Abstract
Blastocystis hominis is the most common intestinal parasite in humans. An extensive genetic variability has been described recently in B. hominis isolates. The aim of this study was to analyze genotypes of B. hominis isolates obtained from the healthy individuals and patients with irritable bowel syndrome-diarrhea (IBS-D). The patients with IBS-D were enrolled from gastroenterology outpatient department at the Aga Khan University Hospital. History and physical examination was done. Stool microscopy, culture, and polymerase chain reaction for B. hominis genotyping were carried out. The study included 158 patients with IBS-D, mean age 41 ± 15, age range 16–83 years, and male/female ratio of 109:49. One hundred fifty-seven (49.8%) were taken as healthy control. The dominant B. hominis genotypes were genotype 1 in 87 (65%) and type 3 in 49 (37%). In IBS-D, genotype 1 was present in 75 (86%; P < 0.001) compared to 12 (14%) in controls while type 3 was present in 23 (47%) compared to 26 (53%) in controls (P < 0.001), respectively. Infection with single genotype of B. hominis was present in 70 (73%) with IBS-D and in 26 (27%) in control group while with multiple genotypes in 25 (64%) in IBS-D and 14 (36%) in control group (P = 0.30), respectively. Majority of our patients had typeable B. hominis infection. The genotype of B. hominis in IBS-D was type 1 while in control genotype 3 was predominant.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Blastocystis hominis is a common intestinal protozoan parasite of humans and many animals. It has a worldwide distribution and is often the most commonly isolated organism found in human stools. The prevalence and incidence of human Blastocystis infections may be more common than is known. It demonstrates morphological diversity and the commonly used diagnostic techniques such as light microscopy of fecal smears, concentrates, or permanently stained smears that have low sensitivity (Stensvold et al. 2006). Culture of B. hominis which is more sensitive for detection of the B. hominis in fecal samples is not routinely done in many laboratories. Despite years of study, the pathogenic role of B. hominis is still regarded by some as controversial as it is frequently found not only in individuals with enteric symptoms but also in apparently healthy and asymptomatic subjects (Tan et al. 2002). Extensive genetic diversity was demonstrated among human B. hominis by various molecular techniques (Clark 1997; Hoevers et al. 2000; Yoshikawa et al. 2004c). It is thought that establishing relevant genotypic differences between the asymptomatic and symptomatic isolates should assist in determining the pathogenicity of Blastocystis by clearly assigning symptoms to its genotype. Several methods that include arbitrarily primed polymerase chain reaction (PCR), subtype-specific sequence-tagged-site (STS) primers, have been developed and used in several studies to detect genetic variations (Arisue et al. 2003; Yoshikawa et al., 2003). This PCR-based technique is currently being used for typing B. hominis isolates from humans and animals (Abe et al. 2003c; Li et al. 2007b; Yan et al. 2006; Yoshikawa et al. 2004c).
In a previous study in Pakistan, the prevalence of B. hominis infection was determined in different age and sex groups (Haider and Baqai 2008). Two hundred and thirty fecal samples were collected from patients with gastrointestinal symptoms, and direct microscopy was used with formol-ether concentration method. Parasites were detected in 161 (70%) of patients with B. hominis present in 31% (Haider and Baqai 2008). In another study, the prevalence of intestinal parasitic infections was 53% among children 1 to 5 years old (Mehraj et al. 2008). Giardia lamblia was the most common parasite followed by Ascaris lumbricoides, B. hominis, and Hymenolepis nana (Mehraj et al. 2008). These studies did not examine subtypes of Blastocystis isolates, which is important as it has been proposed that genetically different genotype (subtype) may be correlated with pathogenic potential (Hussein et al. 2008; Tan 2008; Yan et al. 2006). The aim of this study was to analyze genotypes of B. hominis isolates obtained from patients with irritable bowel syndrome-diarrhea (IBS-D) as defined by Rome III criteria and healthy controls by in vitro culture and PCR using seven kinds of STS primers and to determine the correlation between the genotype and symptomatology.
