Abstract
Transplantation of human umbilical cord blood (hucb) cells in a model of hypoxic-ischemic brain injury led to the amelioration of lesion-impaired neurological and motor functions. However, the mechanisms by which transplanted cells mediate functional recovery after brain injury are largely unknown. In this study, the effects of hucb cell transplantation were investigated in this experimental paradigm at the cellular and molecular level. As the pathological cascade in hypoxic-ischemic brain injury includes inflammation, reduced blood flow, and neuronal cell death, we analyzed the effects of peripherally administered hucb cells on these detrimental processes, investigating the expression of characteristic marker proteins. Application of hucb cells after perinatal hypoxic-ischemic brain injury correlated with an increased expression of the proteins Tie-2 and occludin, which are associated with angiogenesis. Lesion-induced apoptosis, determined by expression of cleaved caspase-3, decreased, whereas the number of vital neurons, identified by counting of NeuN-positive cells, increased. In addition, we observed an increase in the expression of neurotrophic and pro-angiogenic growth factors, namely BDNF and VEGF, in the lesioned brain upon hucb cell transplantation. The release of neurotrophic factors mediated by transplanted hucb cells might cause a lower number of neurons to undergo apoptosis and result in a higher number of living neurons. In parallel, the increase of VEGF might cause growth of blood vessels. Thus, hucb transplantation might contribute to functional recovery after brain injury mediated by systemic or local effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypoxic-ischemic brain injury is an important cause of perinatal mortality und morbidity. The infants outliving this insult often suffer from permanent neurological deficits such as spastic paresis, cerebral palsy, epilepsy, and disorders of sensorimotor coordination (Volpe 2008, 2009). One of the major causes of perinatal brain damage is severe fetal or neonatal asphyxia (Berger and Garnier 2000; Jensen and Berger 1991).
As efficient clinical or pharmaceutical strategies to prevent or to reduce the incidence of perinatal hypoxic-ischemic brain damage are limited, regenerative therapies might provide an alternative. Over the past few years, transplantation of stem cells became a very promising approach for the putative treatment of neurological diseases in human (Kim and de Vellis 2009; Park et al. 2009b).
The therapeutic potential of human umbilical cord blood (hucb) cells in diseases of the nervous system has been shown in many experimental animal models (Rosenkranz and Meier 2011) including this for perinatal hypoxic-ischemic brain injury. Transplantation of hucb cells resulted in amelioration of lesion-impaired neurological and motor functions (Geissler et al. 2011; Meier et al. 2006; Pimentel-Coelho et al. 2010; Yasuhara et al. 2010). In our model, the observed beneficial effects correlate with the directed migration of hucb cells to the lesioned brain area and with the detection of these cells in this region up to 7 weeks after application (Geissler et al. 2011; Meier et al. 2006; Rosenkranz et al. 2010).
However, the mechanisms underlying the improvements mediated by umbilical cells are largely unknown. Although hucb cells are capable to differentiate into neural cells in culture (Buzanska et al. 2002; Ha et al. 2001; Neuhoff et al. 2007; Sanchez-Ramos et al. 2001), cell replacement seems to be a rare event in vivo (Garbuzova-Davis et al. 2003; Zigova et al. 2002). Therefore research now focuses on secondary mechanisms following hucb cell transplantation. One potential mode of action might be the release of neurotrophic factors by transplanted umbilical cells, resulting in indirect effects on the damaged host tissue. As we and others have demonstrated before, hucb cells are capable of secreting interleukins, growth factors, and chemotactic proteins in vitro (Neuhoff et al. 2007; Newman et al. 2006). Most of these secreted factors are renowned for their neuroprotective, angiogenic, or anti-inflammatory actions (Bai et al. 1997; Li et al. 2005; Nikkhah et al. 1993).
Given that cell death via apoptotic mechanisms is one of the most detrimental processes caused by hypoxic-ischemic injury (Hagberg et al. 2009; Hossain 2008), we analyzed the influence of transplanted hucb cells on cleaved caspase-3 expression and on the number of NeuN-expressing cells in a model of hypoxic-ischemic brain injury in newborn rats. In addition, we investigated proteins associated with angiogenesis as another potential downstream parameter.
Our results indicate that transplantation of hucb cells in a model of hypoxic-ischemic brain injury correlates with decreased cleaved caspase-3 expression, increased expression of occludin and Tie-2, and an augmented number NeuN-expressing cells. Together with the detected increase in VEGF and BDNF mRNA expression in vivo after hucb cell transplantation, our data correlate hucb cell transplantation with the observed beneficial effects on the lesioned tissue.
Materials and methods
Preparation of hucb-derived mononuclear cells for transplantation
Blood from umbilical cord and placenta was obtained from the Department of Gynecology and Obstetrics (St. Elisabeth-Hospital, Bochum, Germany), after receiving the mother’s written informed consent. The umbilical vein was punctured post partum, and the blood was collected in umbilical cord blood collection bags containing citrate phosphate dextrose as anticoagulant (Maco Pharma, Langen, Germany) and stored at 18 °C until further processing. Preparation of the mononuclear cell fraction was performed by Ficoll Paque (GE Healthcare, Munich, Germany) density gradient centrifugation according to the manufacturer’s instructions. The mononuclear fraction of cells was collected from the interphase, and resuspended in phosphate-buffered saline (PBS). Viability of mononuclear cells was 97 ± 2% as determined by toluidine blue staining.
The local Ethic Committee of the Ruhr-University Bochum approved use of cord blood samples.
Animals and hypoxic-ischemic injury surgical procedure
All surgical and experimental protocols were approved by the appropriate institutional review committee (LANUV Recklinghausen, Germany) and met the guidelines of the German animal protection law.
