Abstract
It is well established the link between inflammation and the development of insulin resistance and pathogenesis of type 2 diabetes. Type 1 diabetes is an autoimmune disease characterized by the destruction of insulin-producing pancreatic β cells mediated by autoreactive T lymphocytes and pro-inflammatory agents. Therefore, developing new strategies to efficiently control dysregulated inflammation could have substantial benefits in the treatment of diabetes. Recently, a novel population of non-tumorigenic pluripotent stem cells, named multilineage-differentiating stress-enduring (Muse) cells, was discovered. Muse cells secrete significant amounts of TGF-β1, a key cytokine governing down-modulation of T lymphocytes and macrophages. In this chapter, we discuss the immunomodulatory properties of Muse cells as well as the molecular mechanism of TGF-β1 as mediator of Muse cell action. We also describe the role of certain cytokines/growth factors highly expressed in Muse cells as potential mediators of their effects. Finally, we provide evidence of the beneficial effects of adipose tissue-derived Muse cells in an experimental mice model of type 1 diabetes.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Stem cells
- Inflammation
- Tissue regeneration
- TGF-β1
- Interleukins
- T lymphocytes
- Macrophages
- Adipose-derived stem cells
6.1 Introduction
Mesenchymal stromal cells (MSCs) are a group of multipotent stem cells from adult tissues with capacity to regulate the immune system, participating in both the innate and adaptive responses [1,2,3,4,5,6,7]. These cells have been described as capable of inhibiting both T cell proliferation and cytokine secretion [1, 3, 6]. They are also able to drive T helper balance towards a regulatory phenotype, laying the ground for tolerogenic environment. Other immunomodulatory abilities already attributed to MSCs are inhibition of activation and proliferation of dendritic cells [4], as well as blocking the proliferation of natural killer (NK) cells, being both key actors of the innate immune response [3, 4, 6]. These effects are thought to be a consequence of soluble factors released by MSCs; however, the precise mechanisms of stimulation, production of active agents and their secretion by MSCs are still not fully understood. MSCs release soluble factors with major impact on the regulation of the immune system including hepatocyte growth factor (HGF), transforming growth factor-β1 (TGF-β1), prostaglandin E2 (PGE2) and interleukin-10 (IL-10) among others [5, 7]. The non-classic MHC I molecule, HLA-G, expressed in the surface of MSCs, has also been described as a mediator of their immunosuppressive effects [3, 6, 8]. Based on their immunomodulatory properties, the use of MSCs has been thought to be an excellent therapeutic alternative for immune-mediated diseases.
In contrast to induced pluripotent stem cells (iPSCs), MSCs became good candidates for cell regeneration therapy both due to their easy accessibility and their lack of tumorigenic activity, making them a good therapeutic alternative for immune-mediated diseases. However, one of the main reasons why MSCs regenerative therapies have not been successful so far is because of the low rate of cell implantation [9, 10]. That is why, in the past few years, researchers have tried to encounter other candidates for cell therapy.
In 2010, a subset of pluripotent stem cells was described and named multilineage-differentiating stress-enduring (Muse) cells, isolated from adult tissues [11]. Currently, Muse cells can be isolated from mesenchymal tissues mainly skin, bone marrow and adipose tissue [11, 12]. These conspicuous stem cells have been characterized for their SSEA-3 expression (a well-known surface marker for human embryonic stem cells). They also express pluripotency markers, such as octamer-binding transcription factor 3/4 (Oct3/4), sex-determining region Y-box 2 (Sox-2) and Nanog [11,12,13]. Furthermore, Muse cells have high capacity of migrating to injured areas, regenerating damage tissues and fostering function recovery.
Remarkably, Muse cells express low levels of HLA-DR, a major histocompatibility class (MHC) II molecule, suggesting the potential use of Muse cells for allogeneic transplantation. Muse cells telomerase activity is very low, and it has been proven their incapacity of undergoing teratogenesis in vivo [11, 13,14,15,16]. Based on all these properties, Muse cells are ideal candidates for tissue regeneration and cell therapy.
6.2 Diabetes
During the last two decades, several attempts have been made to employ the administration of MSCs for the treatment of diabetes. Diabetes is a highly prevalent endocrine-metabolic disease with a constant growing rate, affecting nearly half a billion people worldwide. It is characterized by hyperglycaemia as a result of whether a lack of insulin production in the pancreas (type 1 diabetes) or peripheral insulin resistance and insufficient insulin production (type 2 diabetes), in addition to genetic and environmental components. Type 1 and type 2 diabetes are distinguished by their etiopathogenesis, where the former is characterized by an autoimmune-mediated destruction of β cells in the pancreatic islets, while type 2 diabetes comes out as a consequence of insulin resistance, which leads to β cells inability to cope with high blood glucose and, eventually, their death by apoptosis [17].
In type 1 diabetic patients, autoantigens produced by damaged β cells (regardless of the primary stimulus) are recognized by antigen-presenting cells (APCs) and activate pro-inflammatory responses. In this context, MSCs and Muse cells may either modulate the action of the uncontrolled immune system or protect pancreatic β cells from death.
Dendritic cells and macrophages belong to the first line of immune cells infiltrating pancreatic islets in type 1 diabetes, followed by B and T lymphocytes. At early disease stages, benign T helper type 2 (Th2) cells can be found within islets, followed by a wave of Th1 lymphocytes generating a pro-inflammatory environment [18]. Later on, cytotoxic T lymphocytes (CD8+) contribute to the pathogenesis establishing direct contact and damaging insulin-producing cells through the release of perforin and granzyme molecules, among other agents [17, 19]. Also, β cell damage is promoted by pro-inflammatory cytokines released by macrophages and activated T lymphocytes, such as IL-1β, TNF-α and IFN-γ [20, 21], and it is further accelerated by superoxide production [17]. These pro-inflammatory stimuli, together with radical oxygen and nitrogen species generated by the intracellular oxidative stress of β cells, will lead to their demise and inability of the remaining β cells to cope appropriately with blood glucose levels.
