Abstract
Pulmonary endothelial permeability is an important determinant of vascular adaptation to changes in oxygen tension, blood pressure, levels of growth factors or inflammatory cytokines. The Ras homologous (Rho) family of guanosine triphosphate phosphatases (Rho GTPases), key regulators of the actin cytoskeleton, regulate endothelial barrier function in response to a variety of environmental factors and signalling agents via the reorganization of the actin cytoskeleton, changes in receptor trafficking or the phosphorylation of junctional proteins. This review provides a brief summary of recent knowledge on Rho-GTPase-mediated effects on pulmonary endothelial barrier function and focuses in particular on their role in pulmonary vascular disorders, including pulmonary hypertension, chronic obstructive pulmonary disease, acute lung injury and acute respiratory distress syndrome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Lung-function: general overview
Pulmonary circulation is a low-pressure high-volume circulation that responds to hypoxia with vasoconstriction. It is exposed to the highest oxygen tension of all vascular beds (Stan 2009) and its function impacts the whole circulatory system, as the entire cardiac output passes through the lung with every heartbeat. Only a 0.3-μm-thick barrier separates the capillary blood from the alveolar gas (West 2013). The integrity of the pulmonary endothelial barrier is important in maintaining the dry interstitium and alveolar airspaces that are necessary for effective gas exchange. It also affects vascular tone, inflammation, coagulation and angiogenesis. Vascular leakage can be initiated by a number of environmental and chemical factors including sudden or sustained changes in oxygen tension, mechanical injury and agents produced by cells in response to injury, cancer or inflammation, such as vascular endothelial growth factor (VEGF), thrombin and histamine.
Proteins and liquids are transported across the endothelium via transcellular or paracellular routes. Transcellular routes, involving the active transport of molecules larger than 3 nm in radius, are mediated by caveolae, vesiculo–vacuolar organelles and fenestrations (Weis 2008; Wang and Dudek 2009). Paracellular permeability, usually induced in pathological situations, is caused by the disruption of intercellular junctions and allows the passive transport of larger volumes of liquids and molecules of radii smaller than 3 nm across the endothelium (Weis 2008; Wang and Dudek 2009).
Endothelial cells are connected to each other by three different junctional complexes, comprising (1) adherens junctions (AJ), (2) tight junctions (TJ) and (3) gap junctions (GJ; Bazzoni and Dejana 2004). Vascular endothelial cadherin (VE-cadherin) is the major structural protein of AJ in endothelial cells (Dejana et al. 2009). The VE-cadherin cytoplasmic tail binds β-catenin or plakoglobin, which associates with a number of actin-binding proteins such as α-catenin, vinculin, α-actinin and eplin (Dejana et al. 2009). This complex stabilizes AJ anchorage to the actin cytoskeleton.
TJ are composed of claudins, occludins and junctional adhesion molecules. The link between the TJ proteins and the actin cytoskeleton is modulated by intermediate signalling proteins (catenins, zonula occludens 1 protein [ZO-1]) and is subject to regulation by kinases and phosphatases (Bazzoni and Dejana 2004; Dejana et al. 2009).
GJ form channels between adjacent cells and allow the exchange of small signalling molecules such as cyclic nucleotides, calcium, adenosine triphosphate and inositol 1,4,5-trisphosphate between cells. In the vascular system, the core proteins of these channels are connexins (Cx) 37, 40 and 43 (van Kempen and Jongsma 1999; Parthasarathi and Quadri 2009). GJ are located in close proximity to the TJ and AJ that form the endothelial barrier and share common linker proteins that bind to the actin cytoskeleton (Derangeon et al. 2009).
The association of the actin cytoskeleton to junctional proteins, integrins and their extracellular ligands is essential for the maintenance of endothelial barrier function. The barrier is regulated by a balance between competing contractile forces, which generate centripetal tension and adhesive tethering forces created by cell-cell and cell-matrix adhesions (Wojciak-Stothard and Ridley 2002). Contractility of the actin cytoskeleton is controlled directly by myosin light chain kinase (MLCK) and Ras homologous (Rho) guanosine triphosphate (GTP) phosphatases (GTPases).
Rho GTPases
Rho GTPases are key regulators of cytoskeletal dynamics (Hall 1998; Hall and Lalli 2010) and affect several vascular processes such as endothelial permeability (Beckers et al. 2010), cell motility (Ridley 2001), angiogenesis (Bryan and D’Amore 2007), nitric oxide (NO) production (Takemoto et al. 2002), smooth muscle contractility (Somlyo and Somlyo 2003), cell proliferation, differentiation and apoptosis (Vega and Ridley 2008; Pedersen and Brakebusch 2012). Rho proteins share approximately 30 % homology with the Ras family of proteins and 80-90 % homology with each other (Hall 1998).
Rho GTPases are activated by a number of factors known to affect endothelial permeability, such as thrombin, histamine, angiotensin II, endothelin-1 (ET-1), VEGF, tyrosine kinase receptors or integrin clustering. In addition, Rho proteins are also activated by mechanical and physical stimuli such as shear stress, stretch, pressure and hypoxia (Wojciak-Stothard and Ridley 2002; Wojciak-Stothard 2008).
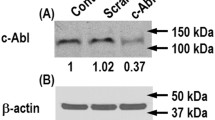
Rho GTPases cycle between an active GTP-bound and an inactive guanosine diphosphate (GDP)-bound conformation. Inactive GDP-bound Rho proteins remain in the cytosol in complex with guanine nucleotide dissociation inhibitors (GDIs). Upon phosphorylation triggered by signalling mediators, GDIs dissociate from Rho GTPases allowing them to interact with guanine nucleotide exchange factors (GEFs). GEFs activate the exchange of GDP for GTP allowing Rho GTPases to interact with their downstream effectors (Jaffe and Hall 2005). GTPase-activating proteins (GAPs) mediate the inactivation of GTPases. Apart from GTP/GDP binding, Rho GTPases can be regulated through isoprenylation, carboxylmethylation, oxidation, direct phosphorylation or ubiquitination (Storck and Wojciak-Stothard 2013). Isoprenylation of the C-terminus of Rho GTPases enhances their binding to the cell membrane, a characteristic that is important for interaction with signalling effectors (Gao et al. 2009).
In this review, we describe the implications of the dysregulation of Rho GTPase signalling in pulmonary vascular barrier dysfunction and highlight some of the potential therapeutic strategies.
RhoA, RhoB and Rho kinase
The basal activity of RhoA is important in the maintenance of inter-endothelial junctions by promoting membrane localization of the AJ protein, VE-cadherin and by strengthening endothelial cortical actin via its effector diaphanous in a profilin-dependent manner (van Nieuw Amerongen et al. 2007; Spindler et al. 2010). However, excessive activation of RhoA and its effector Rho kinase (ROCK), by agents such as thrombin, tumour necrosis factor alpha (TNF-α), oxidative or mechanical stress, is associated with a decrease in endothelial barrier function (Wojciak-Stothard and Ridley 2002; Wojciak-Stothard 2008; Beckers et al. 2010; Spindler et al. 2010). This is caused by an increase in the contractile forces that pull the endothelial intercellular junctions apart (Wojciak-Stothard and Ridley 2002; Wojciak-Stothard 2008; Beckers et al. 2010; Spindler et al. 2010).
