Abstract
Transforming growth factor beta (TGF-β) has been recognized as an important mediator in the genesis of chronic kidney diseases (CKD), which are characterized by the accumulation of extracellular matrix (ECM) components in the glomeruli (glomerular fibrosis, glomerulosclerosis) and the tubular interstitium (tubulointerstitial fibrosis). Glomerulosclerosis is a major cause of glomerular filtration rate reduction in CKD and all three major glomerular cell types (podocytes or visceral epithelial cells, mesangial cells and endothelial cells) participate in the fibrotic process. TGF-β induces (1) podocytopenia caused by podocyte apoptosis and detachment from the glomerular basement membrane; (2) mesangial expansion caused by mesangial cell hypertrophy, proliferation (and eventually apoptosis) and ECM synthesis; (3) endothelial to mesenchymal transition giving rise to glomerular myofibroblasts, a major source of ECM. TGF-β has been shown to mediate several key tubular pathological events during CKD progression, namely fibroblast proliferation, epithelial to mesenchymal transition, tubular and fibroblast ECM production and epithelial cell death leading to tubular cell deletion and interstitial fibrosis. In this review, we re-examine the mechanisms involved in glomerulosclerosis and tubulointerstitial fibrosis and the way that TGF-β participates in renal fibrosis, renal parenchyma degeneration and loss of function associated with CKD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction to chronic kidney diseases
Definition, causes, consequences and epidemiology
Chronic kidney disease (CKD) is a condition in which the renal excretory function progressively and irreversibly decreases as a consequence of renal tissue injury, dysfunction (namely, reduced filtration rate) and nephron loss. Decreased excretory function gives way to the accumulation of metabolic and waste products in the blood and organs, which cause azotemia and multiorgan damage. Eventually, patients can die from secondary conditions, the most important being cardiovascular events, or need renal replacement therapy (RRT) in the form of renal transplant or dialysis to avoid sure death (Remuzzi et al. 2006). Because of its high incidence and prevalence and the disproportionate cost of RRT, CKD represents a heavy human, clinical and socioeconomic burden. It is estimated that 10%-20% of the adult population have some degree of CKD and that dialysis (applied to 0.1% of the population) consumes about 2% of total health expenditure in many developed countries (De Vecchi et al. 1999). CKD can be caused by a variety of factors, including diabetes, hypertension, infections, atherosclerosis, renal artery and ureteral obstruction and genetic alterations. Renal function usually declines over a period of years or decades, although some patients become eligible for RRT after only a few months (López-Novoa et al. 2010, 2011).
A critical concept in CKD is that, early in the course of the disease, renal tissue injury crosses a point of no return beyond which a malignant scenario of self-destruction ensues independently of the initial insult. Regardless of etiology, a typical pathological phenotype appears in which the number of nephrons decreases progressively and fibrosis and interstitial scarring replace the space left by the destroyed nephrons. Transforming growth factor beta (TGF-β) has been recognized as an important mediator of a variety of glomerular, tubular and inflammatory processes involved in the appearance of this phenotype (Schnaper et al. 2009). Specifically, this review deals with its effects at inducing glomerular and tubulointerstitial fibrosis, which are the structural changes supporting the appearance of CKD.
General etiopathology
CKD can be initiated by damage in the glomeruli, in the tubuli, or in the renal vessels. Whether started as glomerular, tubular, or renovascular damage, CKD progression eventually converges into common renal histological and functional alterations affecting all renal structures; these changes lead to progressive and generalized fibrosis, nephron loss and replacement with scar tissue. During progression, the structural damage compromises the function of an increasingly number of nephrons. In the beginning, nephrons that are little damaged or non-affected adapt and functionally compensate the dysfunctional nephrons. As a result, the glomerular filtration rate (GFR) is not significantly decreased. Overall renal function is thus maintained until the damage halts the function of over 60% of the nephrons. By such a time, the extant nephrons, probably also somewhat compromised, are incapable of coping with the whole renal function necessary to cleanse the blood and uremia ensues (López-Novoa et al. 2010, 2011).
The kidneys have an intrinsic repair capacity, as demonstrated by the complete or almost complete structural and functional restoration after most episodes of acute lesions, even following severe acute damage (Humphreys et al. 2006). As such, we can reasonably think that a parallel repair response is initiated in the initial steps of CKD. The key and yet unanswered issue is why and through which mechanisms, the persistence of triggering damage or repetitive bouts, which are initially repairable as in acute damage events, eventually go beyond a point of no return, after which repair becomes either skewed or overwhelmed and non-reversible chronicity ensues.
Glomerulopathies are renal disorders affecting glomerular structure and function. Primary glomerulopathies encompass inflammatory glomerular diseases (glomerulonephritis) and non-inflammatory glomerulopathies, such as the consequence of hypertension and diabetes, which are the most frequent and major causes of CKD (Couser 1998). Glomerular pathogenetic mechanisms are as diverse as types of the primary glomerulopathies. Dependent on the etiology, specific glomerular diseases exhibit specific renal histopathological patterns, including focal and segmental sclerosis, diffuse sclerosis, mesangial, membranous, or endocapillary proliferation, membranous alterations and immune deposits, crescent formations, thrombotic microangiopathy and vasculitis. A serious glomerular disease may evolve through various histopathological patterns. Most commonly, these alterations have two types of consequences. On the one hand, they might disrupt the sieving properties of the glomerular filtration barrier (GFB), leading to proteinuria and tubular damage. On the other hand, they destroy the corpuscular structure leading to fibrosis and sclerosis and to reduced or blocked filtration (López-Novoa et al. 2010, 2011).
Characteristic hallmarks of tubulointerstitial diseases are tubular atrophy leading to cell infiltration, inflammation, tubule deletion and interstitial fibrosis (Cogan 1980), resulting in a significant increment in interstitial volume (Norman and Fine 1999). In early stages, glomerular filtration becomes slowly altered and tubular dysfunction constitutes the main manifestation of tubulointerstitial nephropathies (Cogan 1980; Okoń et al. 2007). As the disease progresses, the tubules collapse or become obstructed, which reduces renal filtration (López-Novoa et al. 2010, 2011). Renovascular diseases comprise a group of progressive conditions involving renal dysfunction and renal damage derived from the narrowing or blockage of the renal blood vessels. According to the US Renal Data System (2002), about one third of all end-stage renal disease cases are related to renovascular diseases. Renovascular diseases usually appear as thrombotic microangiopathies, although renal artery occlusion, renal vein thrombosis and renal atheroembolism are also potential causes. In renovascular diseases, renal dysfunction results from a reduction in renal blood flow (RFB). This leads directly to reduced filtration and to renal parenchymal damage associated with low oxygen input and ischemia. In turn, reduced RBF is the consequence of atherosclerotic narrowing or renal vasoconstriction (López-Novoa et al. 2010, 2011).
Inflammation plays a pivotal role in the progression of many, if not all, forms of CKD. In the glomerulus, inflammation exerts various effects that amplify the damage and directly contribute to the reduction in glomerular filtration (see below). Initially, inflammation is probably activated as a repair mechanism upon cellular and tissue injury. However, undetermined pathological circumstances skew persistent inflammation into a vicious circle of destruction and progression. Indeed, inflammation activates many renal cell types to produce cytokines, which directly damage renal cells and intensify inflammation.
TGF-β signaling
TGF-β is a group of three ubiquitous cytokines (named 1–3) belonging to the TGF-β superfamily. The most abundant form in mammals is TGF-β1. In addition to its transcription, a key regulatory step of TGF-β action is its activation from its reservoir, a latent protein complex in the extracellular matrix (ECM). Activation of TGF-β receptors in the cell membrane induces intracellular signals that mediate many developmental, physiological and pathological processes, including CKD (Schnaper et al. 2009). TGF-β has been recognized as a central player in many pathological events related to CKD progression, at the glomerular, tubulointerstitial and vascular levels (López-Novoa et al. 2011; Schnaper et al. 2009). Indeed, the experimental inhibition of TGF-β actions has proven efficacious at impeding or softening the chronic renal damage in a number of different pathological scenarios (López-Novoa et al. 2011; Schnaper et al. 2009), whereas TGF-β overexpression causes renal fibrosis (Kopp et al. 1996; Mozes et al. 1999).
Both the physiological and the pathological effects of TGF-β are induced by the stimulation of specific receptors in the surface membrane of target cells. The TGF-β membrane receptor complex comprises two families of proteins with serin-threonin kinase activity, namely type II (TβRII) and type I (TβRI) receptors. TβRI includes activin-like kinase (ALK) receptors. TGF-β binds to TβRII, which then recruits TβRI. The complex phosphorylates and activates several intracellular signaling cascades including (1) Smads (small mothers against decapentaplegic), (2) mitogen-activated protein kinases (MAPKs), such as extracellular regulated kinases (ERKs), p38 and Jun kinase and (3) integrin-linked kinase (ILK; Massagué and Chen 2000; Siegel and Massagué 2003). These effectors modulate the expression of target genes involved in physiological and CKD-associated events, e.g., cell growth, differentiation, apoptosis and ECM deposition.