The pathophysiological mechanisms of type 2 diabetes differ from type 1 diabetes, although recent evidence demonstrated the participation of selected components of the immune system as well [19]. Autoreactive CD4+ T cells have been found in the blood of type 2 diabetic patients, and their cytokine production (particularly IFN-γ and IL-10) is similar to that observed in type 1 diabetic subjects. Insulin resistance in type 2 diabetes determines higher blood glucose levels which, combined with reduced β cell function, are translated into poor insulin output and subsequent dysregulated glucose homeostasis [22].
The nonobese diabetic (NOD) mouse is frequently employed as a spontaneous model of type 1 diabetes, in which the immune system plays an essential role in the pathogenesis of the disease. This mouse strain is characterized by multiple defects in regulatory pathways of the immune system [23]. Infiltration of leukocytes in the pancreatic islets – insulitis – can be observed as early as 4 weeks of age in females, and incidence of diabetes commonly occurs in 60–80% of 30-week-old female NOD mice. In this chapter, we describe the effects of adipose tissue-derived Muse cells modulating diabetogenic T lymphocytes and their beneficial administration in diabetic NOD mice.
6.3 Immunomodulatory Action of Muse-AT Cells
Muse cells are generally obtained by cell sorting based on pluripotent surface marker SSEA-3 expression [11]. However, we obtained Muse cell-enriched fraction from human lipoaspirates (Muse-AT cells) by simple, fast and affordable procedure, based on the original method reported by Heneidi et al. [12]. The lipoaspirate was treated with severe cellular stress conditions combining long-term collagenase incubation, lack of nutrients, low temperature and hypoxia and resulted in the enrichment stage-specific embryonic antigen-3 (SSEA-3)-positive cells for up to ~60% of [13].
Recent reports have described the immunoregulatory capacity of Muse-AT cells. The fact that Muse-AT cells isolated from adipose tissue secrete high levels of TGF-β1 is a major milestone supporting the immunomodulatory properties of these conspicuous stem cells [13]. TGF-β1 is a cytokine which plays a critical role in inflammation and other biological processes, depending on the microenvironment surrounding damaged tissues. We demonstrated that the expression level of TGF-β1 secreted by Muse-AT cells in culture increases spontaneously over time, reaching the highest levels between 5 and 10 days, probably as a response to the stringent stress culture conditions triggered by clustering formation in suspension culture.
The immunomodulatory capacity of Muse-AT cells is mainly mediated by secreted TGF-β1 [13]. T cells and macrophages secrete pro-inflammatory cytokines upon stimulation in vitro. Pro-inflammatory IFN-γ and TNF-α secreted by T cells and macrophages, respectively, boost the immune response. To investigate whether Muse-AT cells might influence the response of macrophages, we first employed the mouse macrophage cell line RAW 264.7. LPS activates and dramatically induces the secretion of TNF-α by RAW264.7 cells [24]. Muse-AT cells co-cultured with RAW 264.7 macrophages significantly reduced TNF-α secretion upon LPS stimulation. In addition, using a transwell co-culture system to find out whether soluble factors were the mediators of the observed inhibition, we discovered a significant decrease of TNF-α production by RAW264.7 cells upon LPS stimulation. These results indicate that soluble mediators secreted by Muse-AT cells are, in part, responsible for their immunomodulatory effects. Similarly, Muse-AT cell conditioned-media significantly reduced TNF-α secretion by LPS-stimulated RAW264.7 cells. We could also confirm the presence of TGF-β1 in Muse-AT cell conditioned-media as the one responsible for the observed effects on RAW 264.7 cells. Co-culture experiments were performed in the presence of SB-431542 (SB), a small molecule inhibitor that blocks TGF-β1 action. Under these circumstances, the inhibitory effect of Muse-AT cell conditioned-media was reverted, indicating that TGF-β1 plays a critical role as a mediator of Muse-AT cell immunomodulation. The same results were obtained when a more reliable source of macrophages was used. Indeed, Muse-AT cell conditioned-media reduced TNF-α secretion by LPS-stimulated freshly isolated murine macrophages, and the incorporation of SB into the media restored TNF-α secretion.
We then explored the ability of Muse-AT cells on T-lymphocyte responses. For this purpose, an in vitro antigen-specific T-lymphocyte assay was employed. NOD BDC2.5 CD4+ T cells specifically recognize a chromogranin-A peptide in the context of major histocompatibility class II complex (H-2 g7) of the NOD mice. BDC2.5 CD4+ T lymphocytes mainly differentiate into a Th1 phenotype secreting high amounts of pro-inflammatory cytokines, e.g. IFN-γ, upon antigen stimulation and have been extensively characterized regarding pathogenicity in autoimmune diabetes [25]. Thus, BDC2.5 CD4+ T cells responded with a high secretion of INF-γ upon antigen challenge [26, 27]. Muse-AT cell conditioned-media diminished IFN-γ secretion by antigen-stimulated BDC2.5 CD4+ T lymphocytes in a dose-dependent manner. Interestingly, conditioned-media from Muse-AT cells generated more efficient results in blocking INF-γ secretion when compared to conditioned-media obtained from culturing MSCs isolated from adipose tissue. When comparing TGF-β1 expression from cells isolated from a single individual, Muse-AT cells express higher levels than adipose MSCs, suggesting this cytokine may be responsible for the observed immune downregulating effect.
To further confirm whether the immune-regulatory potency exerted by Muse-AT cells on T cells might depend on their TGF-β1 expression levels, we blocked its signalling pathway using SB. When SB was applied to T cell cultures in the presence of Muse-AT cell conditioned-media, the secretion of IFN-γ by antigen-specific stimulated BDC2.5 CD4+ T lymphocytes was restored. Similar results were observed when a neutralizing anti-TGF-β1 antibody was added. These results confirmed the role of TGF-β1 as a key mediator of Muse-AT immunomodulatory activities in macrophages and T lymphocytes. In addition, we discovered upregulation of the classic anti-inflammatory IL-10 in the presence of Muse-AT cell conditioned-media in BDC2.5 CD4+ T-lymphocyte cultures [13].