Activation of actomyosin contractility by RhoA results predominantly from a ROCK-mediated increase in the level of myosin light chain (MCL20) phosphorylation (Somlyo and Somlyo 2003; Connolly and Aaronson 2011). ROCK can also facilitate actomyosin contractility by increasing the levels of intracellular calcium, following inhibition of voltage-gated potassium channels (Aaronson et al. 2006). RhoA can also compromise endothelial barrier function by reducing the expression of endothelial NO synthase (eNOS) and NO generation by endothelial cells (Takemoto et al. 2002). Conversely, NO might inhibit RhoA by reducing its stability and membrane localization (Sauzeau et al. 2000, 2003).
RhoB, a protein 85 % homologous to RhoA, has also recently been implicated in the regulation of pulmonary endothelial barrier function. RhoB expression and activity can be increased by numerous agents including oxidative stress, tyrosine kinases, the transforming growth factor beta/bone morphogenetic protein/Smad pathway and growth factors such as fibroblast growth factor, epidermal growth factor and platelet-derived growth factor (Huang et al. 2007; Kajimoto et al. 2007; Vardouli et al. 2008; Wojciak-Stothard et al. 2012). Similar to RhoA, RhoB can interact with ROCK, increase MLC20 phosphorylation and promote actin polymerization (Conway et al. 2004; Fernandez-Borja et al. 2005). Under hypoxic conditions, RhoB appears to have a complementary effect to RhoA on actomyosin contractility and pulmonary endothelial permeability (Wojciak-Stothard et al. 2012). Whereas RhoA acts as a major activator of ROCK-mediated serine MLC20 phosphorylation, RhoB promotes actin filament formation by interacting with a mammalian homologue of Drosophila diaphanous, a protein known to induce actin nucleation (Wojciak-Stothard et al. 2012). RhoB can also activate the pro-inflammatory transcription factor, nuclear factor kappa B (Rodriguez et al. 2007), an event of potential importance in the regulation of endothelial barrier function during inflammatory responses.
Rac1 and Cdc42
Rac1 and Cdc42 generally have endothelial-barrier-protective effects and their activation co-incides with the formation of intercellular adhesions, whereas RhoA activity is reduced (Wojciak-Stothard and Ridley 2002; Beckers et al. 2010; Spindler et al. 2010). GTP-bound Rac1 and Cdc42 bind to and allow the autophosphorylation and activation of p21-activated protein kinases (PAK). Phosphorylation of MLCK by PAK results in the inhibition of the phosphorylation of MLC20 in vitro and in vivo (Bokoch 2003), counteracting actomyosin contraction. Whereas basal levels of PAK activity are required for the maintenance of the junction-associated cortical actin rim, excessive activation of PAK can activate extracellular signal-regulated kinase (Erk) and induce barrier breakdown (Stockton et al. 2004, 2007).
Physiological activation of Rac by barrier-protective molecules (i.e., sphingosine-1 phosphate [S1P], NO) and specific mechanical stimuli (physiological level of laminar shear stress, low magnitude cyclic stretch) enhances the peripheral actin cytoskeleton and improves endothelial cell monolayer integrity (Garcia et al. 2001; Vouret-Craviari et al. 2002; Birukov et al. 2002; Dudek et al. 2004; Mehta et al. 2005; Birukova et al. 2006, 2007a, 2007b). Rac1 also enhances endothelial NO production by increasing eNOS mRNA and protein levels or by stimulating the uptake of eNOS substrate, L-arginine (Sawada et al. 2008). Whereas basal levels of Rac1 activity are endothelium-protective, sustained Rac1 activation can lead to endothelial dysfunction associated with the generation of reactive oxygen species (ROS; Hordijk 2006). Rac1 is a part of the nicotinamide adenine dinucleotide phosphate (NADPH) oxidase complex, the main source of ROS generation in the vasculature (Hordijk 2006).
Cdc42 appears to have a unique role in endothelial barrier restoration, possibly as a result of the regulation of VE-cadherin turnover in endothelial cells (Spindler et al. 2010). For instance, the delayed activation of Cdc42 following the activation of cells with thrombin contributes to the reassembly of inter-endothelial junctions and the re-establishment of barrier integrity (Kouklis et al. 2004).
Rho GTPases in endothelial barrier dysfunction in lung diseases
Dysregulation of Rho GTPase signalling by mechanical stress, hypoxia or inflammation is a shared feature of many lung diseases such as pulmonary hypertension (PH), asthma, acute lung injury (ALI) or acute respiratory distress syndrome (ARDS). Below, we present evidence of abnormal Rho GTPase signalling in endothelial barrier dysfunction in selected examples of lung disorders. A summary of the effects of various regulatory factors on the activity of Rho GTPases and pulmonary endothelial barrier function is presented in Table 1. Signalling pathways leading to changes in the organization of the actin cytoskeleton and endothelial junctional integrity are illustrated in Fig. 1.
Proposed mechanisms of Rho-GTPase-mediated changes in the organization of the actin cytoskeleton and endothelial junctional integrity. Details regarding signalling mediators shown in this diagram are provided in the text (arrows activation/upregulation, lines with a black circular ending downregulation/inhibition, open arrows an increase or decrease depending on arrow direction, ABP actin-binding proteins, ADMA asymmetric dimethylarginine, AJ adherens junction, Ang-1 angiopoietin-1, cGMP cyclic guanosine monophosphate, DDAH dimethylarginine dimethylhydrolase, mDia mammalian diaphanous, ETRA endothelin receptor antagonist, FVIIa factor VIIa, GJ gap junction, HGF hepatocyte growth factor, Il-6 interleukin-6, Il-8 interleukin-8, LIMK LIM kinase, LPS lipopolysaccharide, MLC-P phosphorylated myosin light chain, MLCK myosin light chain kinase, NO nitric oxide, OxPAPC oxidized 1-palmitoyl-2-arachidonyl-sn-glycero-3-phosphatidylcholine, PAK p21-activated protein kinase, PKCi PKC inhibitor, Rho Ras homologous, ROCK Rho kinase, S1P sphingosine-1 phosphate, TIP TNF-derived tonoplast intrinsic protein, TJ tight junction, VASP vasodilator-stimulated phosphoprotein, VASP-P phosphorylated VASP)
Pulmonary hypertension
Pulmonary hypertension (PH) is a condition characterized by abnormal remodelling of small pulmonary arteries, leading to increased pulmonary vascular resistance and right heart hypertrophy (Schermuly et al. 2011). The current classification is based on similar pathogenesis, clinical features and therapeutic options and has five main sub-categories: (1) pulmonary arterial hypertension (PAH); (2) PH resulting from left heart disease; (3) PH attributable to lung diseases and/or hypoxia; (4) chronic thromboembolic pulmonary hypertension (CTEPH); (5) PH with unclear multifactorial mechanisms (Archer et al. 2010; Schermuly et al. 2011).
Endothelial dysfunction is believed to be an early component of the disease and involves a decrease in endothelial barrier function, a decrease in the production of vasorelaxants such as NO and prostacyclin and an increase in the production of vasoconstrictors such as ET-1 or thromboxane (Budhiraja et al. 2004; Archer et al. 2010; Burton et al. 2011; Schermuly et al. 2011). RhoA and Rho kinase are activated in the pulmonary vasculature of PH patients and animals (Wojciak-Stothard 2008).