TGF-β is also a mediator of the pathological effects induced by other hormones and cytokines, most prominently represented by the renin-angiotensin system (López-Novoa et al. 2010, 2011). Indeed, angiotensin II (Ang II), a trophic and proinflammatory hormone widely implicated in the progression of CKD stimulates the expression of TGF-β (Wolf 1998). In turn, TGF-β directly stimulates the expression of other throphic and pro-fibrotic factors, such as connective tissue growth factor (CTGF; Weston et al. 2003; Wolf 1998). Indirectly, TGF-β also induces the production of other pathological mediators, such as tumor necrosis factor alpha (TNF-α) and inteleukins, because it participates in inflammatory cell infiltration and activation and in the conversion of epithelial cells and fibroblasts into myofibroblasts (Border and Noble 1997; Strutz and Neilson 2003; Tamaki and Okuda 2003).
Glomerular effects of TGF-β
Introduction
Glomerular sclerosis is a process by which normally functional glomerular tissue is replaced by deposits of ECM, resulting in excessive protein ultrafiltration and a progressively reduced GFR. It represents a common pathway for the loss of functioning glomeruli associated with primary diseases as diverse as chronic glomerulonephritis, diabetic nephropathy, hypertension, obstructive uropathy and retroviral infection (López-Novoa et al. 2011). All three major glomerular cell types, namely podocytes or visceral epithelial cells, mesangial cells and endothelial cells participate in the fibrotic process. In addition, alterations in the glomerular basement membrane (GBM) also play a role in glomerulosclerosis. TGF-β has a major function in the pathogenesis of glomerulosclerosis. Overexpression of active TGF-β1 in transgenic mice causes mesangial expansion, interstitial fibrosis, decreased GFR and progressive proteinuria (Kopp et al. 1996).
Effect of TGF-β on podocytes
Podocytes are highly specialized pericytes that cover the outside layer of glomerular capillaries and extend long processes toward the GBM, to which they affix by cell surface adhesion proteins. The foot processes of adjacent podocytes interdigitate and are separated by narrow spaces (30–40 nm) linked by a porous membrane called the slit diaphragm, which is freely permeable to water and small solutes but relatively impermeable to plasma proteins. The integrity of the slit diaphragm is one of the principal determinants of the perm-selective properties of the GFB. Alterations in the number, structure and function of the podocytes have been reported in patients with glomerulopathies (Srivastava et al. 2001) and diabetes (Steffes et al. 2001) and in transgenic mouse models of glomerulosclerosis (Shih et al. 1999). This suggests that the loss of podocytes is significantly involved in glomerular diseases. In addition, TGF-β1 plays a major part in podocyte loss in glomerular disease. TGF-β induces podocyte apoptosis by the activation of mitogen-activated protein (MAP) kinase p38 and classic effector caspase-3 (Schiffer et al 2001). In TGF-β1–overexpressing transgenic mice, podocytes undergo apoptosis in situ shortly after the sclerotic lesion appears in the glomerulus (Schiffer et al. 2001). In patients with progressive podocyte diseases, such as focal segmental glomerulosclerosis and membranous nephropathy, the expression of TGF-β is enhanced in podocytes. Biomechanical strain in these diseases can cause the overexpression of TGF-β and Ang II by podocytes. Oxidative stress induced by Ang II might activate the latent TGF-β. Increased TGF-β activity by podocytes might induce not only the thickening of the GBM but also podocyte apoptosis and detachment from the GBM, initiating the development of glomerulosclerosis (Lee 2011). In cultured mouse podocytes, high glucose or Ang II significantly upregulates the expression of TβRII (Iglesias-de la Cruz et al. 2002; Wolf et al. 2005). This makes the podocyte more sensitive to elevated levels of TGF-β , which is produced by stimulated mesangial cells and that reaches podocytes through the glomerular ultrafiltrate (Wang et al. 2000). Ang-II-induced apoptosis in cultured podocytes is mediated by TGF-β (Ding et al. 2002). TGF-β seems also to be responsible for the detachment of podocytes from GBM (Chen et al. 2000; Regoli and Bendayan 1997). Some debate exists about which mechanism, namely podocyte apoptosis or detachment, is quantitatively more important for podocyte loss in glomerulopathies such as diabetic nephropathy. Although TGF-β has been shown to induce podocyte apoptosis in vitro and in vivo, the apoptosis rates detected in vivo are low (Nam et al. 2011). The studies of Wharram et al. (2005) have demonstrated that high rates of podocyte loss are necessary to cause glomerular scarring: depletion of podocytes by up to 40% results in only minor changes in the glomerular structure and moderate proteinuria without measurable changes in renal function, with podocyte depletion of over 40% being required before a detectable decrease in renal function can be observed. These data are in agreement with those observed in patients with type 2 diabetic nephropathy thereby demonstrating that a high level of podocyte depletion is necessary to cause macroalbuminuria and glomerulosclerosis (Dalla Vestra et al. 2003). All these data suggest that podocyte detachment is probably the main mechanism of TGF-β-mediated podocyte injury.
Furthermore, TGF-β1 stimulates endogenous vascular endothelial growth factor (VEGF) secretion by podocytes (Iglesias-de la Cruz et al. 2002), which in turn increases the production of alfa3(IV) collagen (Chen et al. 2004). Blockade of endogenous VEGF action by the specific inhibitor of VEGF receptor kinase, SU5416, reduces the TGF-β1 induced expression of alfa3(IV) collagen. Taken together, these data suggest a major role for the TGF-β1–VEGF autocrine system in the regulation of GBM composition by podocytes (Chen et al. 2004).
Effect of TGF-β on mesangial cells
Mesangial cells are crucial for glomerular function under both physiological and pathological conditions; they provide structural support for the glomerular capillary loops and modulate glomerular capillary flow and the ultrafiltration surface, thereby regulating GFR. In addition, the mesangium serves as a source and target of vasoactive hormones, growth factors, cytokines and ECM proteins and thus contributes to the pathophysiology of a variety of glomerular diseases (Sinuani et al. 2010; Schlöndorff and Banas 2009). These factors activate mesangial cells in an autocrine manner and mediate interactions with glomerular endothelial and epithelial cells and with blood-borne inflammatory cells. A major event in the glomerulosclerosis of any origin is an increase in the mesangial compartment size, attributable to both mesangial matrix deposition and mesangial cell proliferation and hypertrophy, at least in the early stage.
Strong evidence has been provided that TGF-β is important in many cases of glomerulosclerosis (Hoffman et al. 1998). TGF-β over-expression produces renal fibrosis in mice (Mozes et al. 1999) and rats (Isaka et al 1993). Conversely, intrarenal infusion of antisense oligonucleotides to decrease the expression of TGF-β ameliorates sclerosis in experimental nephropathy (Akagi et al. 1996). TGF-β plays a role in mesangial cell hypertrophy associated with diabetes and other glomerulopathies (Das et al. 2010) through a mechanisms mediated by CTGF (Wahab et al. 2002; Ito et al. 1998). TGF-β also plays also a major part in glomerular ECM accumulation in several glomerular diseases including diabetic nephropathy (Yoshioka et al. 1993; Chiarelli et al. 2009; Ziyadeh 2008). In cultured murine and human mesangial cells, TGF-β1 stimulates the production of type I and IV collagen, laminin, fibronectin and heparan sulfate proteoglycans (MacKay et al. 1989; McKay et al. 1993; Poncelet and Schnaper 1998; Suzuki et al. 1993; Rodríguez-Barbero et al. 2006). The down-regulation of ECM degradation by TGF-β also plays a major part in ECM accumulation (Baricos et al. 1999).
The mechanisms by which TGF-β stimulates ECM synthesis by mesangial cells is complex. The Smad pathway is present and functional in mesangial cells and can mediate collagen I expression (Poncelet et al. 1999). However, the inhibitory Smad7 decreases the collagen production in TGF-β-stimulated mesangial cells (Chen et al. 2002). TGF-β1 might also stimulate a variety of kinases in mesangial cells. In human and rat mesangial cells, TGF-β has been shown to activate ERK1/2, PI3K and JNK-MAP kinase pathways (Chin et al. 2001; Huwiler and Pfeilschifter 1994; Martínez-Salgado et al. 2008), whereas p38 stimulation has been found by some authors (Chin et al. 2001; Rodríguez-Barbero et al. 2006) but not by others (Hayashida et al. 1999). Activation of p38 has been implicated in TGF-β1-stimulated α1(I) collagen mRNA expression (Chin et al. 2001; Rodríguez-Barbero et al. 2006), whereas ERK1/2 has been associated with the accumulation of collagen (Hayashida et al. 1999) and fibronectin (Inoki et al. 2000).
In cultured human mesangial cells, Erk5, another MAP kinase mainly localized at the glomerular mesangium, is activated by TGF-β and the expression of a dominant-negative form of Erk5 results in a significant decrease in TGF-β1-induced collagen I expression (Dorado et al. 2008). Furthermore, the transfection of ERK5-specific small interfering RNA results in a significant decrease in ANG-II-induced soluble collagen secretion (Urushihara et al. 2010), thus suggesting that ERK5 also mediates the effect of TGF-β and Ang II on mesangial-derived ECM expansion. In addition, in human mesangial cells, mechanical stretch activates p38 MAP kinase, which independently induces TGF-β1 and fibronectin. In turn, TGF-β1 contributes to maintaining late p38 MAP kinase activation, which perpetuates fibronectin accumulation (Gruden et al. 2000).
