Abstract
Bone marrow–derived mesenchymal stem cells (BM-MSCs) represent an interesting alternative to liver or hepatocyte transplantation to treat liver injuries. Many studies have reported that MSCs can treat several diseases, including liver damage, just by injection into the bloodstream, without evidence of differentiation. The improvements were attributed to the organotrophic factors, low immunogenicity, immunomodulatory, and anti-inflammatory effects of MSCs, rather than their differentiation. The aim of the present study was to answer the question of whether the presence of BM-MSCs in the hepatic microenvironment will lead to their differentiation to functional hepatocyte-like cells. The hepatic microenvironment was mimicked in vitro by culture for 21 d with liver extract. The resulted cells expressed marker genes of the hepatic lineage including AFP, CK18, and Hnf4a. Functionally, they were able to detoxify ammonia into urea, to store glycogen as observed by PAS staining, and to synthesize glucose from pyruvate/lactate mixture. Phenotypically, the expression of MSC surface markers CD90 and CD105 decreased by differentiation. This evidenced differentiation into hepatocyte-like cells was accompanied by a downregulation of the stem cell marker genes sox2 and Nanog and the cell cycle regulatory genes ANAPC2, CDC2, Cyclin A1, and ABL1. The present results suggest a clear differentiation of BM-MSCs into functional hepatocyte-like cells by the extracted liver microenvironment. This differentiation is confirmed by a decrease in the stemness and mitotic activities. Tracking transplanted BM-MSCs and proving their in vivo differentiation remains to be elucidated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Liver damage and chronic liver diseases represent a significant and severe health care problem that affects millions of patients all over the world. In end-stage liver disease, liver transplantation is mostly the first therapeutic option. However, it bears several major obstacles such as increasing shortage of suitable donor organs that markedly compromises liver transplantation, patients require lifelong immunosuppressive medication and hence medical supervision, and the procedure involves major surgery and is very costly (Hyder et al. 2018). An attractive approach to overcome the problems of whole organ transplantation is the transplantation of liver cells. Cell transplantation could help to alleviate donor organ shortage and, if proven effective, would be simpler, safer, and less expensive than a whole organ transplant. However, the lack of methodology to maintain hepatocytes in long-term in vitro culture retards the research development (Hyder et al. 2012). Other adult multipotent mesenchymal stem and reprogrammable cells still represent a promising alternative in regenerative medicine and in hepatic tissue engineering (Ungefroren et al. 2015; Ungefroren et al. 2016).
There are many studies that report the treatment of several diseases just by injection of mesenchymal stem cells (MSCs). MSCs were reported to repair liver fibrosis (Stutchfield et al. 2010; Ali et al. 2012; Yu et al. 2017), improve the outcome of islet grafts in diabetes (Kerby 2013), provide immunosuppressive effects in rheumatologic diseases (Sun et al. 2010; Keyszer 2011; Wang et al. 2011; Xu 2012; Liu et al. 2015a; Li et al. 2015), repair and improve cartilage quality in osteoarthritis and other osteochondral defects (Orozco et al. 2013; Harada 2015), prevent cell death in ischemic brain, recover motor and sensory function, and cause significant improvements in Parkinson, Alzheimer and other neurologic diseases (Okazaki 2008; Venkataramana et al. 2010; Honmou 2011; Liu et al. 2015b), and treat many cardiac dysfunctions (Ammar 2015; Kawamura 2015; de Morais et al. 2015; Roura 2015; Wang et al. 2015). However, all of these reports did not prove that MSCs have been differentiated into the target cells to replace the damaged tissue. Many mechanisms of action have been suggested for these MSCs, but none of them has suggested that MSCs have been differentiated in vivo, and little studies have even traced MSCs after their injection.