PH is a disease of multifactorial origin and a number of different stimuli implicated in the pathogenesis of PH converge on Rho GTPase signalling pathways. Hypoxia activates RhoA and inhibits Rac1 and Cdc42 in cultured pulmonary endothelial cells (PAECs; Wojciak-Stothard et al. 2005). This change might be transient and reversible by reoxygenation or might be sustained and irreversible depending on the duration of hypoxic exposure (Wojciak-Stothard et al. 2005, 2006). Endothelial cells isolated from pulmonary arteries of chronically hypoxic hypertensive piglets show increased permeability associated with the activation of RhoA and the inhibition of Rac1 (Wojciak-Stothard et al. 2006). Regulation of RhoA and Rac1 during hypoxia/reoxygenation depends on the activity of NADPH oxidase, phosphoinositide 3 kinase and intracellular ROS production (Wojciak-Stothard et al. 2005). Activation of RhoA by hypoxia in PH rat lungs depends on superoxide generation (Broughton et al. 2010). However, RhoA activation in cultured pulmonary endothelial and smooth muscle cells is ROS-independent (Chi et al. 2010) suggesting that the mechanism is cell-type-/tissue-specific. RhoA/ROCK can also be activated by the Src family of tyrosine kinases in agonist- and hypoxia-induced stimulation of pulmonary arteries in rats (Wang et al. 2001; Knock et al. 2008).
RhoB is rapidly and transiently upregulated in response to stress conditions. Both RhoA and RhoB are upregulated by hypoxia and the inhibition of either RhoA or RhoB prevents hypoxia-induced stress fibre formation and an increase in endothelial permeability in human pulmonary endothelial cells (HPAECs), indicating that both GTPases are important (Wojciak-Stothard et al. 2012). Inhibition of RhoB farnesylation prevents hypoxia-induced pulmonary endothelial permeability in vitro (Wojciak-Stothard et al. 2012). RhoB also stabilizes hypoxia inducible factor 1 alpha (HIF-1α) in HPAECs and therefore might impact pulmonary endothelial permeability induced by factors acting downstream of HIF-1α, such as VEGF. The mechanism of RhoB-induced stabilization of HIF-1α in endothelial cells will require further studies. In glioblastoma cells, RhoB prevents proteolytic degradation of HIF-1α by the Akt/glycogen synthase kinase-3β pathway (Skuli et al. 2006). Rac1, which activates the RhoB promoter (Huelsenbeck et al. 2013), has been shown to stabilize HIF-1α in hypoxic Hep3B cells (Hirota and Semenza 2001).
VEGF is important for the maintenance of pulmonary vascular homeostasis and protects against chronic hypoxia-induced PH in rats (Partovian et al. 2000; Tuder and Yun 2008). However, VEGF expression is increased in remodelled hypertensive arteries and is prominent in plexiform lesions in PH, suggesting that VEGF contributes to vascular pathology (for a review, see Tuder et al. 2000). VEGF induces pulmonary endothelial permeability in vitro and in vivo (Bates 2010) as a result of the rapid endocytosis of vascular endothelial cadherin (Gavard and Gutkind 2006). This process is initiated by VEGF-receptor-2-induced activation of the small GTPase Rac through a Src-dependent pathway. Rac1 activation promotes PAK-mediated phosphorylation of VE followed by internalization of the protein into clathrin-coated vesicles and a breakdown of inter-endothelial junctional integrity. Interestingly, the VEGF-induced decrease in endothelial barrier function is preceded by a Rac1-dependent transient enhancement of the endothelial barrier (Seebach et al. 2005).
Inhibition of NO signalling in PH is associated with increased plasma and tissue levels of the endogenous NOS inhibitor, asymmetric dimethylarginine (ADMA), mainly because of a decrease of its metabolism by the dimethylarginine dimethylhydrolase (DDAH) enzymes (Arrigoni et al. 2003; Millatt et al. 2003; Pullamsetti et al. 2005). ADMA activates RhoA and inhibits Rac1 in cultured endothelial cells, causing pulmonary endothelial barrier dysfunction, cell motility defects and abnormal angiogenesis in vitro and in vivo (Wojciak-Stothard et al. 2005, 2007, 2009). ADMA-induced RhoA activation in PAECs results from a decrease in NO/cyclic guanine monophosphate/protein kinase G (PKG) signalling and reduced levels of Ser188-phosphorylated RhoA, whereas Rac1 downregulation is associated with reduced phosphorylation of the PKG substrate scaffolding protein, vasodilator-stimulated phosphoprotein (VASP). Phosphorylation of RhoA on Ser188 weakens membrane binding because of electrostatic repulsion with negatively charged phospholipids and also results in an increased affinity for Rho-GDIs. Rho-GDI is sequestered in the cytosol, disabling downstream signalling (Lang et al. 1996; Sauzeau et al. 2000). Phosphorylation additionally plays a role in regulating the levels of cellular RhoA by inhibiting ubiquitin-mediated proteasomal degradation (Rolli-Derkinderen et al. 2005). VASP associates with AJ (Vasioukhin and Fuchs 2001) and TJ (Comerford et al. 2002) and links intercellular junction proteins with the actin cytoskeleton (Krause et al. 2003). Mice lacking proteins of the VASP family consistently die from oedema formation attributable to defective vascular barrier function (Furman et al. 2007). VASP-deficient endothelial cells show increased permeability and reduced Rac1 activity under basal conditions (Schlegel et al. 2008). Although the way that the NO/PKG-induced phosphorylation of VASP activates Rac1 is not fully understood, interactions of VASP with Rac1 regulatory proteins such as p120Ras GAP, GTP exchange factors for Rac1 or the TJ component ZO-1, are likely to play a role (Comerford et al. 2002; Schlegel et al. 2008).
In addition to the Rho/Rac1-mediated reorganization of the actin cytoskeleton and of AJ, ADMA reduces the expression, activation and membrane localization of a GJ protein, Cx43, in PAECs (Tsang et al. 2014). These changes are associated with decreased expression and phosphorylation of c-jun and increased pulmonary endothelial permeability in vitro and in vivo (Tsang et al. 2014). Interestingly, endothelial-like cells derived from the peripheral blood of patients with idiopathic PAH exhibit abnormal DDAH1/Cx43 signalling and increased permeability in vitro, highlighting the potential importance of this pathway in the disease. Rotigaptide, an anti-arrhytmic drug that enhances Cx43 function, prevents ADMA-induced pulmonary endothelial leakage in vitro and in vivo (Tsang et al. 2014). GJ proteins might affect pulmonary endothelial permeability by facilitating the assembly of AJ and TJ (Nagasawa et al. 2006) and/or mediating the exchange of secondary signalling mediators such as Ca2+ or cyclic nucleotides between cells in the lung capillary bed (Parthasarathi et al. 2006).
Chronic obstructive pulmonary disease
ROCK is activated by agents known to contribute to the pathogenesis of chronic obstructive pulmonary disease such as inflammatory cytokines (e.g., interleukin-6 [IL-6] and monocyte chemoattractant protein-1) or cigarette smoke (Fukumoto and Shimokawa 2011; Sakai et al. 2011). Cigarette smoke has been shown to induce ET-1 release in a ROS-dependent manner and to cause endothelial barrier dysfunction in vitro by activating the RhoA/ROCK pathway in HPAECs (Milara et al. 2010). These effects are attenuated by endothelin receptor antagonists, antioxidant N-acetylcysteine and ROCK inhibitor Y-27632 (Milara et al. 2010). In contrast, in another study, cigarette smoke has been shown to induce ROS and to increase endothelial permeability by the inhibition of RhoA signalling (Lu et al. 2011). Although the activation of RhoA/ROCK is commonly associated with an increase in endothelial permeability, the inhibition of RhoA can also compromise endothelial barrier function as a baseline level of active RhoA is essential for the maintenance of intercellular junctions (Beckers et al. 2010). ROS activate RhoA in cells by the direct oxidation of two cysteine residues located in the redox-sensitive motif of the protein (Aghajanian et al. 2009) but can also inhibit RhoA by the formation of an intramolecular disulfide bridge that prevents GTP binding (Heo et al. 2006). The differential effects of ROS on RhoA activity have been proposed to depend on ROS levels and on the balance of oxidizing and reducing agents within the cell (Lu et al. 2011). Physiological levels of ROS and a high reduction potential tend directly to oxidize and activate RhoA, whereas high levels of ROS and a low reduction potential tend to inhibit RhoA by the formation of disulfide bridges (Aghajanian et al. 2009; Lu et al. 2011).
