Abstract
We develop “autologous bone marrow cell infusion (ABMi) therapy” for the treatment of human decompensated liver cirrhosis and confirm the efficacy and safety of this treatment in multicenter clinical studies. With the goal of further expanding the applications of ABMi, we first cultured human bone marrow cells and then determined whether a cell fraction found to be effective in improving liver fibrosis can be amplified. Cells harvested after two passages (P2 cells) consistently contained approximately 94 % mesenchymal stem cells (MSCs); conversely, the cells harvested after only medium change (P0 cells) contained many macrophages. MSCs (2.8 × 108) in P2 cells were harvested from 3.8 × 108 bone marrow-derived mononuclear cells after 22 days. DNA-chip analysis also showed during the culturing step that bone marrow-derived cells decreased with macrophage phenotype. The infused 5 × 105 P2 cells significantly improved liver fibrosis in the nonobese diabetic/severe combined immunodeficient (NOD-SCID) mouse carbon tetrachloride (CCl4) liver cirrhosis model and induced the expression of matrix metalloproteinase (MMP)-9 and suppressed expressions of alpha smooth muscle actin (αSMA), tumor necrosis factor alpha (TNFα) and transforming growth factor beta (TGFβ) in the liver. Cultured human bone marrow-derived cells (P2 cells) significantly inhibited liver fibrosis. The increase of MMP-9 and suppressed activation of hepatic stellate cells (HSCs) through the regulation of humoral factors (TNFα and TGFβ) contribute to the improvement of liver fibrosis by MSCs comprising about 94 % of P2 cells. MSCs in cultured human bone marrow-derived mono-nuclear cells (BM-MNCs) proliferate sufficiently in cell therapy, so we believe our cultured bone marrow-derived cell therapy can lead to expanded clinical applications and enable outpatient therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the past, fluorescence in situ hybridization has been used to confirm the presence of the Y chromosome in liver and gastrointestinal tissues in autopsies of patients (XX) with blood disorders who had undergone bone marrow grafts (XY) and these findings suggested the presence of pluripotent stem cells in bone marrow cells (Alison et al. 2000; Theise et al. 2000). In addition, adherent cells (CD90+, CD44+ CD14−, CD34− and CD45−) have been isolated from human bone marrow aspirate, which suggests that these pluripotent cells are MSCs (Pittenger et al. 1999).
In our laboratory, we began basic research in mice concerning autologous bone marrow cell infusion (ABMi) therapy for liver cirrhosis by focusing on the presence in bone marrow of these pluripotent cells that engraft in the liver. We established a “murine green fluorescent protein (GFP)/CCl4 model” to evaluate bone marrow cell differentiation and proliferation in liver cirrhosis (Terai et al. 2003). We found that liver fibrosis was improved in the same liver cirrhosis model because the infused bone marrow cells produce MMP-9 and other substances (Sakaida et al. 2004). Using the results of this basic research in mice as a foundation, in 2003, we began a clinical study entitled “ABMi therapy for decompensated liver cirrhosis” and we were the first to report on the efficacy and safety of this therapy (Terai et al. 2006). In joint research with this laboratory, researchers at Yonsei University in Korea have recently found that the therapeutic effect of ABMi lasts for at least 1 year in patients with hepatitis B-induced liver cirrhosis (Kim et al. 2010). In addition, in joint research with Yamagata University, we found that improved liver function in patients with alcoholic liver cirrhosis continues for 6 months after ABMi therapy (Saito et al. 2011). Cell therapy using bone marrow cells is a promising therapy for liver cirrhosis (Terai et al. 2012; Takami et al. 2012).
However, current ABMi therapy requires the collection of bone marrow aspirate under general anesthesia, so there are strict usage criteria regarding the general health condition of patients. Therefore, with the goal of expanding the therapeutic applications of ABMi, in our laboratory, we cultured human bone marrow cells and evaluated whether the cell fraction that has an improving effect on liver fibrosis can be amplified. We found that, from the standpoint of growth capability and pluripotency, the second passage (P2) cells comprise a fraction that is clearly more important for liver cirrhosis therapy. In addition, we set out to analyze the mechanism of liver fibrosis improvement using mouse livers in which an improvement in fibrosis brought about by cell infusion had already been confirmed. Here, we report our findings on the effect on liver fibrosis of cultured human bone marrow-derived cells.
Materials and methods
Preparation of culture of human BM-MNCs and human MSCs
Human BM-MNCs (Code:2M-125A, male, HIV/HBV/HCV-negative) were purchased from Lonza (Basel, Switzerland). Human BM-MNCs were cultured in Dulbecco’s Modified Eagle’s Medium (DMEM) (GIBCO, NY, USA) supplemented with 10 % fetal bovine serum (FBS) (GIBCO) and penicillin/streptomycin (GIBCO) on non-coated dishes (Becton and Dickinson, NJ, USA). Human BM-MNCs were plated at a density of 1 × 106 cells/cm2 and incubated at 37 °C with 5 % CO2. After 20–23 days culture, proliferated cells grown under only medium change every 3 days (P0 cells) or through two successive passages on days 10–13 and 5 additional days before confluence (P2 cells) were harvested (Fig. 1a). The cells were detached with trypsin-EDTA (0.05 % trypsin, 0.53 mM EDTA-4Na) (GIBCO) for 5 min at 37 °C. Human MSCs were cultured in the same manner and 2–3 successive passages were performed. Before infusion, these cells were trypsinized and washed twice with phosphate-buffered saline (PBS) (GIBCO).