Little is known about the differentiation into hepatocyte-like cells after transplantation (Sato et al. 2005; Chamberlain et al. 2007). For stem cell transplantation to treat liver diseases, it is important to determine that MSCs will undergo differentiation after transplantation. Otherwise, the differentiation step into hepatocytes should be first undertaken in vitro before transplantation. Leaving the continuously dividing MSCs without differentiation in vivo has many risks including malignant transformation (Casiraghi et al. 2013). The interaction between stem cells and the environment surrounding them regulates differentiation or stem cell self-renewal so that a particular culture condition is required for differentiation potential towards hepatocytes; otherwise, stem cells will not be differentiated. To mimic the in vivo target tissue microenvironment, tissue homogenates have been used in several systems to induce in vitro stem cell differentiation into functional cells (Perán et al. 2010; Wang et al. 2012; Xue et al. 2016). Liver homogenate contains about 643 proteins that undertake many functions including providing high range of substances necessary for the growth of liver cells (Chu et al. 2004; Nhung et al. 2015). It is also likely to include all necessary stimulating factors and nutrients for hepatocytic differentiation (Fan et al. 2015; Kedarisetty et al. 2014), which are sufficient for liver regeneration after damage or partial removal (Michalopoulos 2014). Also, decellularized cell-deposited extracellular matrix was suggested to facilitate the hepatic maturation and promote stem cell–based liver generation (He et al. 2013). Liver homogenate was shown earlier to differentiate other kinds of stem cells as human umbilical cord stem cells (Xue et al. 2016) and placental amniotic membrane stem cells (Sarvandi et al. 2015) into hepatic linage. Here, we used different concentrations of liver homogenate to answer the question of whether the presence of bone marrow–derived MSCs in this hepatic environment will be sufficient for their differentiation into functional hepatocyte-like cells.
Material and Methods
Mesenchymal stem cell isolation and culture
Rat bone marrow was isolated by flushing femurs and tibias by DMEM as described by Zhang and Chan (Zhang and Chan 2010). All bone marrow cells were cultured for 4 d, and the plastic adhered cells were washed several times and cultured until reached confluence. BM-MSCs in passages 3, 4, and 5 were used in this study.
Liver extract preparation and treatment
Livers were excised from 7- to 12-d-old rats, washed many times with sterile PBS, cut into small segments in 10 ml sterile DMEM, and homogenized for 30 s at low speed on wet ice. The homogenate was centrifuged at 15000 rpm for 20 min at 4°C. The supernatant was sterile filtered (0.45 μm) then stored at − 20°C until needed.
BM-MSCs in passages 3, 4, and 5 at 70% confluence were cultured in DMEM-F12 supplied with 5% FCS and different concentrations of liver extract (0 (control), 6, 18, 30, and 60 μg/ml) for 21 d. The culture medium was changed every 3rd day. Cells of different cultures were then characterized by flow cytometry using anti-CD90, anti-CD105, and anti-CD34.
Periodic acid-Schiff staining
The differentiated hepatocyte-like cells should be capable of glycogen storage as hepatocytes do. Glycogen storage has been tested by periodic-acid Schiff (PAS) stain (Hui et al. 2017) at day 21. The medium was removed from the flasks; cells rinsed with PBS three times and fixed with 4% paraformaldehyde for 20 min at room temperature, washed 3 times with PBS for 2 to 3 min, oxidized for 15 min with 1% periodic acid, and washed 3× with deionized water. Cells were then stained with Schiff’s reagent for 30 min and washed 3 times with PBS prior to microscopic examination and imaging.
Hepatocyte metabolic function testing
Differentiated cells have been tested for their ability to detoxify ammonia into urea and to synthesize glucose from pyruvate/lactate. The experimental details were published in our previous reports (Hyder et al. 2018, 2012).
Real-time PCR
The expression of some genes characterizing hepatic cells, cell cycle genes, and stem cell marker genes has been tested. The expression of these genes has been analyzed by quantitative RT-PCR as described elsewhere (Hyder 2019). The forward and reverse primers for the selected genes are mentioned in Table 1.
Statistical analysis
Data are presented as mean ± SEM. All experiments were carried out only in MSC culture passages 3, 4, and 5 (N = 3 in all cases). Experiments were repeated 3 times within each tested passage, but the average value was considered N = 1. Analysis of variance (ANOVA) was applied for the statistical analysis followed by t test as a post hoc test. A p < 0.05 was considered significant in all cases.
Results
Expression of hepatocyte lineage-specific marker genes
We first sought to determine whether cells stemming from BM-MSCs and differentiated using liver homogenate display mature characteristics of the hepatic lineage; we examined by PCR the gene expression patterns of various early hepatic marker genes. RNA was collected after the differentiation process and subsequently analyzed using RT-qPCR for the lineage-specific markers, namely hepatocyte nuclear factor 4 (Hnf4a), alpha-fetoprotein (AFP), and cytokeratin 18 (CK18, also known as KRT18). As shown in Fig. 1, the 3 genes were upregulated (ANOVA p = 0.001, 0.009, and 0.0013 for Hnf4a, AFP, and CK18, respectively). However, this upregulation was significant only in cells differentiated in the higher concentrations (30 and 60 μg/ml) of liver extracts (Student’s t test p < 0.05), as compared with the corresponding mRNA expression of cells cultured with 0 μg/ml of liver extract.