ALI and ARDS
Vascular leakage is a hallmark of ALI and ARDS induced by direct or indirect mechanical, toxic, infectious or inflammatory challenges to the lung (Kumar et al. 2009). Several activators of RhoA/ROCK including endotoxin, IL-6, thrombin, ROS and mechanical stress have been implicated in pulmonary endothelial barrier dysfunction and oedema formation in these conditions (Maniatis and Orfanos 2008). Endotoxin-induced lung oedema in mice can be attenuated by the ROCK inhibitor, Y-27632 (Gorovoy et al. 2007), or by the endothelium-specific over-expression of Cdc42 (Ramchandran et al. 2008). Y-27632 has also been shown to attenuate ALI in septic rats (Cinel et al. 2012). Plasma levels of redox-reactive non-transferrin bound iron can increase under various pathophysiological conditions, including those associated with ALI (Gorbunov et al. 2012). The addition of [Fe2+] increases pulmonary endothelial permeability in vitro; this can also be attenuated by Y-27632 (Gorbunov et al. 2012).
Thrombin, one of the mediators of ALI, increases RhoA activity by activating p115-RhoGEF (Birukova et al. 2004). Fluorescent resonance energy transfer analysis has revealed an initial rise in RhoA activity at the cell periphery, followed by a shift of activity towards the cytosolic F-actin filaments, accompanied by the disruption of junctional integrity and intercellular gap formation (Szulcek et al. 2013).
The effects of thrombin can be attenuated by a number of factors. Factor VIIa, a clotting protease that binds to tissue factor, protects the endothelium from thrombin-induced barrier dysfunction in a Rac1-mediated manner (Sen et al. 2011). Angiopoietin-1 has also been shown to attenuate the effects of thrombin by increasing Rac1 activity, which enforces VE-cadherin organization and reduces RhoA activity in human pulmonary microvascular endothelial cells (van der Heijden et al. 2011).
The activation of RhoA/ROCK by a stretch induced by mechanical ventilation might constitute a “second hit” to Rho-independent lung injury induced by factors such as IL-6 (Birukova et al. 2012b). RhoA/ROCK activation in this model can be attenuated by the prostacyclin analogue, iloprost, which probably acts via the protein-kinase-A-mediated phosphorylation of Rho inhibitor, RhoGDI, or the negative regulation of RhoA by the cAMP/Epac/Rap1/Rac pathway (Birukova et al. 2010).
The mechanochemical environment can significantly affect the severity of ALI/ARDS (Birukov 2009). An 18 % cyclic stretch enhances thrombin-induced Rho activation, whereas a 5 % cyclic stretch promotes Rac activation, critical for the recovery of endothelial barrier function (Shikata et al. 2005; Birukova et al. 2006). Another Rac1-activating agent, hepatocyte growth factor (HGF), has been shown to prevent endothelial barrier dysfunction induced by a cyclic stretch and VEGF (Birukova et al. 2008). A combination of physiological cyclic stretch preconditioning and HGF has been demonstrated to attenuate VEGF-induced barrier dysfunction via the downregulation of the Rho pathway. These results highlight the importance of the mechanochemical environment in the control of Rho GTPase activity and lung endothelial permeability in ALI/ARDS.
The severity of permeability oedema during infection with the Gram-positive bacterium, Listeria monocytogenes, correlates with the levels of the cholesterol-binding pore-forming toxin, listeriolysin, which it produces (Rose et al. 2001; Repp et al. 2002; Munder et al. 2005). Listeriolysin-induced permeability is accompanied by an increased ROS generation, RhoA activation and MLC phosphorylation and can be completely inhibited by the protein kinase C (PKC) α/β inhibitor GÖ6976, indicating a crucial role for PKC in the induction of barrier dysfunction. The TNF-derived tonoplast intrinsic protein, which mimics the lectin-like domain of the cytokine, blunts listeriolysin-induced hyperpermeability in vitro, upon inhibiting PKC-α activation, ROS generation and MLC phosphorylation and upon restoring the RhoA/Rac1 balance. These results indicate that the lectin-like domain of TNF has a potential therapeutic value in protection from listeriolysin-induced pulmonary endothelial hyperpermeability (Xiong et al. 2010).
The platelet-derived phospholipid S1P can improve pulmonary endothelial barrier dysfunction in ALI by inducing Rac-dependent rearrangement of cortical actin (Abbasi and Garcia 2013; Dudek et al. 2004; McVerry et al. 2004)). S1P-induced cortical rearrangement of actin involves PAK activation, the phosphorylation and activation of LIM kinase and the subsequent inactivation of actin-severing protein, cofilin (Garcia et al. 2001). The importance of S1P signalling in the regulation of pulmonary vascular permeability has also been demonstrated by Zhao et al. (2009). Paracrine release of S1P by bone-marrow-derived endothelial progenitor cells in co-culture with pulmonary microvascular endothelial cells helps to re-anneal endothelial AJ and prevent lipopolysaccharide (LPS)-induced pulmonary endothelial leakage in vitro and in vivo (Zhao et al. 2009). The protective mechanism involves the activation of Rac1 and Cdc42 (Zhao et al. 2009).
The levels of phospholipid oxidation products, specifically oxidized 1-palmitoyl-2-arachidonoyl-sn-glycero-3-phosphatidylcholine (OxPAPC), derived from lipoproteins and membranes of cells undergoing oxidative stress or apoptosis are increased in inflammatory diseases including atherosclerosis, lung inflammation and tissue injury (Birukova et al. 2012a). Low concentrations of OxPAPC (5–20 mg/ml) enhance pulmonary endothelial barrier function in vitro and in vivo and reduce inflammation in animal models of acute lung injury caused by LPS or mechanical stress (Ma et al. 2004; Nonas et al. 2006, 2008). Protective effects of OxPAPC involve the enhancement of the peripheral actin cytoskeleton and of AJ and TJ mediated by Rac and Rap1 GTPases (Birukova et al. 2007a, 2011).
Plasma levels of adenosine are increased in response to lung injury (Lu et al. 2012). Acutely elevated adenosine has been shown to protect against pulmonary oedema in various animal models of ALI. This effect is thought to be mediated through transporter- and receptor-A2 and to involve the activation of Rac1, possibly via G-protein-coupled receptors (Lu et al. 2012). Whereas acute exposure of the lung to adenosine is protective, sustained adenosine exposure decreases endothelial cell barrier function, elevates cellular ROS levels and activates p38, c-jun N terminal kinases and RhoA (Lu et al. 2012).
Concluding remarks
Basal activity of Rho GTPases is required for the maintenance of normal pulmonary endothelial barrier function. Pathological activation of Rho GTPases by hypoxia, NO deprivation, inflammatory cytokines or mechanical stress leads to imbalance in the activities of RhoA, Rac1 and Cdc42 and causes profound changes in the structure and function of endothelial AJ, TJ and GJ. Improved understanding of the temporal and spacial activity changes of Rho GTPases in the pulmonary vasculature in response to stress conditions is required for the success of future therapeutic efforts in the treatment of endothelial barrier dysfunction in lung diseases.