The majority of cultured human bone marrow-derived mono nuclear cells (BM-MNCs) (P2 cells) were phenotypically mesenchymal stem cells (MSCs). a Human BM-MNCs (hBM) were plated at a density of 1 × 106 cells/cm2 on non-coated dishes in 10 % FBS-DMEM and incubated. After 20–23 days of culture, proliferated cells with only medium change every 3 days (P0 cells) or two successive passages on days 10–13 and 5 additional days before confluence (P2 cells) were harvested. b–d Cellular characteristics of P0 cells. Typical data from analysis by flow cytometry are shown. P0 cells were approximately fractionated into two subgroups: MSCs and macrophages. CD45 (+) cells (hematopoietic cells) accounted for 43.1 % of P0 cells and macrophages (CD45 and CD11b positive and CD90 (−) cells) accounted for 34.9 %; conversely, 51.8 % were MSCs (CD45 (−) and CD90, CD105, and CD73 positive). e–g Cellular characteristics of P2 cells. In contrast to P0 cells, the majority of cultured human BM-MNCs after two passages (P2) were MSCs (95.5 %), 2.6 % were CD45 (+) cells, and 0.2 % were macrophages. h On the photomicrograph (×100), P0 cells were contaminated with many round hematopoietic cells. Conversely, i on the photomicrograph (×100), P2 cells were homogenous fibroblastic-shaped cells. j The mean MSC percentage of P2 cells from four healthy men was 94.1 ± 2.6 % and individual differences were small. k After 13 days of plating of human BM-MNCs at a density of 1 × 106 cells/cm2 (3.8 × 106 cells/3.8 cm2) and incubation in 10 % FBS-DMEM, adhesive cells had proliferated to 0.7 ± 0.3 × 105 cells/3.8 cm2 (n = 5) and under two successive passages (P2) grew to 28.3 ± 15.9 × 105 cells/3.8 cm2 (n = 5)
Characterization of cultured human BM-MNCs
The cell marker expressions of P0 and P2 cells were analyzed by flow cytometry (FACS Calibur; Becton and Dickinson). Cells were stained using the following preconjugated antibodies: CD45, CD90, CD105 (eBioscience, CA, USA), CD73 and CD11b (Beckman Coulter, CA, USA). Through fluorescence-activated cell sorting analysis, the phenotypical MSC ratio (%) was examined. P2 cells were stained with additional antibodies to confirm MSC phenotypically: CD34, CD13, CD45, CD73, CD90, HLA-DR, HLA-ABC, iso IgG (BD Pharmingen, CA, USA), CD44, CD105, CD11b (Beckman Coulter) and CD117 (Beckton and Dickinson).
Differentiation and DNA-chip analysis
P2 cells were cultured with each differentiation medium and evaluated for adipogenesis (Oil-Red O, anti-mouse FABP-4 antibody), osteogenesis (Alizarin Red) and chondrogenesis (anti-human aggrecan antibody) with a human MSC functional identification kit (Invitrogen, NY, USA). We compared DNA expression between P0 and P2 cells using the DNA-chip system (Agilent Technology, CA, USA). We next also analyzed the expression pattern using the IPA software system (Ingenuity Systems, CA, USA).
Experimental protocol for the NOD-SCID mouse CCl4 liver cirrhosis model
All animals received humane care and the experiments were approved by the Animal Experiment Committee of Yamaguchi University School of Medicine according to the National Institutes of Health criteria. NOD.CB17-Prkdcsscid/J female mice 5 weeks of age purchased from Charles River Laboratories (MA, USA) were properly anesthetized during the experiments.
NOD.CB17-Prkdcsscid/J female mice 6 weeks of age were treated with CCl4 (Wako, Tokyo, Japan) dissolved in corn oil (Wako) (1:3) twice a week for 6 weeks, only once with 0.5 mL/kg body (0.25 μg/g) CCl4, from the second time with 1.0 mL/kg body weight (0.5 μg/g), and for the last 4 weeks with 1.5 mL/kg body weight (0.75 μg/g). These were used as the control group of the NOD-SCID mouse CCl4 liver cirrhosis model. Treatment with 1.5 mL/kg body weight CCl4 was continued for a further 4 weeks. Then, 5.0 × 105 P2 cells for the P2-administration group (n = 18) and 5.0 × 105 P0 cells for the P0-administration group (n = 7) were infused through the tail vein, while in the control group (n = 13), only PBS was injected.