Expression of the hepatic lineage marker genes α-fetoprotein (A), cytokeratin-18 (B), and hepatocyte nuclear factor 4 alpha (C) in BM-MSCs differentiated for 21 d by different concentrations of liver homogenate. Data are presented as mean ± SEM of N = 3 as described in the “Material and Methods” section. Statistical analyses: ANOVA p < 0.05 in all cases, asterisk denotes significantly higher value than that of the control (post hoc t test p < 0.05).
Hepatocellular functional aspects in cells differentiated using liver extract
Next, we examined the hepatic-related functions in cells derived from BM-MSCs and differentiated using liver homogenate. Ideally, the differentiation procedure should not only upregulate the hepatocyte-specific marker genes but also improve features of the newly differentiated cells in a way that they become functionally more hepatocyte-like. We therefore tested whether the used differentiation medium (liver extract) would alter functional parameters of the differentiated cells. Bone marrow–derived mesenchymal stem cells were allowed to differentiate for 3 wk in different concentrations of liver extract and at the end of this period were analyzed for hepatocyte-specific functions (Fig. 2).
Metabolic functions of hepatocyte-like cells differentiated from BM-MSCs by incubation with different concentrations of liver extract for 21 d. (A) Detoxification: differentiated cells are able to detoxify ammonia to urea. Cells were incubated with or without 5 mM NH4Cl for 24 h before the estimation of urea. (B) Gluconeogenesis: differentiated cells were incubated with a mixture of lactate and pyruvate for 24 h before the estimation of formed glucose. (C) Glycogen storage: MSCs incubated in either 0 (upper photo) or 60 mg/ml (lower photo) of liver extract for 21 d were subjected to PAS staining. Data are presented in (A) and (B) as mean ± SEM. Statistical analyses: asterisk denotes significantly higher value of the stimulated cells than that of the basal value (t test p < 0.05).
All cell groups, regardless of treatment, formed and secreted urea in a quantity ranged from 28 to 30 mg/dl under basic conditions. Incubation with NH4Cl increased urea formation significantly in all settings formerly differentiated using any concentration of liver extract (Fig. 2A). This reflects the ability of these differentiated cells to detoxify ammonia into urea, which is a proper hepatocellular function.
To measure the ability of these cells to perform gluconeogenesis, after the 3-wk differentiation period, they were incubated for 24 h with a buffer supplemented with Na-pyruvate and Na-l-lactate. Stimulation with pyruvate/lactate induced higher glucose secretion compared with non-stimulated cultures. As observed for urea, the effect on gluconeogenesis from lactate/pyruvate was significantly higher (p < 0.05, t test) in cells differentiated with any concentration of liver extract than in the corresponding control (Fig. 2B).
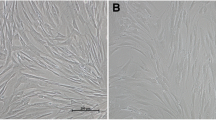
To observe the ability of liver extract-differentiated cells to store glycogen, after the 3-wk differentiation period, they were subjected to PAS staining. Figure 2C shows representative micrographs of stained cells after incubation for the 21 d without (upper panel) or with liver extract (60 mg/ml, lower panel). PAS-positive cells could be observed after differentiation using any of the applied liver extract concentrations. Regarding cell morphology, it should be mentioned that most differentiated cells kept their fibroblast-like spindle-shaped morphology, although they looked bigger or more round. However, the characteristic polygonal structure of hepatocytes could not be observed after differentiation with any liver extract concentration.
Stem cell markers in cells differentiated from BM-MSCs by liver extract
The differentiation of BM-MSC into hepatocyte-like cells using liver extract should be accompanied by inhibition of stemness markers. We have examined the gene expression of 2 pluripotency marker genes, namely sox2 and Nanog, and analyzed some phenotypic cell surface markers of MSCs.
Cell surface marker proteins of MSCs were examined by flow cytometry after differentiation for 21 d using different concentrations (0–60 μg/ml) of liver extract. Both undifferentiated and differentiated cells were positive for the cell surface markers CD90, and CD105 while being negative for CD34 (Fig. 3A). The CD90 expression decreased from 92.7 to 56.3%, while the expression of CD105 decreased from 96.1 to 61.9% after differentiation using 60 μg/ml of liver extract.
The differentiation process of BM-MSCs into hepatocyte-like cells by incubation with different concentrations of liver extract for 21 d is accompanied by a decrease of stem cell markers. (A) Cell surface marker proteins of MSCs were examined by flow cytometry. Cells were positive for CD90 and CD105 while being negative for CD34. Note the decrease in the expression of these markers after incubation with liver extract. (B) Incubation with liver extract decreases the expression of stem cell marker genes Nanog and sox2. Data are presented as mean ± SEM. Statistical analyses: asterisk denotes significantly lower value of differentiated cells than that of the control (t test p < 0.05).