The pro-fibrotic effect of TGF-β is modulated by endoglin. Endoglin is a type 3 TGF-β receptor that modulates some TGF-β functions (López-Novoa and Bernabeu 2010). Renal endoglin expression has been reported to be up-regulated in some models of renal fibrosis (Rodríguez-Peña et al. 2001, 2002). TGF-β also upregulates endoglin expression in cultured human and rat mesangial cells (Diez-Marques et al. 2002; Rodríguez-Barbero et al. 2001). Endoglin negatively regulates TGF-β-induced collagen I and IV synthesis (Diez-Marques et al. 2002). To assess the clinical importance of these data, endoglin expression has been studied in skin fibroblasts of patients with type 1 diabetes, namely 20 with the fastest rate of mesangial expansion (estimated by electron microscopy) and proteinuria ("fast-track"), 20 with the slowest rate and normoalbuminuria ("slow-track") and 20 controls; endoglin mRNA expression levels assessed by microarray and quantitative reverse transcription with the polymerase chain reaction were significantly higher in slow-track than in fast-track patients or controls (Alvarez-Muñoz et al. 2010). These findings suggest that endoglin can downregulate the fibrotic effects of TGF-β.
Effect of TGF-β on glomerular endothelial cells
Glomerular endothelial cells are fenestrated endothelial cells covered by a glycocalyx and characterized by their high hydraulic permeability; they share a basement membrane with podocytes and interact closely with them (Hirschberg et al. 2008). As such, glomerular endothelial cells constitute an integral part of the GFB and play key roles in the modulation of vascular tone and glomerular filtration, thrombosis and fibrosis (Navar 2009; Fogo and Kon 2010). In addition, endothelial cells have been implicated in the sclerotic process (Akaoka et al. 1995; Lee et al. 1995). In early diabetic injury, glomerular endothelial cell proliferation and capillary surface area increase resulting in glomerular hypertrophy, a characteristic of early diabetic nephropathy (Ichinose et al. 2005; Nyengaard and Rasch 1993; Yamamoto et al. 2004).
TGF-β regulates many endothelial functions including proliferation, migration and apoptosis (Lebrin et al. 2005). Arciniegas et al. (1992) have demonstrated that TGF-β1 can induce aortic endothelial cells to differentiate into cells positive for α-smooth muscle actin (α-SMA) in vitro, in a process called endothelial to mesenchymal transition (EndoMT). EndoMT has been observed in vivo in the heart, where it is induced by TGF-β and plays a role in cardiac fibrosis (Goumans et al. 2008). Similarly, EndoMT has been suggested to be involved in glomerular fibrosis by increasing the number of glomerular myofibroblasts (Zeisberg et al. 2008). The Smad3 pathway is essential for TGF-β1-induced EndoMT and for the autoinduction of TGF-β1 (Sato et al. 2003). A specific inhibitor for Smad3, SIS3, abrogates TGF-β1-induced EndoMT in renal endothelial cells and reduces diabetic glomerulosclerosis (Li et al. 2010).
Unifying hypothesis on the effect of TGF-β in glomerular sclerosis
All recent evidence suggests that mesangial cells, podocytes and endothelial cells play a critical role in the early functional and structural changes of glomerulosclerosis,. In glomerulosclerosis, glomerular cells are subjected to several types of pro-sclerotic stimuli, including physical and chemical stimuli. Cell stretch is probably the most important physical stimulus. It results from both increased intraglomerular pressure attributable to afferent vasodilatation and increased wall tension attributable to increased vascular radius secondary to glomerular hypertrophy (Laplace´s Law). Cyclic stretch caused by pulsatile changes in perfusion pressure is also crucial in inducing glomerular sclerosis, mainly in the mesangium (Cortes et al. 1999). The most important chemical stimuli are hormones and cytokines, which reach the glomerular cells from the blood or are produced by the glomerular cells themselves, acting in an autocrine and paracrine manner. These chemical stimuli include advanced glycation end products (AGE), Ang II, reactive oxygen species, TGF-β, VEGF and platelet-derived growth factor (PDGF).
Podocytes suffer the harmful effects of high glucose, AGE, Ang II, ROS, TGF-β and mechanical stretch. For instance, Ang II, whose local concentration is increased in most glomerular diseases, induces TβRII expression in podocytes, perhaps intensifying the paracrine effects of the TGF-β derived from the mesangium or glomerular endothelium. Increased TGF-β activity can lead to podocyte apoptosis and/or detachment, which induce podocytopenia and the development of progressive glomerulosclerosis. However, podocytes are also responsible for glomerular damage. Increased ANG II suppresses nephrin, which leads to the broadening and effacement of podocyte foot processes. In addition, increased VEGF production might exacerbate GBM thickening and proteinuria, leading to tubular atrophy and interstitial fibrosis.
Endothelial cell function is dependent on determined factors produced by other glomerular cells. Podocyte-derived growth factors are key for the maintenance of endothelial cell viability and function and conversely, endothelial cells affect both podocytes and mesangial cells. Podocytes produce angiogenic factors, including VEGF and angiopoietin-1 (Angio-1), which reach the glomerular endothelium and are necessary for endothelial cell survival. Mesangial cells produce Angio-2, which reaches endothelial cells, modulates endothelial cell function and might counteract the proangiogenic effects of Angio-1. Endothelial cells themselves produce numerous vasoactive factors, such as endothelin-1, renin angiotensin system factors, nitric oxide synthase and prostacyclin; they also modulate hemostasis by balancing, for example, the plasmin/plasminogen activator system and its inhibitors and upregulate adhesion molecules in response to injury.
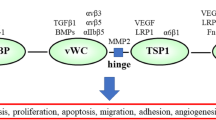
In many models of glomerulosclerosis (and in idiopathic focal segmental glomerulosclerosis), ECM accumulation often appears to begin in the mesangium. In addition, filtered macromolecules might be trapped in the mesangium and initiate an inflammatory response that possibly plays a role in stimulating ECM synthesis. Increased hyperfiltration can be caused by glomerular capillary hypertension or a genetic or acquired abnormality of podocyte adhesion or structure that allows the hyperfiltration of macromolecules. Signals from epithelial or endothelial cells to the mesangium or the direct delivery of proinflammatory substances through the glomerular filtrate initiate a process that culminates in the accumulation of ECM. In turn, mesangial expansion infringes on the capillary spaces, impairing glomerular hemodynamics and decreasing filtration surface area in the glomerular tuft. These relationships are presented schematically in Fig. 1.
Effects of TGF-β leading to glomerulosclerosis during chronic kidney disease (AGE advanced glycation end products, Angio-1 angiopoietin 1, BMbasement membrane, ECM extracellular matrix, EndoMT endothelial to mesenchymal transition, GFB glomerular filtration barrier, PDGF platelet-derived growth factor, ROS reactive oxygen species, TGF-β transforming growth factor beta, VEGF vascular endothelial growth factor)
Tubular effects of TGF-β
Regardless of CKD etiology, TGF-β exerts various effects leading to tubule deletion and fibrosis. TGF-β has been shown to mediate several key tubular pathological events during CKD progression, namely interstitial fibrosis, epithelial to mesenchymal transition (EMT) and epithelial cell death and proliferation (García-Sánchez et al. 2010). TGF-β is a strong profibrotic cytokine that activates the expression of ECM components, such as collagens I and IV and fibronectin and the inhibition of collagen-degrading enzymes such as certain matrix metalloproteinases (MMPs) involved in the control of ECM homeostasis (Eddy 1996). This leads to excessive ECM accumulation and fibrosis. In addition, TGF-β is the strongest known inducer of the EMT process in tubule epithelial cells; this process transforms them into profibrotic and pro-inflammatory myofibroblasts (López-Novoa and Nieto 2009). TGF-β also seems to be involved in the death of tubule cells. The in vivo inhibition of TGF-β, or even of Ang II, reduces the extent of tubule cell death in animal models of CKD (see below).
TGF-β in tubule loss
The involvement of TGF-β in tubule cell apoptosis has been evidenced by studies showing that the inhibition of the actions of TGF-β in vivo reduces the extent of apoptosis seen in the tubular compartment under CKD situations. For example, treatment of mice with an anti-TGF-β antibody reduces tubular apoptosis in a model of kidney damage by ureteral obstruction (Miyajima et al. 2000). This effect might result from either direct effects of TGF-β on tubular cells or indirect effects, such as fibrosis or inflammation, to the induction of which TGF-β might contribute. In this sense, some studies have reported that TGF-β activates apoptosis in cultured tubule epithelial and other cell lines (Bhaskaran et al. 2003; Docherty et al. 2006). However, the extent of cell apoptosis induced by TGF-β in cultured cells is low in these systems. On this basis, hypotheses have been proposed that either (1) the proapoptotic effect of TGF-β only takes place under pathological circumstances with the cooperation of other mediators or cytokines, or (2) amplifying mechanisms of damage are present only in vivo but are absent in in vitro systems.