Abbreviations
- ADMA:
-
Asymmetric dimethylarginine
- AJ:
-
Adherens junction
- ALI:
-
Acute lung injury
- ARDS:
-
Acute respiratory distress syndrome
- Cx:
-
Connexin
- DDAH:
-
Dimethylarginine dimethylhydrolase
- eNOS:
-
Endothelial nitric oxide synthase
- ET-1:
-
Endothelin-1
- GAPs:
-
GTPase-activating proteins
- GEFs:
-
Guanine nucleotide exchange factors
- GDIs:
-
Guanine nucleotide dissociation inhibitors
- GDP:
-
Guanosine diphosphate
- GJ:
-
Gap junction
- GTP:
-
Guanosine triphosphate
- GTPase:
-
GTP phosphatase
- HGF:
-
Hepatocyte growth factor
- HIF1α:
-
Hypoxia inducible factor 1 alpha
- HPAECs:
-
Human pulmonary artery endothelial cells
- LPS:
-
Lipopolysaccharide
- MLC20 :
-
Myosin light chain 20
- MLCK:
-
Myosin light chain kinase
- NADPH:
-
Nicotinamide adenine dinucleotide phosphate
- NO:
-
Nitric oxide
- OxPAPC:
-
Oxidized 1-palmitoyl-2-arachidonyl-sn-glycero-3-phosphatidylcholine
- PAECs:
-
Pulmonary artery endothelial cells
- PAH:
-
Pulmonary arterial hypertension
- PAK:
-
p21-activated protein kinase
- PH:
-
Pulmonary hypertension
- PKC:
-
Protein kinase C
- PKG:
-
Protein kinase G
- Rho:
-
Ras homologous
- ROCK:
-
Rho kinase
- ROS:
-
Reactive oxygen species
- S1P:
-
Sphingosine-1 phosphate
- TJ:
-
Tight junction
- TNF-α:
-
Tumour necrosis factor alpha
- VASP:
-
Vasodilator-stimulated phosphoprotein
- VE-cadherin:
-
Vascular endothelial cadherin
- VEGF:
-
Vascular endothelial growth factor
- ZO-1:
-
Zonula occludens protein 1
References
Aaronson PI, Robertson TP, Knock GA, Becker S, Lewis TH, Snetkov V, Ward JP (2006) Hypoxic pulmonary vasoconstriction: mechanisms and controversies. J Physiol (Lond) 570:53–58
Abbasi T, Garcia JG (2013) Sphingolipids in lung endothelial biology and regulation of vascular integrity. Handb Exp Pharmacol 2013:201–226
Aghajanian A, Wittchen ES, Campbell SL, Burridge K (2009) Direct activation of RhoA by reactive oxygen species requires a redox-sensitive motif. PLoS ONE 4:e8045
Archer SL, Weir EK, Wilkins MR (2010) Basic science of pulmonary arterial hypertension for clinicians: new concepts and experimental therapies. Circulation 121:2045–2066
Arrigoni FI, Vallance P, Haworth SG, Leiper JM (2003) Metabolism of asymmetric dimethylarginines is regulated in the lung developmentally and with pulmonary hypertension induced by hypobaric hypoxia. Circulation 107:1195–1201
Bates DO (2010) Vascular endothelial growth factors and vascular permeability. Cardiovasc Res 87:262–271
Bazzoni G, Dejana E (2004) Endothelial cell-to-cell junctions: molecular organization and role in vascular homeostasis. Physiol Rev 84:869–901
Beckers CM, van Hinsbergh VW, van Nieuw Amerongen GP (2010) Driving Rho GTPase activity in endothelial cells regulates barrier integrity. Thromb Haemost 103:40–55
Birukov KG (2009) Small GTPases in mechanosensitive regulation of endothelial barrier. Microvasc Res 77:46–52
Birukov KG, Birukova AA, Dudek SM, Verin AD, Crow MT, Zhan X, DePaola N, Garcia JG (2002) Shear stress-mediated cytoskeletal remodeling and cortactin translocation in pulmonary endothelial cells. Am J Respir Cell Mol Biol 26:453–464
Birukova AA, Smurova K, Birukov KG, Kaibuchi K, Garcia JG, Verin AD (2004) Role of Rho GTPases in thrombin-induced lung vascular endothelial cells barrier dysfunction. Microvasc Res 67:64–77
Birukova AA, Chatchavalvanich S, Rios A, Kawkitinarong K, Garcia JG, Birukov KG (2006) Differential regulation of pulmonary endothelial monolayer integrity by varying degrees of cyclic stretch. Am J Pathol 168:1749–1761
Birukova AA, Malyukova I, Poroyko V, Birukov KG (2007a) Paxillin-beta-catenin interactions are involved in Rac/Cdc42-mediated endothelial barrier-protective response to oxidized phospholipids. Am J Physiol Lung Cell Mol Physiol 293:L199–L211
Birukova AA, Zagranichnaya T, Fu P, Alekseeva E, Chen W, Jacobson JR, Birukov KG (2007b) Prostaglandins PGE(2) and PGI(2) promote endothelial barrier enhancement via PKA- and Epac1/Rap1-dependent Rac activation. Exp Cell Res 313:2504–2520
Birukova AA, Moldobaeva N, Xing J, Birukov KG (2008) Magnitude-dependent effects of cyclic stretch on HGF- and VEGF-induced pulmonary endothelial remodeling and barrier regulation. Am J Physiol Lung Cell Mol Physiol 295:L612–L623
Birukova AA, Burdette D, Moldobaeva N, Xing J, Fu P, Birukov KG (2010) Rac GTPase is a hub for protein kinase A and Epac signaling in endothelial barrier protection by cAMP. Microvasc Res 79:128–138
Birukova AA, Zebda N, Fu P, Poroyko V, Cokic I, Birukov KG (2011) Association between adherens junctions and tight junctions via Rap1 promotes barrier protective effects of oxidized phospholipids. J Cell Physiol 226:2052–2062
Birukova AA, Lee S, Starosta V, Wu T, Ho T, Kim J, Berliner JA, Birukov KG (2012a) A role for VEGFR2 activation in endothelial responses caused by barrier disruptive OxPAPC concentrations. PLoS One 7:e30957
Birukova AA, Tian Y, Meliton A, Leff A, Wu T, Birukov KG (2012b) Stimulation of Rho signaling by pathologic mechanical stretch is a “second hit” to Rho-independent lung injury induced by IL-6. Am J Physiol Lung Cell Mol Physiol 302:L965–L975
Bokoch GM (2003) Biology of the p21-activated kinases. Annu Rev Biochem 72:743–781
Broughton BR, Jernigan NL, Norton CE, Walker BR, Resta TC (2010) Chronic hypoxia augments depolarization-induced Ca2+ sensitization in pulmonary vascular smooth muscle through superoxide-dependent stimulation of RhoA. Am J Physiol Lung Cell Mol Physiol 298:L232–L242
Bryan BA, D’Amore PA (2007) What tangled webs they weave: Rho-GTPase control of angiogenesis. Cell Mol Life Sci 64:2053–2065
Budhiraja R, Tuder RM, Hassoun PM (2004) Endothelial dysfunction in pulmonary hypertension. Circulation 109:159–165
Burton VJ, Ciuclan LI, Holmes AM, Rodman DM, Walker C, Budd DC (2011) Bone morphogenetic protein receptor II regulates pulmonary artery endothelial cell barrier function. Blood 117:333–341
Chi AY, Waypa GB, Mungai PT, Schumacker PT (2010) Prolonged hypoxia increases ROS signaling and RhoA activation in pulmonary artery smooth muscle and endothelial cells. Antioxid Redox Signal 12:603–610