We have also examined the effect of MSC differentiation by different concentrations of the liver extract on the expression of stemness genes Nanog and sox2 by qRT-PCR (Fig. 3B). The results revealed a significant transcriptional downregulation of both genes, even in response to the lowest applied liver extract concentration. These findings suggest that differentiation of BM-MSCs into hepatocyte-like cells is accompanied by the downregulation of stem cell characters.
The differentiation process is accompanied by transcriptional downregulation of genes involved in cell cycle regulation
Stem cells are characterized by continuous division, a feature that is inhibited by differentiation. Since the inhibition of mitotic activity involves transcriptional changes in key cell cycle regulators, we examined by qPCR analysis whether the differentiation of BM-MSCs by liver extract into hepatocyte-like cells was associated with the regulation of genes that have regulatory roles in different stages of the cell cycle. As seen in Table 2, the 21-d differentiation period using liver extract significantly downregulated the mRNA expression of the ANAPC2 and CDC2 significantly, and ABL-1 and cyclinA1 insignificantly. These transcriptional effects on cell cycle genes are likely mediated by a differentiation process.
Discussion
Direct injection/transfusion of MSCs has been reported to improve the function of different damaged tissues and systems (Okazaki 2008; Stutchfield et al. 2010; Sun et al. 2010; Venkataramana et al. 2010; Honmou 2011; Keyszer 2011; Wang et al. 2011; Ali et al. 2012; Xu 2012; Kerby 2013; Orozco et al. 2013; Ammar 2015; de Morais et al. 2015; Harada 2015; Li et al. 2015; Kawamura 2015; Liu et al. 2015a; Liu et al. 2015b; Roura 2015; Wang et al. 2015; Yu et al. 2017). Mechanisms of action are not clearly elucidated, but suggested to be due to the stem cell–derived organotrophic factors (Schuppan and Pinzani 2012; Liu et al. 2015c) and exosomes (Rong et al. 2019) that treat and protect cells from damage or activate endogenous mechanisms to restore the injured tissue, and to the low immunogenicity, immunomodulatory, and anti-inflammatory effects of MSCs (Meier et al. 2013; Jang et al. 2014; Zekri et al. 2015). The aim of the present study was to elucidate whether the presence of MSCs in the hepatic microenvironment will lead to their differentiation to functional hepatocyte-like cells. This is crucial because of the multifunctional nature of hepatocytes and to avoid the risk resulted from the presence of undifferentiated continuously dividing cells inside the liver tissue.
There are 3 conditions to consider the differentiation process of these BM-MSCs into hepatocyte-like cells successful. The first condition is that differentiated cells must have less expression of stemness markers. In the present study, a transcriptional downregulation was observed in both pluripotency genes sox2 and Nanog. The characteristic MSC surface marker proteins decreased. However, despite the apparent differentiation, the resulted cells still expressed the mesenchymal stem cell markers CD90 and CD105, suggesting, in agreement with previous studies (Campard et al. 2008; Bao et al. 2016), incomplete differentiation.
The second condition to consider the BM-MSC differentiation into hepatocyte-like cells successful is that differentiated cells must have inhibited cell division and cell cycle parallel to the differentiation process. The present data showed downregulation at the mRNA level of cell cycle regulatory genes ANAPC2, CDC2, cyclin A1, and ABL-1. ANAPC2 controls the regulation of the G1/S and G2/M transitions, CDC2 takes part in M-phase regulation, ABL-1 regulates the S-phase and DNA replication, and cyclin A defines control points of the cell cycle by binding CDK2 and CDC2 resulting in 2 distinct cyclin A kinase activities, one appearing in S phase and the other one in G2 phase. Inhibition of ANAPC2 and CDC2 has been reported to induce cell cycle arrest at G2/M (Pagano et al. 1992; Heilman et al. 2005; Enserink and Kolodner 2010; Hyder et al. 2012, 2018). As shown above, the results showed that differentiation was associated also with a decrease in pluripotency, which is known to be associated with self-renewal and proliferation (Hyder et al. 2018). The downregulation of sox2, for example, can exert exiting of the cell cycle (Bylund et al. 2003) which is in line with the inhibited cell cycle regulating gene activity in the present study.
The last condition is that the differentiated cells must express some of the hepatic lineage marker genes and perform hepatic metabolic functions. The present study revealed a clear differentiation of BM-MSCs to hepatocyte-like cells. These cells expressed the hepatic lineage-specific genes Hnf4a, AFP, and CK18. They performed also some hepatocellular-specific functions: detoxification of ammonia into urea, storage of glycogen, and gluconeogenesis from pyruvate/lactate mixture. Thus, the applied hepatic tissue extract, which was suggested to mimic the liver microenvironment, was sufficient to differentiate BM-MSCs into hepatocyte-like cells.