Tubule loss can also occur by EMT in which tubule cells transform into mesenchymaloid cells, a process that has been postulated to contribute to tubule degeneration and renal fibrosis (López-Novoa and Nieto 2009). TGF-β is the strongest inducer of EMT in tubule cells. TGF-β initiates and completes the EMT process in vitro and in vivo under determined conditions (Liu 2004). In most in vivo studies, EMT is assessed by the appearance of fibroblastoid markers (i.e., fibroblast-specific protein, α-SMA, or vimentin) in tubule cells co-expressing epithelial markers, actin reorganization and basement membrane disruption (Liu 2004). Nevertheless, this is a transition state toward the acquisition of a full phenotype underlying the behavior as a mesenchymal fibroblastoid cell, which is used as a surrogate marker of the extent of EMT. Three TβRIs have been implicated in TGF-β-induced EMT, namely ALK 4, 5 and 7, of which ALK-5 seems to play the most central role in vivo. Upon receptor stimulation, both TGF-β-activated Smad and the ILK and ERK signaling pathways have been shown to be crucial for EMT through the modulation of the expression of key genes. Abrogation of TGF-β action by expression of mutant TGF-β receptors lacking the ability to activate Smads, together with inactive mutants of Smad-2, 3 and 4, prevent EMT-related target gene expression, EMT and excessive ECM deposition in cultured cells. In addition, the selective inhibition of components of the Ras-ERK (Xie et al. 2004) and ILK (Li et al. 2009) axis also suppresses EMT in various tumoral cell types. In addition, the lower renal level of myofibroblast markers (α-SMA and vimentin) in an in vivo model of obstructive nephropathy after ERK and PI3K/Akt inhibition is also consistent with a reduced EMT (Rodríguez-Peña et al. 2008). The Ras familiy of proteins mediates TGF-β-induced activation of ERK (Rodríguez-Peña et al. 2008). Interestingly, upon unilateral ureteral obstruction, EMT markers (α-SMA, vimentin and snail-1 and snail-2) are significantly reduced in mice lacking H-ras compared with WT mice (Grande et al. 2010a). However, although TGF-β-induced EMT is a well-defined process “in vitro”, several studies cast doubts about the quantitative relevance of EMT in “in vivo” models (for a review, see Kriz et al 2011). A detailed description of the evidence for and against a significant role of EMT on tubule degeneration in response to TGF-β “in vivo” is outside the scope of this review.
Inflammation as a mechanism of tubular damage: role of TGF-β
Injured tubular cells and immune system cells are activated by TGF-β and other growth factors to produce inflammatory cytokines and to unleash an inflammatory response in a nuclear factor kappa B (NF-κB)-dependent manner. In addition, TGF-β directly and indirectly stimulates monocyte and macrophage infiltration (Tian and Schiemann 2009). In turn, inflammation activates tubule cells, fibroblasts and myofibroblasts to produce ECM and amplifies fibrosis and tubular damage (Border and Noble 1997; Tamaki and Okuda 2003). Inflammation (1) further activates renal cells to produce TGF-β and cytokines that, in turn, stimulate fibroblasts (Strutz and Neilson 2003) and (2) activates macrophages, which damage tubule cells (Lenda et al. 2003) through the production of proapoptotic molecules, such as TNF-α, reactive oxygen species and NO. However, TGF-β is essential for the correct homeostasis of the immune system and its surveillance function (Tian and Schiemann 2009). Indeed, TGF-β1 knock-out mice exhibit spontaneous multifocal inflammation and deregulated inflammatory responses (Schull et al. 1992; Kulkarni et al. 1993). However, under pathological circumstances, an imbalance between the opposing actions of TGF-β and other cytokines probably causes the net effect of TGF-β to change from regulated repair, in order to control the extent of the inflammatory response, toward deregulated injuring inflammation.
TGF-β in tubulointerstitial fibrosis
Tubulointerstitial fibrosis is considered a central event in the progression of CKD, independently of etiology. Even in glomerulopathies, tubulointerstitial fibrosis correlates better than glomerular injury with their evolution and prognosis (Nath 1992). TGF-β is widely recognized as a strong inducer of fibrosis in renal structures during CKD. Renal fibrosis is thought not only to be a primary pathological event leading to glomerular and tubular dysfunction and degeneration but also to act as a mediator of the scarring process that replaces lost structures by abnormal ECM in the aftermath of a failed repair process. Nevertheless, the mechanisms underlying the damaging action of fibrosis on tubular cells are not well understood (García-Sánchez et al. 2010). Tubulointerstitial fibrosis is the result of an increased deposition of ECM, resulting from an increased production and an altered degradation of ECM components. The pro-fibrotic effect of TGF-β results from a number of actions including increased ECM synthesis, decreased ECM degradation, resident myofibroblast activation, EMT and inflammation. Although EMT has become widely accepted as a mechanism that contributes to the development of fibrosis in CKD, several studies suggest that unequivocal evidence supporting the contribution of EMT to kidney fibrosis is lacking (Kriz et al. 2011). In addition to stimulating EMT and inflammation, TGF-β activates resident fibroblasts, myofibroblasts and tubule epithelial cells to produce ECM components and downregulates ECM degradation (Grande and López-Novoa 2009). The transformation of the normal production of ECM for the basement membrane and tissue repair into a deleterious action is thought to be the consequence of (1) the persistence of overstimulation and (2) the imbalance of other homeostatic signalers such as other cytokines that counteract the effects of TGF-β, such as human growth factor (HGF) and bone morphogenetic protein 7 (BMP7; Zeisberg et al. 2003; Zeisberg and Kalluri 2008).
The interstitial wound in the fibrotic kidney is formed by excessive deposition of constituents of the interstitial matrix (e.g., collagens I, III, V, VII and XV and fibronectin), components restricted to tubular basement membranes in normal conditions (collagen IV and laminin) and by de novo synthesized proteins (e.g., tenascin, certain fibronectin isoforms and laminin chains; Vleming et al. 1999). Fibronectin has chemoattractant effects for the recruitment of fibroblasts and the deposition of other ECM components (Gharaee-Kermani et al. 1996). Fibroblasts, myofibroblasts, macrophages and mesangial and tubular cells are sources of fibronectin in inflammation and fibrogenesis (Eddy 1996; Van Vliet et al. 2001).
In certain types of CKD, a marked reduction of renal collagenase activity is observed. Renal fibrosis in mice with ureteral obstruction is also the result of decreased collagenolytic activity (Gonzalez-Avila et al. 1988). In damaged kidneys, the upregulation of TGF-β activation also contributes to counterbalance the natural ECM homeostatic equilibrium by downregulating the expression of determined MMPs and activating the expression of the MMP-inhibitor plasminogen activator inhibitor 1 (PAI-1; Border and Noble 1997; Cheng and Grande 2002). Moreover, TIMP-1, an endogenous tissue inhibitor of MMPs, is actively synthesized by renal cells in progressive CKD (Roberts et al. 1992) and its expression is stimulated by TGF-β, TGF-α, epithelial growth factor (EGF), PDGF, TNF-α, interleukin 1 (IL-1) and IL-6, oncostatin M, endotoxin and thrombin (Eddy 2000).
Critical view of the tubular effects of TGF-β
Inhibition of TGF-β significantly reduces tubular fibrosis and EMT markers and the tubular epithelial cell death seen in many different experimental and etiologically diverse scenarios of CKD (López-Novoa and Nieto 2009). The latter suggests a relevant pathological role of TGF-β in CKD progression. However, even under pathological circumstances, TGF-β activation might also be viewed as an element of a repair response (Massagué 1990) that, when distorted, gives way to damage progression, which can be understood as an epiphenomenon of repair. Not in vain, this coincides with the critical localization and potential sentry function of pre-active TGF-β in the ECM and basement membranes. The pathological elements that turn the repair process into degeneration are only partially known. The persistence of injuring stimulation has been hypothesized to prevail over repairing mechanisms, whose effects would taper off over time for undetermined reasons. As a consequence, the dominance of the damaging factors would make the homeostasis of the renal parenchyma cross over a point of no return and install a degenerative process in a progressively vicious circle of damage and imbalance. Accordingly, TGF-β might be considered to be a passive player in the outcome, which might mainly depend on the modulation of inflammatory and fibrotic responses by the relative level of other mediators. However, because of the absence of modulation, under pathological circumstances, TGF-β turns into a deleterious player and a subject of therapeutic targeting.
TGF-β participates in most of the mechanisms being initially activated by the damage to the tubular epithelium as a repair response. Surviving tubule cells become activated by (1) the insult itself, (2) death cell remains, (3) an absence of appropriate cell-cell signaling and (4) inflammatory mediators arising from damaged tubule cells or activated resident macrophages (initially) and infiltrated cells (progressively). In this setting, TGF-β is increasingly produced and activated by all these cells and participates in the inflammatory response and EMT. However, at some time, myofibroblasts should re-differentiate into tubule epithelial cells but this is not observed during progressive tubule degeneration in CKD. Moreover, after regenerating the intercellular scaffold and basement membranes, ECM deposition, cell activation and inflammation should cease. However, these events are also not observed in CKD.