Quantitative analysis of liver fibrosis
After 4 weeks of administration of P2 or P0 cells, the livers of the NOD-SCID mouse CCl4 liver cirrhosis model were fixed in 4 % formaldehyde and 3-μm paraffin sections were used for analysis. The liver fibrosis area was quantified with Sirius red staining and assessed by application software (BIOREVO microscope BZ-9000, BZ-II; KEYENCE, Osaka, Japan) at a magnification of ×100. The mean value of 10 randomly selected areas per sample was used as the expressed percent area of fibrosis.
Immunohistochemistry of MMP-9 and αSMA
Three-micrometer paraffin sections of livers 2 or 4 weeks after administration of P2 cells were used for immunostaining. MMP-9 and αSMA detection required antigen retrieval with Vector Antigen Unmasking Solution (Vector Laboratories, CA, USA) and the bound antibodies were detected using the avidin-biotin complex method staining kit (Vector Laboratories). Primary antibodies were used at the following dilutions: 1:100 for MMP-9 (R and D Systems, MN, USA) and 1:300 for αSMA (Abcam, Cambridge, UK). Biotinylated antibody was used as the secondary antibody. The number of MMP-9(+) cells was counted at a magnification of ×200 and the mean value of six randomly selected areas per sample was assessed. The αSMA(+) area (%) was quantified at a magnification of ×100 and the mean value of ten randomly selected areas per sample was assessed. The same application software described above was used.
Quantification of messenger RNA levels by real-time reverse-transcription polymerase chain reaction (PCR)
Total RNA was extracted from the liver of mice 4 weeks after P2 cell infusion using RNA extraction solution (ISOGEN; Nippon Gene, Tokyo, Japan) and complementary DNA was generated from 500 ng of RNA using a Transcriptor First Strand cDNA Synthesis Kit (Roche Applied Science, IN, USA). Primers for the messenger RNA (mRNA) expression of MMP-9, αSMA, TNFα and TGFβ were evaluated using real-time PCR. Real-time PCR was performed with SYBR Green Master Mix (Roche Diagnostic, Basel, Switzerland). The primers used for MMP-9 were 5’-TCT CTA CGG CCG GCT TTG CT-3’ (forward) and 5’-GGC AAG TCT TCA GAG TAG TT-3’ (reverse), those for αSMA were 5’-ACT CTC TTC CAG CCA TCT TTC A-3’ (forward) and 5’-ATA GGT GGT TTC GTG GAT GC-3’ (reverse), those for TNFα were 5’-CAG GTT CTG TCC CTT TCA CTC ACT-3’ (forward) and 5’-GTT CAG TAG ACA GAA GAG CGT GGT-3’ (reverse), those for TGFβ1 were 5’-TGG AGC AAC ATG TGG AAC TC-3’ (forward) and 5’-CAG CAG CCG GTT ACC AAG-3’ (reverse) and those for β-actin were 5’-TGA CAG GAT GCA GAA GGA GA-3’ (forward) and 5’-GCT GGA AGG TGG ACA GTG AG-3’ (reverse).
Statistics
Data are presented as mean ± standard error of the mean. The two-tailed Student’s t test was used to analyze parametric data.
Results
The majority of P2 cells were phenotypically and functionally MSCs
Cultured human BM-MNCs without passage (P0 cells) were approximately fractionated into two subgroups: MSCs and macrophages. CD45 (+) cells (hematopoietic cells) accounted for 43.1 % of P0 cells and macrophages [CD45 and CD11b positive and CD90 (−) cells] accounted for 34.9 %; conversely, 51.8 % were MSCs [CD45 (−) and CD90, CD105 and CD73 positive] (Fig. 1b–d). In contrast to P0 cells, the majority of cultured human BM-MNCs under two passages (P2 cells) were MSCs (95.5 %), 2.6 % were CD45 (+) cells and only 0.2 % were macrophages (Fig. 1e–g). On the photomicrograph (×100), P0 cells were contaminated with many round hematopoietic cells; conversely, P2 cells were homogenous fibroblastic-shaped cells (Fig. 1h–i). The mean MSC percentage of P2 cells from four healthy men were 94.1 ± 2.6 % and individual differences were small (Fig. 1j). After 13 days of plating of human BM-MNCs at a density of 1 × 106 cells/cm2 (3.8 × 106 cells/3.8 cm2) and incubation in 10 % FBS-DMEM, adhesive cells grew to 0.7 ± 0.3 × 105 cells/3.8 cm2 (n = 5) and, under two successive passages, P2 cells grew to 28.3 ± 15.9 × 105 cells/3.8 cm2 (n = 5) (Fig. 1k). The phenotypical character of P2 cells was consistent with that of MSCs. Hematopoietic stem cell marker (CD34)-positive cells in P2 cells accounted for only 0.06 % (Fig. 2a). P2 cells differentiated into adipocytes, osteocytes and chondrocytes (Fig. 2b–e).