6.4 Mechanistic Insights into Muse-AT Cells Activity
Based on all the results described above, we analysed the TGF-β1 signalling pathway of Muse-AT cells. Analysing several preparations of human Muse-AT cells, we have found that these cells express TGF-βII receptor, the cognate receptor for TGF-β1, on their surface membrane (Gimeno et al. unpublished), suggesting that this cytokine may promote autocrine/paracrine effects on the cells. What could be the role of TGF-β1 signalling in Muse-AT cells? This pleiotropic cytokine has been proposed as a stemness regulator of haematopoietic stem cells (HSCs); interestingly, these cells require stimulation with activin-like kinase 5 (TGF-β type I receptor) ligands to maintain a quiescent state within the bone marrow niche. In accordance to this, we observed that increments of TGF-β1 levels in Muse-AT cell clusters also matched with very low proliferation cell activity, while very low TGF-β1 levels were observed in highly proliferative ASCs. Thus, our observations led us to speculate that TGF-β1 autocrine/paracrine loop might help maintain Muse-AT cells at low proliferative rate [11]. Freshly isolated Muse-AT cells express TGF-βII-receptor, suggesting that they might show an early response to TGF-β1 ligands (see Fig. 6.1). Regarding this, Ylöstalo et al. proposed that aggregation of MSCs into spheroids induces a type of cellular stress that results in intracellular signalling leading to upregulation of anti-inflammatory effectors [28]. In vivo, activation might occur by the action of soluble factors released from injured tissues [29]. Accordingly, we found that Muse-AT cells spontaneously expressed high levels of TGF-β1 when cultured in non-adherent conditions (e.g. after 5–10 days). Cell aggregation might trigger this expression. Furthermore, when cells are transplanted and reach damaged tissues, it can be expected to find low levels of TGF-β1 in the microenvironment, which in turn will allow cell differentiation and tissue repair.
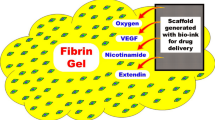
Schematic diagram illustrating the agents secreted by Muse-AT cells, their impact on immune cells response and possible therapeutic effects. Secreted-TGF-β1 by Muse-AT cells binds to its cognate receptor (TβR I/II) on T lymphocytes and macrophages. A putative intracellular TGF-β1 signalling pathway involves the expression of phosphorylated-SMAD proteins regulating the secretion of indicated cytokines. Also, putative action of biologics in indicated diseases is represented with “?”. X represents unknown factors. T reg T regulatory lymphocytes, MΦ macrophages
TGF-β binds to its specific receptor initiating intracellular signalling cascades and activating several phosphorylated mediators. Among them, SMAD2 has been described as an important mediator of the TGF-β1 anti-inflammatory pathway [30,31,32]. We analysed phosphorylated SMAD2 (pSMAD2) in T lymphocytes treated with Muse-AT cells conditioned-media. For this purpose, we employed BDC2.5 CD4+ T lymphocytes, as described [25, 27]. When BDC2.5 CD4+ T lymphocytes were cultured in Muse-AT cell conditioned-media, pSMAD2 levels increased in an antigen-specific dependent manner evaluated by Western blot [13] (see Fig. 6.1).
Upon antigen stimulation, naïve CD4+ T lymphocytes have the ability to differentiate into several Th effector subsets. NOD BDC2.5 CD4+ T cells have a marked Th1 bias [25]. Surprisingly, the presence of Muse-AT cells conditioned-media in antigen-stimulated BDC2.5 CD4+ T cells augmented the secretion and expression of IL-10 and its mRNA, respectively. Therefore, Muse-AT cells change the balance between the hallmark Th1 cytokine (IFN-γ) and regulatory IL-10 in T lymphocytes.
To further evaluate the intracellular mechanisms that govern T cells regulation by TGF-β1-mediated Muse-AT cells conditioned-media, we evaluated the master transcription factor TBX21 (T-box transcription factor, also known as T-bet) which governs Th1 differentiation and IFN-γ expression [33]. Our Western blot analysis indicated that Muse-AT cell conditioned-media reduced the expression of T-bet by antigen-specific stimulated BDC2.5 CD4+ T lymphocytes, suggesting that low levels of IFN-γ expression might be due, in part, to reduced synthesis of T-bet.
Are Muse-AT cells able to modify the expression of any other master transcription factor involved in T-lymphocyte differentiation? Although the levels of GATA-3 mRNA, a master transcription factor for Th2 differentiation, were not influenced by Muse-AT cell conditioned-media in BDC2.5 CD4+ T lymphocytes, we should not rule out the possibility that different diabetogenic clones may respond differentially to the conditioned-media. On the other hand, our preliminary data suggest the existence of other biologics expressed by Muse-AT cells which might influence immune responses, probably through direct action on T lymphocytes and macrophages. Therefore, a comprehensive knowledge of the microenvironment generated by Muse-AT cells is further needed.
TGF-β1 is also capable of maintaining the undifferentiated state of MSCs [34]. The Smad3 signalling pathway, mediated by the nuclear translocation of β-catenin, is required for the proliferation of MSCs. Complementary to this, it has been observed that osteoblast maturation is induced when endogenous TGF-β1 is inhibited [35]. Moreover, differentiation towards an osteogenic phenotype was inhibited in the presence of TGF-β1 in the medium, according to published results.