The Levine model (Levine 1960; Rice et al. 1981) was used to achieve reproducible hypoxic-ischemic injury in neonatal Wistar rats on postnatal day (P) 7 and was performed as described previously (Meier et al. 2006). Briefly, 7-day-old Wistar rat pups were deeply anesthetized by inhalation of isoflurane. The left common carotid artery was exposed, double ligated, and severed. To induce systemic hypoxia, the pups were exposed to a hypoxic gas mixture (8 % oxygen/92 % nitrogen) for 80 min. The environmental temperature was strictly maintained at 36 °C. Sham animals were anesthetized and the left common carotid artery was exposed, but not ligated. Sham animals did not undergo systemic hypoxia.
Transplantation of hucb-derived mononuclear cells (1 × 107/500 μl 0.9 % NaCl), or vehicle (NaCl) was performed by intraperitoneal injection 24 h after the insult as established in previous studies (Geissler et al. 2011; Meier et al. 2006; Rosenkranz et al. 2010) without any further use of anesthesia or immunosuppressant.
At P9 and P21, i.e. 2 and 14 days after the insult, rats were anesthetized and decapitated. Brains were dissected and macroscopic brain injury was assessed immediately (Bona et al. 1997). For immunoblot analysis and isolation of RNA, brains were trimmed (−3 mm frontal, −2 mm occipital), and left and right hemispheres were separated and frozen in liquid nitrogen until further processing. All further animal testing and quantifications were performed in a blinded fashion.
Animal groups used in this study were as follows: sham; sham+hucb (=sham with transplantation of hucb cells); lesion (=hypoxic-ischemic lesion with transplantation of vehicle); lesion+hucb (=hypoxic-ischemic lesion with transplantation of hucb cells).
Immunoblots
Immunoblot analysis was performed as described previously (Neuhoff et al. 2007). Proteins (10 μg/lane) were separated on 10 % SDS-polyacrylamid gels. After electrophoretic transfer of proteins, nitrocellulose membranes were incubated with primary antibodies at 4 °C overnight. After washing, the immunoblots were incubated with horseradish–peroxidase-conjugated secondary antibodies (1:8000; Jackson ImmunoResearch, Newmarket, UK) for 1 h. Visualization was performed by enhanced chemiluminescence detection (GE Healthcare).
Quantification was carried out by densitometric analysis of signal intensities (Jackson ImmunoResearch) using actin expression for normalization. All sham-values were set to 100 %, thus allowing comparison of samples within one time point only. Immunoblot analyses were performed in three independent experiments and are expressed as mean ± standard error of the mean. Primary antibodies were as follows: cleaved caspase-3 (1:100; Cell Signaling Technology, Danvers, USA), Tie-2 (1:100; Santa Cruz Biotechnology, Heidelberg, Germany), NeuN (1:100; Millipore, Schwalbach, Germany), β-actin (1:8000; Sigma-Aldrich, Taufkirchen, Germany).
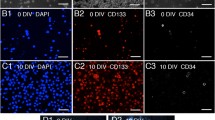
Immunohistochemistry and histological analysis
Brains were covered in tissue freezing medium (Leica, Nussloch, Germany) and cryopreserved. Histology and immunohistochemistry were performed on cryosections of 12-μm thickness. Precise localization of the lesion areas was assured by histological staining according to Kluever–Barrera, showing myelinated fiber tracts in light green and cell bodies in blue. Immunohistochemistry was performed as described previously (Meier et al. 2006). Fluorescence was documented using conventional fluorescence microscopy (Zeiss 200 M inverted microscope including the Apotome device). Data were exported as TIFF files into Adobe Photoshop CS2 (Adobe Imaging Systems, USA). For all immunohistochemical analysis controls omitting the primary antibody were performed. Primary antibodies were: cleaved caspase-3 (1:100; Cell Signaling Technology), NeuN (1:100; Millipore), occludin (1:100; Zymed Laboratories, San Francisco, USA). Secondary antibodies were: Alexa Fluor™ 488 or 546 conjugated goat-anti-rabbit or goat-anti-mouse (1:3,000; Invitrogen, Karlsruhe, Germany).
Quantification of immunohistochemical signals
Randomly selected animals were assigned to three different experimental groups and investigated at P21: sham (n = 3), lesion with transplantation of vehicle (lesion; n = 3), and lesion followed by intraperitoneal transplantation of 1 × 107 mononuclear cells (lesion+hucb; n = 3). Quantification was performed on cryosections at a level corresponding to Bregma –2.9 ± 0.5 mm in the adult brain by determining expression in eight/ten brain regions per hemisphere (Rosenkranz et al. 2010). Photographs of these regions were taken and used for quantification of the immunosignal (imageJ) and the number of immunopositive cells (cell counts).
In the imageJ program (NIH, http://rsb.info.nih.gov/ij/), the threshold mode was applied to photographs, i.e. any fluorescent signal, irrespective of its intensity, was assigned black color, and any area devoid of immunostaining was attributed white. The area covered by the fluorescent signal (black) was expressed as percent of the background (white).
For quantification of cell numbers, counting of immunopositive cells was carried out in the photographs of eight (for NeuN) or ten (for cleaved caspase-3) brain regions per hemisphere.
In both methods, the mean of all regions investigated per hemisphere was compared for statistical analysis. The graphs represent the mean of three individual analyzed animals per group.