Renal tissue repair is a tightly controlled process whereby the intensity and duration of every event must be precisely coordinated, so that cell proliferation, ECM production and the inception and resolution of inflammation take place appropriately and in a timely fashion (Chanson et al. 2005). The malfunction of any of these events might send the wrong information and alter tissue homeostasis. In this setting, TGF-β appears to have a central pathological role, as a consequence of the absence of an appropriate modulation and timely counterbalance of its effects by antagonistic mediators, such as HGF and BMP7, which converts TGF-β into a surrogate therapeutic target. After EMT-mediated tubule cell dedifferentiation, TGF-β locks the mesenchymal phenotype through the expression of snail and prevents a myofibroblast mesenchymal to epithelial transition (MET) to the tubule epithelial phenotype. In mice, BMP7 counteracts this effect, the increased ECM deposition (Zeisberg et al. 2003; Zeisberg and Kalluri 2008) and the production of pro-inflammatory cytokines (Gould et al. 2002). Moreover, the administration of exogenous BMP-7 reverses moderate fibrosis in experimental models of CKD. Under inappropriate modulation, the effects of TGF-β prevail, thereby maintaining MET, inhibiting tubule regeneration and promoting fibrosis. These events further damage the renal tissue and lead to the scarring of unrepaired areas.
Role of TGF-β in renal inflammation
Chronic renal fibrosis, even when the origin of the renal damage is not an immune disease, has a major inflammatory component, as it is accompanied by the overexpression of inflammatory genes, the release of pro-inflammatory cytokines, the activation of NF-κB and the infiltration of macrophages and lymphocytes (Grande et al. 2010b). Thus, renal fibrosis can also be considered the end result of chronic inflammatory reactions.
Continuous renal injury is associated with the increased expression of the pro-inflammatory cytokines TNF-α and IL-1 (Misseri et al. 2005; Meldrum et al. 2006) and with the activation of NF-κB, the major inflammatory response pathway, via increased IκB-alpha phosphorylation (Meldrum et al. 2006). Continuous renal injury also leads to the activation of the intrarenal renin–angiotensin system (Ruiz-Ortega et al. 2006) and Ang II behaves as a pro-inflammatory cytokine in the kidney by activating NF-κB (Ruiz-Ortega et al. 2001; Wolf 2006). In addition to NF-κB, Ang II signaling, through its receptors AT1 and AT2, also increases the expression of other proinflammatory genes, including those encoding IL-6, monocyte chemoattractant protein 1 and RANTES (regulated upon activation, normal T cell expressed and secreted; Ruiz-Ortega et al. 2001; Esteban et al. 2003). Increased Ang II production further induces renal oxidative stress (Zhong et al. 2011), which plays an important role in inducing an inflammatory state as oxidative stress is a major activator of the NF-κB pathway.
In addition to the secretion of inflammatory cytokines, the kidney and other organs release TGF-β1 after injury (Kisseleva and Brenner 2008]. TGF-β1 is considered a major anti-inflammatory cytokine (Letterio and Roberts 1998) as TGF-β1 knockout mice suffer from a lethal multifocal inflammatory disease (Kulkarni et al. 1993). The biological meaning of TGF-β1 release by renal cells in the damaged kidney is probably to moderate the inflammatory reaction and to heal the damaged tissue. Among its anti-inflammatory functions, TGF-β1 antagonizes the proinflammatory cytokines IL-1 and TNF-α in glomerular diseases and is a prominent macrophage deactivator during kidney injury (Kitamura and Suto 1997). TGF-β1 is induced by Ang II (Wolf 2006) and is also produced by interstitial fibroblasts and infiltrating macrophages (Diamond et al. 1998; Ding et al. 1993).
Even though TGF-β1 acts as an anti-inflammatory cytokine to heal the injured kidney, it also promotes the development of chronic renal disease as it plays a major role as a fibrogenic agent, as previously described. Therefore, sustained aberrant expression of TGF-β1 results in the pathological accumulation of ECM material in both the glomerulus and interstitial compartments (Bottinger 2007). TGF-β1 also has some pro-inflammatory properties, as it functions as a chemo-attractant for leukocytes (Wahl et al. 1987) and induces cyclooxygenase-2 in mesangial cells (Rodríguez-Barbero et al. 2006). The profibrotic role of TGF-β1 is also based on being a major contributor to the formation of myofibroblasts through the activation of resident fibroblasts and the induction of the transition of epithelial and endothelial cells to mesenchymal cells (EMT; Zavadil and Böttinger 2005; Zeisberg et al. 2008). Inflammation also seems to contribute to EMT, since Ang II induces the synthesis of TGF-β1 and its receptors in tubular epithelial cells (Wolf 2006).
Thus, TGF-β1, the molecule secreted to control inflammation in the kidney, also promotes the development of fibrosis (López-Novoa and Nieto 2009).
Integrative view
The preceding information reveals that TGF-β is a central player in CKD regardless of etiology, with multiple effects in all renal compartments. In this section, an integrated view of all these responses during CKD inception and progression is provided. Most renal lineages produce TGF-β when damaged or activated by auto- or paracrine mediators, including hormones, cytokines and chemokines. This local TGF-β, in turn, acts on renal structures and exerts a mixture of repair, physiological and pathological effects. Under pathological circumstances, the final effect of TGF-β is deleterious for the kidneys. For unknown reasons, very early and probably coinciding with trespassing over the point of no return, initial repair actions become distorted by the pathological scenario and turn TGF-β into a key factor of CKD progression (García-Sánchez et al. 2010), regardless of whether the disease is initiated in the glomeruli, the tubuli, or renal vessels. In any case, TGF-β gains central stage at all damaged compartments as they are recruited to degeneration.
Primarily, tubular diseases cause glomerular damage through: (1) the paracrine action of pro-inflammatory and profibrotic factors produced in the tubulointerstitial compartment, which include TGF-β and (2) tubular collapse leading to the scission of the glomeruli from the tubuli and the ulterior degeneration of the former. Similarly, primarily glomerular diseases induce tubular damage through: (1) increased filtration of proteins resulting from the lesion of the GBM, (2) para-glomerular exudates originating in glomerular sclerotic areas, (3) post glomerular low perfusion causing tubular ischemia and (4) the action of pro-inflammatory and pro-fibrotic mediators, including TGF-β, which reach the tubuli through the interstitial space or the ultrafiltrate.
As depicted in Fig. 2, TGF-β significantly contributes to a number of key pathological events leading to renal parenchymal degeneration and to reduced filtration and impaired renal function. Renal dysfunction is the result not only of renal tissue damage but also of other events that, independently, cause vasoconstriction. At the glomerular level, TGF-β mainly contributes to GFB alteration, fibrosis and sclerosis, which reduce filtration and finally cause glomerular collapse. At the tubular level, TGF-β has been shown to participate directly and indirectly in tubule degeneration. On the one hand, damaged tubuli shed tissue debris to the tubular lumen, which partially or totally obstructs them and causes filtration to decrease. On the other hand, collapsed tubuli physically split from their glomeruli and cancel the contribution of those nephrons to the overall filtration (García-Sánchez et al. 2010). Finally, inflammation acts as a mechanism of damage amplification. Pro-inflammatory cytokines activate renal cells to produce vasocontracting mediators, such as Ang II, endothelin-1 and platelet-activating factor (López-Novoa et al. 2010, 2011).
In perspective, because TGF-β is a central player of chronic renal disease, it is also a potential target for pharmacological intervention aimed at reducing or stopping CKD progression. A number of pharmaceutical companies have identified new ALK receptor inhibitors that are now under development for their application to various diseases. They might indeed have an application in the treatment of CKD progression. However, in this case, the chronic inhibition of the actions of TGF-β needs to be carefully tested for toxicity and side effects. In addition to its pathological role in CKD, TGF-β exerts many physiological effects that contribute to the homeostasis of diverse systems, organs and tissues, including the immune system, the cardiovascular system and bones.
