miura M, Miura Y, Padilla-Nash HM, Molinolo AA, Fu BJ, Patel V, Shi ST (2006) Accumulated chromosomal instability in murine bone marrow mesenchymal stem cells leads to malignant transformation. Stem Cells 24(4):1095–1103. doi:10.1634/stemcells.2005-0403
Moustakas A, Pardali K, Gaal A, Heldin CH (2002)_Mechanisms of TGF-beta signaling in regulation of cell growth and differentiation. Immunol Lett 82(1–2):85–91
Mounayar M, Kefaloyianni E, Smith B, Solhjou Z, Maarouf OH, Azzi J, Abdi R (2015) PI3kalpha and STAT1 Interplay Regulates Human Mesenchymal Stem Cell Immune Polarization. Stem Cells 33(6):1892–1901. doi:10.1002/stem.1986
Nemeth K, Leelahavanichkul A, Yuen PS, et al. (2009) Bone marrow stromal cells attenuate sepsis via prostaglandin E(2)-dependent reprogramming of host macrophages to increase their interleukin-10 production. Nature Med 15(1):42–49
Nemeth K, Mayer B, Mezey E (2010) Modulation of bone marrow stromal cell functions in infectious diseases by toll-like receptor ligands. J Mol Med (Berl) 88(1):5–10. doi:10.1007/s00109-009-0523-7
Notkins AL (2002) Immunologic and genetic factors in type 1 diabetes. J Biol Chem 277(46):43545–43548. doi:10.1074/jbc.R200012200
Park KS, Kim YS, Kim JH, et al. (2010) Trophic molecules derived from human mesenchymal stem cells enhance survival, function, and angiogenesis of isolated islets after transplantation. Transplantation. 89(5):509–517
Patel SA, Meyer JR, Greco SJ, Corcoran KE, Bryan M, Rameshwar P (2010) Mesenchymal Stem Cells Protect Breast Cancer Cells through Regulatory T Cells: Role of Mesenchymal Stem Cell-Derived TGF-beta. J Immunol 184(10):5885–5894. doi:10.4049/jimmunol.0903143
Plock JA, Schnider JT, Schweizer R, Gorantla VS (2013) Are cultured mesenchymal stromal cells an option for immunomodulation in transplantation? Front Immunol 4:41. doi:10.3389/fimmu.2013.00041
Raffaghello L, Bianchi G, Bertolotto M, et al. (2008) Human mesenchymal stem cells inhibit neutrophil apoptosis: a model for neutrophil preservation in the bone marrow niche. Stem Cells 26(1):151–162
Rahavi H, Hashemi SM, Soleimani M, Mohammadi J, Tajik N (2015) Adipose tissue-derived mesenchymal stem cells exert in vitro immunomodulatory and beta cell protective functions in streptozotocin-induced diabetic mice model. J Diabetes Res 2015:878535. doi:10.1155/2015/878535
Raicevic G, Rouas R, Najar M, Stordeur P, Boufker HI, Bron D, Lagneaux L (2010) Inflammation modifies the pattern and the function of Toll-like receptors expressed by human mesenchymal stromal cells. Hum Immunol 71(3):235–244. doi:10.1016/j.humimm.2009.12.005
Ramasamy R, Fazekasova H, Lam EW, Soeiro I, Lombardi G, Dazzi F (2007) Mesenchymal stem cells inhibit dendritic cell differentiation and function by preventing entry into the cell cycle. Transplantation 83(1):71–76. doi:10.1097/01.tp.0000244572.24780.54
Rasmusson I, Uhlin M, Le Blanc K, Levitsky V (2007) Mesenchymal stem cells fail to trigger effector functions of cytotoxic T lymphocytes. J Leukoc Biol 82(4):887–893. doi:10.1189/jlb.0307140
Ren G, Zhang L, Zhao X, Xu G, Zhang Y, Roberts AI, Shi Y (2008) Mesenchymal stem cell-mediated immunosuppression occurs via concerted action of chemokines and nitric oxide. Cell Stem Cell 2(2):141–150. doi:10.1016/j.stem.2007.11.014
Ren G, Zhao X, Zhang L, Zhang J, L’Huillier A, Ling W, Shi Y (2010) Inflammatory cytokine-induced intercellular adhesion molecule-1 and vascular cell adhesion molecule-1 in mesenchymal stem cells are critical for immunosuppression. J Immunol 184(5):2321–2328. doi:10.4049/jimmunol.0902023
Rubio D, Garcia-Castro J, Martin MC, de la Fuente R, Cigudosa JC, Lloyd AC, Bernad A (2005) Spontaneous human adult stem cell transformation (Retracted article. See vol. 70, pp. 6682, 2010). Cancer Res 65(8):3035–3039
Salomon B, Lenschow DJ, Rhee L, Ashourian N, Singh B, Sharpe A, Bluestone JA (2000) B7/CD28 costimulation is essential for the homeostasis of the CD4 + CD25+ immunoregulatory T cells that control autoimmune diabetes. Immunity 12(4):431–440
Scuteri A, Donzelli E, Rodriguez-Menendez V, Ravasi M, Monfrini M, Bonandrini B, Tredici G (2014) A double mechanism for the mesenchymal stem cells’ positive effect on pancreatic islets. PLoS ONE 9(1):e84309. doi:10.1371/journal.pone.0084309