Quantitative real time polymerase chain reaction
For detection of the growth factors BDNF and VEGF in the rat brain after transplantation of hucb cells, real time PCR was carried out. RNA was extracted from brain tissue (sham (n = 3); sham+hucb (n = 3); lesion (n = 3); lesion+hucb (n = 3)), and reversed transcribed three times independently. Primers for real time PCR were as follows: BDNF-upstream primer (USP): 5’-actctggagagcgtgaatgg-3’ (Asai et al. 2007), BDNF-downstream primer (DSP): 5’-tccaaaggcacttgactgct-3’, VEGF-USP: 5’-acgaaagcgcaagaaatccc-3’, VEGF-DSP: 5’-tgcaacgcgagtctgtgttt-3’, 18S-USP: 5’-agaacgaaagtcggaggttcg-3’, 18S-DSP: 5’-tgagtcaaattaagccgcagg-3’. The rat specific VEGF primer sequences were according to Wakabayashi et al. (2010).
Cycling was performed using Sybr Green (Eurogentec, Seraign, Belgium) on the GeneAmp 5700 Sequence Detection System (Applied Biosystems, Darmstadt, Germany) or on the DNA Engine Opticon 2 Realtime System (Biorad Laboratories, Munich, Germany). All experiments were performed three times independently in sets of left hemispheres analyzed in triplicate. The average Cycle threshold (Ct) values of three independent experiments were used to calculate the ratios using the equation procedure introduced by Pfaffl (2001). Primer efficiencies were calculated using the LinRegPCR program (Ramakers et al. 2003). Calculation of ratios, standard error, and statistical analysis were performed using the Relative Expression software Tool (REST) (Pfaffl et al. 2002), with ratio of sham values set 1.
Statistical analysis
Initial analysis of variance (ANOVA) was followed by Tukey HSD post hoc test using the SPSS 18 statistic program. A probability of error less than 0.05 (p < 0.05) was considered statistically significant. All data are expressed as mean ± standard error of the mean.
For statistical analysis of the ratios of real time PCR results, we used the Relative Expression software Tool (REST) (Pfaffl et al. 2002).
Results
Hucb cell transplantation promotes neuronal survival after hypoxic-ischemic brain injury
Expression of cleaved caspase-3, a protein activated during apoptosis, was used to determine the extent of cell death. We performed immunohistochemistry on cryosections using anti-cleaved caspase-3 antibodies 14 days after induction of the lesion at postnatal day (P) 21. Quantification of cleaved caspase-3 immunoreactivity in ten corresponding regions of the lesioned/left and the intact/right hemisphere (Fig. 1a–d), revealed a significantly higher immunoreactivity in left hemispheres of lesioned animals compared to left hemispheres of sham animals (p < 0.05; Fig. 1e). After transplantation of hucb cells, this increase of cleaved caspase-3 immunoreactivity in the lesioned hemisphere was no longer significant compared to sham animals (Fig. 1e). Also, the significant difference within the lesion group was no longer present upon hucb treatment (Fig. 1e).
HUCB cell transplantation after hypoxic-ischemic brain injury leads to a reduction of cleaved caspase-3. a Schematic representation of a P21 rat brain with hypoxic-ischemic lesion showing the ten regions in the ipsilateral (black circles) and contralateral (white circles) hemispheres chosen for quantification. For evaluation of cleaved caspase-3 expression (red), immunohistochemistry was performed in three experimental groups: b sham, c lesion, d lesion+hucb. e Quantification of the immunosignal of cleaved caspase-3 at P21 in ten regions per section using the ImageJ program. f Quantification of the mean number of cleaved caspase-3 positive cells counted in ten regions per section. g Quantification of cleaved caspase-3 protein expression after immunoblot analysis at P9 and P21. Analyses were performed in left hemispheres of sham, lesion and lesion+hucb animals. Significant differences (p < 0.05) are indicated by ***. Hoechst staining (blue) labeled all nuclei (b–d). Scale bar 50 μm
At P21, right hemispheres of all groups showed minimal cleaved caspase-3 immunoreactivity, and quantification of expression did not show any significant differences between experimental groups (Fig. 1e).
In addition to quantification of immunosignals using imageJ, we counted cleaved caspase-3 immunopositive cells in these ten brain regions of the three animal groups (sham, lesion, lesion+hucb). Cell numbers increased significantly in the lesion group compared to the sham group (Fig. 1f). After transplantation of hucb cells, these differences were no longer significant (Fig. 1f). The comparison of left and right hemispheres within the individual groups showed significant differences between the lesion group and the group of lesion+hucb (Fig. 1f).
Supplementarily, we investigated expression of cleaved caspase-3 after immunoblot analysis in left hemispheres of the three groups (sham, lesion, lesion+hucb) (Fig. 1g). Two different time points were investigated, i.e. 2 days (at P9) and 14 days (at P21) after induction of the lesion. At both time points, left hemispheres of lesion animals expressed higher amounts of cleaved caspase-3 compared to sham animals (sham = 100 %). Expression of cleaved caspase-3 protein in the lesion+hucb group decreased in comparison to the lesion group. At P21, protein levels of cleaved caspase-3 in animals of lesion+hucb reached nearly baseline values as observed in sham animals (Fig. 1g).
Because neuronal cells are most affected by apoptosis in the model of perinatal brain injury, we decided to assess neuronal cell numbers in vivo using the neuronal nuclei protein (NeuN) as a marker.
Immunohistochemical analysis was carried out to evaluate the number of NeuN-immunopositive cells in left and right brain hemispheres of the three animal groups (sham, lesion, lesion+hucb). The number of immunopositive cells was quantified in eight defined regions of each hemisphere (Fig. 2a). At P21, the reduced number of NeuN-immunopositive cells observed in left hemispheres of lesion and lesion+hucb groups was not significantly different from sham animals (Fig. 2b, c, e). However, quantification of NeuN-immunopositive cells in left and right hemispheres within the experimental groups revealed significant differences in the group of lesion and lesion+hucb (p < 0.05; Fig. 2e).
