Abstract
The banking of testicular tissue before highly gonadotoxic treatment is a prerequisite for the preservation of fertility in pre-pubertal boys not yet producing sperm. The aim of the current study is to evaluate the impact of a soaking temperature performed at −7 °C, −8 °C or −9 °C on the ability of frozen-thawed mouse spermatogonial stem cells (SSCs) to generate haploid germ cells after in vitro maturation. Testes of 6.5-day-old post-partum CD-1 mice were cryopreserved by using a controlled slow freezing protocol with soaking at −7 °C, −8 °C or −9 °C. Frozen-thawed pre-pubertal testicular tissues were cultured in vitro on agarose gel for 30 days. Histological evaluations were performed and flagellated late spermatids were counted after mechanical dissection of the cultured tissues. The differentiation of frozen SSCs into elongated spermatids was more efficient after treatment at −9 °C than at −7 °C and −8 °C. After dissection, flagellated late spermatids were observed by using Shorr staining. The number of flagellated late spermatids was significantly decreased after slow freezing when compared with a fresh tissue control. Therefore, the soaking temperature during slow freezing of pre-pubertal mouse testicular tissue might positively influence the course of in vitro spermatogenesis. Our slow freezing protocol with a soaking temperature at −9 °C was the optimal condition in terms of the achievement of in vitro spermatogenesis with a higher production of elongated spermatids, although the effectiveness of the maturation process was reduced compared with the fresh tissue control.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The survival of paediatric cancer patients has considerably improved within the last few decades because of the remarkable progress in diagnostic and treatment strategies (for a review, see Wyns et al. 2010). Anti-neoplastic treatments have, unfortunately, deleterious effects on gonad function with the spermatogonial stem cells (SSCs) being the most sensitive cells in the pre-pubertal testis (for a review, see Wyns et al. 2010). The freezing of sperm has been proposed in young adult males and adolescents for several years (Loren et al. 2013). However, pre-pubertal boys cannot benefit from the banking of sperm and, thus, the freezing of testicular tissue prior to highly gonadotoxic treatment is the only potential strategy for the preservation of their fertility, even though this procedure remains under investigation (Loren et al. 2013). Indeed, the cryopreservation of testicular tissue pieces instead of cell suspensions has the advantage of maintaining cell-to-cell interactions between Sertoli and germ cells and, therefore, of preserving the stem cell niche necessary for the survival and subsequent differentiation of SSCs (Ogawa et al. 2005). Currently, no standardized protocol has been established for the freezing of testicular tissue in terms of optimal cryopreservation techniques or for fertility restoration procedures to allow the generation of sperm cells from the frozen SSCs (Pacchiarotti et al. 2013). Hence, an optimized cryopreservation protocol of testicular tissue is necessary to increase the chances of frozen-thawed SSCs successfully passing through complete spermatogenesis.
Frozen-thawed SSCs must undergo a maturation process to restore sperm production; this can be achieved after (1) in vivo transplantation of SSCs into seminiferous tubules or testicular grafting into sterile patients after recovery (Wyns et al. 2010; Goossens et al. 2013) and (2) in vitro culture of isolated SSCs or organotypic culture of testicular fragments before or after testicular tissue freezing (Reuter et al. 2012; Song and Wilkinson 2012). In animal models, encouraging data have been reported for the restoration of complete spermatogenesis after in vivo transplantation of frozen SSCs into host testes, namely after orthotopic or heterotopic allografts or xenografts of testicular fragments from mammals, human and non-human primates into immunodeficient nude mice (for a review, see Arregui and Dobrinski 2014). However, autologous germ cell transplantation or testicular tissue grafting expose the cured patient to the risk of the re-introduction of malignant cells (Hou et al. 2007), whereas xenografts run the risk of zoonosis development (Fishman et al. 2012).
In order to avoid these concerns, the in vitro maturation of frozen-thawed pre-pubertal testicular tissue might represent an alternative method to restore fertility. Indeed, neonatal mouse testis, cryopreserved either by a non-controlled slow freezing or by a vitrification protocol, can generate spermatozoa after organotypic culture system by using agarose gel and supplementation of the medium with 10 % Knock-out Serum Replacement (KSR; Yokonishi et al. 2014). However, in vitro sperm production remains a rare event. Our group has previously demonstrated that retinol (RE) at 10−6M is able to initiate spermatogenesis until the pachytene stage in fresh and frozen-thawed pre-pubertal mouse testicular tissues during a short-term culture period involving the use of polycarbonate membrane inserts (Travers et al. 2013). More recently, we improved the efficiency of in vitro spermatogenesis by adding RE at 10−6M into the culture medium in the agarose gel system (Arkoun et al. 2015). Indeed, RE increases not only round and elongated spermatid production but also sperm generation with a better maintenance of seminiferous tubule integrity after one wave of in vitro spermatogenesis (Arkoun et al. 2015). The course of the in vitro spermatogenesis depends upon the ability of the culture system and the medium used to maintain the germ cell microenvironment and, with frozen-thawed testicular tissue, on the quality and functionality of the tissue after thawing.
Several slow freezing protocols have been previously examined in order to determine the best cryopreservation strategy for the mammalian testis. The type of cryoprotective agents (CPA), the cooling rate and the soaking temperature are known parameters that influence the freezing process. Among permeant CPA, previous studies have shown that dimethylsulfoxide (DMSO) ensures a better cryoprotection of testicular tissue than 1,2-propanediol, probably because of its low molecular weight and high penetration, in mouse (Milazzo et al. 2008, 2010; Yildiz et al. 2013; Yokonishi et al. 2014) or human (Keros et al. 2005) testicular tissue (Table 1). In addition, glycerol provides lower protection than DMSO for the pre-pubertal rat (Unni et al. 2012) or adult human testicular fragments (Keros et al. 2005). With regard to the rate of freezing, controlled slow freezing appears to be the most reported protocol for the cryopreservation of pre-pubertal mouse (Milazzo et al. 2010; Yildiz et al. 2013; Travers et al. 2013) or human testicular tissue (Keros et al. 2007; Wyns et al. 2008, 2011; Table 1). Indeed, the use of a controlled rate of freezing rather than an uncontrolled rate of freezing is well established as being a critical condition to maximize post-thaw cell viability. During the freezing process, ice undergoes uncontrolled growth and forms large ice crystals that alter cell membranes and organelles. However, controlled slow freezing procedures do not completely prevent intracellular ice crystal formation and consequently cellular damage. Therefore, in order to prevent intracellular ice crystal formation, the control of cell dehydration before temperatures at which intracellular ice nucleation occurs and consequently the selection of the best soaking temperature appears necessary (for a review, see Shaw and Jones 2003). However, the soaking temperature reported in the published data of controlled slow freezing protocols of testicular tissue vary but lie within a close temperature range, i.e., at −7 °C (Shinohara et al. 2002; Luetjens et al. 2008 and Curaba et al. 2011), −8 °C (Keros et al. 2007; Wyns et al. 2011; Baert et al. 2013) and −9 °C (Kvist et al. 2006; Milazzo et al. 2008, 2010; Dumont et al. 2015). A previous study of our group showed that a soaking temperature of −8 °C, rather than −7 °C or −9 °C, allows the proliferation of germ cells and their ability to initiate spermatogenesis in frozen-thawed pre-pubertal mouse testicular tissue (Travers et al. 2013). However, the culture period was limited to 9 days and the impact of the different soaking temperatures on in vitro spermatogenesis was only evaluated for the proliferation of spermatogonia and entry into the meiotic process as far as the pachytene stage.