References
Akagi Y, Isaka Y, Arai M, Kaneko T, Takenaka M, Moriyama T, Kaneda Y, Ando A, Orita Y, Kamada T, Ueda N, Imai E (1996) Inhibition of TGF-β1 expression by antisense oligonucleotides suppressed extracellular matrix accumulation in experimental glomerulonephritis. Kidney Int 50:148–155
Akaoka K, White RHR, Raafat F (1995) Glomerular morphometry in childhood reflux nephropathy, emphasizing the capillary changes. Kidney Int 47:1108–1114
Alvarez-Muñoz P, Mauer M, Kim Y, Rich SS, Miller ME, Russell GB, López-Novoa JM, Caramori ML (2010) Cellular basis of diabetic nephropathy. V. Endoglin expression levels and diabetic nephropathy risk in patients with type 1 diabetes. J Diabetes Complications 24:242–249
Arciniegas E, Sutton AB, Allen TD, Schor AM (1992) Transforming growth factor beta 1 promotes the differentiation of endothelial cells into smooth muscle-like cells in vitro. J Cell Sci 103:521–529
Baricos WH, Cortez SL, Deboisblanc M, Xin S (1999) Transforming growth factor-β is a potent inhibitor of extracellular matrix degradation by cultured human mesangial cells. J Am Soc Nephrol 10:790–795
Bhaskaran M, Reddy K, Radhakrishanan N, Franki N, Ding G, Singhal PC (2003) Angiotensin II induces apoptosis in renal proximal tubular cells. Am J Physiol Renal Physiol 284:F955–F965
Border WA, Noble NA (1997) TGF-β in kidney fibrosis: a target for gene therapy. Kidney Int 51:1388–1396
Bottinger EP (2007) TGF-β in renal injury and disease. Semin Nephrol 27:309–320
Chanson M, Derouette JP, Roth I, Foglia B, Scerri I, Dudez T, Kwak BR (2005) Gap junctional communication in tissue inflammation and repair. Biochim Biophys Acta 1711:197–207
Chen HC, Chen CA, Guh JY, Chang JM, Shin SJ, Lai YH (2000) Altering expression of alpha3beta1 integrin on podocytes of human and rats with diabetes. Life Sci 67:2345–2353
Chen R, Huang C, Morinelli TA, Trojanowska M, Paul RV (2002) Blockade of the effects of TGF-beta1 on mesangial cells by overexpression of Smad7. J Am Soc Nephrol 13:887–893
Chen S, Kasama Y, Lee JS, Jim B, Marin M, Ziyadeh FN (2004) Podocyte-derived vascular endothelial growth factor mediates the stimulation of α3(IV) collagen production by transforming growth factor-α1 in mouse podocytes. Diabetes 53:2939–2949
Cheng J, Grande JP (2002) Transforming growth factor-beta signal transduction and progressive renal disease. Exp Biol Med (Maywood) 227:943–956
Chiarelli F, Gaspari S, Marcovecchio ML (2009) Role of growth factors in diabetic kidney disease. Horm Metab Res 41:585–593
Chin BY, Mohsenin A, Li SX, Choi AM, Choi ME (2001) Stimulation of pro-alfa1(I) collagen by TGF-beta1 in mesangial cells: role of the p38 MAPK pathway. Am J Physiol Renal Physiol 280:F495–F504
Cogan MG (1980) Medical Staff Conference. Tubulo-interstitial nephropathies—a pathophysiologic approach. West J Med 132:134–140
Cortes P, Riser BL, Yee J, Narins RG (1999) Mechanical strain of glomerular mesangial cells in the pathogenesis of glomerulosclerosis: clinical implications. Nephrol Dial Transplant 14:1351–1354
Couser WG (1998) Pathogenesis of glomerular damage in glomerulonephritis. Nephrol Dial Transplant 13:10–15
Dalla Vestra M, Masiero A, Roiter AM, Saller A, Crepaldi G, Fioretto P (2003) Is podocyte injury relevant in diabetic nephropathy? Studies in patients with type 2 diabetes. Diabetes 52:1031–1035
Das F, Ghosh-Choudhury N, Kasinath BS, Choudhury GG (2010) TGFβ enforces activation of eukaryotic elongation factor-2 (eEF2) via inactivation of eEF2 kinase by p90 ribosomal S6 kinase (p90Rsk) to induce mesangial cell hypertrophy. FEBS Lett 584:4268–4272
De Vecchi AF, Dratwa M, Wiedemann ME (1999) Healthcare systems and end-stage renal disease (ESRD) therapies—an international review: costs and reimbursement/funding of ESRD therapies. Nephrol Dial Transplant 14 (Suppl 6):31–41
Diamond JR, Ricardo SD, Klahr S (1998) Mechanisms of interstitial fibrosis in obstructive nephropathy. Semin Nephrol 18:594–602
Diez-Marques L, Ortega-Velazquez R, Langa C, Rodríguez-Barbero A, López-Novoa JM, Lamas S, Bernabeu C (2002) Expression of endoglin in human mesangial cells: modulation of extracellular matrix synthesis. Biochim Biophys Acta 1587:36–44
Ding G, Pesek-Diamond I, Diamond JR (1993) Cholesterol, macrophages, and gene expression of TGF-β1 and fibronectin during nephrosis. Am J Physiol Renal Physiol 264:F577–F584
Ding G, Reddy K, Kapasi AA, Franki N, Gibbons N, Kasinath BS, Singhal PC (2002) Angiotensin II induces apoptosis in rat glomerular epithelial cells. Am J Physiol Renal Physiol 283:F173–F180
Docherty NG, O'Sullivan OE, Healy DA, Murphy M, O'Neill AJ, Fitzpatrick JM, Watson RW (2006) TGF-beta1-induced EMT can occur independently of its proapoptotic effects and is aided by EGF receptor activation. Am J Physiol Renal Physiol 290:F1202–F1212
Dorado F, Velasco S, Esparís-Ogando A, Pericacho M, Pandiella A, Silva J, López-Novoa JM, Rodríguez-Barbero A (2008) The mitogen-activated protein kinase Erk5 mediates human mesangial cell activation. Nephrol Dial Transplant 23:3403–3411
Eddy AA (1996) Molecular insights into renal interstitial fibrosis. J Am Soc Nephrol 7:2495–2508
Eddy AA (2000) Molecular basis of renal fibrosis. Pediatr Nephrol 15:290–301
Esteban V, Ruperez M, Vita JR, López ES, Mezzano S, Plaza JJ, Egido J, Ruiz-Ortega M (2003) Effect of simultaneous blockade of AT1 and AT2 receptors on the NFkappaB pathway and renal inflammatory response. Kidney Int Suppl 86:S33-S38
Fogo AB, Kon V (2010) The glomerulus—a view from the inside—the endothelial cell. Int J Biochem Cell Biol 42:1388–1397
García-Sánchez O, López-Hernández FJ, López-Novoa JM (2010) An integrative view on the role of TGF-β in the progressive tubular deletion associated with chronic kidney disease. Kidney Int 77:950–955
Gharaee-Kermani M, Wiggins R, Wolber F, Goyal M, Phan SH (1996) Fibronectin is the major fibroblast chemoattractant in rabbit anti-glomerular basement membrane disease. Am J Pathol 148:961–967
Gonzalez-Avila G, Vadillo-Ortega F, Perez-Tamayo R (1988) Experimental diffuse interstitial renal fibrosis. A biochemical approach. Lab Invest 59:245–252
Gould SE, Day M, Jones SS, Dorai H (2002) BMP-7 regulates chemokine, cytokine, and hemodynamic gene expression in proximal tubule cells. Kidney Int 61:51–60
Goumans MJ, Zonneveld AJ van, Dijke P ten (2008) Transforming growth factor beta-induced endothelial-to-mesenchymal transition: a switch to cardiac fibrosis? Trends Cardiovasc Med 18:293–298
Grande MT, López-Novoa JM (2009) Fibroblast activation and myofibroblast generation in obstructive nephropathy. Nat Rev Nephrol 5:319–328
Grande MT, Fuentes-Calvo I, Arévalo M, Heredia F, Santos E, Martínez-Salgado C, Rodríguez-Puyol D, Nieto MA, López-Novoa JM (2010a) Targeted disruption of H-Ras decreases renal fibrosis after ureteral obstruction in mice. Kidney Int 77:509–518
Grande MT, Perez-Barriocanal F, López-Novoa JM (2010b) Role of inflammation in tubulo-interstitial damage associated to obstructive nephropathy. J Inflamm (Lond) 22:19
Gruden G, Zonca S, Hayward A, Thomas S, Maestrini S, Gnudi L, Viberti GC (2000) Mechanical stretch-induced fibronectin and transforming growth factor-beta1 production in human mesangial cells is p38 mitogen-activated protein kinase-dependent. Diabetes 49:655–661
Hayashida T, Poncelet AC, Hubchak SC, Schnaper HW (1999) TGF-β1 activates MAP kinases in human mesangial cells: a possible role in collagen expression. Kidney Int 56:1710–1720
Hirschberg R, Wang S, Mitu GM (2008) Functional symbiosis between endothelium and epithelial cells in glomeruli. Cell Tissue Res 331:485–493
Hoffman BB, Sharma K, Ziyadeh FN (1998) Potential role of TGF-beta in diabetic nephropathy. Miner Electrolyte Metab 24:190–196
Humphreys BD, Duffield JS, Bonventre JV (2006) Renal stem cells in recovery from acute kidney injury. Minerva Urol Nefrol 58:329–337