Positive effects on neuronal survival after transplantation of hucb cells. a Schematic representation of a P21 rat brain with hypoxic-ischemic lesion showing the eight regions in the ipsilateral (black circles) and contralateral (white circles) hemisphere chosen for counting of NeuN-positive cells. NeuN immunohistochemistry (green) was performed on brain sections at P21 of animals of the following groups: b sham, c lesion and d lesion+hucb (lesion plus additional application of hucb cells). e Quantification of the mean number of NeuN-immunopositive cells in the ipsilateral and contralateral hemispheres of the three experimental groups. f At P9 and P21, immunoblot analysis of NeuN expression was performed in left hemispheres of animals of the sham, lesion, and lesion+hucb group. Significant differences (p < 0.05) are indicated by ***. Hoechst staining (blue) labeled all nuclei (b–d). Scale bar 50 μm
Immunoblot analysis revealed a significant decrease of NeuN protein expression 2 days after hypoxic-ischemic brain injury (P9). Upon transplantation of hucb cells, this decrease was no longer present and NeuN expression differed significantly from that observed in the lesion group (p < 0.05; Fig. 2f). At P21, there were no significant differences in NeuN expression between any of the experimental groups (Fig. 2f).
Changes in expression of occludin and Tie-2 after hucb cell transplantation
Blood vessels of the immature brain are another major target of perinatal hypoxic-ischemic brain injury. Their perturbation causes perivascular edema and disruption of the blood-brain-barrier. Thus, we investigated effects of hucb cell transplantation on the expression of endothelial proteins associated with angiogenesis, like the angiopoietin receptor tyrosine kinase with immunoglobulin-like and EGF-like domains (Tie)-2, and with blood–brain barrier integrity, like the tight junction protein occludin.
Expression of occludin was analyzed immunohistochemically. For quantification of occludin immunoreactivity at P21, we determined the area covered by the immunostaining in ten regions of the ipsilateral and contralateral hemisphere (Fig. 3a). In Fig. 3b, a characteristic immunohistochemical staining of occludin is shown at high magnification. Representative lower magnification images used for quantification of occludin are provided in Electronic Supplementary Material, Fig. S1. Statistical evaluation exhibited a significant increase of occludin immunosignal in left hemispheres of the lesion group compared to right hemispheres of the lesion group (p < 0.05; Fig. 3c). After hucb cell transplantation, significant differences between hemispheres were no longer present.
Transplantation of hucb cells affects expression of the proteins Tie-2 and occludin in vivo. a Schematic view of a rat brain with hypoxic-ischemic brain injury at P21 with circles labeling the regions chosen for quantification of occludin immunoreactivity. b Representative image of occludin immunolabeling (green); nuclei are labeled in blue (Hoechst staining). c Quantification of occludin immunoreactivity (mean of all regions investigated) in ipsilateral and contralateral hemispheres at P21 in the following experimental groups: sham, lesion, lesion+hucb. d Quantitative analysis of Tie-2 protein expression at two different time points, P9 and P21. Immunoblot analysis was performed in left hemispheres of sham, lesioned, and lesioned animals with hucb cell transplantation (lesion+hucb). Significant differences of p < 0.05 are indicated by ***. Scale bar 50 μm
In order to determine the expression of Tie-2, immunoblot analysis was carried out and protein levels of Tie-2 were quantified in left hemispheres of the three animal groups. Tie-2 showed a reduced expression in the lesion group as compared to animals of the sham group, which was significant at P9 but not at P21 (Fig. 3d). After transplantation of hucb cells, significant differences were no longer detectable (Fig. 3d).
Local effects in the brain: Increased expression of BDNF and VEGF one day after hucb cell transplantation
Observed effects in the brain, i.e. reduced cleaved caspase-3 expression, increased protein levels of Tie-2 and occludin, and an increase in the number of NeuN-positive cells, correlating with intraperitoneal application of hucb cells might be mediated by local effects, for instance by the secretion of paracrine factors.
In order to investigate whether the observed beneficial effects after transplantation of hucb cells might be due to the secretion of growth factors in vivo, we exemplarily analyzed the expression of two potentially relevant growth factors 2 and 14 days after the insult, i.e. at P9 and P21. Brain-derived neurotrophic factor (BDNF; Fig. 4a) was shown to participate in inhibition of apoptosis and inflammation (Almeida et al. 2005; Makar et al. 2008), whereas vascular endothelial growth factor (VEGF; Fig. 4b) even has, besides its renowned vasodilatative and pro-angiogenic effects, a neuroprotective function (Jin et al. 2002). For the determination of changes in expression of these two growth factors, quantitative real time PCR was performed in left hemispheres of three experimental groups (sham, lesion, lesion+hucb) using non-species-specific primer pairs. As shown in Fig. 4a, c, expression of both BDNF and VEGF significantly decreased 2 days after hypoxic-ischemic brain damage. Transplantation of hucb cells, in turn, yielded in an up-regulation of BDNF and VEGF mRNA expression as compared to the lesion group, which was significant for VEGF (Fig. 4a, c). Fourteen days after the insult, mRNA expression of both growth factors was similar between all experimental groups (P21; Fig. 4a, c). In addition, expression in sham animals was compared to that in sham animals that received hucb transplantation (sham+hucb). A significant increase in the expression of both growth factors was observed in sham+hucb animals at P9 (Fig. 4b, d). Furthermore, we performed real time PCR with rat specific VEGF primers (Wakabayashi et al. 2010) using the same experimental groups. At P9, lesion-associated reduction of rat VEGF mRNA was less pronounced in the lesion+hucb group (Electronic Supplementary Material, Fig. S2).