To the best of our knowledge, no study has evaluated the effects of various soaking temperatures on the complete in vitro germ cell differentiation of frozen-thawed pre-pubertal mouse testicular tissue. Therefore, the aim of the current study was to evaluate the impact of soaking performed at −7 °C, −8 °C or −9 °C on the ability of frozen-thawed SSCs to generate haploid germ cells after in vitro maturation. We also explored several objective parameters after culture, notably, germ cell proliferation ability, seminiferous tubule growth, structural integrity of seminiferous epithelium and Leydig cell functional integrity via testosterone measurements.
Materials and methods
Animals and testis collection
All experiments were approved by the Regional Ethical Committee of Normandy for Animal Care and Use under licence N/23-11-12/46/11-15. CD-1 mice aged 6.5 days post-partum (dpp) were killed by decapitation (Charles River Breeding Laboratories, L’Arbresle, France). The testes were excised and rinsed in Leibovitz L-15 medium (Eurobio, Courtaboeuf, France). The tunica albuginea was removed by using sterile needles and the testes were then rinsed again in the medium mentioned above. For each litter, one testis was fixed in Bouin’s solution to ensure that the seminiferous cords contained no germ cells more advanced than spermatogonia (for 6.5-dpp mice).
Controlled slow freezing
The controlled slow freezing protocol used was as previously described (Travers et al. 2013). Briefly, each testis, weighing approximately 3 mg, was placed into a cryovial (Cryotube Vials, Nunc, Roskilde, Denmark) containing 1.5 ml cryoprotective medium that consisted of Leibovitz L-15 medium supplemented with 1.5 M DMSO (Sigma-Aldrich, Saint-Quentin Fallavier, France), 0.05 M sucrose (Sigma-Aldrich) and 10 % (v/v) fetal calf serum (FCS; Eurobio). Equilibration was performed at 4 °C for 30 min. The vials were cooled within a programmable freezer (Nicool Freezal, Marne La Vallée, France) at a rate of −2 °C/min from 5 °C until reaching the soaking temperature at −7 °C, −8 °C or −9 °C, stabilized for 8 min without seeding (Milazzo et al. 2008) and, then cooled at a rate of −0.3 °C/min to −40 °C and, finally, at −25 °C/min to −150 °C. Subsequently, the samples were directly plunged into and stored in liquid nitrogen at −196 °C (Electronic Supplementary Material, Fig. S1a).
After 1 month of cryostorage in liquid nitrogen, samples were thawed rapidly in a 37 °C water bath. Testicular tissues were then placed into several baths with a progressive dilution of CPA to avoid osmotic stress. Subsequently, the cryomedium was removed in a four-step procedure with 5 min for each step: (1) 1 M DMSO, 0.05 M sucrose, 10 % FCS; (2) 0.5 M DMSO, 0.05 M sucrose, 10 % FCS; (3) 0.05 M sucrose; (4) Leibovitz L-15 medium without CPA (Electronic Supplementary Material, Fig. S1b).
In vitro culture procedure
On the day before the start of each culture experiment, 1.5 % (w/v) agarose gels (A6013-10G, Sigma-Aldrich) were placed into small Petri dishes (Center-Well Organ Culture Dish-BDFalcon; BD Biosciences, Franklin Lakes, New Jersey, USA) and soaked overnight in a culture medium composed of α-minimum essential medium (α-MEM; Life Technologies, Carlsbad, Calif., USA), 10 % (v/v) KnockOut Serum Replacement (KSR; Life Technologies) and gentamycin (Sigma-Aldrich, Saint-Quentin Fallavier, France) at a final concentration of 5 μg/ml in a humidified incubator supplied with 5 % CO2 in air at 34 °C. On day 0 (D0) of the experiments, frozen-thawed testis was cut into four fragments and inserted into a pair of 1.5 % (w/v) agarose gels (A6013-10G, Sigma-Aldrich), each containing two tissue fragments (Electronic Supplementary Material, Fig. S1c). The culture medium was supplemented with RE at 10−6 M and changed every 3 days from D0 until D30 (Electronic Supplementary Material, Fig. S1d). For each soaking temperature and with fresh tissue being used as controls, four testes from mice of different litters were cultured with the same procedure as described above.
Histological analysis
For each testicular fragment, three sections (3 μm thick) obtained at intervals of 15 μm were evaluated via periodic acid-Schiff (PAS)-haemalun (RAL diagnostic, Martillac, France) staining to allow a global evaluation of germ cell differentiation and seminiferous tubule architecture. Slides were coded for blinded analysis by one technician and counts were performed by one observer not involved in the slide preparation. To assess the proportions of haploid spermatids in seminiferous tubules, the mean proportion of intratubular cells (Sertoli cells, spermatogonia, spermatocytes I, round spermatids and elongated spermatids) was determined in 30 cross-sectioned tubules (Arkoun et al. 2015).
The integrity and structural changes of seminiferous tubule sections of frozen-thawed and fresh testicular tissues were evaluated semi-quantitatively. The seminiferous epithelium was scored as previously described by Milazzo et al. (2008): (1) detachment of cells from the basement membrane was scored as 0 if absent, 2 if partial and 3 if total or observed in more than 75 % of the circumference; (2) gap formation and shrinkage were scored as 0 if absent, 1 if slight and 2 if more obvious. Therefore, the global score for each seminiferous epithelium section was between 0 and 5. For each specimen, the mean score obtained from 30 seminiferous tubule sections was used as the global score.
The seminiferous tubule area and intratubular cell density (number of intratubular cells/1000 μm2) were simultaneously assessed in 10 cross-sectioned tubules by using a digital imaging analysis system (LAS, Leica) connected to an inverted microscope (DM4000B, Leica). A cross-sectioned tubule was defined when a ratio of less than 1.5 was observed between the longest diameter of the tubule and the diameter perpendicular to it. Subsequently, the mean cellular density per tubule cross-section was determined.
Cellular death was determined after quantification of pyknotic nuclei, corresponding to necrosis, in 30 sectioned seminiferous tubules of each condition tested. A pyknotic nucleus was defined as being small, spherical and shrunken with highly condensed chromatin. The number of pyknotic nuclei per seminiferous tubule section was determined, after which the seminiferous tubules were classified as: not pyknotic (less than 10 % of pyknotic nuclei per tubule section), partially pyknotic (between 10 % and 90 % of pyknotic nuclei per tubule section) or totally pyknotic (more than 90 % of pyknotic nuclei per tubule section).