Neonatal livers have been used for homogenization in the present study. Fetal and neonatal tissues are supposed to have higher levels of growth and differentiation factors than the adult tissue (Hyder et al. 2010). In fact, liver homogenate, if proven efficient, will represent a very cost-effective medium for the in vitro differentiation of bone marrow stem cells towards hepatic lineage. Therefore, some previous studies have applied it in different concentrations to promote the differentiation of other kinds of stem cells (Sarvandi et al. 2015; Xue et al. 2016). In one study (Sarvandi et al. 2015), 6 μg/ml concentration of liver extract was found the effective dose for induction of omentum tissue mesenchymal stem cell differentiation. In the other studies, higher concentrations of 50 mg/ml with decidua-derived stem cells (Bornstein et al. 2012) or 150 mg/ml (Xue et al. 2016) with umbilical cord stem cells have been applied. We applied concentrations ranging from 6 to 60 μg/ml and observed that the lowest concentration was sufficient to inhibit the stem cell and cell cycle gene expressions. However, hepatic cell functions and the expression levels of hepatic lineage genes were concentration dependent within the applied low range of concentrations. These results are in agreement with the previous reports of other stem cell types differentiated by liver homogenates.
Although they acquired some hepatocellular functions and became morphologically more round, the differentiated hepatocyte-like cells kept their original bipolar fibroblast-like structure. Also, as mentioned above, only a fraction of cells has lost the typical cell surface markers CD90 and CD105. Moreover, the downregulation of the cell cycle regulatory genes cyclin A1 and ABL1 was weak and not significant. All of these findings suggest that the differentiation of BM-MSCs into hepatocyte-like cells was partial. The differentiation of only a small fraction into hepatocytes is similar to the results of other in vitro studies using variable differentiation media as previously reported (Aurich et al. 2009; Lin et al. 2011; Piryaei et al. 2011), so that the entire functionality of the differentiated cell, regardless of the differentiation methodology, was only 8–23% of the native hepatocytes (Hengstler et al. 2005). This differentiation fraction may vary in vivo, but this remains to be determined. Nevertheless, this limited fraction still raises the question about the efficacy and safety of direct MSC transplantation.
Conclusion
Bone marrow–derived mesenchymal stem cells can be differentiated in vitro into functional hepatocyte-like cells just by culturing in a hepatic microenvironment represented by liver homogenate. This differentiation was accompanied by a logic downregulation of cell division and stem cell markers. Labelling MSCs and persuading their landing and behavior in the liver after transplantation to prove this differentiation in vivo is still required.
References
Ali G, Mohsin S, Khan M, Nasir GA, Shams S, Khan SN, Riazuddin S (2012) Nitric oxide augments mesenchymal stem cell ability to repair liver fibrosis. J Transl Med 10(1):75
Ammar HI (2015) Comparison of adipose tissue- and bone marrow- derived mesenchymal stem cells for alleviating doxorubicin-induced cardiac dysfunction in diabetic rats. Stem Cell Res Ther 6:1–16
Aurich H, Sgodda M, Kaltwasser P, Vetter M, Weise A, Liehr T, Brulport M, Hengstler JG, Dollinger MM, Fleig WE, Christ B (2009) Hepatocyte differentiation of mesenchymal stem cells from human adipose tissue in vitro promotes hepatic integration in vivo. Gut 58(4):570–581
Bao J, Wu Q, Wang Y, Li Y, Li L, Chen F, Wu X, Xie M, Bu H (2016) Enhanced hepatic differentiation of rat bone marrow-derived mesenchymal stem cells in spheroidal aggregate culture on a decellularized liver scaffold. Int J Mol Med 38(2):457–465
Bornstein R, Macias MI, de la Torre P, Grande J, Flores AI (2012) Human decidua-derived mesenchymal stromal cells differentiate into hepatic-like cells and form functional three-dimensional structures. Cytotherapy 14(10):1182–1192