Muse cells seem to have a dual therapeutic effect: apart from their immunomodulatory activity, they can regenerate damaged tissue and restore its function, for example, inhibiting fibrosis. This is in accordance with the ability of Muse cells to produce matrix metalloprotease 9 (MMP-9), which has been proven to have an anti-inflammatory role [36]. High levels of expression of MMP-9 by Muse cells could explain their capacity to degrade and remove extracellular molecules, promoting fibrolysis or suppressing fibrosis and contributing to healing of the damaged tissue [37]. Once Muse cells reach the damaged tissue, they start differentiating into new cells for tissue repair. We can speculate that, during this process, a decrease in TGF-β1 production by Muse-AT cells would facilitate synthesis of metalloproteinases, therefore promoting fibrolysis. Furthermore, TGF-β1 also induces the expression of TIMP, a metalloproteinase inhibitor [38]; it would be interesting to analyse transcription levels of this protein in differentiated cells derived from Muse-AT cells and to compare TGF-β1 and MMP-9/TIMP levels. Crosstalk between TGF-β1 and metalloproteinases could explain the mechanism through which Muse-AT cells control fibrosis. It has also been described that TGF-β1 induces differentiation into myofibroblasts, therefore contributing to fibrosis [31]. It also induces the expression of fibronectin, a characteristic protein of the extracellular matrix (ECM) and mediator of cell proliferation [39, 40], preventing the degradation of ECM by regulating transcriptional levels of metalloproteinases and its inhibitor [38]. Taking all this into consideration, Muse-AT cells would act as promoters of fibrosis due to their expression of TGF-β1. However, treatment with Muse cells tested in murine models of liver fibrosis and nephropathy proved to be effective and showed no development of fibrosis [37, 41].
The complete molecular mechanism and cytokine interplay are not completely understood. If TGF-β1 secretion is decreased after differentiation of Muse cells, other biologics may be involved in its maintenance of the stem state. For example, inhibition of PGE2 synthesis in human umbilical cord mesenchymal stem cells (hUC-MSCs) co-cultured with human peripheral blood monocytes (PBMCs) resulted in the loss of stem cells properties, evaluated as proliferation of hPBMCs and secretion of IFN-γ [7]. Interestingly, PGE2 levels were increased when stimulated hPBMCs and hUC-MSCs were incubated together, indicating that a pro-inflammatory stimulus, possibly the secretion of IFN-γ and IL-1β, was needed to induce secretion of the PGE2 by MSCs. When NK cells were co-cultured with MSCs, a synergistic effect between indoleamine 2,3-dioxygenase (IDO) and PGE2 was observed to inhibit the cytotoxic phenotype of these immune cells [5]. Remarkably, as in the case of hPBMCs and hUC-MSCs, PGE2 secretion by MSCs was augmented when cultured together with NK cells but not when cultured alone.
IDO is a critical enzyme that catalyses the first and rate limiting step of tryptophan catabolism along the kynurenine pathway, which is involved in immune tolerance, preventing autoimmunity or immunopathology that could result from uncontrolled and overreacting immune responses [42]. When IDO catalyses tryptophan, this essential amino acid is locally depleted, while its catabolites accumulate, including kynurenine and its derivatives. As a result, tryptophan shortage inhibits T-lymphocyte division [43], and accumulation of tryptophan catabolites induces T cell apoptosis and differentiation into regulatory T cells [44,45,46]. Muse cells were also reported to express IDO in the similar level to MSCs, indicating that the pro-inflammatory environment observed in autoimmune diseases may trigger IDO expression in Muse cells and contribute to the abrogation of reactive immune cells. This could be another mechanistic process explaining the immunosuppressive phenotype of Muse cells [41].
Not only soluble factors are involved in modulating the immune system. As it has been demonstrated [47], bone marrow stromal cells (BMSCs) suppress T-lymphocyte proliferation, and this inhibition is less effective when cells are cultured together but not allowed to have cell-to-cell contact (transwell system). Interaction between MSCs and leukocytes may require the expression of several leukocyte chemokines by the former, such as CXCL9, CXCL10 and CXCL11 [48]. In mice, VCAM-1 and ICAM-1 are some of the surface molecules expressed by MSCs, also participating in inhibition of T-lymphocyte proliferation.
Another mechanism that might contribute to the regeneration of the tissue is the ability of Muse cells to migrate to damaged tissue with high efficiency. This property enhances their potential use as regenerative and anti-inflammatory agents, since they act locally in the affected area. The CXCR4-SDF-1 axis is one of the pathways involved in homing of stem cells into the damaged tissue [49, 50], and it seems to be one that drives Muse cell migration. This axis was abrogated when cells were incubated with a CXCR4 antagonist, proving its participation in Muse cells migration in a model of liver fibrosis [37]. In addition to CXCR4-SDF-1 axis, recent study suggested that sphingosine-1-phosphate (S1P) is more specific migratory factor for Muse cells in acute myocardial infarction patients [51]. The next question that arouse from these observations was related to the fate of Muse cells once they have arrived in the damaged tissues. It has been proven that, when administered intravenously, MSCs can transmigrate through the endothelial barrier and reach the lesion site [52, 53]. This migration may be generated by a chemokine gradient released from the injured tissue.
In a mouse model of focal segmental glomerulosclerosis damaged kidney cells, Muse cells showed high efficacy of homing, tissue regeneration and function recovery. Interestingly, the renal tissue of the Muse cell-treated group showed significantly high levels of expression of IGF-1, VEGF-A, VEGF-B, VEGF-C, VEGF-D and EGF known factors that not only protect kidney cells from damage but also participate in the generation of new blood vessels, a desirable characteristic which may lengthen tissue survival [41]. Previous reports indicate that TGF-β1 is a recognized regulator of angiogenesis, both during developmental stages and pathophysiological conditions [54, 55]. Binding of TGF-β1 to its type II receptor (TβRII) recruits type I receptors termed activin receptor-like kinase (ALKs). Pro-angiogenic responses in endothelial cells are elicited by downstream phosphorylation of Smad 1/5/8. Exploring this signalling pathway promoted by Muse cells could uncover new properties related to neovascularization and open new horizons for cell therapy.
6.5 Muse-AT Cells as Drivers of Diabetes Improvement
Strategies aim to preserve β cell function in type 1 diabetes, improve glycaemic control and decrease microvascular complications and hypoglycaemic events [56]. Despite intensive efforts, several clinical attempts have failed to preserve residual β cell mass for long periods of time, and progressive loss of β cells is ineluctable in most cases of type 1 diabetes. MSCs contribute to tissue repair and have demonstrated potential capacity against autoimmunity development [57]. For example, MSCs are capable of (i) suppressing antigen- or alloantigen-challenged T cell proliferation and (ii) upregulating the activity and number of T reg cells [58, 59]. This immunomodulatory activity is commonly associated to a decrease in inflammatory cytokine production [60]. Several agents produced by MSCs have been described as mediators of immunomodulation including heme oxygenase-1 (HO-1), IDO, MMPs and nitric oxide (NO). In this regard, infusion of bone marrow MSCs improves β cell function in diabetic NOD mice and even in patients [61].