Immunohistochemistry
Germ cells in tissue sections (3 μm thick) were immunohistochemically identified by using Tra98 (for spermatogonia and leptotene/zygotene and pachytene spermatocytes I) and cAMP-responsive element modulator antibodies (CREM-1, for post-meiotic spermatids). Briefly, sections were deparaffinized, rehydrated in a graded ethanol series and incubated in 10 mM citrate (pH 6; Sigma-Aldrich) for 40 min at 96 °C. Hydrogen peroxide (Thermo Scientific, Mass., USA) was used to inactivate endogenous peroxidases during a 5-min treatment, followed by incubation with 5 % normal horse serum (Thermo Scientific) for 10 min at room temperature to prevent non-specific antibody binding. The slides were incubated with primary antibody, namely rat anti-Tra98 (Tra98; 1:50, Abcam) overnight at 4 °C or rabbit anti-CREM-1 (X-12; 1:50, Santa Cruz Biotechnology) for 60 min at room temperature. Negative controls were performed with rat pre-immune IgGs (SC-2026, Santa Cruz Biotechnology) or pre-immune rabbit IgGs (SC-2027, Santa Cruz Biotechnology) according to the primary antibody used. The washing steps following the primary antibody incubation were performed by using TRIS-buffered saline (TBS; Dako, Paris, France).
For the detection of Tra98, a secondary antibody (1:200; rabbit anti-rat IgGs/horseradish peroxidase [HRP], Dako) was used and sections were subsequently incubated with biotinylated tertiary antibody (1:200; biotinylated swine anti-rabbit IgG, Dako). CREM-1 was detected by using biotinylated goat anti-rabbit IgG (1:200, Santa Cruz Biotechnology). Positive staining was obtained by incubation with a streptavidin-HRP solution (Thermo Scientific) for 15 min followed by incubation with 3,3′-diaminobenzidine substrate (DAB, Thermo scientific) for 1–10 min. Finally, the nuclei were counterstained with haematoxylin (Dako). The proliferative ability of the intratubular cells was evaluated by using a proliferating cell nuclear antigen antibody (PCNA, Invitrogen, Carlsbad, Calif., USA) according to the manufacturer’s instructions. A negative control was performed with the same procedure but with a pre-immune biotinylated mouse IgG (SC-2762, Santa Cruz Biotechnology).
Flagellated late spermatids present in cell suspensions obtained after in vitro culture of frozen-thawed testicular fragments were identified by immunofluorescent staining of their flagella by using a monoclonal mouse anti-acetylated tubulin antibody (T6793, 1:100, Sigma; see “Enumeration of flagellated late spermatids”). A pre-immune mouse IgG (SC-2025, Santa Cruz Biotechnology) was also used as a control antibody with the same procedure. Subsequently, slides were incubated with a fluorescein-isothiocyanate-conjugated goat anti mouse IgG secondary antibody (F4143, 1:100, Sigma-Aldrich), mounted in medium containing 4′,6-diamidino-2-phenylindole (DAPI; Abbott, Chicago, Ill., USA) and analysed by using an epifluorescence microscope at ×600 magnification (BX61; Olympus, Tokyo, Japan).
Enumeration of flagellated late spermatids
Fresh and frozen-thawed explants (n = 4 for controls, n = 4 for each soaking temperature performed at −7 °C, −8 °C or −9 °C), obtained from 6.5-dpp mice of different litters, were cultured for 30 days. After culture, each group of explants was weighed, placed into a Petri dish (BD Biosciences) containing 500 μl α-MEM at 34 °C with 5 % CO2 and shredded with insulin syringes. Subsequently, 20 μl of each testicular cell suspension was observed under a light microscope at ×400 magnification (Laborlux, Leica) to count the flagellated spermatozoa. Thereafter, the remaining testicular cell suspension was centrifuged for 10 min at 600g at room temperature and the pellet was subjected to Shorr staining (Merck, Darmstadt, Germany).
Testosterone measurement
In vitro steroidogenesis was evaluated by measuring testosterone secretion into the medium under fresh and −9 °C conditions. Media samples stored at −20 °C after 7, 11, 18 and 30 days of culture were analysed by using a direct radioimmunoassay (testosterone kit [IM1087]; Immunotech Beckman-Coulter, Roissy, France). The samples were assayed in duplicate according to the manufacturer’s recommendations. The assay had a lower limit of sensitivity of 0.04 ng/ml with average intra- and inter-assay variations of 7.2 % and 10.7 %, respectively.
Statistical analysis
Statistical analysis was performed for all experiments by using the Friedman test for global comparisons, the Mann–Whitney test for unpaired rank comparisons or the Wilcoxon test for paired rank comparisons. The data are presented as the means ± SEM. A P-value below 0.05 was considered as statistically significant.
Results
Structural integrity of seminiferous epithelium is better maintained with a soaking temperature at −7 °C and −9 °C after in vitro culture of frozen-thawed pre-pubertal mouse testes
At D30 of culture, morphological alterations of the seminiferous epithelium corresponding notably to gap formation and shrinkage were observed under the various conditions tested (Fig. 1a-d). The lesion scores did not vary significantly between −7 °C and −9 °C (P = 0.24; Fig. 1e). However, the lesion score was significantly higher with a soaking temperature at −8 °C when compared with −7 °C (P = 0.01) or −9 °C (P = 0.02). In addition, compared with the fresh control, the lesion score was significantly increased at −8 °C (P = 0.01) but not at −7 °C (P = 0.1) or −9 °C (P = 0.1). The results of the soaking temperatures at −7 °C and −9 °C were similar to those of fresh tissue control, although the lesion score at −7 °C was less elevated.
Assessment of morphological alterations of seminiferous epithelium after in vitro culture (at day 30 [D30]) of frozen-thawed pre-pubertal (6.5 days post-partum [dpp]) mouse testicular tissue. a–d Histological evaluation of gap formation (vacuolization; green asterisks) in seminiferous tubules under the various conditions tested. Periodic acid-Schiff staining. Magnification ×1000. Bars 40 μm. e Global lesion scores corresponding to the sum of cell detachments from the basement membrane and gap formation in seminiferous tubules. Results are expressed as means ± standard error of mean (SEM); n = 4 mouse testes for each condition. *Statistically significant difference, P < 0.05 (D day)
Soaking temperature at −9 °C gives best match to fresh tissue control with regard to seminiferous tubule growth, intratubular cell density, germ/Sertoli cell ratio and cellular death per tubule section after in vitro culture (D30) of frozen-thawed pre-pubertal mouse testes
Regardless of the soaking temperatures tested, the seminiferous tubule area markedly increased during culture, as in the fresh tissue control (P = 0.031; Fig. 2a). At D30 of culture, the highest seminiferous tubule area was observed with a soaking temperature at −9 °C and was significantly higher when compared with −7 °C (8637.25 ± 457.69 μm2 vs. 6852.95 ± 141.48 μm2; P = 0.01), even though no statistical difference was apparent when compared with −8 °C (8637.25 ± 457.69 μm2 vs. 6874.58 ± 489.56 μm2; P = 0.057). Moreover, the seminiferous tubule area observed for −7 °C and −8 °C appeared less elevated compared with the fresh control (9016.50 ± 799.71), although no statistical differences were observed (P = 0.057, for both). The closest surface area to that of the fresh tissue control was obtained with a soaking temperature at −9 °C (P = 0.17).