Relative expression of BDNF and VEGF after hypoxic-ischemic lesion (lesion) and lesion followed by hucb cell transplantation (lesion+hucb). Quantitative real time PCR analysis of BDNF (a, b) and VEGF (c, d) mRNA expression at P9 and P21 in left hemispheres of rat brains of the following experimental groups: sham, lesion, lesion+hucb (a, c) and sham+hucb (b, d). Significant differences of p < 0.05 are indicated by ***
Discussion
Insufficient supply of oxygen (hypoxia) or poor blood flow (ischemia) in the neonatal brain leads to activation of primary and secondary cell death cascades, i.e. necrosis and apoptosis, to disturbed blood vessel integrity as well as to a local and/or systemic immune reaction. The prevention of severe impairments resulting from hypoxia-ischemia is a major goal of current therapeutic developments, cell therapy being one of them. We have previously demonstrated in a rat model of perinatal hypoxic-ischemic brain damage that transplantation of umbilical cord blood cells was associated with an amelioration of lesion-impaired sensorimotor behavior (Meier et al. 2006). In view of the cascade of pathophysiological events, any therapy must have the aim of preventing the detrimental processes associated with the second phase after the insult (Rosenkranz and Meier 2011). Here, we investigate whether the beneficial effects of hucb cell transplantation are indeed associated with (1) the decline in harmful processes of the secondary phase after the insult, including apoptosis, and (2) the increase of beneficial processes, like angiogenesis and neuronal survival. Together, the positive effects of hucb cell transplantation might be due to the establishment of a regenerative environment in the brain.
The secondary and final cell loss in the brain is mediated mainly by apoptosis (Hagberg et al. 2009; Nakajima et al. 2000). Hypoxic-ischemic injury in the immature brain leads to induction of apoptosis associated with extensive activation of caspase-3 (Wang et al. 2001), whereas hucb cell transplantation was associated with reduced levels of cleaved-caspase-3 protein, pointing to reduced apoptosis. Pimentel-Coelho et al. (2010) also observed the constraint of apoptosis upon hucb cell transplantation after hypoxic-ischemic brain damage; however, in their study, the effects were demonstrated for the striatum only. A reduction of neuronal cell death as observed in our model of perinatal hypoxic-ischemic injury has also been reported in an adult model of stroke, where a significant decrease in apoptosis was observed 28 days after transplantation of bone marrow stromal cells (Chen et al. 2003a).
As neurons are most sensitive to anoxia, and as caspase-3 is involved in the apoptotic pathway of neurons, neuronal cell numbers were evaluated in our experimental paradigm using NeuN. Upon transplantation of hucb cells, NeuN protein expression, reflecting the number of NeuN-positive cells, was significantly higher than in animals of the lesion group. As this increase was observed rapidly, i.e. within 1 day after transplantation, neurogenesis seems an unlikely reason. This is further supported by the fact that NeuN is a marker for mature neurons and therefore improbable to be expressed within 1 day after generation of neurons. Thus, the increase in the number of NeuN-expressing cells is likely related to improved survival. However, hypoxia has also been described to result in the down-regulation of NeuN protein not associated with cell death (Unal-Cevik et al. 2004).
The integrity of brain blood vessels is another important event disturbed by hypoxic-ischemic brain injury. After the insult, inadequate circulation leads to tissue death. Angiogenesis, i.e. the growth of new capillary blood vessels, is the attempt to restore blood flow. The Angiopoetin-1/Tie-2 system is crucial for angiogenesis during development and upon impairment of adult brain by ischemia or during tumor vascularisation (Fukuhara et al. 2008).
Indeed, in our study, Tie-2 protein expression decreased 2 and 14 days after the insult, pointing to a lesion-induced diminishment of existent and regenerated blood vessels. In turn, Tie-2 protein levels were higher after hucb cell transplantation. New blood vessel formation will improve blood supply to the injured region, thereby efficiently providing nutrients and oxygen to the degenerating and regenerating neurons in the lesioned brain.
Breakdown of the blood–brain barrier (bbb) is another consequence of ischemia and was traced back to a loss of the tight junction proteins occludin and zonula occludens-1 (ZO-1) (Bolton et al. 1998; Liu et al. 2009). In our study, occludin expression also decreased after the insult, which is, with occludin being an integral component of the bbb (Balda et al. 1996), indicative of a disturbed bbb composition. Again, hucb cell transplantation was associated with an increase in occludin expression, possibly pointing to the molecular reconstruction of the bbb.
To investigate potential factors mediating generalized effects on angiogenesis and neuronal survival, expression of BDNF and VEGF were exemplarily analyzed. Both growth factors are secreted by hucb cells in vitro (Neuhoff et al. 2007) and both are expressed within the brain. The neurotrophic factor BDNF participates in proliferation and differentiation of cells, as well as in inhibition of apoptosis and inflammation (Almeida et al. 2005; Makar et al. 2008). Application of BDNF protected the neonatal rat brain from hypoxic-ischemic injury (Han and Holtzman 2000). VEGF was shown to be a major contributor to angiogenesis (Marti 2002; Park et al. 2009a). Furthermore it was demonstrated that VEGF treatment in vivo and in vitro could provide protection against several forms of neuronal injury independently of its angiogenic action (Jin et al. 2002; Plate et al. 1999).
The significant decline of BDNF and VEGF mRNA levels after hypoxic-ischemic brain injury was no longer present in the lesion group that received transplantation of hucb cells. A raised expression of VEGF and the associated enhanced angiogenesis was also observed after transplantation of bone marrow-derived cells in a model of stroke (Chen et al. 2003b).
Expression of BDNF and VEGF could account for many of the beneficial effects observed after hucb cell transplantation. In terms of apoptosis and neuronal survival, it was demonstrated that application of BDNF blocks activation of caspase-3 in a model of neonatal hypoxia-ischemia, likely to account for the protective action of BDNF against neuronal injury (Han et al. 2000). Moreover, VEGF was shown to provide neuroprotective effects via down-regulation of caspase-3 in a mouse model of intracerebral hemorrhage (Lee et al. 2007). Furthermore, the neuroprotective effect of VEGF is accomplished by an active regulation of the expression of pro-and anti-apoptotic factors (Jin et al. 2002; Sun et al. 2003).