Huwiler A, Pfeilschifter J (1994) Transforming growth factor β2 stimulates acute and chronic activation of the mitogen-activated protein kinase cascade in rat renal mesangial cells. FEBS Lett 354:255–258
Ichinose K, Maeshima Y, Yamamoto Y, Kitayama H, Takazawa Y, Hirokoshi K (2005) Antiangiogenic endostatin peptide ameliorates renal alterations in the early stage of a type 1 diabetic nephropathy model. Diabetes 54:2891–2903
Iglesias-de la Cruz MC, Ziyadeh FN, Isono M, Kouahou M, Han DC, Kalluri R, Mundel P, Chen S (2002) Effects of high glucose and TGF-beta1 on the expression of collagen IV and vascular endothelial growth factor in mouse podocytes. Kidney Int 62:901–913
Inoki K, Haneda M, Ishida T, Mori H, Maeda S, Koya D, Sugimoto T, Kikkawa R (2000) Role of mitogen-activated protein kinases as downstream effectors of transforming growth factor-β in mesangial cells. Kidney Int Suppl 77:S76–S80
Isaka Y, Fujiwara Y, Ueda N, Kaneda Y, Kamada T, Imai E (1993) Glomerulosclerosis induced by in vivo transfection of transforming growth factor-beta or platelet-derived growth factor gene into the rat kidney. J Clin Invest 92:2597–2601
Ito Y, Bende RJ, Oemar BS, Rabelink TJ, Weening JJ, Goldschmeding R (1998) Expression of connective tissue growth factor in human renal fibrosis. Kidney Int 53:853–861
Kisseleva T, Brenner DA (2008) Fibrogenesis of parenchymal organs. Proc Am Torac Soc 5:338–342
Kitamura M, Suto TS (1997) TGF-β and glomerulonephritis: anti-inflammatory versus prosclerotic actions. Nephrol Dial Transplant 12:669–679
Kopp JB, Factor VM, Mozes M, Nagy P, Sanderson N, Bottinger EP, Klotman PE, Thorgeirsson SS (1996) Transgenic mice with increased plasma levels of TGF-beta 1 develop progressive renal disease. Lab Invest 74:991–1003
Kriz W, Kaissling B, Le Hir M (2011) Epithelial-mesenchymal transition (EMT) in kidney fibrosis: fact or fantasy? J Clin Invest 121:468–474
Kulkarni AB, Huh CG, Becker D, Geiser A, Lyght M, Flanders KC, Roberts AB, Sporn MB, Ward JM, Karlsson S (1993) Transforming growth factor beta 1 null mutation in mice causes excessive inflammatory response and early death. Proc Natl Acad Sci USA 90:770–774
Lebrin F, Deckers M, Bertolino P, ten Dijke P (2005) TGF-beta receptor function in the endothelium. Cardiovasc Res 65:599–608
Lee HS (2011) Pathogenic role of TGF-β in the progression of podocyte diseases. Histol Histopathol 26:107–116
Lee LK, Meyer TM, Pollock AS, Lovett DH (1995) Endothelial cell injury initiates glomerular sclerosis in the rat remnant kidney. J Clin Invest 96:953–964
Lenda DM, Kikawada E, Stanley ER, Kelley VR (2003) Reduced macrophage recruitment, proliferation, and activation in colony-stimulating factor-1-deficient mice results in decreased tubular apoptosis during renal inflammation. J Immunol 170:3254–3262
Letterio JJ, Roberts AB (1998) Regulation of immune responses by TGF-β. Annu Rev Immunol 16:137–161
Li J, Qu X, Yao J, Caruana G, Ricardo SD, Yamamoto Y, Yamamoto H, Bertram JF (2010) Blockade of endothelial-mesenchymal transition by a Smad3 inhibitor delays the early development of streptozotocin-induced diabetic nephropathy. Diabetes 59:2612–2624
Li Y, Tan X, Dai C, Stolz DB, Wang D, Liu Y (2009) Inhibition of integrin-linked kinase attenuates renal interstitial fibrosis. J Am Soc Nephrol 20:1907–1918
Liu Y (2004) Epithelial to mesenchymal transition in renal fibrogenesis: pathologic significance, molecular mechanism, and therapeutic intervention. J Am Soc Nephrol 15:1–12
López-Novoa JM, Bernabeu C (2010) The physiological role of endoglin in the cardiovascular system. Am J Physiol Heart Circ Physiol 299:H959–H974
López-Novoa JM, Nieto MA (2009) Inflammation and EMT: an alliance towards organ fibrosis and cancer progression. EMBO Mol Med 1:303–314
López-Novoa JM, Martínez-Salgado C, Rodríguez-Peña AB, López-Hernández FJ (2010) Common pathophysiological mechanisms of chronic kidney disease: therapeutic perspectives. Pharmacol Ther 128:61–81
López-Novoa JM, Rodríguez-Peña AB, Ortiz A, Martínez-Salgado C, López-Hernández FJ (2011) Etiopathology of chronic tubular, glomerular and renovascular nephropathies: clinical implications. J Transl Med 9:13
MacKay K, Striker LJ, Stauffer JW, Doi T, Agodoa LY, Striker GE (1989) Transforming growth factor-beta. Murine glomerular receptors and responses of isolated glomerular cells. J Clin Invest 83:1160–1167
Martínez-Salgado C, Rodríguez-Peña AB, López-Novoa JM (2008) Involvement of small Ras GTPases and their effectors in chronic renal disease. Cell Mol Life Sci 65:477–492
Massagué J (1990) The transforming growth factor-family. Annu Rev Cell Biol 6:597–641
Massagué J, Chen YG (2000) Controlling TGF-β signaling. Genes Dev 14:627–644
McKay NG, Khong TF, Haites NE, Power DA (1993) The effect of transforming growth factor-1 on mesangial cell fibronectin synthesis: increased incorporation into the extracellular matrix and reduced pI but no effect on alternative splicing. Exp Mol Pathol 59:211–224
Meldrum KK, Metcalfe P, Leslie JA, Misseri R, Hile KL, Meldrum DR (2006) TNF-alpha neutralization decreases nuclear factor-kappaB activation and apoptosis during renal obstruction. J Surg Res 131:182–188
Misseri R, Meldrum DR, Dinarello CA, Dagher P, Hile KL, Rink RC, Meldrum KK (2005) TNF-alpha mediates obstruction-induced renal tubular cell apoptosis and proapoptotic signaling. Am J Physiol Renal Physiol 288:F406–F411
Miyajima A, Chen J, Lawrence C, Ledbetter S, Soslow RA, Stern J, Jha S, Pigato J, Lemer ML, Poppas DP, Vaughan ED, Felsen D (2000) Antibody to transforming growth factor-beta ameliorates tubular apoptosis in unilateral ureteral obstruction. Kidney Int 58:2301–2313
Mozes MM, Böttinger EP, Jacot TA, Kopp JB (1999) Renal expression of fibrotic matrix proteins and of transforming growth factor-beta (TGF-beta) isoforms in TGF-beta transgenic mice. J Am Soc Nephrol 10:271–280
Nam BY, Paeng J, Kim SH, Lee SH, Kim DH, Kang HY, Li JJ, Kwak SJ, Park JT, Yoo TH, Han SH, Kim DK, Kang SW (2011) The MCP-1/CCR2 axis in podocytes is involved in apoptosis induced by diabetic conditions. Apoptosis (in press)
Nath KA (1992) Tubulointerstitial changes as a major determinant in the progression of renal damage. Am J Kidney Dis 20:1–17
Navar LG (2009) Glomerular permeability: a never-ending saga. Am J Physiol Renal Physiol 296:F1266–F1268
Norman JT, Fine LG (1999) Progressive renal disease: fibroblasts, extracellular matrix, and integrins. Exp Nephrol 7:167–177
Nyengaard JR, Rasch R (1993) The impact of experimental diabetes mellitus in rats on glomerular capillary number and sizes. Diabetologia 36:189–194
Okoń K, Sułowicz W, Smoleński O, Sydor A, Chruściel B, Kirker-Nowak A, Rosiek Z, Sysło K, Stachura J (2007) Interstitial, tubular and vascular factors in progression of primary glomerulonephritis. Pol J Pathol 58:73–78
Poncelet AC, Schnaper HW (1998) Regulation of mesangial cell collagen turnover by transforming growth factor-beta1. Am J Physiol Renal Physiol 275:F458–F466
Poncelet AC, Caestecker MP de, Schnaper HW (1999) The TGF-beta/SMAD signaling pathway is present and functional in human mesangial cells. Kidney Int 56:1354–1365
Regoli M, Bendayan M (1997) Alterations in the expression of the alpha 3 beta1 integrin in certain membrane domains of the glomerular epithelial cells (podocytes) in diabetes mellitus. Diabetologia 40:15–22
Remuzzi G, Benigni A, Remuzzi A (2006) Mechanisms of progression and regression of renal lesions of chronic nephropathies and diabetes. J Clin Invest 116:288–296
US Renal Data System (2002) Annual Data Report: Atlas of end-stage renal disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda
Roberts AB, McCune BK, Sporn MB (1992) TGF-beta: regulation of extracellular matrix. Kidney Int 41:557–559