Material and methods
Sources and isolates of B. hominis
A total of 315 stool samples were obtained from patients with IBS-D 158 (50.2%) and healthy controls 157 (49.8%) who attended the gastroenterology outpatient clinic at the Aga Khan University, Karachi between September 2007 and November 2009, respectively. In IBS-D group patients presented with abdominal pain or discomfort associated with diarrhea. The Rome III criteria for IBS-D states at least 12 weeks or more, which need not be consecutive, in the preceding 12 months of stool frequency greater than three bowel movements per day, abnormal stool form, e.g., loose/watery stool and abnormal stool passage, i.e., urgency (Longstreth et al. 2006). In control group, there were healthy volunteers or those with upper abdominal discomfort not suggestive of IBS. These patients underwent thorough history, physical examination, complete blood count, erythrocyte sedimentation rate, liver function tests, blood urea nitrogen, creatinine, electrolytes, stool microscopy, culture, and PCR for genotyping of B. hominis. The study was approved by the institutional ethics review committee. Technologists were unaware of the classification status of the patients. All the stool specimens for microscopy and culture of B. hominis were processed by the same technicians, and a note was made for presence of other parasites such as G. lamblia, Entamoeba histolytica, etc. A microbiological investigation was also performed to detect Salmonella spp., Campylobacter jejuni, Clostridium difficile, and Vibrio cholerae. However, a viral screen was not performed on stool specimens obtained in view of cost limitations.
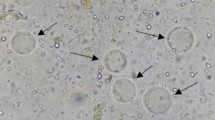
Microscopy of fecal smear
Fecal sample microscopy was done as described before (Zaman and Khan 1994). Briefly, approximately 2 mg of feces was thoroughly emulsified on a glass slide in one drop of physiologic saline and covered with a cover slip. A similar preparation was made on another slide using Lugol’s iodine. These preparations were examined under both the low power (×10) and high dry (×40) objectives.
Culture of feces
Cultures were done by inoculating approximately 50 mg of feces into Jones’ medium. For culturing B. hominis, Jones medium without starch was used (Zaman and Khan 1994). The cultures were incubated at 37°C and examined after 2–3 days. The sediment was examined under both the low power (×10) and high dry (×40) objectives. The positive samples were subcultured for another 3 days using fresh media.
Extraction of genomic DNA
Genomic DNA of Blastocystis was extracted by using Stool DNA Extraction kit (Qiagen) according to the manufacturer's protocol. Extracted DNA was stored at −20°C until PCR was carried out for B. hominis genotyping.
Genotyping by PCR with STS primers
Seven kinds of STS primers developed for typing the Blastocystis isolates were used as described previously (Abe et al. 2003a, b, c; Li et al. 2007a, b; Yan et al. 2006; Yoshikawa et al. 1998, 2000, 2003). Seven standardized subtype-specific STS primers were used, namely SB83 (351 bp) for subtype 1, SB340 (704 bp) for subtype 2, SB227 (526 bp) for subtype 3, SB337 (487 bp) for subtype 4, SB336 (317 bp) for subtype 5, SB332 (338 bp) for subtype 6, and SB155 (650 bp) for subtype 7 (Yoshikawa et al. 2003), according to a recent classification terminology (Stensvold et al. 2007). Typing of the Blastocystis isolates was conducted through PCR amplification on the basis of the presence or absence of the products within parallel control PCR amplification. The PCR conditions consisted of one cycle denaturing at 94°C for 3 min, 30 cycles including annealing at 59°C for 30 s, extending at 72°C for 60 s, denaturing at 94°C for 30 s, and additional cycle with a 5-min chain elongation at 72°C (PCR System 9700, Perkin Elmer, USA). The PCR products and molecular markers were electrophoresed in 2% agarose gel with Tris–acetate–EDTA electrophoresis buffer. The size markers were 100-bp ladder (Promega, USA). The PCR amplification for each primer pair was repeated at least thrice. Bands were visualized by the imaging system (Gel Doc 2000, Gel Documentation System, Bio Rad, UK) after being stained with ethidium bromide.