Cinel I, Ark M, Dellinger P, Karabacak T, Tamer L, Cinel L, Michael P, Hussein S, Parrillo JE, Kumar A (2012) Involvement of Rho kinase (ROCK) in sepsis-induced acute lung injury. J Thorac Dis 4:30–39
Comerford KM, Lawrence DW, Synnestvedt K, Levi BP, Colgan SP (2002) Role of vasodilator-stimulated phosphoprotein in PKA-induced changes in endothelial junctional permeability. FASEB J 16:583–585
Connolly MJ, Aaronson PI (2011) Key role of the RhoA/Rho kinase system in pulmonary hypertension. Pulm Pharmacol Ther 24:1–14
Conway AM, James AB, O’Kane EM, Rakhit S, Morris BJ (2004) Regulation of myosin light chain phosphorylation by RhoB in neuronal cells. Exp Cell Res 300:35–42
Dejana E, Tournier-Lasserve E, Weinstein BM (2009) The control of vascular integrity by endothelial cell junctions: molecular basis and pathological implications. Dev Cell 16:209–221
Derangeon M, Spray DC, Bourmeyster N, Sarrouilhe D, Hervé JC (2009) Reciprocal influence of connexins and apical junction proteins on their expressions and functions. Biochim Biophys Acta 1788:768–778
Dudek SM, Jacobson JR, Chiang ET, Birukov KG, Wang P, Zhan X, Garcia JG (2004) Pulmonary endothelial cell barrier enhancement by sphingosine 1-phosphate: roles for cortactin and myosin light chain kinase. J Biol Chem 279:24692–24700
Fernandez-Borja M, Janssen L, Verwoerd D, Hordijk P, Neefjes J (2005) RhoB regulates endosome transport by promoting actin assembly on endosomal membranes through Dia1. J Cell Sci 118:2661–2670
Fukumoto Y, Shimokawa H (2011) Recent progress in the management of pulmonary hypertension. Circ J 75:1801–1810
Furman C, Sieminski AL, Kwiatkowski AV, Rubinson DA, Vasile E, Bronson RT, Fässler R, Gertler FB (2007) Ena/VASP is required for endothelial barrier function in vivo. J Cell Biol 179:761–775
Gao J, Liao J, Yang GY (2009) CAAX-box protein, prenylation process and carcinogenesis. Am J Transl Res 3:312–325
Garcia JG, Liu F, Verin AD, Birukova A, Dechert MA, Gerthoffer WT, Bamberg JR, English D (2001) Sphingosine 1-phosphate promotes endothelial cell barrier integrity by Edg-dependent cytoskeletal rearrangement. J Clin Invest 108:689–701
Gavard J, Gutkind JS (2006) VEGF controls endothelial-cell permeability by promoting the beta-arrestin-dependent endocytosis of VE-cadherin. Nat Cell Biol 8:1223–1234
Gorbunov NV, Atkins JL, Gurusamy N, Pitt BR (2012) Iron-induced remodeling in cultured rat pulmonary artery endothelial cells. Biometals 25:203–217
Gorovoy M, Neamu R, Niu J, Vogel S, Predescu D, Miyoshi J, Takai Y, Kini V, Mehta D, Malik AB, Voyno-Yasenetskaya T (2007) RhoGDI-1 modulation of the activity of monomeric RhoGTPase RhoA regulates endothelial barrier function in mouse lungs. Circ Res 101:50–58
Hall A (1998) Rho GTPases and the actin cytoskeleton. Science 279:509–514
Hall A, Lalli G (2010) Rho and Ras GTPases in axon growth, guidance, and branching. Cold Spring Harb Perspect Biol 2:a001818
Heo J, Raines KW, Mocanu V, Campbell SL (2006) Redox regulation of RhoA. Biochemistry 45:14481–14489
Hirota K, Semenza GL (2001) Rac1 activity is required for the activation of hypoxia-inducible factor 1. J Biol Chem 276:21166–21172
Hordijk PL (2006) Regulation of NADPH oxidases: the role of Rac proteins. Circ Res 98:453–462
Huang M, Duhadaway JB, Prendergast GC, Laury-Kleintop LD (2007) RhoB regulates PDGFR-beta trafficking and signaling in vascular smooth muscle cells. Arterioscler Thromb Vasc Biol 27:2597–2605
Huelsenbeck SC, Roggenkamp D, May M, Huelsenbeck J, Brakebusch C, Rottner K, Ladwein M, Just I, Fritz G, Schmidt G, Genth H (2013) Expression and cytoprotective activity of the small GTPase RhoB induced by the Escherichia coli cytotoxic necrotizing factor 1. Int J Biochem Cell Biol 45:1767–1775
Jaffe AB, Hall A (2005) Rho GTPases: biochemistry and biology. Annu Rev Cell Dev Biol 21:247–269
Kajimoto H, Hashimoto K, Bonnet SN, Haromy A, Harry G, Moudgil R, Nakanishi T, Rebeyka I, Thébaud B, Michelakis ED, Archer SL (2007) Oxygen activates the Rho/Rho-kinase pathway and induces RhoB and ROCK-1 expression in human and rabbit ductus arteriosus by increasing mitochondria-derived reactive oxygen species: a newly recognized mechanism for sustaining ductal constriction. Circulation 115:1777–1788
Knock GA, Shaifta Y, Snetkov VA, Vowles B, Drndarski S, Ward JP, Aaronson PI (2008) Interaction between src family kinases and rho-kinase in agonist-induced Ca2+−sensitization of rat pulmonary artery. Cardiovasc Res 77:570–579
Kouklis P, Konstantoulaki M, Vogel S, Broman M, Malik AB (2004) Cdc42 regulates the restoration of endothelial barrier function. Circ Res 94:159–166
Krause M, Dent EW, Bear JE, Loureiro JJ, Gertler FB (2003) Ena/VASP proteins: regulators of the actin cytoskeleton and cell migration. Annu Rev Cell Dev Biol 19:541–564
Kumar P, Shen Q, Pivetti CD, Lee ES, Wu MH, Yuan SY (2009) Molecular mechanisms of endothelial hyperpermeability: implications in inflammation. Expert Rev Mol Med 11:e19
Lang P, Gesbert F, Delespine-Carmagnat M, Stancou R, Pouchelet M, Bertoglio J (1996) Protein kinase A phosphorylation of RhoA mediates the morphological and functional effects of cyclic AMP in cytotoxic lymphocytes. EMBO J 15:510–519
Lu Q, Sakhatskyy P, Grinnell K, Newton J, Ortiz M, Wang Y, Sanchez-Esteban J, Harrington EO, Rounds S (2011) Cigarette smoke causes lung vascular barrier dysfunction via oxidative stress-mediated inhibition of RhoA and focal adhesion kinase. Am J Physiol Lung Cell Mol Physiol 301:L847–L857
Lu Q, Newton J, Hsiao V, Shamirian P, Blackburn MR, Pedroza M (2012) Sustained adenosine exposure causes lung endothelial barrier dysfunction via nucleoside transporter-mediated signaling. Am J Respir Cell Mol Biol 47:604–613
Ma Z, Li J, Yang L, Mu Y, Xie W, Pitt B, Li S (2004) Inhibition of LPS- and CpG DNA-induced TNF-alpha response by oxidized phospholipids. Am J Physiol Lung Cell Mol Physiol 286:L808–L816
Maniatis NA, Orfanos SE (2008) The endothelium in acute lung injury/acute respiratory distress syndrome. Curr Opin Crit Care 14:22–30
McVerry BJ, Peng X, Hassoun PM, Sammani S, Simon BA, Garcia JG (2004) Sphingosine 1-phosphate reduces vascular leak in murine and canine models of acute lung injury. Am J Respir Crit Care Med 170:987–993