Evaluation of seminiferous tubule growth by surface area and intratubular cell density (a, b), germ/Sertoli cell ratio (c–e) and cellular death (f, g) according to the soaking temperatures and tested at D30 of culture. Results were compared between the different soaking temperatures tested and between the soaking temperatures and fresh testicular tissue control. Data are expressed as means ± SEM; n = 4 mouse testes for each condition. Conditions that do not share a common letter are significantly different (a, b, g). *Statistically significant difference, P < 0.05
Whatever the soaking temperature tested, the intratubular cell density per tubule section decreased significantly during culture, as in the fresh tissue control (P = 0.031; Fig. 2b). At D30 of culture, the lowest cellular density was observed with a soaking temperature at −8 °C and was significantly lower when compared with −7 °C (3.98 ± 0.24 vs. 4.81 ± 0.14; P = 0.01) or −9 °C (3.98 ± 0.24 vs. 6.05 ± 0.90; P = 0.01). Intratubular cell density decreased significantly at −7 °C and −8 °C when compared with the fresh tissue condition (4.81 ± 0.14 vs. 6 ± 0.51; P = 0.02 and 3.98 ± 0.24 vs. 6 ± 0.51; P = 0.01, respectively). However, intratubular cell density following soaking at −9 °C was similar to that of the fresh tissue control and no statistical differences were obtained (P = 0.44).
With regard to the mean number of germ cells per seminiferous tubule section, no statistical differences were observed between the different soaking temperatures (P > 0.05; Fig. 2c). However, compared with the fresh tissue control, a significant decrease of the mean number of germ cells per tubule section was observed, irrespective of the soaking temperature used (P = 0.01). For the mean number of Sertoli cells per tubule section, the results were similar between all the conditions tested (P > 0.05; Fig. 2d). Concerning the ratio between germ cells and Sertoli cells, a significant decrease was obtained for the −8 °C soaking temperature when compared with −9 °C (1.36 ± 0.12 vs. 1.93 ± 0.13; P = 0.01; Fig. 2e). Furthermore, compared with the fresh tissue control, a significant decrease in the germ/Sertoli cell ratio was observed for the −7 °C and −8 °C conditions (2.48 ± 0.36 vs. 1.65 ± 0.11 and 2.48 ± 0.36 vs. 1.36 ± 0.12, respectively; P = 0.01). However, the ratio between germ cells and Sertoli cells did not vary significantly between the −9 °C soaking temperature and the fresh tissue control (P = 0.17).
The mean number of pyknotic nuclei per tubule section was similar between −7 °C and −8 °C (1.82 ± 0.31 vs. 2.47 ± 0.23; p = 0.1; Fig. 2f). However, a significant reduction of the mean number of pyknotic nuclei per tubule section was obtained with −9 °C (0.83 ± 0.24) or in the fresh tissue control (1.02 ± 0.19) when compared with −7 °C (1.82 ± 0.31) and −8 °C (2.47 ± 0.23; P = 0.01, for both), whereas no significant difference was observed between −9 °C and the fresh tissue control (0.83 ± 0.24 vs. 1.02 ± 0.19; P = 0.24). The lowest mean percentage with no pyknotic tubules was obtained at −7 °C and −8 °C and no significant difference was observed between them (85.83 ± 3.69 % vs. 80 ± 3.60 %; P = 0.17; Fig. 2g). However, the mean percentage of no pyknotic tubules was significantly higher for −9 °C when compared with −8 °C (94.17 ± 1.60 % vs. 80 ± 3.60 %; P = 0.01), even though no significant difference was observed when compared with the −7 °C treatment (94.17 ± 1.60 % vs. 85.83 ± 3.69 %; P = 0.057). The mean percentage of partially pyknotic tubules was significantly lower at −9 °C than at −8 °C (5.83 ± 1.60 % vs. 20 ± 3.60 %; P = 0.01), even though no significant difference was observed when compared with −7 °C (5.83 ± 1.60 % vs. 14.17 ± 3.69 %; P = 0.057). The mean percentage of partially pyknotic tubules was similar between −9 °C and the fresh tissue control (5.83 ± 1.60 % vs. 2.50 ± 1.60 %; P = 0.1). None of the seminiferous tubules were totally pyknotic, regardless of the culture conditions tested (Fig. 2g).
Soaking temperatures at −7 °C, −8 °C or −9 °C do not influence intratubular cell proliferation after in vitro culture (D30) of frozen-thawed pre-pubertal mouse testes
PCNA-positive cells were detected by immunohistochemistry at D30 of culture, irrespective of the soaking temperature tested, as in the fresh tissue control (Fig. 3a-d). Specific immunostaining was verified by using a pre-immune IgG as the negative control for each condition tested (Fig. 3e-h). After culture of frozen-thawed testicular tissues, the lowest rate of PCNA expression was observed with a soaking temperature at −8 °C, even though no statistical differences were observed when compared with −7 °C (P = 0.1) or −9 °C (P = 0.44; Fig. 3i). Moreover, no statistical differences were observed in terms of PCNA expression for the soaking temperatures tested when compared with the fresh tissue control (P > 0.05).
Intratubular cell proliferation assessed by proliferating cell nuclear antigen (PCNA) immunostaining after in vitro culture of frozen-thawed pre-pubertal CD-1 mouse testicular tissue. a–d Immunodetection of PCNA-positive cells in seminiferous tubule sections at D30 of culture under all conditions tested. e–h Negative control for each condition by using pre-immune biotinylated mouse immunoglobulin G (IgG). Magnification ×200. Bars 40 μm. i Intratubular cell proliferation rates assessed by PCNA staining. Results are represented as means ± SEM; n = 4 mouse testes for each condition. Results were compared between the different soaking temperatures tested and between the soaking temperatures and the fresh testicular tissue control cultured under the same conditions (NS not significant)
Soaking temperature at −9 °C is optimal condition for elongated spermatid production after in vitro culture of frozen-thawed pre-pubertal testicular tissues and remains best match to fresh tissue control
At D0 of culture, seminiferous tubules contained only spermatogonia as the most advanced germ cell stage regardless of the soaking temperature tested, as in the fresh tissue control (Fig. 4a-d). By D30 of culture, the meiotic process was underway, with round and elongated spermatid production after soaking at −7, −8 and −9 °C, as in the fresh tissue control (Fig. 4e-h). Tra98 immunostaining allowed an accurate distinction between germ cells (spermatogonia, leptotene/zygotene and early pachytene spermatocytes I) and Sertoli cells (Fig. 4i-l) for stereological analyses under all the conditions tested. In addition, CREM-1 allowed the genuine identification of round spermatids (Fig. 4m-p), with the elongated spermatids being counterstained with haematoxylin (Fig. 4o, p).