A step forward in the characterization of Muse-AT cells would be to determine whether the immunomodulatory properties observed in vitro might translate into therapeutic benefits, reducing the incidence and/or ameliorating diabetes in mice. As stated earlier in this chapter, type 1 diabetes is characterized by a dysregulated immune system contributing to disease progression. Therefore, our findings regarding the ability of Muse-AT cells to down-regulate diabetogenic BDC2.5 Th1 T lymphocytes encourage efforts to prove whether these cells have potential for diabetes treatment. Thus, if Muse-AT cells can abrogate the pro-inflammatory surge, a more suitable environment would be generated, and survival of insulin-producing cells within islets would be extended.
We tested this hypothesis employing overt diabetic NOD mice, as a model of spontaneous autoimmune diabetes. NOD mice were considered diabetic when spontaneously reached glycaemia levels above 250 mg/dl during two consecutive days. Diabetic animals were divided into two groups: (1) one of them received intraperitoneally a single injection of 1 × 106 Muse-AT cells, and (2) the control group was injected with the same volume of sterile PBS (100 μl). Our preliminary results indicated that glucose levels from the control group dramatically increased, reaching glycaemia >500 mg/dl after a week, while the Muse-AT cell group showed oscillating blood glucose levels between 202 and 500 mg/dl during the 7-week period of observation (Gimeno et al., unpublished). While body weight diminished abruptly (between 2 and 5 g) within the 2 weeks of follow-up in the control group, showing clear signs of cachexia, all mice belonging to the Muse-AT cell group maintained a stably body weight during 7-week post-treatment. These results suggest that Muse-AT cells may control the autoimmune process after onset of spontaneous diabetes. Current ongoing experiments in our laboratory aim to improve these observations by several means, including increasing the total number of injected Muse-AT cells, repeating the administration once a week during several weeks and/or changing the route of administration, e.g. i.v. Also, therapy targeting major players involved in the immune-mediated destruction of β cells, such as the use of sub-therapeutic doses of CD3 antibodies, in combination with Muse-AT cells would be an interesting approach to tackle autoimmune diabetes.
Once the in vivo experiment is optimized, it would be interesting to elucidate the mechanism by which Muse-AT cells improve glycaemic control in immune-mediated diabetes. In this regard, it would be possible that Muse cells can differentiate into insulin-producing cells in vivo. It has already been established that Muse cells are able to migrate to damaged liver and differentiate into hepatocytes in a model of murine liver fibrosis [37]. Therefore, migration of Muse cells damage islets might be possible to explore. In this scenario, the anti-inflammatory environment promoted by Muse-AT cell population could also protect β cells from immune-driven demise and, even more, nourish their functionality.
The prevalence of chronic wounds related to diabetes is a major focus of diabetes care and hospitalization, as many as one in four patients with diabetes develops diabetic foot ulcer [62]. Kinoshita et al. employed Muse cells in an experimental mice model of type 1 diabetes skin ulcers [63]. Skin ulcers generated in SCID mice suffering type 1 diabetes showed delayed wound healing compared with nondiabetic SCID mice. Interestingly, injection of Muse cells around the wound significantly accelerated wound healing. The mechanism by which Muse cells promotes wound healing remains to be elucidated. A possible explanation may be that the high amount of growth factors secreted by Muse cells, particularly under hypoxic conditions, might be responsible for their accelerated skin repair process.
6.6 Muse Cells: Source of Factors Involved in Cell Survival and Immunoregulation
Whether Muse-AT cells secrete soluble factors able to directly promote β cell proliferation and/or survival is a matter of interest. However, there is a lack of information so far. A microarray analysis study revealed the expression of growth factors such as PDGF-A, EGF and SDF-1 under hypoxic conditions; however, this study was limited to only one sample [63]. Researchers found secreted growth factors, including PDGF-BB, TGF-β, bFGF and TNF-α in large quantities, particularly under hypoxic conditions. EGF- and PDGF-R signalling contributes to β cell mass expansion during high-fat mass diet and pregnancy in mice [64] and controls age-dependent proliferation of β cells in mice and humans [65]. Growth factors secreted could explain, at least in part, the repair effect of Muse-AT cells regarding β cell damage during diabetes.
Recently, a comprehensive secretome study of Muse cells was reported. In brief, Muse cells secretome was enriched in biologics that might have potential in conferring stemness preservation, cell survival under stress conditions and immunomodulatory properties [66]. It is worth highlighting the expression by Muse cells of several 14-3-3 isoforms that have the capacity to inactivate pro-apoptotic BAD, proteins belonging to protein kinase A pathways with putative roles in autocrine/paracrine signalling and proteins involved in cellular proliferation and lipid metabolism, such as liver X receptor (LXR) and farnesoid X receptor (FXR) with multiple metabolic roles. Lastly, some components of the complement system are expressed by Muse cells, among other proteins with immune-associated activities, such as alpha-2 macroglobulin and pregnancy zone protein, together with the expression of large number of interleukins and factors involved in the regulation of extracellular matrix remodelling with recognized immune functions [66]. All these biologics are worth investigating to further characterize Muse and Muse-AT cells and their therapeutic potential.