Statistical method
Results are expressed as mean ± standard deviation for continuous variables (e.g., age) and number (percentage) for categorical data (e.g., gender, stool culture, diarrhea, etc.). Univariate analysis was performed by using the independent sample t test. Pearson Chi-square test and Fisher’s exact test were also used whenever appropriate. A P value of <0.05 was considered as statistically significant. All P values were two sided. Statistical interpretation of data was performed by using the computerized software program SPSS version 16.0.
Results
Of the 315 enrolled, 158 (50.2%) had IBS-D while 157 (49.8%) were controls. The symptoms consisted of diarrhea in 158 (50%), abdominal pain in 43 (14%), and no gastrointestinal symptoms in 114 (36%). In fecal samples examined, 119 (38%) were positive for B. hominis on stool microscopy and 133 (42%) on stool culture (Table 1). Stool microscopy was significantly positive for B. hominis in patients with IBS-D, 87 (73%; P < 0.001) compared to 32 (27%) in control (Table 1). Stool culture was also significantly positive for B. hominis in patients with IBS-D, 95 (71%; P < 0.001) compared to 38 (29%) in control (Table 1).
Identification of B. hominis genotypes by PCR
In IBS-D, B. hominis subtype 1 infection was present in 75 (86%; P < 0.001) compared to 12 (14%) in controls while subtype 3 was present in 23 (47%) with IBS-D compared to 26 (53%) in controls (P < 0.001; Table 2).
Genotypes associated with groups
Blastocystis infection with single genotype was present in 96 (30.5%) while with two or more genotypes in 39 (12.5%). B. hominis infection with single genotype was seen in 70 (73%) with IBS-D compared to 26 (27%) in control while infection with two or more B. hominis subtypes were present in 25 (64%) with IBS-D and 14 (36%) in control (P = 0.30). B. hominis infection with single or multiple subtypes did not demonstrate age and gender predisposition.
Discussion
In this study, prevalence of B. hominis infection in IBS-D was 71%, which superseded the 29% seen in control (Table 1). This is consistent with our previous study where an increase in incidence of B. hominis infection was demonstrated in association with IBS compared to healthy population (Yakoob et al. 2004). However, this is also in contrast to other local studies in symptomatic patients with diarrhea that described a B. hominis prevalence of 31% in adults (Haider and Baqai 2008) and 53% among children 1 to 5 years old (Mehraj et al. 2008). However, in both studies, culture of B. hominis that is known to be more sensitive than other routine parasitological examination techniques (Windsor et al. 2002) was not carried out. Therefore, the actual prevalence of B. hominis might be higher than reported in these studies (Mehraj et al. 2008; Haider and Baqai 2008). This study showed that all the seven B. hominis genotypes based on STS primers were found in Pakistan (Table 2). B. hominis subtypes 1 and 3 were predominant. Blastocystis subtypes 2, 4 5, 6, and 7 infection were also demonstrated in our patient and controls varying from 2.5% to 3% (Table 2). Subtype 1 was commonly found in IBS-D while subtype 3 was equally common in patients with IBS-D and in the controls. In individual patients, Blastocystis subtypes 1 and 3 were also common as the cause of multiple genotype infection. B. hominis infection with single subtype was common compared to one with multiple subtypes. These results are in keeping with Yoshikawa et al. (2004a) who, using STS primers, examined five populations of human B. hominis isolates obtained from Japan, Pakistan, Bangladesh, Germany, and Thailand. The most dominant genotype among four populations was subtype 3 varying from 41.7% to 92.3% followed by among four populations excluding Thailand, which was either subtype 1 (7.7–25.0%) or subtype 4 (10.0–22.9%). However, in this study, limited number of isolates was examined from Pakistan to draw any conclusion regarding B. hominis subtypes found in our population.