Assessment of in vitro maturation of frozen-thawed pre-pubertal CD-1 mouse testes at D30 of culture. a–h Histological evaluation of spermatogonial stem cell (SSC) differentiation according to the various soaking temperatures tested (HES haemalun eosin saffron, PAS periodic acid-Schiff). Fresh testicular tissues were used as controls before and after culture (d, h, respectively). At D0 of culture, seminiferous tubules contained only spermatogonia (a–d, green boxes) as the most advanced germ cell stage. At D30 of culture, round (black boxes) and elongated (blue boxes) spermatids were generated from frozen-thawed pre-pubertal SSCs, irrespective of the soaking temperature used (−7 °C, −8 °C and −9 °C), as in the fresh tissue control (e–h). Magnification ×500 (a–d), ×1000 (e–h, insets). Bars 40 μm (5 μm in insets). i–p Distinction of intratubular cell types by using immunohistological markers. Negative controls are shown right of each positive immunostaining tested (IgG immunoglobulin G). i–l Clear histological distinction between germ cells (spermatogonia, leptotene/zygotene and early pachytene spermatocytes I) and Sertoli cells (counterstained with haematoxylin) by using Tra98 immunostaining. m–p Immunodetection of round spermatids by using cAMP-responsive element modulator-1 (CREM-1) antibody (brown) for all the conditions tested (ES elongated spermatid, E-P early pachytene spermatocyte I, L/Z leptotene/zygotene spermatocyte I, L-P late pachytene spermatocyte, RS round spermatid, S Sertoli cell, Sg spermatogonia). Elongated spermatids are counterstained with haematoxylin (o, p, red boxes). Magnification ×1000. Bars 40 μm
At D30 of culture, stereological analyses showed that the lowest percentage of round spermatids per tubule section was obtained with soaking at −8 °C, although no significant differences were observed when compared with soaking at −7 °C (1.79 ± 0.76 % vs. 5.18 ± 1.40 %; P = 0.057) or −9 °C (1.79 ± 0.76 % vs. 5.39 ± 2.56 %; P = 0.1) (Fig. 5a). Moreover, compared with the fresh tissue control, the percentages of round spermatids per tubule section did not vary significantly in comparison with −7 °C and −9 °C soaking temperatures (9.10 ± 2.57 % vs. 5.18 ± 1.40 % and 9.10 ± 2.57 % vs. 5.39 ± 2.56 %, respectively; P = 0.1), whereas a significant decrease was observed under −8 °C conditions (9.10 ± 2.57 % vs. 1.79 ± 0.76 %; P = 0.01; Fig. 5a). A significant increase of the mean percentage of elongated spermatids per tubule section was observed with a soaking temperature at −9 °C when compared with −7 °C and −8 °C (1.26 ± 0.62 % vs. 0.14 ± 0.08 % and 1.26 ± 0.62 % vs. 0.12 ± 0.12 %, respectively; P = 0.01; Fig. 5b). In addition, compared with the fresh tissue control, the mean percentages of elongated spermatids per tubule at −7 °C and −8 °C were significantly lower (2.05 ± 0.65 % vs. 0.14 ± 0.08 % and 2.05 ± 0.65 % vs. 0.12 ± 0.12 %, respectively; P = 0.01). On the contrary, the mean percentage of elongated spermatids per tubule was similar between −9 °C and the fresh tissue control (1.26 ± 0.62 % vs. 2.05 ± 0.65 %; P = 0.17).
Evaluation of in vitro differentiation of frozen-thawed 6.5-dpp mouse SSCs into spermatids at D30 of culture according to the various soaking temperatures tested. a, b Mean proportion of round (a) and elongated (b) spermatids per seminiferous tubule section. c, d Mean proportion of seminiferous tubules containing round (c) or elongated spermatids (d). Data (%) are expressed as the mean percentage ± SEM; n = 4 mouse testes for each condition. Results are compared between −7 °C and −8 °C, between −7 °C and −9 °C, between −8 °C and −9 °C and between the different soaking temperatures and the fresh testicular tissue control. *Statistically significant difference; P < 0.05
On the other hand, when compared with the −8 °C condition, the mean percentage of tubules containing round spermatids appeared significantly higher at −7 °C (19.17 ± 4.38 % vs. 39.17 ± 3.70 %; P = 0.01) but not at −9 °C (19.17 ± 4.38 % vs. 40 ± 11.71 %; P = 0.17; Fig. 5c). In comparison with the fresh tissue control, −8 °C was the only condition that showed a significant decrease of the percentages of seminiferous tubules containing round spermatids (50.83 ± 3.70 % vs. 19.17 ± 4.38 %; P = 0.01). Although the −9 °C condition had the highest percentage of tubules containing elongated spermatids when compared with −7 °C (11.67 ± 3.97 % vs. 4.17 ± 2.50) or −8 °C (11.67 ± 3.97 % vs. 1.67 ± 1.67 %), no statistical differences were observed between these different soaking temperatures (P > 0.05; Fig. 5d). In comparison with the fresh tissue control, the mean percentage of tubules containing elongated spermatids was significantly decreased regardless of the soaking temperature used (P = 0.01), although the soaking temperature at −9 °C appeared to be the closest match to the fresh tissue control.
In vitro differentiation of SSCs into flagellated late spermatids from frozen-thawed pre-pubertal (6.5 dpp) testicular tissues is possible but less efficient, when compared with fresh tissue control
Pre-pubertal fresh and frozen-thawed testicular tissues were cultured for 30 days in order to generate spermatozoa. After dissection of the cultured explants, elongated spermatids and flagellated late spermatids were detected for each condition tested. The mean number of elongated spermatids and flagellated late spermatids per milligram of tissue was significantly reduced under frozen-thawed conditions when compared with the fresh control (P = 0.029). However, the mean number of elongated spermatids observed with a soaking temperature at −9 °C was higher when compared with −7 °C or −8 °C (P = 0.029, for both). In addition, although not significant, the mean number of flagellated late spermatids observed with a soaking temperature at −9 °C (10 ± 2) was higher when compared with −7 °C (4 ± 2) or −8 °C (4 ± 1; Fig. 6a). Flagellated late spermatids were evidenced with Shorr colouration (Fig. 6b) and the flagellum was detected by immunofluorescence with anti-α-tubulin antibody (Fig. 6c).