References
Yañez R, Lamana ML, García-Castro J, Colmenero I, Ramírez M, Bueren JA (2006) Adipose tissue-derived mesenchymal stem cells have in vivo immunosuppressive properties applicable for the control of the graft-versus-host disease. Stem Cells 24:2582–2591
Le Blanc K, Rasmusson I, Sundberg B, Götherström C, Hassan M, Uzunel M, Ringdén O (2004) Treatment of severe acute graft-versus-host disease with third party haploidentical mesenchymal stem cells. Lancet 363:1439–1441
Selmani Z, Naji A, Zidi I, Favier B, Gaiffe E, Obert L, Borg C, Saas P, Tiberghien P, Rouas-Freiss N et al (2008) Human leukocyte antigen-G5 secretion by human mesenchymal stem cells is required to suppress T lymphocyte and natural killer function and to induce CD4+CD25highFOXP3+ regulatory T cells. Stem Cells 26:212–222
Ramasamy R, Fazekasova H, Lam EW-F, Soeiro I, Lombardi G, Dazzi F (2007) Mesenchymal stem cells inhibit dendritic cell differentiation and function by preventing entry into the cell cycle. Transplantation 83:71–76
Spaggiari GM, Capobianco A, Abdelrazik H, Becchetti F, Mingari MC, Moretta L (2008) Mesenchymal stem cells inhibit natural killer-cell proliferation, cytotoxicity, and cytokine production: role of indoleamine 2,3-dioxygenase and prostaglandin E2. Blood 111(3):1327–1333
Yen BL, Chang CJ, Liu K-J, Chen YC, Hu H-I, Bai C-H, Yen M-L (2009) Brief report--human embryonic stem cell-derived mesenchymal progenitors possess strong immunosuppressive effects toward natural killer cells as well as T lymphocytes. Stem Cells 27:451–456
Chen K, Wang D, Du WT, Han Z-B, Ren H, Chi Y, Yang SG, Zhu D, Bayard F, Han ZC (2010) Human umbilical cord mesenchymal stem cells hUC-MSCs exert immunosuppressive activities through a PGE2-dependent mechanism. Clin Immunol 135:448–458
Spaggiari GM, Capobianco A, Becchetti S, Mingari MC, Moretta L (2006) Mesenchymal stem cell-natural killer cell interactions: evidence that activated NK cells are capable of killing MSCs, whereas MSCs can inhibit IL-2-induced NK-cell proliferation. Blood 107:1484–1490
Hodgetts SI, Beilharz MW, Scalzo AA, Grounds MD (2000) Why do cultured transplanted myoblasts die in vivo? DNA quantification shows enhanced survival of donor male myoblasts in host mice depleted of CD4+ and CD8+ cells or Nk1.1+ cells. Cell Transplant 9:489–502
Mingliang R, Bo Z, Zhengguo W (2011) Stem cells for cardiac repair: status, mechanisms, and new strategies. Stem Cells Int 2011:1–8. https://doi.org/10.4061/2011/310928
Kuroda Y, Kitada M, Wakao S, Nishikawa K, Tanimura Y, Makinoshima H, Goda M, Akashi H, Inutsuka A, Niwa A et al (2010) Unique multipotent cells in adult human mesenchymal cell populations. Proc Natl Acad Sci 107:8639–8643
Heneidi S, Simerman AA, Keller E, Singh P, Li X, Dumesic DA, Chazenbalk G (2013) Awakened by cellular stress: isolation and characterization of a novel population of pluripotent stem cells derived from Hu-man adipose tissue. PLoS One 8:e64752
Gimeno ML, Fuertes F, Barcala Tabarrozzi AE, Attorressi AI, Cucchiani R, Corrales L, Oliveira TC, Sogayar MC, Labriola L, Dewey RA, Perone MJ (2017) Pluripotent nontumorigenic adipose tissue-derived Muse-AT cells have immunomodulatory capacity mediated by transforming growth factor-β1. Stem Cells Transl Med 6:161–173
Wakao S, Kitada M, Kuroda Y, Shigemoto T, Matsuse D, Akashi H, Tanimura Y, Tsuchiyama K, Kikuchi T, Goda M et al (2011) Multiline-age-differentiating stress-enduring (Muse-AT) cells are a primary source of induced pluripotent stem cells in human fibroblasts. Proc Natl Acad Sci 108:9875–9880
Simerman AA, Dumesic DA, Chazenbalk GD (2014) Pluripotent Muse-AT cells derived from human adipose tissue: a new perspective on regenerative medicine and cell therapy. Clin Transl Med 3:12
Ogura F, Wakao S, Kuroda Y, Tsuchiyama K, Bagheri M, Heneidi S, Chazenbalk G, Aiba S, Dezawa M (2014) Human adipose tissue possesses a unique population of pluripotent stem cells with nontumorigenic and low telomerase activities: potential implications in regenerative medicine. Stem Cells Dev 23:717–728
Burrack AL, Martino T, Fife BT (2017) T cell-mediated Beta cell destruction: autoimmunity and alloimmunity in the context of type 1 diabetes. Front Endocrinol 8:343. https://doi.org/10.3389/fendo.2017.00343
Rothe H, Hausmann A, Casteels K, Okamura H, Kurimoto M, Burkart V, Mathieu C, Kolb H (1999) IL-18 inhibits diabetes development in nonobese diabetic mice by counterregulation of Th1-dependent destructive insulitis. J Immunol 163:1230–1236
Sarikonda G, Pettus J, Phatak S, Sachithanantham S, Miller JF, Wesley JD, Cadag E, Chae J, Ganesan L, Mallios R, Edelman S, Peters B, von Herrath M (2013) CD8 T-cell reactivity to islet antigens is unique to type 1 while CD4 T-cell reactivity exists in both type 1 and type 2 diabetes. J Autoimmun 50:77–82. https://doi.org/10.1016/j.jaut.2013.12.003
Suarez-Pinzon WL, Rabinovitch A (2001) Approaches to type 1 diabetes prevention by intervention in cytokine immunoregulatory circuits. Int J Exp Diabetes Res 2(1):3–17