The implications of this study are that Blastocystis subtype 1 infection was common in the IBS-D population. However, presence of subtype 3 in this group does not necessarily mean that it is also associated with symptoms though there have been studies that demonstrated subtype 3 commonly associated with subtype 1 (Yoshikawa et al. 2004a; Table 3). Hussein et al. (2008), in their study of experimental infection in animals with human Blastocystis isolates, demonstrated that subtype 1 was associated with elevated pathogenicity. Recently, Yan et al. (2006) also demonstrated predominant subtype 1 in a group of symptomatic patients with Blastocystis. In this study, control subjects were mostly healthy without symptoms that are suggestive of IBS-D, and in them, subtype 3 was predominant followed by subtype 1 (Table 3). Blastocystis subtype 5 infections which indicate zoonosis was equally common in the control and IBS-D groups (Table 2; Yan et al. 2007). This subtype 5 infection in our subjects might be explained on the basis that we are a developing country with a high incidence of infections transmitted by feco-oral route due to unavailability of clean water for usage among many other factors (Zaman and Khan 1994). The frequency of mixed infections with different subtypes was 39 (12.4%) with predominance of mixed infection by subtypes 1 and 3 in 18 (6%). Other studies have also reported low prevalence of mixed infections with different subtypes (Yan et al. 2006; Li et al. 2007a, b; Yoshikawa et al. 2004b) suggesting geographical variation.
This is the first investigation of molecular epidemiology of human Blastocystis in Pakistan, and it indicates the predominance of subtype 1 and 3 among human cases, as in other regions of the world.
References
Abe N, Wu Z, Yoshikawa H (2003a) Molecular characterization of Blastocystis isolates from birds by PCR with diagnostic primers and restriction fragment length polymorphism analysis of the small subunit ribosomal RNA gene. Parasitol Res 89:393–396
Abe N, Wu Z, Yoshikawa H (2003b) Molecular characterization of Blastocystis isolates from primates. Vet Parasitol 113:321–325
Abe N, Wu Z, Yoshikawa H (2003c) Zoonotic genotypes of Blastocystis hominis detected in cattle and pigs by PCR with diagnostic primers and restriction fragment length polymorphism analysis of the small subunit ribosomal RNA gene. Parasitol Res 90:124–128
Arisue N, Hashimoto T, Yoshikawa H (2003) Sequence heterogeneity of the small subunit RNA genes among Blastocystis isolates. Parasitology 126:1–9
Clark CG (1997) Extensive genetic diversity in Blastocystis hominis. Mol Biochem Parasitol 87:79–83
Dogruman-Al F, Dagci H, Yoshikawa H, Kurt O, Demirel M (2008) A possible link between subtype 2 and asymptomatic infections of Blastocystis hominis. Parasitol Res 103:685–689
Eroglu F, Genc A, Elgun G, Koltas IS (2009) Identification of Blastocystis hominis isolates from asymptomatic and symptomatic patients by PCR. Parasitol Res 105:1589–1592
Haider SS, Baqai R (2008) Detection of Blastocystis hominis in Humans and Poultry. IDJ Pakistan 17:43–47
Hoevers J, Holman P, Logan K, Hommel M, Ashford R, Snowden K (2000) Restriction-fragment-length polymorphism analysis of small-subunit rRNA genes of Blastocystis hominis isolates from geographically diverse human hosts. Parasitol Res 86:57–61
Hussein EM, Hussein AM, Eida MM, Atwa MM (2008) Pathophysiological variability of different genotypes of human Blastocystis hominis Egyptian isolates in experimentally infected rats. Parasitol Res 102:853–860
Li LH, Zhou XN, Du ZW, Wang XZ, Wang LB, Jiang JY, Yoshikawa H, Steinmann P, Utzinger J, Wu Z, Chen JX, Chen SH, Zhang L (2007a) Molecular epidemiology of human Blastocystis in a village in Yunnan province, China. Parasitol Int 56:281–286
Li LH, Zhang XP, Lv S, Zhang L, Yoshikawa H, Wu Z, Steinmann P, Utzinger J, Tong XM, Chen SH, Zhou XN (2007b) Cross-sectional surveys and subtype classification of human Blastocystis isolates from four epidemiological settings in China. Parasitol Res 102:83–90