Increased expression of BDNF and VEGF mRNA in lesioned brains after hucb cell transplantation might even have an influence on angiogenesis. There has been a study reporting that overexpression of BDNF in mouse hearts resulted in increased capillary density and reduced endothelial cell apoptosis (Donovan et al. 2000), whereas after up-regulation of VEGF, enhanced neovascularization and angiogenesis were observed in ischemic brain (Zhang et al. 2000).
Thus, with the observed restoration of BDNF and VEGF expression levels, hucb cells might also exert generalized effects on neuronal survival and angiogenesis. The increase of BDNF and VEGF in the lesion+hucb group was 5.3-fold and 4.0-fold, respectively, when compared to the lesion group. Interestingly, transplantation of hucb cells to sham animals (sham+hucb) also resulted in a corresponding increase of BDNF (3.5-fold) and a slightly lower increase of VEGF expression (1.7-fold) when compared to non-transplanted sham groups.
Because the primer pairs used for real time PCR analysis in general recognized both human and rat mRNA, it is not clear whether expression of these two factors occurs in hucb cells themselves or whether hucb cells induce endogenous rat cells to express and secrete BDNF and VEGF. Therefore, an increase in mRNA expression following hucb transplantation as detected by non-species-specific primers, might reflect the number of human cells in the brain. As PCR analysis using rat-specific primers did not reveal significant changes in expression, the source of these growth factors could not be determined unequivocally in our study. However, an increase of rat VEGF and BDNF mRNA levels has been described upon transplantation of human mesenchymal stem cells in a middle cerebral artery occlusion model (Wakabayashi et al. 2010), supporting the hypothesis that human cell transplantation might induce expression of endogenous growth factors in the lesioned rat brain.
The present study provides an insight into the mechanisms by which hucb cells may exert their beneficial effects on the lesioned brain. The investigation of a therapeutic action of hucb cells comprised local effects in the damaged brain including expression of Tie-2, occludin, cleaved caspase-3, and NeuN. The determination of increased BDNF and VEGF levels in vivo supports the hypothesis of an indirect action of these cells.
Taken together, the results indicate that neurological and motor improvements observed after hucb cell transplantation are likely due to the release of trophic factors. These effects may contribute to a regenerative environment, allowing neuroplasticity and functional regeneration (Geissler et al. 2011) to occur.
References
Almeida RD, Manadas BJ, Melo CV, Gomes JR, Mendes CS, Graos MM, Carvalho RF, Carvalho AP, Duarte CB (2005) Neuroprotection by BDNF against glutamate-induced apoptotic cell death is mediated by ERK and PI3-kinase pathways. Cell Death Differ 12:1329–1343
Asai N, Abe T, Saito T, Sato H, Ishiguro S, Nishida K (2007) Temporal and spatial differences in expression of TrkB isoforms in rat retina during constant light exposure. Exp Eye Res 85:346–355
Bai XF, Zhu J, Zhang GX, Kaponides G, Hojeberg B, van der Meide PH, Link H (1997) IL-10 suppresses experimental autoimmune neuritis and down-regulates TH1-type immune responses. Clin Immunol Immunopathol 83:117–126
Balda MS, Whitney JA, Flores C, Gonzalez S, Cereijido M, Matter K (1996) Functional dissociation of paracellular permeability and transepithelial electrical resistance and disruption of the apical-basolateral intramembrane diffusion barrier by expression of a mutant tight junction membrane protein. J Cell Biol 134:1031–1049
Berger R, Garnier Y (2000) Perinatal brain injury. J Perinat Med 28:261–285
Bolton SJ, Anthony DC, Perry VH (1998) Loss of the tight junction proteins occludin and zonula occludens-1 from cerebral vascular endothelium during neutrophil-induced blood-brain barrier breakdown in vivo. Neuroscience 86:1245–1257
Bona E, Aden U, Gilland E, Fredholm BB, Hagberg H (1997) Neonatal cerebral hypoxia-ischemia: the effect of adenosine receptor antagonists. Neuropharmacology 36:1327–1338
Buzanska L, Machaj EK, Zablocka B, Pojda Z, Domanska-Janik K (2002) Human cord blood-derived cells attain neuronal and glial features in vitro. J Cell Sci 115:2131–2138
Chen J, Li Y, Katakowski M, Chen X, Wang L, Lu D, Lu M, Gautam SC, Chopp M (2003a) Intravenous bone marrow stromal cell therapy reduces apoptosis and promotes endogenous cell proliferation after stroke in female rat. J Neurosci Res 73:778–786
Chen J, Zhang ZG, Li Y, Wang L, Xu YX, Gautam SC, Lu M, Zhu Z, Chopp M (2003b) Intravenous administration of human bone marrow stromal cells induces angiogenesis in the ischemic boundary zone after stroke in rats. Circ Res 92:692–699
Donovan MJ, Lin MI, Wiegn P, Ringstedt T, Kraemer R, Hahn R, Wang S, Ibanez CF, Rafii S, Hempstead BL (2000) Brain derived neurotrophic factor is an endothelial cell survival factor required for intramyocardial vessel stabilization. Development 127:4531–4540