P2 cells were phenotypically and functionally mesenchymal stem cells (MSCs). a The phenotypical character of P2 cells was consistent with that of MSCs. Hematopoietic stem cell marker (CD34)-positive cells in P2 cells were only 0.06 %. b–e P2 cells (×200) (b) differentiated into adipocytes (×200) (c), osteocytes(×200) (d), and chondrocytes (× 40) (e). The control group cells (b) were cultured in only 10 % FBS-DMEM. f Category of up-regulated genes in P2 cells than those in P0 cells. g Category of down-regulated genes in P0 cells than those in P2 cells
Comparison of DNA expressions between P2 cells and P0 cells
We performed DNA-chip analysis using an IPA system. The majority gene that is upregulated is 1,569 probe. In P2 cells, genes related with cell cycle, G2/M DNA damage checkpoint regulated genes were up-regulated. On the other hand, genes related with function of blood cells, proliferation of blood cells and leukocyte migration were down-regulated, indicating that the macrophage fraction was decreased (Fig. 2f, g). Moreover, in P2 cells, we also confirmed that many clusters of differentiation (CD) markers related to monocytes and lymphocytes were down-regulated, consistent with the decreased macrophage phenotype in P2 cells (Table 1).
Cultured human bone marrow-derived cell (P2 cells) infusion improves liver fibrosis
P2 cells (5 × 105) infused into the liver cirrhosis model mice resulted in a significant reduction in fibrosis measured by Sirius red quantification after 4 weeks of the infusion (Fig. 3a). The infusion of P2 cells improved liver fibrosis in this liver fibrosis model [P = 0.009, **P < 0.01, 1.5 ± 0.5 % (n = 11) vs. control 2.6 ± 1.1 % (n = 7); P = 0.048, # P < 0.05 vs. P0-administration group 2.2 ± 0.9 % (n = 7)] (Fig. 3b–f).
Advanced liver fibrosis was induced in NOD.CB17-Prkdcsscid/J mice by chronic administration of CCl4 (NOD-SCID mouse CCl4 liver cirrhosis model). Liver fibrosis in this model was improved by infusion of P2 cells. a NOD.CB17-Prkdcsscid/J female mice 6 weeks of age were treated with CCl4 dissolved in corn oil (1:3) twice a week for 6 weeks, only once with 0.5 mL/kg body weight CCl4, from the second time with 1.0 mL/kg body weight, and for the last 4 weeks with 1.5 mL/kg body weight. In the NOD-SCID mouse CCl4 liver cirrhosis model, P2 or P0 cells were infused. Treatment with 1.5 mL/kg body weight CCl4 was continued further for 4 weeks. b–c Photomicrograph showing Sirius red staining for hepatic collagens after 4 weeks 5 × 105 P2 cells infusion into the liver cirrhosis model mouse (×100) (c), and control PBS-infusion (×100) (b). d–e Photomicrograph of the right lobe of the liver (control group d and P2 cells infused group e) (original magnification ×100). f P2 cells (5 × 105) infused in the liver cirrhosis model mouse resulted in a significant reduction in fibrosis measured by Sirius red quantification after 4 weeks of infusion. The infusion of P2 cells improved liver fibrosis in this liver fibrosis model [P = 0.009, **P < 0.01, 1.5 ± 0.5 % (n = 11) vs. control 2.6 ± 1.1 % (n = 7); P = 0.048, # P < 0.05 vs. P0-administration group 2.2 ± 0.9 % (n = 7)]
Up-regulation of MMP-9 expression in P2 cells-infused cirrhosis liver
Messenger RNA expression of MMP-9, which degrades the extracellular matrix, in the liver after 4 weeks of infusion of P2 cells was significantly up-regulated [P = 0.003, **P < 0.01, MMP-9/β-actin 0.9 ± 0.5 (n = 6) vs. 0.2 ± 0.1 control (n = 6)] (Fig. 4a). P2 cells also significantly up-regulated MMP-9 protein expression in the liver after 2 and 4 weeks of P2 cell infusion [P = 0.031, *P < 0.05 and P = 0.047, *P < 0.05, MMP-9(+) cell number 9.2 ± 6.5 (n = 10) vs. 3.9 ± 1.7 control (n = 9), 9.2 ± 4.9 (n = 12) vs. 4.9 ± 3.5 control (n = 8), ×200] (Fig. 4b–h).