Bylund M, Andersson E, Novitch BG, Muhr J (2003) Vertebrate neurogenesis is counteracted by Sox 1–3 activity. Nat Neurosci 6(11):1162–1168
Campard D, Lysy PA, Najimi M, Sokal EM (2008) Native umbilical cord matrix stem cells express hepatic markers and differentiate into hepatocyte-like cells. Gastroenterology 134(3):833–848
Casiraghi F, Remuzzi G, Abbate M, Perico N (2013) Multipotent mesenchymal stromal cell therapy and risk of malignancies. Stem Cell Rev 9(1):65–79
Chamberlain J, Yamagami T, Colletti E, Theise ND, Desai J, Frias A, Pixley J, Zanjani ED, Porada CD, Almeida-Porada G (2007) Efficient generation of human hepatocytes by the intrahepatic delivery of clonal human mesenchymal stem cells in fetal sheep. Hepatology 46(6):1935–1945
Chu R, Lim H, Brumfield L, Liu H, Herring C, Ulintz P, Davison M (2004) Protein profiling of mouse livers with peroxisome proliferator-activated receptor α activation. Mol Cell Boil 24(14):6288–6297
de Morais SB, da Silva LE, Lataro RM, Silva CA, de Oliveira LF, de Carvalho EE, Simões MV, da Silva ML, Fazan R Jr, Salgado HC (2015) Mesenchymal stem cells improve heart rate variability and baroreflex sensitivity in rats with chronic heart failure. Stem Cells Dev 24:2181–2192
Enserink JM, Kolodner RD (2010) An overview of Cdk1-controlled targets and processes. Cell Div 5(1):11
Fan M, Wang X, Xu G, Yan Q, Huang W (2015) Bile acid signaling and liver regeneration. Biochim Biophys Acta 1849(2):196–200
Harada Y (2015) Combination therapy with intra-articular injection of mesenchymal stem cells and articulated joint distraction for repair of a chronic osteochondral defect in the rabbit. J Orthop Res 33:1466–1473
He H, Liu X, Peng L, Gao Z, Ye Y, Su Y, Zhao Q, Wang K, Gong Y, He F (2013) Promotion of hepatic differentiation of bone marrow mesenchymal stem cells on decellularized cell-deposited extracellular matrix. Biomed Res Int 2013:406871
Heilman DW, Green MR, Teodoro JG (2005) The anaphase promoting complex: a critical target for viral proteins and anticancer drugs. Cell Cycle 4(4):560–563
Hengstler JG, Brulport M, Schormann W, Bauer A, Hermes M, Nussler AK, Fandrich F, Ruhnke M, Ungefroren H, Griffin L, Bockamp E, Oesch F, von Mach MA (2005) Generation of human hepatocytes by stem cell technology: definition of the hepatocyte. Expert Opin Drug Metab Toxicol 1(1):61–74
Honmou O (2011) Intravenous administration of auto serum-expanded autologous mesenchymal stem cells in stroke. Brain 134:1790–1807
Hui H, Ma W, Cui J, Gong M, Wang Y, Zhang Y, He T, Bi Y, He Y (2017) Periodic acid-Schiff staining method for function detection of liver cells is affected by 2% horse serum in induction medium. Mol Med Rep 16(6):8062–8068
Hyder A, Ehnert S, Fändrich F, Ungefroren H (2018) Transfection of peripheral blood monocytes with SOX2 enhances multipotency, proliferation, and redifferentiation into neohepatocytes and insulin-producing cells. Stem Cells Int 2018.4271875
Hyder A (2019) PGlyRP3 concerts with PPARγ to attenuate DSS-induced colitis in mice. Int Immunopharmacol 67:46–53
Hyder A, Ehnert S, Reiling N, Nüssler AK, Fändrich F, Ungefroren H (2012) EGF enhances the proliferation of human programmable cells of monocytic origin (PCMO) through activation of MEK/ERK signaling and improves the differentiation/function of PCMO-derived neohepatocyte-like cells. Cell Commun Signal 10:23–32
Hyder A, Laue C, Schrezenmeir J (2010) Metabolic aspects of neonatal rat islet hypoxia tolerance. Transpl Int 23(1):80–89
Jang YO, Kim MY, Cho MY, Baik SK, Cho YZ, Kwon SO (2014) Effect of bone marrow-derived mesenchymal stem cells on hepatic fibrosis in a thioacetamide-induced cirrhotic rat model. BMC Gastroenterol (1):14–198
Kawamura M (2015) Xenotransplantation of bone marrow-derived human mesenchymal stem cell sheets attenuates left ventricular remodeling in a porcine ischemic cardiomyopathy model. Tissue Eng A 21:2272–2280