Mehta D, Konstantoulaki M, Ahmmed GU, Malik AB (2005) Sphingosine 1-phosphate-induced mobilization of intracellular Ca2+ mediates rac activation and adherens junction assembly in endothelial cells. J Biol Chem 280:17320–17328
Milara J, Ortiz JL, Juan G, Guijarro R, Almudever P, Martorell M, Morcillo EJ, Cortijo J (2010) Cigarette smoke exposure up-regulates endothelin receptor B in human pulmonary artery endothelial cells: molecular and functional consequences. Br J Pharmacol 161:1599–1615
Millatt LJ, Whitley GS, Li D, Leiper JM, Siragy HM, Carey RM, Johns RA (2003) Evidence for dysregulation of dimethylarginine dimethylaminohydrolase I in chronic hypoxia-induced pulmonary hypertension. Circulation 108:1493–1498
Munder A, Zelmer A, Schmiedl A, Dittmar KE, Rohde M, Dorsch M, Otto K, Hedrich HJ, Tümmler B, Weiss S, Tschernig T (2005) Murine pulmonary infection with Listeria monocytogenes: differential susceptibility of BALB/c, C57BL/6 and DBA/2 mice. Microbes Infect 7:600–611
Nagasawa K, Chiba H, Fujita H, Kojima T, Saito T, Endo T, Sawada N (2006) Possible involvement of gap junctions in the barrier function of tight junctions of brain and lung endothelial cells. J Cell Physiol 208:123–132
Nonas S, Miller I, Kawkitinarong K, Chatchavalvanich S, Gorshkova I, Bochkov VN, Leitinger N, Natarajan V, Garcia JG, Birukov KG (2006) Oxidized phospholipids reduce vascular leak and inflammation in rat model of acute lung injury. Am J Respir Crit Care Med 173:1130–1138
Nonas S, Birukova AA, Fu P, Xing J, Chatchavalvanich S, Bochkov VN, Leitinger N, Garcia JG, Birukov KG (2008) Oxidized phospholipids reduce ventilator-induced vascular leak and inflammation in vivo. Crit Care 12:R27
Parthasarathi K, Quadri SK (2009) Cadherins and connexins in pulmonary endothelial function. In: Voelkel NF, Rounds S (eds) The pulmonary endothelium: function in health and disease. Wiley, Chichester, pp 33–50
Parthasarathi K, Ichimura H, Monma E, Lindert J, Quadri S, Issekutz A, Bhattacharya J (2006) Connexin 43 mediates spread of Ca2+−dependent proinflammatory responses in lung capillaries. J Clin Invest 116:2193–2200
Partovian C, Adnot S, Raffestin B, Louzier V, Levame M, Mavier IM, Lemarchand P, Eddahibi S (2000) Adenovirus-mediated lung vascular endothelial growth factor overexpression protects against hypoxic pulmonary hypertension in rats. Am J Respir Cell Mol Biol 23:762–771
Pedersen E, Brakebusch C (2012) Rho GTPase function in development: how in vivo models change our view. Exp Cell Res 318:1779–1787
Pullamsetti S, Kiss L, Ghofrani HA, Voswinckel R, Haredza P, Klepetko W, Aigner C, Fink L, Muyal JP, Weissmann N, Grimminger F, Seeger W, Schermuly RT (2005) Increased levels and reduced catabolism of asymmetric and symmetric dimethylarginines in pulmonaryhypertension. FASEB J 19:1175–1177
Ramchandran R, Mehta D, Vogel SM, Mirza MK, Kouklis P, Malik AB (2008) Critical role of Cdc42 in mediating endothelial barrier protection in vivo. Am J Physiol Lung Cell Mol Physiol 295:L363–L369
Repp H, Pamukçi Z, Koschinski A, Domann E, Darji A, Birringer J, Brockmeier D, Chakraborty T, Dreyer F (2002) Listeriolysin of Listeria monocytogenes forms Ca2+−permeable pores leading to intracellular Ca2+ oscillations. Cell Microbiol 4:483–491
Ridley AJ (2001) Rho GTPases and cell migration. J Cell Sci 114:2713–2722
Rodriguez PL, Sahay S, Olabisi OO, Whitehead IP (2007) ROCK I-mediated activation of NF-kappaB by RhoB. Cell Signal 19:2361–2369
Rolli-Derkinderen M, Sauzeau V, Boyer L, Lemichez E, Baron C, Henrion D, Loirand G, Pacaud P (2005) Phosphorylation of serine 188 protects RhoA from ubiquitin/proteasome-mediated degradation in vascular smooth muscle cells. Circ Res 96:1152–1160
Rose F, Zeller SA, Chakraborty T, Domann E, Machleidt T, Kronke M, Seeger W, Grimminger F, Sibelius U (2001) Human endothelial cell activation and mediator release in response to Listeria monocytogenes virulence factors. Infect Immun 69:897–905
Sakai H, Fujita A, Watanabe A, Chiba Y, Kamei J, Misawa M (2011) Different effects of smoke from heavy and light cigarettes on the induction of bronchial smooth muscle hyperresponsiveness in rats. J Smooth Muscle Res 47:1–10
Sauzeau V, Le Jeune H, Cario-Toumaniantz C, Smolenski A, Lohmann SM, Bertoglio J, Chardin P, Pacaud P, Loirand G (2000) Cyclic GMP-dependent protein kinase signaling pathway inhibits RhoA-induced Ca2+ sensitization of contraction in vascular smooth muscle. J Biol Chem 275:21722–21729
Sauzeau V, Rolli-Derkinderen M, Marionneau C, Loirand G, Pacaud P (2003) RhoA expression is controlled by nitric oxide through cGMP-dependent protein kinase activation. J Biol Chem 278:9472–9480
Sawada N, Salomone S, Kim HH, Kwiatkowski DJ, Liao JK (2008) Regulation of endothelial nitric oxide synthase and postnatal angiogenesis by Rac1. Circ Res 103:360–368
Schermuly RT, Ghofrani HA, Wilkins MR, Grimminger F (2011) Mechanisms of disease: pulmonary arterial hypertension. Nat Rev Cardiol 8:443–455
Schlegel N, Burger S, Golenhofen N, Walter U, Drenckhahn D, Waschke J (2008) The role of VASP in regulation of cAMP- and Rac 1-mediated endothelial barrier stabilization. Am J Physiol Cell Physiol 294:C178–C188
Seebach J, Mädler HJ, Wojciak-Stothard B, Schnittler HJ (2005) Tyrosine phosphorylation and the small GTPase rac cross-talk in regulation of endothelial barrier function. Thromb Haemost 94:620–629
Sen P, Gopalakrishnan R, Kothari H, Keshava S, Clark CA, Esmon CT, Pendurthi UR, Rao LV (2011) Factor VIIa bound to endothelial cell protein C receptor activates protease activated receptor-1 and mediates cell signaling and barrier protection. Blood 117:3199–3208
Shikata Y, Rios A, Kawkitinarong K, DePaola N, Garcia JG, Birukov KG (2005) Differential effects of shear stress and cyclic stretch on focal adhesion remodeling, site-specific FAK phosphorylation, and small GTPases in human lung endothelial cells. Exp Cell Res 304:40–49
Skuli N, Monferran S, Delmas C, Lajoie-Mazenc I, Favre G, Toulas C, Cohen-Jonathan-Moyal E (2006) Activation of RhoB by hypoxia controls hypoxia-inducible factor-1alpha stabilization through glycogen synthase kinase-3 in U87 glioblastoma cells. Cancer Res 66:482–489