Shi Y, Hu G, Su J, Li W, Chen Q, Shou P, Ren G (2010) Mesenchymal stem cells: a new strategy for immunosuppression and tissue repair. Cell Res 20(5):510–518. doi:10.1038/cr.2010.44
Spaggiari GM, Abdelrazik H, Becchetti F, Moretta L (2009) MSCs inhibit monocyte-derived DC maturation and function by selectively interfering with the generation of immature DCs: central role of MSC-derived prostaglandin E2. Blood 113(26):6576–6583
Su WR, Zhang QZ, Shi SH, Nguyen AL, Le AD (2011) Human gingiva-derived mesenchymal stromal cells attenuate contact hypersensitivity via prostaglandin E2-dependent mechanisms. Stem Cells 29(11):1849–1860. doi:10.1002/stem.738
Thankamony SP, Sackstein R (2011) Enforced hematopoietic cell E- and L-selectin ligand (HCELL) expression primes transendothelial migration of human mesenchymal stem cells. Proc Natl Acad Sci U S A 108(6):2258–2263. doi:10.1073/pnas.1018064108
Tolar J, Nauta AJ, Osborn MJ, Mortari AP, McElmurry RT, Bell S, Blazar BR (2007) Sarcoma derived from cultured mesenchymal stem cells. Stem Cells 25(2):371–379. doi:10.1634/stemcells.2005-0620
Tomchuck SL, Zwezdaryk KJ, Coffelt SB, Waterman RS, Danka ES, Scandurro AB (2008) Toll-like receptors on human mesenchymal stem cells drive their migration and immunomodulating responses. Stem Cells 26(1):99–107. doi:10.1634/stemcells.2007-0563
Uccelli A, Moretta L, Pistoia V (2006) Immunoregulatory function of mesenchymal stem cells. Eur J Immunol 36(10):2566–2573. doi:10.1002/eji.200636416
Waldron-Lynch F, Herold KC (2011) Immunomodulatory therapy to preserve pancreatic beta-cell function in type 1 diabetes. Nat Rev Drug Discov 10(6):439–452. doi:10.1038/nrd3402
Wan YY, Flavell RA (2009) How diverse--CD4 effector T cells and their functions. J Mol Cell Biol 1(1):20–36. doi:10.1093/jmcb/mjp001
Wang HW, Qiu XY, Ni P, Qiu XR, Lin XB, Wu WZ, Ma L (2014) Immunological characteristics of human umbilical cord mesenchymal stem cells and the therapeutic effects of their transplantion on hyperglycemia in diabetic rats. Int J Mol Med 33(2):263–270. doi:10.3892/ijmm.2013.1572
Waterman RS, Tomchuck SL, Henkle SL, Betancourt AM (2010) A new mesenchymal stem cell (MSC) paradigm: polarization into a pro-inflammatory MSC1 or an Immunosuppressive MSC2 phenotype. PLoS ONE 5(4):e10088. doi:10.1371/journal.pone.0010088
Xie QP, Huang H, Xu B, Dong X, Gao SL, Zhang B, Wu YL (2009) Human bone marrow mesenchymal stem cells differentiate into insulin-producing cells upon microenvironmental manipulation in vitro. Differentiation 77(5):483–491. doi:10.1016/j.diff.2009.01.001
Yaochite JN, Caliari-Oliveira C, de Souza LE, Neto LS, Palma PV, Covas DT, Donadi EA (2015) Therapeutic efficacy and biodistribution of allogeneic mesenchymal stem cells delivered by intrasplenic and intrapancreatic routes in streptozotocin-induced diabetic mice. Stem Cell Res Ther 6:31. doi:10.1186/s13287-015-0017-1
Yen BL, Yen ML, Hsu PJ, et al. (2013) Multipotent human mesenchymal stromal cells mediate expansion of myeloid-derived suppressor cells via hepatocyte growth factor/c-met and STAT3. Stem Cell Rep 1(2):139–151
Yeung TY, Seeberger KL, Kin T, Adesida A, Jomha N, Shapiro AM, Korbutt GS (2012) Human mesenchymal stem cells protect human islets from pro-inflammatory cytokines. PLoS ONE 7(5):e38189. doi:10.1371/journal.pone.0038189
Zanone MM, Favaro E, Miceli I, Grassi G, Camussi E, Caorsi C, Camussi G (2010) Human mesenchymal stem cells modulate cellular immune response to islet antigen glutamic acid decarboxylase in type 1 diabetes. J Clin Endocrinol Metab 95(8):3788–3797. doi:10.1210/jc.2009-2350
Acknowledgments
This research was supported by the National Natural Science Foundation of China (Grant No. 31150007, 31201052), Jilin Province Science and Technology Development Program for Young Scientists Fund (Grant No. 20150520036JH) and Bethune Medical Research Support Program - Advanced Interdisciplinary Innovation Project (Grant No. 2013101004).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Junbi Xv and Qianwen Ming contributed equally to this work.
Rights and permissions
About this article
Cite this article
Xv, J., Ming, Q., Wang, X. et al. Mesenchymal stem cells moderate immune response of type 1 diabetes. Cell Tissue Res 368, 239–248 (2017). https://doi.org/10.1007/s00441-016-2499-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-016-2499-2