Matrix metalloproteinase (MMP)-9 expression in P2 cells infused cirrhosis liver was up-regulated. a mRNA expression of MMP-9 in the liver after 4 weeks of P2 cells infusion was significantly up-regulated [P = 0.003, **P < 0.01, MMP-9/β-actin 0.9 ± 0.5 (n = 6) vs. 0.2 ± 0.1 control (n = 6)]. b P2 cells also significantly up-regulated MMP-9 protein expression in the liver after 2 and 4 weeks of P2 cells-infusion [P = 0.031, *P < 0.05 and P = 0.047, *P < 0.05, MMP-9(+) cell number 9.2 ± 6.5 (n = 10) vs. 3.9 ± 1.7 control (n = 9), 9.2 ± 4.9 (n = 12) vs. 4.9 ± 3.5 control (n = 8)]. c–f Photomicrograph of MMP-9-positive cells in the liver after 2 weeks of P2 cells infusion (f) (original magnification ×400). Arrow indicated. IgG control of PBS group (c) and of P2 group (d) and MMP-9 expression of PBS control group (e). g–h Photomicrograph of MMP-9-positive cells in the liver 4 weeks after P2 cells infusion (h) (original magnification ×400). Arrow indicated. MMP-9 expression of PBS control (g)
Suppressed activation of hepatic stellate cells (HSCs) in P2 cells-infused cirrhosis liver
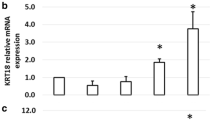
Messenger RNA expression of αSMA, a marker of activated HSCs, in the liver after 4 weeks of infusion of P2 cells was significantly reduced [P = 0.045, *P < 0.05, αSMA/β-actin 0.6;0.2 (n = 4) vs. 0.9;0.2 control (n = 6)] (Fig. 5a). The amount of αSMA staining [αSMA(+) area(%)] in the P2 cells infusion group decreased [P = 0.048, *P < 0.05, 1.0 ± 0.5 % (n = 8) vs. 2.0 ± 1.1 % control (n = 6), ×100] (Fig. 5b–d).
P2 cells delivery causes a reduction of alpha smooth muscle actin (αSMA)-positive hepatic stellate cells (HSCs). a mRNA expression of αSMA in the liver after 4 weeks of P2 cells infusion was significantly reduced [P = 0.045, *P < 0.05, αSMA/β-actin 0.6 ± 0.2 (n = 4) vs. 0.9 ± 0.2 control (n = 6)]. b The amount of αSMA staining [αSMA(+) area(%)] in the P2 cells-infused group decreased [P = 0.048, *P < 0.05, 1.0 ± 0.5 % (n = 8) vs. 2.0 ± 1.1 % control (n = 6)]. c–d Photomicrographs demonstrate the reduction in αSMA(+) HSCs after 4 weeks of P2 cells delivery (d) and PBS control (c) (original magnification ×100)
Reduction of TNFα and TGFβ in P2 cells recipients
Messenger RNA expression of TNFα, an inflammatory cytokine, in the liver after 4 weeks of P2 cells infusion was significantly reduced [P = 0.019, *P < 0.05, TNFα/β-actin 0.2 ± 0.1 (n = 8) vs. 2.3 ± 2.3 control (n = 9)] (Fig. 6a). Messenger RNA expression of TGFβ, which activates HSCs, in the liver after 4 weeks of P2 cells infusion was significantly reduced [P = 0.049, *P < 0.05, TGFβ/β-actin 0.9 ± 0.6 (n = 13) vs. 1.5 ± 1.0 control (n = 12)] (Fig. 6b).
P2 cells delivery causes a reduction of tumor necrosis factor alpha (TNFα) and transforming growth factor beta (TGFβ). a mRNA expression of TNFα, an inflammatory cytokine, in the liver after 4 weeks of P2 cells infusion was significantly reduced [P = 0.019, *P < 0.05, TNFα/β-actin 0.2 ± 0.1 (n = 8) vs. 2.3 ± 2.3 control (n = 9)]. b mRNA expression of TGFβ in the liver, which activates HSCs, after 4 weeks of P2 cells infusion was significantly reduced [P = 0.049, *P < 0.05, TGFβ/β-actin 0.9 ± 0.6 (n = 13) vs. 1.5 ± 1.0 control (n = 12)]
Discussion
We reported in 2004 that we had administered whole bone marrow cells from a GFP transgenic mouse to model mice with cirrhosis induced by repeated administration of CCl4 and that an improvement in liver fibrosis, accompanied by improvements in liver function and survival, was obtained with donor-derived bone marrow cells that adhered to the fibrotic regions of the cirrhotic livers and produced fibrolytic enzymes including MMP-9 (Sakaida et al. 2004). With regard to clinical research, we were the first in the world to begin ABMi therapy, in 2003 and we demonstrated that it improved liver function in patients with cirrhosis without serious adverse events. At that time, we also found an increase in the number of proliferating cell nuclear antigen-positive cells after infusion of the bone marrow (Terai et al. 2006). Furthermore, based on joint research with our laboratory, Kim et al. of Yonsei University reported that the efficacy of ABMi therapy continued for at least 1 year and that, in liver biopsies taken over time, activation of the hepatic progenitor cell fraction was confirmed (Kim et al. 2010). Additionally, based on joint research with our laboratory, Saito et al. of Yamagata University reported that, in patients with alcohol-induced liver cirrhosis, ABMi was effective in improving liver function and their findings indicated that bone marrow may activate this process (Saito et al. 2011). As noted above, ABMi therapy has been shown to improve the pathological condition of cirrhosis in human clinical research but the cell fraction necessary for this therapeutic effect is still unknown. Meanwhile, ABMi therapy has been limited in its application because it requires the collection of 400 mL of bone marrow aspirate under general anesthesia. In reports from other laboratories on cultured bone marrow cells, bone marrow-derived macrophages have been shown to improve liver fibrosis in studies using murine bone marrow cells (Thomas et al. 2011). The proportion of macrophages in murine bone marrow is inherently large and is also large in cultured bone marrow cells. It is possible that the liver fibrosis-improving effect of cultured murine bone marrow cells comes mainly from macrophages. We also performed analyses using a mice model and found that bone marrow cells easily differentiated macrophages and the infusion of the macrophage fraction improved liver fibrosis (Iwamoto et al. 2013; Phinney et al. 1999). Basically, in the mice model, macrophages are easily cultured (Phinney et al. 1999). Huang et al. showed that MSC is also effective in improving liver fibrosis (Huang et al. 2013). So, we believe that both macrophages and MSC might be important for improving liver fibrosis. These are mice data, so we analyzed and cultured human bone marrow cells and then determined whether a cell fraction with this fibrosis-improving effect could be amplified to set up a clinical study.