Longstreth GL, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC (2006) Functional Bowel Disorders. Gastroenterology 130:1480–1491
Mehraj V, Hatcher J, Akhtar S, Rafique G, Beg MA (2008) Prevalence and factors associated with intestinal parasitic infection among children in an urban slum of Karachi. PLoS ONE 3:3680
Stensvold CR, Brillowska-Dabrowska A, Nielsen HV, Arendrup MC (2006) Detection of Blastocystis hominis in unpreserved stool specimens by using polymerase chain reaction. J Parasitol 92:1081–1087
Stensvold CR, Suresh GK, Tan KSW, Thompson RCA, Traub RJ, Viscogliosi E, Yoshikawa H, Clark CG (2007) Terminology for Blastocystis subtypes—a consensus. Trends Parasitol 23:93–96
Tan KSW (2008) New insights on classification, identification and clinical relevance of Blastocystis spp. Clin Microbiol Rev 21:639–665
Tan KS, Singh M, Yap EH (2002) Recent advances in Blastocystis hominis research: hot spots in terra incognita. Int J Parasitol 32:789–804
Windsor JJ, Macfarlane L, Hughes-Thapa G, Jones SKA, Whiteside TM (2002) Incidence of Blastocystis hominis in fecal samples submitted for routine microbiological analysis. Br J Biomed Sci 59:154–157
Yakoob J, Jafri W, Jafri N, Khan R, Islam M, Beg MA, Zaman V (2004) Irritable bowel syndrome: in search of an etiology: role of Blastocystis hominis. Am J Trop Med Hyg 70:383–385
Yan Y, Su S, Ye J, Lai R, Liao H, Ye J, Li X, Luo X, Chen G (2006) Genetic variability of Blastocystis hominis isolates in China. Parasitol Res 99:597–601
Yan Y, Su S, Ye J, Lai X, Lai R, Liao H, Chen G, Zhang R, Hou Z, Luo X (2007) Blastocystis sp. subtype 5: a possibly zoonotic genotype. Parasitol Res 101:1527–1532
Yoshikawa H, Nagano I, Wu Z, Yap EH, Singh M, Takahashi Y (1998) Genomic polymorphism among Blastocystis hominis strains and development of subtype-specific Diagnostic primers. Mol Cell Probes 12:153–159
Yoshikawa H, Abe N, Iwasawa M, Kitano S, Nagano I, Wu Z, Takahashi Y (2000) Genomic analysis of Blastocystis hominis strains isolated from two long-term health care facilities. J Clin Microbiol 38:1324–1330
Yoshikawa H, Abe N, Wu Z (2003) Genomic polymorphism among Blastocystis isolates and development of PCR-based identification of zoonotic isolates. J Eukaryot Microbiol 50:710–711
Yoshikawa H, Morimoto K, Wu Z, Singh M, Hashimoto T (2004a) Problems in speciation in the genus Blastocystis. Trends Parasitol 20:251–255
Yoshikawa H, Wu Z, Kimata I, Iseki M, Ali IK, Hossain MB, Zaman V, Haque R, Takahashi Y (2004b) Polymerase chain reaction-based subtype classification among human Blastocystis hominis populations isolated from different countries. Parasitol Res 92:22–29
Yoshikawa H, Abe N, Wu Z (2004c) PCR-based identification of zoonotic isolates of Blastocystis from mammals and birds. Microbiology 150:1147–1151
Zaman V, Khan K (1994) A comparison of direct microscopy with culture for the diagnosis of Blastocystis hominis. Southeast Asian J Trop Med Hyg Public Health 25:792–793
Acknowledgment
This study was supported by a grant from the Higher Educational Commission of Pakistan Project no. 20-774 to JY. We are grateful to the staff of the Juma Research Laboratory for their help during the completion of this work.
Conflict of interests
The authors declare that they have no conflict of interest.
Ethical standards
Formal ethics approval was granted by the Ethics Review Committee of the institution for this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00436-011-2567-1
An erratum to this article is available at http://dx.doi.org/10.1007/s00436-011-2567-1.
Rights and permissions
About this article
Cite this article
Yakoob, J., Jafri, W., Beg, M.A. et al. Irritable bowel syndrome: is it associated with genotypes of Blastocystis hominis . Parasitol Res 106, 1033–1038 (2010). https://doi.org/10.1007/s00436-010-1761-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00436-010-1761-x