Lundh M, Bugliani M, Dahlby T, Chou DH, Wagner B, Ghiasi SM, De Tata V, Chen Z, Lund MN, Davies MJ, Marchetti P, Mandrup-Poulsen T (2017) The immunoproteasome is induced by cytokines and regulates apoptosis in human islets. J Endocrinol 233(3):369–379
Kahn SE, Cooper ME, Del Prato S (2014) Pathophysiology and treatment of type 2 diabetes: perspectives on the past, present, and future. Lancet 383(9922):1068–1083
Leiter EH, Schile A (2013) Genetic and pharmacologic models for type 1 diabetes. Curr Protoc Mouse Biol 3(1):9–19
Lichtman SN, Wang J, Lemasters JJ (1998) LPS receptor CD14 participates in release of TNF alpha in RAW 264.7 and peritoneal cells but not in Kupffer cells. Am J Phys 275(1 Pt 1):G39–G46
Stadinski BD, Delong T, Reisdorph N, Reisdorph R, Powell RL, Armstrong M, Piganelli JD, Barbour G, Bradley B, Crawford F, Marrack P, Mahata SK, Kappler JW, Haskins K (2010) Chromogranin a is an auto-antigen in type 1 diabetes. Nat Immunol 11:225–231
Judkowski V, Pinilla C, Schroder K, Tucker L, Sarvetnick N, Wilson DB (2001) Identification of MHC class II-restricted peptide ligands, including a glutamic acid decarboxylase 65 sequence, that stimulate diabetogenic T cells from transgenic BDC2.5 nonobese diabetic mice. J Immunol 166:908–917
Castro CN, Barcala Tabarrozzi AE, Winnewisser J, Gimeno ML, Antunica Noguerol M, Liberman AC, Paz DA, Dewey RA, Perone MJ (2014) Curcumin ameliorates autoimmune diabetes. Evidence in accelerated murine models of type 1 diabetes. Clin Exp Immunol 177:149–160
Ylöstalo JH, Bartosh TJ, Coble K, Prockop DJ (2012) Human mesenchymal stem/stromal cells cultured as spheroids are self-activated to produce prostaglandin E2 that directs stimulated macrophages into an anti-inflammatory phenotype. Stem Cells 30(10):2283–2296
Nemeth C, Nunnally M, Bitan Y, Nunnally S, Cook RI (2009) Between choice and chance: the role of human factors in acute care equipment decisions. J Patient Saf 5(2):114–121
Weiss A, Attisano L (2013) The TGF beta superfamily signalling pathway. Wiley Interdiscip Rev Dev Biol 2(1):47–63
Morikawa M, Derynck R, Miyazono K (2016) TGF-β and the TGF-β family: context-dependent roles in cell and tissue physiology. Cold Spring Harb Perspect Biol 8(5):a021873
Ayyaz A, Attisano L, Wrana JL (2017) Recent advances in understanding contextual TGFβ signalling. F1000Research 6:749
Szabo SJ, Kim ST, Costa GL, Zhang X, Fathman CG, Glimcher LH (2000) A novel transcription factor, T-bet, directs Th1 lineage commitment. Cell 100:655–669
Jian H, Shen X, Liu I, Semenov M, He X, Wang XF (2006) Smad3-dependent nuclear translocation of beta-catenin is required for TGF-beta1-induced proliferation of bone marrow-derived adult human mesenchymal stem cells. Genes Dev 20(6):666–674
Maeda S, Hayashi M, Komiya S, Imamura T, Miyazono K (2004) Endogenous TGF-beta signalling suppresses maturation of osteoblastic mesenchymal cells. EMBO J 23(3):552–563
Fingleton B (2017) Matrix metalloproteinases as regulators of inflammatory processes. Biochim Biophys Acta 1864(11 Pt A):2036–2042
Iseki M, Kushida Y, Wakao S, Akimoto T, Mizuma M, Motoi F, Asada R, Shimizu S, Unno M, Chazenbalk G, Dezawa M (2017) Human Muse-AT cells, nontumorigenic pluripotent-like stem cells, have liver regeneration capacity through specific homing and cell replacement in a mouse model of liver fibrosis. Cell Transplant 26:821–840
Edwards DR, Murphy G, Reynolds JJ, Whitham SE, Docherty AJ, Angel P, Heath JK (1987) Transforming growth factor beta modulates the expression of collagenase and metalloproteinase inhibitor. EMBO J 6(7):1899–1904
Ignotz RA, Massagué J (1986) Transforming growth factor-beta stimulates the expression of fibronectin and collagen and their incorporation into the extracellular matrix. J Biol Chem 261(9):4337–4345
Roberts AB, Sporn MB, Assoian RK, Smith JM, Roche NS, Wakefield LM, Heine UI, Liotta LA, Falanga V, Kehrl JH (1986) Transforming growth factor type beta: rapid induction of fibrosis and angiogenesis in vivo and stimulation of collagen formation in vitro. Proc Natl Acad Sci U S A 83(12):4167–4171
Uchida N, Kushida Y, Kitada M, Wakao S, Kumagai N, Kuroda Y, Kondo Y, Hirohara Y, Kure S, Chazenbalk G, Dezawa M (2017) Beneficial effects of systemically administered human Muse-AT cells in adriamycin nephropathy. J Am Soc Nephrol 28(10):2946–2960
van Baren N, Van den Eynde BJ (2015) Tryptophan-degrading enzymes in tumoral immune resistance. Front Immunol 6:34
Munn DH, Shafizadeh E, Attwood JT, Bondarey I, Pashine A, Mellor AL (1999) Inhibition of T cell proliferation by macrophage tryptophan catabolism. J Exp Med 189(9):1363–1372
Fallarino F, Grohmann U, Vacca C, Bianchi R, Orabona C, Spreca A, Fioretti MC, Puccetti P (2002) T cell apoptosis by tryptophan catabolism. Cell Death Differ 9(10):1069–1077
Terness P, Bauer TM, Röse L, Dufter C, Watzlik A, Simon H, Opelz G (2002) Inhibition of allogeneic T cell proliferation by indoleamine 2,3-dioxygenase-expressing dendritic cells: mediation of suppression by tryptophan metabolites. J Exp Med 196(4):447–457