In anticipation of clinical use in humans, we cultured human BM-MNCs in a medium that contained only 10 % FBS without the addition of growth factors. We carried out subculturing twice and, after approximately 3 weeks, we obtained a sufficient number of cells to expect an effect on liver fibrosis. We collected populations of P2 cells with almost no individual differences, in which the cell fractions were stable and contained roughly 94 % MSCs, a few percent hematopoietic cells consisting mainly in macrophages and less than 0.1 % hematopoietic stem cells (Fig. 1b–i). We found that, in cultured human bone marrow cells, the main component of the P2 cells were MSCs and that there was a clear difference in the proportion of MSCs between P2 and P0. DNA-chip analysis also showed that bone marrow-derived cells also decreased the macrophage fraction. Therefore, the characteristics of culturable bone marrow-derived cells may differ between mice and humans.
Next, P2 cells were infused via the caudal vein and they significantly improved liver fibrosis in an immunodeficient liver cirrhosis mouse model (NOD-SCID mouse CCl4 liver cirrhosis model) that we developed for this study. Furthermore, we were also able to confirm that cultured human MSCs brought about a significant improvement in liver fibrosis using the same mouse model. Therefore, this study demonstrates that the liver fibrosis-improving effect in the cultured human bone marrow-derived cells originates in MSCs.
In human clinical research, Mohamadnejad and Kharaziha have shown that MSC from bone marrow can improve the pathological condition of liver cirrhosis by infusion both intravenously and via the portal vein (Mohamadnejad et al. 2007; Kharaziha et al. 2009). In addition, Pai et al. have demonstrated that liver function is improved when CD34-positive cells induced from bone marrow cells by granulocyte colony-stimulating factor are grown in vitro and then administered via the hepatic vein (Pai et al. 2008). In contrast, our research has demonstrated that a sufficient number of homogenous cells with almost no individual differences can be recovered after two passages of human BM-MNCs to which only serum was added without the involvement of growth factors, as well as that cultured cell infusion therapy, that can be expected to improve liver fibrosis, is possible through intravenous infusion. In addition, we developed an animal model that enables the evaluation of human cell function, proved the liver fibrosis-improving effect of MSCs in cultured human bone marrow-derived cells (P2) and demonstrated cultured cell collection conditions that are simple and provide a stable effect. In the future, we plan to assess cultured bone marrow-derived cell fractions from patients with liver cirrhosis and evaluate the effect on improving liver fibrosis in this animal model to enable the collection and infusion of even better cells and to determine the prognosis of therapeutic efficacy in patients.
In this study, we have shown that the mechanism of the improvement in liver fibrosis brought about by cultured human bone marrow-derived cells occurs via the enhanced expression of MMP-9, which is important for fibrolysis and a decrease in fiber production brought about by a decrease in HSC activity. Moreover, we have shown that this mechanism acts by controlling the production of cytokines such as TGFβ and TNFα. As shown in Fig. 6a, b, TNFα and TGFβ expressions were decreased. MSC infusion might induce the decrease of these cytokines and improve liver fibrosis. These results might be similar with our previous analysis and show rapid cytokine change after autologous bone marrow cell infusion (Mizunaga et al. 2012). We also report that TNFα signal is important to regulate the improvement of liver fibrosis after bone marrow cell infusion (Hisanaga et al. 2011). These cytokine changes after cultured human bone marrow cell infusion might be important to improve liver fibrosis.
In our ABMi therapy, we collected 400 mL of autologous bone marrow aspirate (BM-MNC fraction average, 7.8 × 109 cells) and, after the cells had been processed, we administered an average of 5.2 × 109 cells (Terai et al. 2006). In the BM-MNCs, there were 0.001–0.01 % MSC present (Pittenger et al. 1999). Therefore, the number of MSCs administered in ABMi therapy converts to a range of 0.5 to 5 × 105 cells. In this research, approximately 4 × 106 BM-MNCs were cultured through two passages; assuming 94 % of the approximately 3 × 106 recovered cells were MSCs, we obtained approximately 2.8 × 106 MSCs. For example, in 10 mL of bone marrow aspirate, which can be collected under local anesthesia, the number of BM-MNCs is approximately 2 × 108 cells, which converts mathematically to approximately 0.2 to 2 × 104 MSCs; but after these cells undergo two passages, the recovered number of cells is 1.5 × 108 and multiplying that by 94 % means that approximately 1.4 × 108 MSCs can be collected. Even when the loss accompanying the various processing steps is taken into account, the number of recovered MSCs is considered adequate. In other words, this research has demonstrated that ABMi therapy will be possible using cultured cells that can be collected under local anesthesia.