Identification and enumeration of elongated and flagellated late spermatids generated from fresh and frozen-thawed pre-pubertal (6.5 dpp) mouse testes at D30 of culture. a Enumeration of elongated and flagellated late spermatids per milligram of tissue at D30 of culture. Values are expressed as the mean number of spermatids per milligram of testis tissue ± SEM; n = 4 mouse testes for each condition. *Statistically significant difference between the conditions −9 °C and −7 °C or −8 °C; P = 0.029 (a, b statistically significant differences between the slow-frozen and the fresh conditions for elongated and flagellated late spermatids, respectively). b Identification of flagellated late spermatid generation by using Shorr staining. c The flagellum was immunodetected by using a specific anti-acetylated α-tubulin antibody and the nucleus was stained blue with DAPI (4′,6′-diamino-2-phenylindole). d Negative control performed with pre-immune mouse IgG. Magnification ×1000 (a), ×900 (c, d). Bars 10 μm
Soaking temperature at −9 °C maintains functional integrity of Leydig cells but shows higher Leydig cell activity than fresh tissue control in terms of testosterone secretion during in vitro culture
Functional integrity of the Leydig cells was maintained in frozen-thawed pre-pubertal mouse testicular tissues following a −9 °C soaking, since a significant increase in testosterone concentration was obtained during culture between D0 and D30 of culture (P = 0.0067), as in the fresh tissue control (P = 0.0062; Electronic Supplementary Material, Fig. S2). However, compared with the fresh tissue control, the testosterone concentration was significantly increased under the −9 °C condition at D7 (P = 0.01), D11 (P = 0.02) and D30 (P = 0.01).
Discussion
Testicular tissue banking before a highly gonadotoxic treatment is a prerequisite to preserve fertility in young boys not yet producing sperm. However, no established standard protocol exists for testicular tissue freezing and this procedure remains at the investigational stage (Loren et al. 2013). Controlled slow freezing rather than uncontrolled freezing is a critical condition to maximize post-thaw cell viability. However, the controlled slow freezing protocols previously used for testicular tissue include a cooling rate with a soaking temperature that varies between −7 °C, −8 °C and −9 °C (Table 1).
The current study demonstrated that a soaking temperature at −9 °C was the optimal condition that permitted seminiferous tubule growth, the maintenance of intratubular cell proliferation with less cellular death and reduced morphological tissue alterations after the in vitro culture of frozen-thawed pre-pubertal mouse testicular tissue. In addition, we showed that the −9 °C soaking temperature allowed a better progression of frozen-thawed pre-pubertal SSCs through the spermatogenic process giving rise to elongated spermatids and spermatozoa at D30 of culture. The choice of the controlled slow freezing strategy used in the current study was based on the best protocol proposed by Milazzo et al. (2010) whereby pre-pubertal mouse testes were cryopreserved according to 19 different parameters (CPA type and concentration, equilibration time, equilibration temperature and cooling rate). Immature testicular fragments were frozen with the protocol offering the best parameters of assessment and spermatozoa were obtained after allograft into Swiss nude mice for 5 months (Milazzo et al. 2010). In addition, seeding was not performed in the current study, since testis freezing with 1.5 M DMSO without seeding was previously demonstrated to maintain not only immature testicular tissue architecture but also the viability of the testicular cells and endocrine and partial exocrine functions of the testis (Milazzo et al. 2008). However, only one soaking temperature at −9 °C was previously assessed according to previous protocols used for ovarian (Poirot et al. 2002; Perdrix et al. 2010) or pre-pubertal testicular (Kvist et al. 2006) tissue. Here, we opted for an in vitro culture strategy that consisted in the use of an agarose gel system with RE being added to the culture medium (Garcia-Gonzalo and Izpisúa Belmonte 2008; Arkoun et al. 2015), because RE plays a critical role not only in SSC differentiation and their entry into meiosis but also in the progression of spermatocytes into round and elongated spermatids (Arkoun et al. 2015).
Our team previously demonstrated that RE at 10−6 M and the use of polycarbonate membrane inserts maintained intratubular cell proliferation and the ability of spermatogonia to initiate spermatogenesis in fresh and frozen pre-pubertal mouse testicular tissue with a soaking temperature at −8 °C, rather than −7 °C or −9 °C (Travers et al. 2013). However, the percentage of meiotic seminiferous tubules was close to that of the fresh tissue control following a soaking temperature both at −8 °C and at −9 °C. The current study showed that, regardless of the soaking temperature used, round and elongated spermatids were produced at D30 of culture. The impact of the different soaking temperatures on germ cell differentiation reported in the current study is difficult to compare with that reported by Travers et al. (2013). Indeed, no post-meiotic germ cells were obtained with the polycarbonate membrane inserts used as a culture system and high levels of tissue necrosis were observed from D11 of culture (Travers et al. 2013). Therefore, short-term culture methods, notably those with membrane inserts, appear not to be the most suitable tool for determining the optimal soaking temperature for slow freezing protocols. However, our findings are supported by the study performed by Yokonishi et al. (2014) who showed complete in vitro spermatogenesis from mouse pre-pubertal testicular tissue.
The soaking temperature has been implicated in reducing ice crystal formation (for a review, see Shaw and Jones 2003) and therefore might impact on the effectiveness of SSC differentiation. The various soaking temperatures assessed in the current study correspond to water transition from the liquid to solid phase. The withdrawal of water from testis tissues is an equally difficult but necessary condition, because of the tendency for the seminiferous tubules to trap water, potentially leading to ice formation (Woods et al. 2004). This ice formation would probably destroy tubule structure, ultimately affecting post-culture functionality. Indeed, the cooling rate should be sufficiently slow in order to allow the cell to lose water rapidly enough by exosmosis for the resulting concentration of intracellular solutes to eliminate supercooling and to maintain the chemical potential of intra-cellular water in equilibrium with that of extra-cellular water (Mazur 1977). Consequently, the cell dehydrates and does not freeze intracellularly. However, if the cooling rate is too rapid, the cell is not able to lose water fast enough to maintain equilibrium and the result is that the cell freezes intra-cellularly because of intracellular ice crystal formation (Mazur 1977).
In this respect, our results showed that testicular tissue functionality and structural integrity were influenced by the soaking temperature used after in vitro culture. Although few pyknotic cells were found per tubule, ranging from 1–3 in our observations, this parameter is also of major interest. Indeed, necrosis should be avoided at all costs to enable a better course of in vitro spermatogenesis. A significant decrease of pyknotic cells per tubule was obtained for soaking at −9 °C and in the fresh control when compared with −7 °C or −8 °C. In addition, no significant difference was observed between −9 °C and the fresh tissue control suggesting that −9 °C better preserves intratubular cells from necrosis. All these data suggest that the soaking temperature at −9 °C allows the suitable preservation of frozen-thawed SSCs increasing their chance of differentiation and giving rise to the final steps of spermatogenesis. However, the numbers of flagellated late spermatids generated with this soaking temperature were significantly lower in comparison with the fresh tissue control but higher, even if not significantly so, in comparison with the other freezing conditions.