Fukuhara S, Sako K, Minami T, Noda K, Kim HZ, Kodama T, Shibuya M, Takakura N, Koh GY, Mochizuki N (2008) Differential function of Tie2 at cell-cell contacts and cell-substratum contacts regulated by angiopoietin-1. Nat Cell Biol 10:513–526
Garbuzova-Davis S, Willing AE, Zigova T, Saporta S, Justen EB, Lane JC, Hudson JE, Chen N, Davis CD, Sanberg PR (2003) Intravenous administration of human umbilical cord blood cells in a mouse model of amyotrophic lateral sclerosis: distribution, migration, and differentiation. J Hematother Stem Cell Res 12:255–270
Geissler M, Dinse HR, Kumbruch S, Kreikemeier K, Meier C (2011) Human umbilical cord blood cells restore brain damage induced changes in rat somatosensory cortex. PLoS One 6:e20194
Ha Y, Choi JU, Yoon DH, Yeon DS, Lee JJ, Kim HO, Cho YE (2001) Neural phenotype expression of cultured human cord blood cells in vitro. NeuroReport 12:3523–3527
Hagberg H, Mallard C, Rousset CI, Xiaoyang W (2009) Apoptotic mechanisms in the immature brain: involvement of mitochondria. J Child Neurol 24:1141–1146
Han BH, Holtzman DM (2000) BDNF protects the neonatal brain from hypoxic-ischemic injury in vivo via the ERK pathway. J Neurosci 20:5775–5781
Han BH, D'Costa A, Back SA, Parsadanian M, Patel S, Shah AR, Gidday JM, Srinivasan A, Deshmukh M, Holtzman DM (2000) BDNF blocks caspase-3 activation in neonatal hypoxia-ischemia. Neurobiol Dis 7:38–53
Hossain MA (2008) Hypoxic-ischemic injury in neonatal brain: involvement of a novel neuronal molecule in neuronal cell death and potential target for neuroprotection. Int J Dev Neurosci 26:93–101
Jensen A, Berger R (1991) Fetal circulatory responses to oxygen lack. J Dev Physiol 16:181–207
Jin K, Zhu Y, Sun Y, Mao XO, Xie L, Greenberg DA (2002) Vascular endothelial growth factor (VEGF) stimulates neurogenesis in vitro and in vivo. Proc Natl Acad Sci USA 99:11946–11950
Kim SU, de Vellis J (2009) Stem cell-based cell therapy in neurological diseases: a review. J Neurosci Res 87:2183–2200
Lee HJ, Kim KS, Park IH, Kim SU (2007) Human neural stem cells over-expressing VEGF provide neuroprotection, angiogenesis and functional recovery in mouse stroke model. PLoS One 2:e156
Levine S (1960) Anoxic-ischemic encephalopathy in rats. Am J Pathol 36:1–17
Li A, Varney ML, Valasek J, Godfrey M, Dave BJ, Singh RK (2005) Autocrine role of interleukin-8 in induction of endothelial cell proliferation, survival, migration and MMP-2 production and angiogenesis. Angiogenesis 8:63–71
Liu W, Hendren J, Qin XJ, Shen J, Liu KJ (2009) Normobaric hyperoxia attenuates early blood-brain barrier disruption by inhibiting MMP-9-mediated occludin degradation in focal cerebral ischemia. J Neurochem 108:811–820
Makar TK, Trisler D, Sura KT, Sultana S, Patel N, Bever CT (2008) Brain derived neurotrophic factor treatment reduces inflammation and apoptosis in experimental allergic encephalomyelitis. J Neurol Sci 270:70–76
Marti HH (2002) Vascular endothelial growth factor. Adv Exp Med Biol 513:375–394
Meier C, Middelanis J, Wasielewski B, Neuhoff S, Roth-Haerer A, Gantert M, Dinse HR, Dermietzel R, Jensen A (2006) Spastic paresis after perinatal brain damage in rats is reduced by human cord blood mononuclear cells. Pediatr Res 59:244–249
Nakajima W, Ishida A, Lange MS, Gabrielson KL, Wilson MA, Martin LJ, Blue ME, Johnston MV (2000) Apoptosis has a prolonged role in the neurodegeneration after hypoxic ischemia in the newborn rat. J Neurosci 20:7994–8004
Neuhoff S, Moers J, Rieks M, Grunwald T, Jensen A, Dermietzel R, Meier C (2007) Proliferation, differentiation, and cytokine secretion of human umbilical cord blood-derived mononuclear cells in vitro. Exp Hematol 35:1119–1131
Newman MB, Willing AE, Manresa JJ, Sanberg CD, Sanberg PR (2006) Cytokines produced by cultured human umbilical cord blood (HUCB) cells: implications for brain repair. Exp Neurol 199:201–208
Nikkhah G, Odin P, Smits A, Tingstrom A, Othberg A, Brundin P, Funa K, Lindvall O (1993) Platelet-derived growth factor promotes survival of rat and human mesencephalic dopaminergic neurons in culture. Exp Brain Res 92:516–523
Park CW, Kim HW, Lim JH, Yoo KD, Chung S, Shin SJ, Chung HW, Lee SJ, Chae CB, Kim YS, Chang YS (2009a) Vascular endothelial growth factor inhibition by dRK6 causes endothelial apoptosis, fibrosis, and inflammation in the heart via the Akt/eNOS axis in db/db mice. Diabetes 58:2666–2676
Park DH, Eve DJ, Musso J 3rd, Klasko SK, Cruz E, Borlongan CV, Sanberg PR (2009b) Inflammation and stem cell migration to the injured brain in higher organisms. Stem Cells Dev 18:693–702
Pfaffl MW (2001) A new mathematical model for relative quantification in real-time RT-PCR. Nucleic Acids Res 29:e45
Pfaffl MW, Horgan GW, Dempfle L (2002) Relative expression software tool (REST) for group-wise comparison and statistical analysis of relative expression results in real-time PCR. Nucleic Acids Res 30:e36