With regard to the carcinogenicity of human bone marrow cells, a group at Sun Yat-Sen University in China has shown that, when a bone marrow aspirate was administered via the hepatic artery to patients with HBV-induced liver failure, there was no change in the onset of hepatocarcinoma due to the bone marrow cell infusion for up to 192 weeks (Peng et al. 2011). A safety evaluation by oncogenicity tests involving nude mice will be necessary before clinical application but we have already shown that the administration of bone marrow cells does not promote the onset of liver cancer in mice with hepatocarcinogenic liver cirrhosis (N-nitrosodietylamine/GFP-CCl4 model) and, conversely, it significantly inhibits hepatocarcinogenesis (Maeda et al. 2012).
No reports on either the safety or danger of the administration of cultured human bone marrow-derived cells have been published concerning the intravenous infusion of autologous cultured BM-MSCs but a death resulting from contrast nephropathy did occur when CD34-positive hematopoietic stem cells were administered via the hepatic artery (Pai et al. 2008). The majority of cultured human bone marrow-derived cells (P2) that we have studied are MSC and they contain almost no CD34-positive cells (0.06 %). Moreover, we are considering infusion via a peripheral vein in the same manner as ABMi therapy, so, in that respect, the administration of P2 cells should be safe. In addition, it has been reported that no malignant transformation of bone marrow cells has occurred in the past, even with long-term culturing. In this case, the duration of the P2 cell culture is 20–22 days and, from a quality standpoint, we believe that malignant transformation is unlikely to occur (Bernardo et al. 2007).
Finally, in this study, we have revealed the liver fibrosis-improving effect of MSC originating in cultured human bone marrow-derived cells (P2). In the future, further analysis of the liver fibrosis-improving mechanism will be needed but we have now shown that cultured human bone marrow-derived cells (P2) can improve liver fibrosis by regulating the expression of MMP-9 and HSC activation that is mediated by the humoral factors TGFβ and TNFα. This analysis has also revealed that ABMi using cultured cells, which can be collected on an outpatient basis under local anesthesia, is a method with sufficient clinical applicability.
Abbreviations
- αSMA:
-
Alpha smooth muscle actin
- ABMi:
-
Autologous bone marrow cell infusion
- BM-MNC:
-
Bone marrow-derived mononuclear cell
- CCl4 :
-
Carbon tetrachloride
- DMEM:
-
Dulbecco’s modified eagle’s medium
- FBS:
-
Fetal bovine serum
- GFP:
-
Green fluorescent protein
- HSC:
-
Hepatic stellate cell
- IHC:
-
Immunohistochemistry
- MMP:
-
Matrix metalloproteinase
- mRNA:
-
Messenger RNA
- MSC:
-
Mesenchymal stem cell
- NOD-SCID:
-
Nonobese diabetic/severe combined immunodeficient
- PBS:
-
Phosphate-buffered saline
- RT-PCR:
-
Reverse transcription polymerase chain reaction
- TNFα:
-
Tumor necrosis factor alpha
- TGFβ:
-
Transforming growth factor beta
References
Alison MR, Poulsom R, Jeffery R, Dhillon AP, Quaglia A, Jacob J, Novelli M et al (2000) Hepatocytes from non-hepatic adult stem cells. Nature 406:257
Bernardo ME, Zaffaroni N, Novara F, Cometa AM, Avanzini MA, Moretta A, Montagna D et al (2007) Human bone marrow derived mesenchymal stem cells do not undergo transformation after long-term in vitro culture and do not exhibit telomere maintenance mechanisms. Cancer Res 67:9142–9149
Hisanaga T, Terai S, Iwamoto T, Takami T, Yamamoto N, Murata T, Matsuyama T et al (2011) TNFR1-mediated signaling is important to induce the improvement of liver fibrosis by bone marrow cell infusion. Cell Tissue Res 346:79–88
Huang CK, Lee SO, Lai KP, Ma WL, Lin TH, Tsai MY, Luo J et al (2013) Targeting androgen receptor in bone marrow mesenchymal stem cells leads to better transplantation therapy efficacy in liver cirrhosis. Hepatology 57:1550–1563
Iwamoto T, Terai S, Hisanaga T, Takami T, Yamamoto N, Watanabe S, Sakaida I (2013) Bone-marrow-derived cells cultured in serum-free medium reduce liver fibrosis and improve liver function in carbon-tetrachloride-treated cirrhotic mice. Cell Tissue Res 351:487–495