Fallarino F, Grohmann U, You S, McGrath BC, Cavener DR, Vacca C, Orabona C, Bianchi R, Belladonna ML, Volpi C, Santamaria P, Fioretti MC, Puccetti P (2006) The combined effects of tryptophan starvation and tryptophan catabolites down-regulate T cell receptor zeta-chain and induce a regulatory phenotype in naive T cells. J Immunol 176(11):6752–6761
Di Nicola M, Carlo-Stella C, Magni M, Milanesi M, Longoni PD, Matteucci P, Grisanti S, Gianni AM (2002) Human bone marrow stromal cells suppress T-lymphocyte proliferation induced by cellular or nonspecific mitogenic stimuli. Blood 99(10):3838–3843
Haddad R, Saldanha-Araujo F (2014) Mechanisms of T-cell immuno-suppression by mesenchymal stromal cells: what do we know so far? Biomed Res Int 2014:1–14. https://doi.org/10.1155/2014/216806
Kucia M, Jankowski K, Reca R, Wysoczynski M, Bandura L, Allendorf DJ, Zhang J, Ratajczak J, Ratajczak MZ (2004) CXCR4-SDF-1 signalling, locomotion, chemotaxis and adhesion. J Mol Histol 35(3):233–245
Hirbe AC, Morgan EA, Weilbaecher KN (2010) The CXCR4/SDF-1 chemokine axis: a potential therapeutic target for bone metastases? Curr Pharm Des 16(11):1284–1290
Tanaka T, Nishigaki K, Minatoguchi S, Nawa T, Yamada Y, Kanamori H, Mikami A, Ushikoshi H, Kawasaki M, Dezawa M, Minatoguchi S (2017) Mobilized Muse-AT cells after acute myocardial infarction predict cardiac function and remodelling in the chronic phase. Circ J 82(2):561–571
Nitzsche F, Müller C, Lukomska B, Jolkkonen J, Deten A, Boltze J (2017) Concise review: MSC adhesion cascade-insights into homing and transendothelial migration. Stem Cells 35(6):1446–1460
Bayo J, Marrodán M, Aquino JB, Silva M, García MG, Mazzolini G (2014) The therapeutic potential of bone marrow-derived mesenchymal stromal cells on hepatocellular carcinoma. Liver Int 34(3):330–342
Zhao M, Hu Y, Jin J, Yu Y, Zhang S, Cao J, Zhai Y, Wei R, Shou J, Cai W, Liu S, Yang X, Xu GT, Yang J, Corry DB, Su SB, Liu X, Yang T (2017) Interleukin 37 promotes angiogenesis through TGF-β signalling. Sci Rep 7(1):6113
Pardali E, Goumans MJ, ten Dijke P (2010) Signalling by members of the TGF-beta family in vascular morphogenesis and disease. Trends Cell Biol 20:556–567
Bonfanti R, Bazzigaluppi E, Calori G, Riva MC, Viscardi M, Bognetti E, Meschi F, Bosi E, Chiumello G, Bonifacio E (1998) Parameters associated with residual insulin secretion during the first year of disease in children and adolescents with type 1 diabetes mellitus. Diabet Med 15(10):844–850
Abdi R, Fiorina P, Adra CN, Atkinson M, Sayegh MH (2008) Immunomodulation by mesenchymal stem cells: a potential therapeutic strategy for type 1 diabetes. Diabetes 57(7):1759–1767
Di Ianni M, Del Papa B, De Ioanni M, Moretti L, Bonifacio E, Cecchini D, Sportoletti P, Falzetti F, Tabilio A (2008) Mesenchymal cells recruit and regulate T regulatory cells. Exp Hematol 36(3):309–318
Ghannam S, Bouffi C, Djouad F, Jorgensen C, Noël D (2010) Immuno-suppression by mesenchymal stem cells: mechanisms and clinical applications. Stem Cell Res Ther 1(1):2
Oh W, Kim DS, Yang YS, Lee JK (2008) Immunological properties of umbilical cord blood-derived mesenchymal stromal cells. Cell Immunol 251(2):116–123
Li L, Hui H, Jia X, Zhang J, Liu Y, Xu Q, Zhu D (2016) Infusion with human bone marrow-derived mesenchymal stem cells improves β-cell function in patients and nonobese mice with severe diabetes. Sci Rep 6:37894
International Diabetes Federation (2017) International diabetes federation atlas, 7th edn. Brussels, Belgium
Kinoshita K, Kuno S, Ishimine H, Aoi N, Mineda K, Kato H, Doi K, Kanayama K, Feng J, Mashiko T, Kurisaki A, Yoshimura K (2015) Therapeutic potential of adipose-derived SSEA-3-positive Muse-AT cells for treating diabetic skin ulcers. Stem Cells Transl Med 4(2):146–155
Hakonen E, Ustinov J, Mathijs I, Palgi J, Bouwens L, Miettinen PJ, Otonkoski T (2011) Epidermal growth factor (EGF)-receptor signalling is needed for murine beta cell mass expansion in response to high-fat diet and pregnancy but not after pancreatic duct ligation. Diabetologia 54(7):1735–1743
Chen H, Gu X, Liu Y, Wang J, Wirt SE, Bottino R, Schorle H, Sage J, Kim SK (2011) PDGF signalling controls age-dependent proliferation in pancreatic β-cells. Nature 478(7369):349–355
Alessio N, Özcan S, Tatsumi K, Murat A, Peluso G, Dezawa M, Galderisi U (2017) The secretome of MUSE-AT cells contains factors that may play a role in regulation of stemness, apoptosis and immunomodulation. Cell Cycle 16(1):33–44
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Japan KK, part of Springer Nature
About this chapter
Cite this chapter
Perone, M.J., Gimeno, M.L., Fuertes, F. (2018). Immunomodulatory Properties and Potential Therapeutic Benefits of Muse Cells Administration in Diabetes. In: Dezawa, M. (eds) Muse Cells. Advances in Experimental Medicine and Biology, vol 1103. Springer, Tokyo. https://doi.org/10.1007/978-4-431-56847-6_6
Download citation
DOI: https://doi.org/10.1007/978-4-431-56847-6_6
Published:
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-56845-2
Online ISBN: 978-4-431-56847-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)