Kedarisetty CK, Anand L, Khanam A, Kumar A, Rastogi A, Maiwall R, Sarin SK (2014) Growth factors enhance liver regeneration in acute-on-chronic liver failure. Hepatol Int 8(Suppl 2):514–525
Kerby A (2013) Co-transplantation of islets with mesenchymal stem cells in microcapsules demonstrates graft outcome can be improved in an isolated-graft model of islet transplantation in mice. Cytotherapy 15:192–200
Keyszer G (2011) Treatment of severe progressive systemic sclerosis with transplantation of mesenchymal stromal cells from allogeneic related donors: report of five cases. Arthritis Rheum 63:2540–2550
Li D, Wang P, Li Y, Xie Z, Wang L, Su H, Deng W, Wu Y, Shen H (2015) All-trans retinoic acid improves the effects of bone marrow-derived mesenchymal stem cells on the treatment of ankylosing spondylitis: an in vitro study. Stem Cells Int 2015:484528
Lin H, Xu R, Zhang Z, Chen L, Shi M, Wang FS (2011) Implications of the immunoregulatory functions of mesenchymal stem cells in the treatment of human liver diseases. Cell Mol Immunol 8(1):19–22
Liu R, Li X, Zhang Z, Zhou M, Sun Y, Su D, Feng X, Gao X, Shi S, Chen W, Sun L (2015a) Allogeneic mesenchymal stem cells inhibited T follicular helper cell generation in rheumatoid arthritis. Sci Rep 5:12777
Liu Z, Wang C, Wang X, Xu S (2015b) Therapeutic effects of transplantation of As-MiR-937-expressing mesenchymal stem cells in murine model of Alzheimer’s disease. Cell Physiol Biochem 37:321–330
Liu WH, Song FQ, Ren LN, Guo WQ, Wang T, Feng YX, Tang LJ, Li K (2015c) The multiple functional roles of mesenchymal stem cells in participating in treating liver diseases. J Cell Mol Med 19(3):511–520
Meier RP, Müller YD, Morel P, Gonelle-Gispert C, Bühler LH (2013) Transplantation of mesenchymal stem cells for the treatment of liver diseases, is there enough evidence? Stem Cell Res 11(3):1348–1364
Michalopoulos GK (2014) Advances in liver regeneration. Expert Rev Gastroenterol Hepatol 8:897–907
Nhung TH, Nam NH, Nguyen NTK, Nghia H, Van Thanh N, Ngoc PK, Van Pham P (2015) A comparison of the chemical and liver extract-induced hepatic differentiation of adipose derived stem cells. Vitro Cellular & Developmental Biology-Animal 51(10):1085–1092
Okazaki T (2008) Intravenous administration of bone marrow stromal cells increases survivin and Bcl-2 protein expression and improves sensorimotor function following ischemia in rats. Neurosci Lett 430:109–114
Orozco L, Munar A, Soler R, Alberca M, Soler F, Huguet M, Sentís J, Sánchez A, García-Sancho J (2013) Treatment of knee osteoarthritis with autologous mesenchymal stem cells: a pilot study. Transplantation 95:1535–1541
Pagano M, Pepperkok R, Verde F, Ansorge W, Draetta G (1992) Cyclin A is required at two points in the human cell cycle. EMBO J 11:961–971
Perán M, Marchal JA, López E, Jiménez-Navarro M, Boulaiz H, Rodríguez-Serrano F, Carrillo E, Sánchez-Espin G, de Teresa E, Tosh D, Aranega A (2010) Human cardiac tissue induces transdifferentiation of adult stem cells towards cardiomyocytes. Cytotherapy 12(3):332–337
Piryaei A, Valojerdi MR, Shahsavani M, Baharvand H (2011) Differentiation of bone marrow-derived mesenchymal stem cells into hepatocyte-like cells on nanofibers and their transplantation into a carbon tetrachloride-induced liver fibrosis model. Stem Cell Rev 7(1):103–118
Rong X, Liu J, Yao X, Jiang T, Wang Y, Xie F (2019) Human bone marrow mesenchymal stem cells-derived exosomes alleviate liver fibrosis through the Wnt/β-catenin pathway. Stem Cell Res Ther 10(1):98
Roura S (2015) Postinfarction functional recovery driven by a three-dimensional engineered fibrin patch composed of human umbilical cord blood-derived mesenchymal stem cells. Stem Cells Transl Med 4:956–966
Sarvandi SS, Joghataei MT, Parivar K, Khosravi M, Sarveazad A, Sanadgol N (2015) In vitro differentiation of rat mesenchymal stem cells to hepatocyte lineage. Iran J Basic Med Sci 18(1):89–97