Kharaziha P, Hellstrom PM, Noorinayer B, Farzaneh F, Aghajani K, Jafari F, Telkabadi M et al (2009) Improvement of liver function in liver cirrhosis patients after autologous mesenchymal stem cell injection: a phase I–II clinical trial. Eur J Gastroenterol Hepatol 21:1199–1205
Kim JK, Park YN, Kim JS, Park MS, Paik YH, Seok JY, Chung YE et al (2010) Autologous bone marrow infusion activates the progenitor cell compartment in patients with advanced liver cirrhosis. Cell Transplant 19:1237–1246
Maeda M, Takami T, Terai S, Sakaida I (2012) Autologous bone marrow cell infusions suppress tumor initiation in hepatocarcinogenic mice with liver cirrhosis. J Gastroenterol Hepatol 27(Suppl 2):104–111
Mizunaga Y, Terai S, Yamamoto N, Uchida K, Yamasaki T, Nishina H, Fujita Y, et al. (2012) Granulocyte colony-stimulating factor and interleukin-1beta are important cytokine in repair of the cirrhotic liver after bone marrow cell infusion -comparison of humans and model mice. Cell Transplant (in press)
Mohamadnejad M, Alimoghaddam K, Mohyeddin-Bonab M, Bagheri M, Bashtar M, Ghanaati H, Baharvand H et al (2007) Phase 1 trial of autologous bone marrow mesenchymal stem cell transplantation in patients with decompensated liver cirrhosis. Arch Iran Med 10:459–466
Pai M, Zacharoulis D, Milicevic MN, Helmy S, Jiao LR, Levicar N, Tait P et al (2008) Autologous infusion of expanded mobilized adult bone marrow-derived CD34+ cells into patients with alcoholic liver cirrhosis. Am J Gastroenterol 103:1952–1958
Peng L, Xie DY, Lin BL, Liu J, Zhu HP, Xie C, Zheng YB, et al. (2011) Autologous bone marrow mesenchymal stem cell transplantation in liver failure patients caused by hepatitis B: short-term and long-term outcomes. Hepatology (in press)
Phinney DG, Kopen G, Isaacson RL, Prockop DJ (1999) Plastic adherent stromal cells from the bone marrow of commonly used strains of inbred mice: variations in yield, growth, and differentiation. J Cell Biochem 72:570–585
Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA et al (1999) Multilineage potential of adult human mesenchymal stem cells. Science 284:143–147
Saito T, Okumoto K, Haga H, Nishise Y, Ishii R, Sato C, Watanabe H et al (2011) Potential therapeutic application of intravenous autologous bone marrow infusion in patients with alcoholic liver cirrhosis. Stem Cells Dev 20:1503–1510
Sakaida I, Terai S, Yamamoto N, Aoyama K, Ishikawa T, Nishina H, Okita K (2004) Transplantation of bone marrow cells reduces CCl4-induced liver fibrosis in mice. Hepatology 40:1304–1311
Takami T, Terai S, Sakaida I (2012) Advanced therapies using autologous bone marrow cells for chronic liver disease. Discov Med 14:7–12
Terai S, Sakaida I, Yamamoto N, Omori K, Watanabe T, Ohata S, Katada T et al (2003) An in vivo model for monitoring trans-differentiation of bone marrow cells into functional hepatocytes. J Biochem (Tokyo) 134:551–558
Terai S, Ishikawa T, Omori K, Aoyama K, Marumoto Y, Urata Y, Yokoyama Y et al (2006) Improved liver function in patients with liver cirrhosis after autologous bone marrow cell infusion therapy. Stem Cells 24:2292–2298
Terai S, Tanimoto H, Maeda M, Zaitsu J, Hisanaga T, Iwamoto T, Fujisawa K et al (2012) Timeline for development of autologous bone marrow infusion (ABMi) therapy and perspective for future stem cell therapy. J Gastroenterol 47:491–497
Theise ND, Nimmakayalu M, Gardner R, Illei PB, Morgan G, Teperman L, Henegariu O et al (2000) Liver from bone marrow in humans. Hepatology 32:11–16
Thomas JA, Pope C, Wojtacha D, Robson AJ, Gordon-Walker TT, Hartland S, Ramachandran P et al (2011) Macrophage therapy for murine liver fibrosis recruits host effector cells improving fibrosis, regeneration, and function. Hepatology 53:2003–2015
Acknowledgment
This study was supported by Grants-in-Aid for scientific research from the Japan Society for the Promotion of Science (JSPS); Ministry of Health, Labour and Welfare, health and labour sciences research grants and Japan Science and Technology Agency (JST), the project of realization of regenerative medicine and highway. Ms. Mariko Yamada, Ms. Isako Fujimoto and Ms. Yoko Fukusumi helped us with several analyses.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tanimoto, H., Terai, S., Taro, T. et al. Improvement of liver fibrosis by infusion of cultured cells derived from human bone marrow. Cell Tissue Res 354, 717–728 (2013). https://doi.org/10.1007/s00441-013-1727-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-013-1727-2