Our study also revealed the maintenance of the endocrine function of the fresh and frozen-thawed mouse testicular tissue during culture, since the testosterone concentration was markedly increased between D0 and D30. However, Leydig cell steroidogenesis exhibited a higher activity in frozen-thawed testis tissues, with a more elevated basal testosterone secretion throughout culture times, except for D18, when compared with the fresh tissue control. An apparent trend towards an increased basal androgen level in frozen-thawed rat and mouse Leydig cells was previously reported, by using DMSO at 2.1 M and 1.5 M, respectively, as a CPA (Chen et al. 2007; Milazzo et al. 2008). Furthermore, an increase of steroidogenic activity was also previously detected in cultured rat Leydig cells, when DMSO at 100 mM was used as an antioxidant acting as a scavenger of hydroxyl radicals (Abney and Meyers 1987). Therefore, the increased androgen biosynthesis in our frozen-thawed mouse testicular tissue might be attributable to trace amounts of DMSO remaining in the cultured testicular tissues, even though DMSO was removed by four successive washing steps prior to culture in our study. To the best of our knowledge, the mechanism of action by which the freezing-thawing process and DMSO stimulate Leydig cell steroidogenic activity remains unknown and needs further investigation.
In conclusion, the current study suggests that the soaking temperature during the slow freezing of pre-pubertal mouse testicular tissue positively influences the course of in vitro spermatogenesis. The soaking temperature at −9 °C, rather than −7 °C or −8 °C, offers the best parameters evaluated for (1) the mean number of pyknotic nuclei per tubule, (2) the mean percentage of elongated spermatids per seminiferous tubule and (3) the mean number of elongated spermatids per milligram of testicular tissue after dissection at D30. We have demonstrated that our slow freezing protocol with a soaking temperature at −9 °C is the closest match to fresh tissue in terms of the complete achievement of in vitro spermatogenesis and flagellated late spermatid production, even if the effectiveness of the maturation process is reduced in the frozen tissue. Our cryopreservation strategy for pre-pubertal mouse testicular tissue can be proposed in the future for human application.
References
Abney TO, Meyers RB (1987) The effects of low O2 and antioxidants on steroidogenic capacity in cultured rat Leydig cells. Adv Exp Med Biol 219:609–612
Arkoun B, Dumont L, Milazzo J-P, Way A, Bironneau A, Wils J, Macé B, Rives N (2015) Retinol improves in vitro differentiation of prepubertal mouse spermatogonial stem cells into sperm during the first wave of spermatogenesis. PLoS One 10:e0116660
Arregui L, Dobrinski I (2014) Xenografting of testicular tissue pieces: 12 years of an in vivo spermatogenesis system. Reproduction 148:R71–R84
Baert Y, Van Sean D, Haentjens P, In’t Veld P, Tournaye H, Goosses E (2013) What is the best protocol for human testicular tissue banking? Hum Reprod 28:1816–1826
Chen GR, Ge RS, Lin H, Dong L, Sottas CM, Hardy MP (2007) Development of a cryopreservation protocol for Leydig cells. Hum Reprod 22:2160–2168
Curaba M, Verleysen M, Amorim CA, Dolmans MM, Van Langendonckt A, Hovatta O, Wyns C, Donnez J (2011) Cryopreservation of pre-pubertal mouse testicular tissue by vitrification. Fertil Steril 95:1229–1234.e1
Dumont L, Arkoun B, Jumeau F, Milazzo JP, Bironneau A, Liot D, Wils J, Rondanino C, Rives N (2015) Assessment of the optimal vitrification protocol for pre-pubertal mice testes leading to successful in vitro production of flagellated spermatozoa. Andrology 3:611–625
Fishman JA, Scobie L, Takeuchi Y (2012) Xenotransplantation-associated infectious risk: a WHO consultation. Xenotransplantation 19:72–81
Garcia-Gonzalo FR, Izpisúa Belmonte JC (2008) Albumin-associated lipids regulate human embryonic stem cell self-renewal. PLoS One 3:e1384
Goossens E, Frederickx V, Geens M, De Block G, Tournaye H (2008) Cryosurvival and spermatogenesis after allografting prepubertal mouse tissue: comparison of two cryopreservation protocols. Fertil Steril 89:725–727
Goossens E, Van Saen D, Tournaye H (2013) Spermatogonial stem cell preservation and transplantation: from research to clinic. Hum Reprod 28:897–907
Honaramooz A, Snedaker A, Boiani M, Schöler H, Dobrinski I, Schlatt S (2002) Sperm from neonatal mammalian testes grafted in mice. Nature 418:778–781
Hou M, Andersson M, Eksborg S, Söder O, Jahnukainen K (2007) Xenotransplantation of testicular tissue into nude mice can be used for detecting leukemic cell contamination. Hum Reprod 22:1899–1906
Jahnukainen K, Ehmcke J, Hergenrother SD, Schlatt S (2007) Effect of cold storage and cryopreservation of immature non-human primate testicular tissue on spermatogonial stem cell potential in xenografts. Hum Reprod 22:1060–1067
Jezek D, Schulze W, Kalanj-Bognar S, Vukelić Z, Milavec-Puretić V, Krhen I (2001) Effects of various cryopreservation media and freezing-thawing on the morphology of rat testicular biopsies. Andrologia 33:368–378
Keros V, Rosenlund B, Hultenby K, Aghajanova L, Levkov L, Hovatta O (2005) Optimizing cryopreservation of human testicular tissue: comparison of protocols with glycerol, propanediol and dimethylsulphoxide as cryoprotectants. Hum Reprod 20:1676–1687
Keros V, Hultenby K, Borgström B, Fridström M, Jahnukainen K, Hovatta O (2007) Methods of cryopreservation of testicular tissue with viable spermatogonia in pre-pubertal boys undergoing gonadotoxic cancer treatment. Hum Reprod 22:1384–1395
Kvist K, Thorup J, Byskov AG, Høyer PE, Møllgård K, Yding Andersen C (2006) Cryopreservation of intact testicular tissue from boys with cryptorchidism. Hum Reprod 21:484–491
Lee YA, Kim YH, Ha SJ, Kim KJ, Kim BJ, Kim BG, Choi SH, Kim IC, Schmidt JA, Ryu BY (2014) Cryopreservation of porcine spermatogonial stem cells by slow-freezing testis tissue in trehalose. J Anim Sci 92:984–995
Loren AW, Mangu PB, Beck LN, Brennan L, Magdalinski AJ, Partridge AH, Quinn G, Wallace WH, Oktay K (2013) Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol 31:2500–2510