Sato Y, Araki H, Kato J, Nakamura K, Kawano Y, Kobune M, Sato T, Miyanishi K, Takayama T, Takahashi M, Takimoto R, Iyama S, Matsunaga T, Ohtani S, Matsuura A, Hamada H, Niitsu Y (2005) Human mesenchymal stem cells xenografted directly to rat liver are differentiated into human hepatocytes without fusion. Blood 106(2):756–763
Schuppan D, Pinzani M (2012) Anti-fibrotic therapy: lost in translation? J. Hepatol. 56(Suppl. 1):S66–S74
Stutchfield BM, Forbes SJ, Wigmore SJ (2010) Prospects for stem cell transplantation in the treatment of hepatic disease. Liver Transpl 16(7):827–836
Sun L, Wang D, Liang J, Zhang H, Feng X, Wang H, Hua B, Liu B, Ye S, Hu X, Xu W, Zeng X, Hou Y, Gilkeson GS, Silver RM, Lu L, Shi S (2010) Umbilical cord mesenchymal stem cell transplantation in severe and refractory systemic lupus erythematosus. Arthritis Rheum 62:2467–2475
Ungefroren H, Hyder A, Hinz H, Groth S, Lange H, El-Sayed K, Ehnert S, Nüssler A, Fändrich F, Gieseler F (2015) Pluripotency gene expression and growth control in cultures of peripheral blood monocytes during their conversion into programmable cells of monocytic origin (PCMO): evidence for a regulatory role of autocrine activin and TGF-ß. PLoS One 10(2):e0118097
Ungefroren H, Hyder A, Schulze M, Fawzy El-Sayed KM, Grage-Griebenow E, Nussler AK, Fändrich F (2016) Peripheral blood monocytes as adult stem cells: molecular characterization and improvements in culture conditions to enhance stem cell features and proliferative potential. Stem Cells Int 2016:7132751
Venkataramana NK, Kumar SK, Balaraju S, Radhakrishnan RC, Bansal A, Dixit A, Rao DK, Das M, Jan M, Gupta PK, Totey SM (2010) Open-labeled study of unilateral autologous bone-marrow-derived mesenchymal stem cell transplantation in Parkinson’s disease. Transl Res 155:62–70
Wang D, Zhang H, Cao M, Tang Y, Liang J, Feng X, Wang H, Hua B, Liu B, Sun L (2011) Efficacy of allogeneic mesenchymal stem cell transplantation in patients with drug-resistant polymyositis and dermatomyositis. Ann Rheum Dis 70:1285–1288
Wang SS, Hu SW, Zhang QH, Xia AX, Jiang ZX (2015) Mesenchymal stem cells stabilize atherosclerotic vulnerable plaque by anti-inflammatory properties. PLoS One 10:e0136026
Wang X, Wu H, Xue G, Hou Y (2012) Progesterone promotes neuronal differentiation of human umbilical cord mesenchymal stem cells in culture conditions that mimic the brain microenvironment. Neural Regen Res 7(25):1925–1930
Xu J (2012) Allogeneic mesenchymal stem cell treatment alleviates experimental and clinical Sjogren syndrome. Blood 120:3142–3151
Xue G, Han X, Ma X, Wu H, Qin Y, Liu J, Hu Y, Hong Y, Hou Y (2016) Effect of microenvironment on differentiation of human umbilical cord mesenchymal stem cells into hepatocytes in vitro and in vivo. Biomed Res Int 2016:8916534
Yu J, Hao G, Wang D, Liu J, Dong X, Sun Y, Pan Q, Li Y, Shi X, Li L, Cao H (2017) Therapeutic effect and location of GFP-labeled placental mesenchymal stem cells on hepatic fibrosis in rats. Stem Cells Int 2017:1798260
Zekri AR, Salama H, Medhat E, Musa S, Abdel-Haleem H, Ahmed OS, Khedr HA, Lotfy MM, Zachariah KS, Bahnassy A (2015) The impact of repeated autologous infusion of haematopoietic stem cells in patients with liver insufficiency. Stem Cell Res Ther 6(1):118
Zhang L, Chan C (2010) Isolation and enrichment of rat mesenchymal stem cells (MSCs) and separation of single-colony derived MSCs. J Vis Exp 37:1852
Acknowledgments
The work contains part of the MSc thesis of the first author. The authors are grateful to the Faculty of Science, Damietta University, for the support and laboratory facilities, and the Mansoura Experimental Research Center (MERC), Mansoura University for the excellent assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Editor: Tetsuji Okamoto
Rights and permissions
About this article
Cite this article
Eissa, M., Elarabany, N. & Hyder, A. In vitro efficacy of liver microenvironment in bone marrow mesenchymal stem cell differentiation. In Vitro Cell.Dev.Biol.-Animal 56, 341–348 (2020). https://doi.org/10.1007/s11626-020-00436-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11626-020-00436-7