Rodríguez-Barbero A, Obreo J, Eleno N, Rodríguez-Peña A, Düwel A, Jerkic M, Sánchez-Rodríguez A, Bernabéu C, López-Novoa JM (2001) Endoglin expression in human and rat mesangial cells and its upregulation by TGF-beta1. Biochem Biophys Res Commun 282:142–147
Rodríguez-Barbero A, Dorado F, Velasco S, Pandiella A, Banas B, López-Novoa JM (2006) TGF-beta1 induces COX-2 expression and PGE2 synthesis through MAPK and PI3K pathways in human mesangial cells. Kidney Int 70:901–909
Rodríguez-Peña A, Prieto M, Duwel A, Rivas JV, Eleno N, Pérez-Barriocanal F, Arévalo M, Smith JD, Vary CP, Bernabeu C, López-Novoa JM (2001) Up-regulation of endoglin, a TGF-beta-binding protein, in rats with experimental renal fibrosis induced by renal mass reduction. Nephrol Dial Transplant 16 (Suppl 1):34–39
Rodríguez-Peña A, Eleno N, Düwell A, Arévalo M, Pérez-Barriocanal F, Flores O, Docherty N, Bernabeu C, Letarte M, López-Novoa JM (2002) Endoglin upregulation during experimental renal interstitial fibrosis in mice. Hypertension 40:713–720
Rodríguez-Peña AB, Grande MT, Eleno N, Arévalo M, Guerrero C, Santos E, López-Novoa JM (2008) Activation of Erk1/2 and Akt following unilateral ureteral obstruction. Kidney Int 74:196–209
Ruiz-Ortega M, Lorenzo O, Ruperez M, Blanco J, Egido J (2001) Systemic infusion of angiotensin II into normal rats activates nuclear factor-kappaB and AP-1 in the kidney: role of AT(1) and AT(2) receptors. Am J Pathol 158:1743–1756
Ruiz-Ortega M, Rupérez M, Esteban V, Rodríguez-Vita J, Sánchez-López E, Carvajal G, Egido J (2006) Angiotensin II: a key factor in the inflammatory and fibrotic response in kidney diseases. Nephrol Dial Transplant 21:16–20
Sato M, Muragaki Y, Saika S, Roberts AB, Ooshima A (2003) Targeted disruption of TGF-beta1/Smad3 signaling protects against renal tubulointerstitial fibrosis induced by unilateral ureteral obstruction. J Clin Invest 112:1486–1494
Schiffer M, Bitzer M, Roberts IS, Kopp JB, Dijke P ten, Mundel P, Bottinger EP (2001) Apoptosis in podocytes induced by TGF-beta and Smad7. J Clin Invest 108:807–816
Schlöndorff D, Banas B (2009) The mesangial cell revisited: no cell is an island. J Am Soc Nephrol 20:1179–1187
Schnaper HW, Jandeska S, Runyan CE, Hubchak SC, Basu RK, Curley JF, Smith RD, Hayashida T (2009) TGF-β signal transduction in chronic kidney disease. Front Biosci 14:2448–2465
Schull MMI, Ormsby I, Kier AM, Pawlowski S, Diebold RJ, Yin M, Allen R, Sidman C, Proetzel G, Calvin D, Annunziata M, Doetschman T (1992) Targeted disruption of the mouse transforming growth factor-b1 gene results in multifocal inflammatory disease. Nature (Lond) 359:693–699
Shih NY, Li J, Karpitskii V, Nguyen A, Dustin ML, Kanagawa O, Miner JH, Shaw AS (1999) Congenital nephritic syndrome in mice lacking CD2-associated protein. Science 286:312–315
Siegel PM, Massagué J (2003) Cytostatic and apoptotic actions of TGF-beta in homeostasis and cancer. Nat Rev Cancer 3:807–820
Sinuani I, Beberashvili I, Averbukh Z, Cohn M, Gitelman I, Weissgarten J (2010) Mesangial cells initiate compensatory tubular cell hypertrophy. Am J Nephrol 31:326–331
Srivastava T, Garola RE, Whiting JM, Alon US (2001) Synaptopodin expression in idiopathic nephrotic syndrome of childhood. Kidney Int 59:118–125
Steffes MW, Schmidt D, McCrery R, Basgen JM (2001) Glomerular cell number in normal subjects and in type 1 diabetic patients. Kidney Int 59:2104–2113
Strutz F, Neilson EG (2003) New insights into mechanisms of fibrosis in immune renal injury. Springer Semin Immunopathol 24:459–476
Suzuki S, Ebihara I, Tomino Y, Koide H (1993) Transcriptional activation of matrix genes by transforming growth factor beta1 in mesangial cells. Exp Nephrol 1:229–237
Tamaki K, Okuda S (2003) Role of TGF-β in the progression of renal fibrosis. Contrib Nephrol 139:44–65
Tian M, Schiemann WP (2009) The TGF-beta paradox in human cancer: an update. Future Oncol 5:259–271
Urushihara M, Takamatsu M, Shimizu M, Kondo S, Kinoshita Y, Suga K, Kitamura A, Matsuura S, Yoshizumi M, Tamaki T, Kawachi H, Kagami S (2010) ERK5 activation enhances mesangial cell viability and collagen matrix accumulation in rat progressive glomerulonephritis. Am J Physiol Renal Physiol 298:F167–F176
Van Vliet A, Baelde HJ, Vleming LJ, Heer E de, Bruijn JA (2001) Distribution of fibronectin isoforms in human renal disease. J Pathol 193:256–262
Vleming LJ, Bruijn JA, Es LA van (1999) The pathogenesis of progressive renal failure. Neth J Med 54:114–128
Wahab NA, Weston BS, Roberts T, Mason RM (2002) Connective tissue growth factor and regulation of the mesangial cell cycle: role in cellular hypertrophy. J Am Soc Nephrol 13:2437–2445
Wahl SM, Hunt DA, Wakefield LM, McCartney-Francis N, Wahl LM, Roberts AB, Sporn MB (1987) Transforming growth factor type β induces monocyte chemotaxis and growth factor production. Pro Natl Acad Sci USA 84:5788–5792
Wang S-N, LaPage J, Hirschberg R (2000) Role of glomerular ultrafiltration of growth factors in progressive interstitial fibrosis in diabetic nephropathy. Kidney Int 57:1002–1014
Weston BS, Wahab NA, Mason RM (2003) CTGF mediates TGF-β-induced fibronectin matrix deposition by upregulating active α5β1 integrin in human mesangial cells. J Am Soc Nephrol 14:601–610
Wharram BL, Goyal M, Wiggins JE, Sanden SK, Hussain S, Filipiak WE, Saunders TL, Dysko RC, Kohno K, Holzman LB, Wiggins RC (2005) Podocyte depletion causes glomerulosclerosis: diphtheria toxin–induced podocyte depletion in rats expressing human diphtheria toxin receptor transgene. J Am Soc Nephrol 16:2941–2952
Wolf G (1998) Link between angiotensin II and TGF-beta in the kidney. Miner Electrolyte Metab 24:174–180
Wolf G (2006) Renal injury due to renin-angiotensin-aldosterone system activation of the transforming growth factor-β pathway. Kidney Int 70:1914–1919
Wolf G, Chen S, Ziyadeh FN (2005) From the periphery of glomerular capillary wall toward the center of the disease. Podocyte injury comes on age in diabetic nephropathy. Diabetes 54:1626–1634
Xie L, Law BK, Chytil AM et al (2004) Activation of the Erk pathway is required for TGF-beta1-induced EMT in vitro. Neoplasia 6:603–610
Yamamoto Y, Maeshima Y, Kitayama H, Kitamura S, Takazawa Y, Sugiyama H (2004) Tumstatin peptide, an inhibitor of angiogenesis, prevents glomerular hypertrophy in the early stage of diabetic nephropathy. Diabetes 53:1831–1840
Yoshioka K, Takemura T, Murakami K, Okada M, Hino S, Miyamoto H, Maki S (1993) Transforming growth factor-β protein and mRNA in glomeruli in normal and diseased human kidneys. Lab Invest 68:154–163
Zavadil J, Böttinger EP (2005) TGF-β and epithelial-to-mesenchymal transitions. Oncogene 24:5764–5774
Zeisberg M, Kalluri R (2008) Reversal of experimental renal fibrosis by BMP7 provides insights into novel therapeutic strategies for chronic kidney disease. Pediatr Nephrol 23:1395–1398
Zeisberg M, Hanai J, Sugimoto H, Mammoto T, Charytan D, Strutz F, Kalluri R (2003) BMP-7 counteracts TGF-beta1-induced epithelial-to-mesenchymal transition and reverses chronic renal injury. Nat Med 9:964–968
Zeisberg EM, Potenta SE, Sugimoto H, Zeisberg M, Kalluri R (2008) Fibroblasts in kidney fibrosis emerge via endothelial-to-mesenchymal transition. J Am Soc Nephrol 19:2282–2287
Zhong J, Guo D, Chen CB, Wang W, Schuster M, Loibner H, Penninger JM, Scholey JW, Kassiri Z, Oudit GY (2011) Prevention of angiotensin II-mediated renal oxidative stress, inflammation, and fibrosis by angiotensin-converting enzyme. Hypertension 57:314–322
Ziyadeh FN (2008) Different roles for TGF-beta and VEGF in the pathogenesis of the cardinal features of diabetic nephropathy. Diabetes Res Clin Pract 82 (Suppl 1):S38–S41
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
López-Hernández, F.J., López-Novoa, J.M. Role of TGF-β in chronic kidney disease: an integration of tubular, glomerular and vascular effects. Cell Tissue Res 347, 141–154 (2012). https://doi.org/10.1007/s00441-011-1275-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-011-1275-6