Luetjens CM, Stukenborg JB, Nieschlag E, Simoni M, Wistuba J (2008) Complete spermatogenesis in orthotopic but not in ectopic transplants of autologously grafted marmoset testicular tissue. Endocrinology 149:1736–1747
Mazur P (1977) The role of intracellular freezing in the death of cells cooled at supraoptimal rates. Cryobiology 14:251–272
Milazzo JP, Vaudreuil L, Cauliez B, Gruel E, Massé L, Mousset-Siméon N, Macé B, Rives N (2008) Comparison of conditions for cryopreservation of testicular tissue from immature mice. Hum Reprod 23:17–28
Milazzo JP, Travers A, Bironneau A, Safsaf A, Gruel E, Arnoult C, Macé B, Boyer O, Rives N (2010) Rapid screening of cryopreservation protocols for murine pre-pubertal testicular tissue by histology and PCNA immunostaining. J Androl 31:617–630
Ogawa T, Ohmura M, Ohbo K (2005) The niche for spermatogonial stem cells in the mammalian testis. Int J Hematol 2:381–388
Pacchiarotti J, Ramos T, Howerton K, Greilach S, Zaragoza K, Olmstead M, Izadyar F (2013) Developing a clinical-grade cryopreservation protocol for human testicular tissue and cells. Biomed Res Int 2013:930–962
Perdrix A, Macé B, Milazzo JP, Liard-Zmuda A, Baron M, Rives N (2010) Ovarian tissue thawing: a comparison of two conditions. Fertil Steril 93:307–310
Poirot C, Vacher-Lavenu MC, Helardot P, Guibert J, Brugières L, Jouannet P (2002) Human ovarian tissue cryopreservation: indications and feasibility. Hum Reprod 17:1447–1452
Reuter K, Schlatt S, Ehmcke J, Wistuba J (2012) Fact or fiction: in vitro spermatogenesis. Spermatogenesis 2:245–252
Schlatt S, Kim SS, Gosden R (2002) Spermatogenesis and steroidogenesis in mouse, hamster and monkey testicular tissue after cryopreservation and heterotopic grafting to castrated hosts. Reproduction 124:339–346
Shaw JM, Jones GM (2003) Terminology associated with vitrification and other cryopreservation procedures for oocytes and embryos. Hum Reprod Update 9:583–605
Shinohara T, Inoue K, Ogonuki N, Kanatsu-Shinohara M, Miki H, Nakata K, Kurome M, Nagashima H, Toyokuni S, Kogishi K, Honjo T, Ogura A (2002) Birth of offspring following transplantation of cryopreserved immature testicular pieces and in-vitro microinsemination. Hum Reprod 17:3039–3045
Song Y, Silversides FG (2007) Production of offspring from cryopreserved chicken testicular tissue. Poult Sci 86:1390–1396
Song HW, Wilkinson MF (2012) In vitro spermatogenesis: a long journey to get tails. Spermatogenesis 2:238–244
Travers A, Arkoun B, Safsaf A, Milazzo JP, Absyte A, Bironneau A, Perdrix A, Sibert L, Macé B, Cauliez B, Rives N (2013) Effects of vitamin A on in vitro maturation of pre-pubertal mouse spermatogonial stem cells. PLoS One 8:e82819
Unni S, Kasiviswanathan S, D’Souza S, Khavale S, Mukherjee S, Patwardhan S, Bhartiya D (2012) Efficient cryopreservation of testicular tissue: effect of age, sample state, and concentration of cryoprotectant. Fertil Steril 97:200–208
Woods EJ, Benson JD, Agca Y, Critser JK (2004) Fundamental cryobiology of reproductive cells and tissues. Cryobiology 48:146–156
Wyns C, Van Langendonckt A, Wese FX, Donnez J, Curaba M (2008) Long-term spermatogonial survival in cryopreserved and xenografted immature human testicular tissue. Hum Reprod 23:2402–2414
Wyns C, Curaba M, Vanabelle B, Van Langendonckt A, Donnez J (2010) Options for fertility preservation in pre-pubertal boys. Hum Reprod Update 16:312–328
Wyns C, Curaba M, Petit S, Vanabelle B, Laurent P, Wese JF, Donnez J (2011) Management of fertility preservation in pre-pubertal patients: 5 years’ experience at the Catholic University of Louvain. Hum Reprod 26:737–747
Yildiz C, Mullen B, Jarvi K, McKerlie C, Lo KC (2013) Effect of different cryoprotectant agents on spermatogenesis efficiency in cryopreserved and grafted neonatal mouse testicular tissue. Cryobiology 67:70–75
Yokonishi T, Sato T, Komeya M, Katagiri K, Kubota Y, Nakabayashi K, Hata K, Inoue K, Ogonuki N, Ogura A, Ogawa T (2014) Offspring production with sperm grown in vitro from cryopreserved testis tissues. Nat Commun 5:4320
Acknowledgments
The authors are grateful to Agathe Way for her assistance with the immunohistochemistry.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare no competing interests.
Additional information
This study was supported by a PhD grant from ”La Région Haute-Normandie” (awarded to Brahim Arkoun) and funding from Rouen University Hospital, Institute for Research and Innovation in Biomedicine, Agence de la Biomédecine and “la Ligue nationale contre le cancer”.
Electronic supplementary material
Below is the link to the electronic supplementary material.
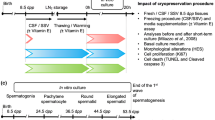
Fig. S1
Representation of experimental procedures performed with pre-pubertal (6.5 dpp) mouse testes. a Controlled slow freezing of pre-pubertal mouse testes with various soaking temperatures (−7 °C, −8 °C or −9 °C) before their storage in liquid nitrogen at −196 °C. b Thawing procedure of immature mouse testes. c In vitro culture of frozen-thawed pre-pubertal mouse testes on agarose gels at a gas-liquid interphase, according to the various soaking temperatures used above. d Set of experiments performed after culture of the frozen-thawed pre-pubertal mouse testicular tissues (D DMSO, dpp day post-partum, FCS fetal calf serum, KSR knock-out serum replacement, L-15 Leibovitz medium, LN 2 liquid nitrogen, α-MEM alpha-minimum essential medium, RE retinol, RIA radioimmunoassay, S sucrose). (PDF 363 kb)
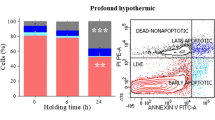
Fig. S2
Assessment of Leydig cell functional integrity during in vitro culture of frozen-thawed pre-pubertal (6.5 dpp) mouse testes using the −9 °C condition. Results indicate the mean of testosterone concentration in the culture medium under the various conditions tested. Data are expressed as mean ± SEM; n = 4 mouse testes for each condition. *Statistically significant difference between −9 °C and fresh tissue control; P < 0.05 (D day, NS not significant). (PDF 246 kb)
Rights and permissions
About this article
Cite this article
Arkoun, B., Dumont, L., Milazzo, JP. et al. Does soaking temperature during controlled slow freezing of pre-pubertal mouse testes influence course of in vitro spermatogenesis?. Cell Tissue Res 364, 661–674 (2016). https://doi.org/10.1007/s00441-015-2341-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-015-2341-2