Somlyo AP, Somlyo AV (2003) Ca2+ sensitivity of smooth muscle and nonmuscle myosin II: modulated by G proteins, kinases, and myosin phosphatase. Physiol Rev 83:1325–1358
Spindler V, Schlegel N, Waschke J (2010) Role of GTPases in control of microvascular permeability. Cardiovasc Res 87:243–253
Stan RV (2009) Anatomy of the pulmonary endothelium. In: Voelkel N, Rounds S (eds) The pulmonary endothelium: function in health and disease. Wiley, Chichester, pp 25–32
Stockton RA, Schaefer E, Schwartz MA (2004) p21-activated kinase regulates endothelial permeability through modulation of contractility. J Biol Chem 279:46621–46630
Stockton R, Reutershan J, Scott D, Sanders J, Ley K, Schwartz MA (2007) Induction of vascular permeability: beta PIX and GIT1 scaffold the activation of extracellular signal-regulated kinase by PAK. Mol Biol Cell 18:2346–2355
Storck EM, Wojciak-Stothard B (2013) Rho GTPases in pulmonary vascular dysfunction. Vascul Pharmacol 58:202–210
Szulcek R, Beckers CM, Hodzic J, de Wit J, Chen Z, Grob T, Musters RJ, Minshall RD, van Hinsbergh VW, van Nieuw Amerongen GP (2013) Localized RhoA GTPase activity regulates dynamics of endothelial monolayer integrity. Cardiovasc Res 99:471–482
Takemoto M, Sun J, Hiroki J, Shimokawa H, Liao JK (2002) Rho-kinase mediates hypoxia-induced downregulation of endothelial nitric oxide synthase. Circulation 106:57–62
Tsang H, Leiper J, Lao KH, Dowsett L, Delahaye MW, Barnes G, Wharton J, Howard L, Iannone L, Lang NN, Wilkins MR, Wojciak-Stothard B (2014) Role of asymmetric methylarginine and connexin 43 in the regulation of pulmonary endothelial function. Pulm Circ (in press)
Tuder RM, Yun JH (2008) Vascular endothelial growth factor of the lung: friend or foe. Curr Opin Pharmacol 8:255–260
Tuder RM, Kasahara Y, Voelkel NF (2000) Inhibition of vascular endothelial growth factor receptors causes emphysema in rats.Chest 117:281S
van der Heijden M, van Nieuw Amerongen GP, van Bezu J, Paul MA, Groeneveld AB, van Hinsbergh VW (2011) Opposing effects of the angiopoietins on the thrombin-induced permeability of human pulmonary microvascular endothelial cells. PLoS One 6:e23448
van Kempen MJ, Jongsma HJ (1999) Distribution of connexin37, connexin40 and connexin43 in the aorta and coronary artery of several mammals. Histochem Cell Biol 112:479–486
van Nieuw Amerongen GP, Beckers CM, Achekar ID, Zeeman S, Musters RJ, van Hinsbergh VW (2007) Involvement of Rho kinase in endothelial barrier maintenance. Arterioscler Thromb Vasc Biol 27:2332–2339
Vardouli L, Vasilaki E, Papadimitriou E, Kardassis D, Stournaras C (2008) A novel mechanism of TGFbeta-induced actin reorganization mediated by Smad proteins and Rho GTPases. FEBS J 275:4074–4087
Vasioukhin V, Fuchs E (2001) Actin dynamics and cell-cell adhesion in epithelia. Curr Opin Cell Biol 13:76–84
Vega FM, Ridley AJ (2008) Rho GTPases in cancer cell biology. FEBS Lett 582:2093–2101
Vouret-Craviari V, Bourcier C, Boulter E, van Obberghen-Schilling E (2002) Distinct signals via Rho GTPases and Src drive shape changes by thrombin and sphingosine-1-phosphate in endothelial cells. J Cell Sci 115:2475–2484
Wang L, Dudek SM (2009) Regulation of vascular permeability by sphingosine 1-phosphate. Microvasc Res 77:39–45
Wang Z, Jin N, Ganguli S, Swartz DR, Li L, Rhoades RA (2001) Rho-kinase activation is involved in hypoxia-induced pulmonary vasoconstriction. Am J Respir Cell Mol Biol 25:628–635
Weis SM (2008) Vascular permeability in cardiovascular disease and cancer. Curr Opin Hematol 15:243–249
West JB (2013) Role of the fragility of the pulmonary blood-gas barrier in the evolution of the pulmonary circulation. Am J Physiol Regul Integr Comp Physiol 304:R171–R176
Wojciak-Stothard B (2008) New drug targets for pulmonary hypertension: Rho GTPases in pulmonary vascular remodelling. Postgrad Med J 84:348–353
Wojciak-Stothard B, Ridley AJ (2002) Rho GTPases and the regulation of endothelial permeability. Vascul Pharmacol 39:187–199
Wojciak-Stothard B, Tsang LY, Haworth SG (2005) Rac and Rho play opposing roles in the regulation of hypoxia/reoxygenation-induced permeability changes in pulmonary artery endothelial cells. Am J Physiol Lung Cell Mol Physiol 288:L749–L760
Wojciak-Stothard B, Tsang LY, Paleolog E, Hall SM, Haworth SG (2006) Rac1 and RhoA as regulators of endothelial phenotype and barrier function in hypoxia-induced neonatal pulmonary hypertension. Am J Physiol Lung Cell Mol Physiol 290:L1173–L1182
Wojciak-Stothard B, Torondel B, Tsang LY, Fleming I, Fisslthaler B, Leiper JM, Vallance P (2007) The ADMA/DDAH pathway is a critical regulator of endothelial cell motility. J Cell Sci 120:929–942
Wojciak-Stothard B, Torondel B, Zhao L, Renné T, Leiper JM (2009) Modulation of Rac1 activity by ADMA/DDAH regulates pulmonary endothelial barrier function. Mol Biol Cell 20:33–42
Wojciak-Stothard B, Zhao L, Oliver E, Dubois O, Wu Y, Kardassis D, Vasilaki E, Huang M, Mitchell JA, Harrington LS, Louise H, Prendergast GC, Wilkins MR (2012) Role of RhoB in the regulation of pulmonary endothelial and smooth muscle cell responses to hypoxia. Circ Res 110:1423–1434
Xiong C, Yang G, Kumar S, Aggarwal S, Leustik M, Snead C, Hamacher J, Fischer B, Umapathy NS, Hossain H, Wendel A, Catravas JD, Verin AD, Fulton D, Black SM, Chakraborty T, Lucas R (2010) The lectin-like domain of TNF protects from listeriolysin-induced hyperpermeability in human pulmonary microvascular endothelial cells—a crucial role for protein kinase C-alpha inhibition. Vascul Pharmacol 52:207–213
Zhao YD, Ohkawara H, Rehman J, Wary KK, Vogel SM, Minshall RD, Zhao YY, Malik AB (2009) Bone marrow progenitor cells induce endothelial adherens junction integrity by sphingosine-1-phosphate-mediated Rac1 and Cdc42 signaling. Circ Res 105:696–704
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Duluc, L., Wojciak-Stothard, B. Rho GTPases in the regulation of pulmonary vascular barrier function. Cell Tissue Res 355, 675–685 (2014). https://doi.org/10.1007/s00441-014-1805-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-014-1805-0