Pimentel-Coelho PM, Magalhaes ES, Lopes LM, Deazevedo LC, Santiago MF, Mendez-Otero R (2010) Human cord blood transplantation in a neonatal rat model of hypoxic-ischemic brain damage: functional outcome related to neuroprotection in the striatum. Stem Cells Dev 19:351–358
Plate KH, Beck H, Danner S, Allegrini PR, Wiessner C (1999) Cell type specific upregulation of vascular endothelial growth factor in an MCA-occlusion model of cerebral infarct. J Neuropathol Exp Neurol 58:654–666
Ramakers C, Ruijter JM, Deprez RH, Moorman AF (2003) Assumption-free analysis of quantitative real-time polymerase chain reaction (PCR) data. Neurosci Lett 339:62–66
Rice JE 3rd, Vannucci RC, Brierley JB (1981) The influence of immaturity on hypoxic-ischemic brain damage in the rat. Ann Neurol 9:131–141
Rosenkranz K, Meier C (2011) Umbilical cord blood cell transplantation after brain ischemia-From recovery of function to cellular mechanisms. Ann Anat 193:371–379
Rosenkranz K, Kumbruch S, Lebermann K, Marschner K, Jensen A, Dermietzel R, Meier C (2010) The chemokine SDF-1 / CXCL12 contributes to the 'homing' of umbilical cord blood cells to a hypoxic-ischemic lesion in the rat brain. J Neurosci Res 88:1223–1233
Sanchez-Ramos JR, Song S, Kamath SG, Zigova T, Willing A, Cardozo-Pelaez F, Stedeford T, Chopp M, Sanberg PR (2001) Expression of neural markers in human umbilical cord blood. Exp Neurol 171:109–115
Sun Y, Jin K, Xie L, Childs J, Mao XO, Logvinova A, Greenberg DA (2003) VEGF-induced neuroprotection, neurogenesis, and angiogenesis after focal cerebral ischemia. J Clin Invest 111:1843–1851
Unal-Cevik I, Kilinc M, Gursoy-Ozdemir Y, Gurer G, Dalkara T (2004) Loss of NeuN immunoreactivity after cerebral ischemia does not indicate neuronal cell loss: a cautionary note. Brain Res 1015:169–174
Volpe JJ (2008) Neurology of the newborn. Elsevier, Philadelphia
Volpe JJ (2009) Brain injury in premature infants: a complex amalgam of destructive and developmental disturbances. Lancet Neurol 8:110–124
Wakabayashi K, Nagai A, Sheikh AM, Shiota Y, Narantuya D, Watanabe T, Masuda J, Kobayashi S, Kim SU, Yamaguchi S (2010) Transplantation of human mesenchymal stem cells promotes functional improvement and increased expression of neurotrophic factors in a rat focal cerebral ischemia model. J Neurosci Res 88:1017–1025
Wang X, Karlsson JO, Zhu C, Bahr BA, Hagberg H, Blomgren K (2001) Caspase-3 activation after neonatal rat cerebral hypoxia-ischemia. Biol Neonate 79:172–179
Yasuhara T, Hara K, Maki M, Xu L, Yu G, Ali MM, Masuda T, Yu SJ, Bae EK, Hayashi T, Matsukawa N, Kaneko Y, Kuzmin-Nichols N, Ellovitch S, Cruz EL, Klasko SK, Sanberg CD, Sanberg PR, Borlongan CV (2010) Mannitol facilitates neurotrophic factor upregulation and behavioral recovery in neonatal hypoxic-ischemic rats with human umbilical cord blood grafts. J Cell Mol Med 14:914–921
Zhang ZG, Zhang L, Jiang Q, Zhang R, Davies K, Powers C, Bruggen N, Chopp M (2000) VEGF enhances angiogenesis and promotes blood-brain barrier leakage in the ischemic brain. J Clin Invest 106:829–838
Zigova T, Song S, Willing AE, Hudson JE, Newman MB, Saporta S, Sanchez-Ramos J, Sanberg PR (2002) Human umbilical cord blood cells express neural antigens after transplantation into the developing rat brain. Cell Transplant 11:265–274
Acknowledgements
The authors would like to thank Janet Moers, Lidia Janota, Heike Groth and Jennifer Heinz for their excellent technical assistance and Helga Schulze for expert drawing.
Author information
Authors and Affiliations
Corresponding author
Additional information
Funding: This study was supported by a grant of the Stem Cell Network North Rhine Westphalia, Germany (to C.M.), and by the Medical Faculty of Ruhr-University Bochum, Germany (FoRUM)
Electronic supplementary material
Below is the link to the electronic supplementary material.
Fig. S1
Expression of occludin in rat brains assessed by immunohistochemistry. Representative images of immunhistochemical staining of occludin (green), on P21 rat brains of animals of the following groups a sham, b lesion and c lesion+hucb (lesion plus additional application of hucb cells). Nuclei are labeled in blue (Hoechst staining a–c). Scale bar in (a) for (a–c) 50 μm (PDF 2484 kb)
Fig. S2
Quantitative real time PCR analysis of rat VEGF mRNA expression. For determination of species origin of VEGF, quantitative real time PCR was performed with primers specific for rat VEGF. Analysis was performed at P9 and P21 in left hemispheres of rat brains of the following experimental groups: sham, sham+hucb, lesion and lesion+hucb. Significant differences of p < 0.05 are indicated by *** (PDF 5 kb)
Rights and permissions
About this article
Cite this article
Rosenkranz, K., Kumbruch, S., Tenbusch, M. et al. Transplantation of human umbilical cord blood cells mediated beneficial effects on apoptosis, angiogenesis and neuronal survival after hypoxic-ischemic brain injury in rats. Cell Tissue Res 348, 429–438 (2012). https://doi.org/10.1007/s00441-012-1401-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-012-1401-0