Abstract
Purpose
Elastin is a signature protein of lungs. Increased elastin turnover driven by altered proteolytic activity is an important part of lung tumorigenesis. Elastin-derived fragments have been shown to be pro-tumorigenic, however, little is known regarding the biomarker potential of such elastin fragments. Here, we present an elastin turnover profile by non-invasively quantifying five specific elastin degradation fragments generated by different proteases.
Methods
Elastin fragments were assessed in serum from patients with stage I–IV non-small cell lung cancer (NSCLC) (n = 40) and healthy controls (n = 30) using competitive ELISAs targeting different protease-generated fragments of elastin: ELM12 (generated by matrix metalloproteinase MMP-9 and -12), ELM7 (MMP-7), EL-NE (neutrophil elastase), EL-CG (cathepsin G) and ELP-3 (proteinase 3).
Results
ELM12, ELM7, EL-NE and EL-CG were all significantly elevated in NSCLC patients (n = 40) when compared to healthy controls (n = 30) (ELM12, p = 0.0191; ELM7, p < 0.0001; EL-NE, p < 0.0001; EL-CG, p < 0.0001). ELP-3 showed no significant difference between patients and controls (p = 0.8735). All fragments correlated positively (Spearman, r: 0.69–0.81) when compared pairwise, except ELM12 (Spearman, r: 0.042–0.097). In general, all fragments were detectable across all stages of the disease.
Conclusions
Elastin fragments generated by different proteases are elevated in lung cancer patients compared to healthy controls but differ in their presence. This demonstrates non-invasive biomarker potential of elastin fragments in serum from lung cancer patients and suggests that different pathological mechanisms may be responsible for the elastin turnover, warranting further validation in clinical trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer is one of the leading causes of cancer death in both men and women (Siegel et al. 2018). Non-small cell lung cancer (NSCLC) comprise roughly 80% of all lung cancer cases and has several subtypes, of which adenocarcinoma (AC) and squamous cell carcinoma (SCC) are the most common (Zamay et al. 2017). Most patients are diagnosed late, after the cancer has spread to distant tissues. For these patients, the 5-year survival rate is only 5%, as opposed to 55% for patients diagnosed with a localized tumor (Siegel et al. 2018). This makes early detection and identification of high-risk individuals critical for improving survival.
Changes in the tumor microenvironment caused by chronic inflammation and desmoplasia forms an environment that drives cancer characteristics, such as unhindered proliferation or invasion, thereby contributing to an aggressive cancer phenotype (Landskron et al. 2014). Thus, the tumor microenvironment has an active role in cancer progression. A major component of the tumor microenvironment is the extracellular matrix (ECM), the non-cellular component of tissues, and the key factor for maintaining tissue microarchitecture and cell polarity (Halaoui and McCaffrey 2015). In healthy tissue, the ECM is maintained in a delicate balance between formation and degradation of proteins. This balance is often compromised in cancer, partly due to tumor-associated proteases such as matrix metalloproteases (MMP) that can modulate the composition of the ECM and the interaction between the tumor and its environment (Balkwill et al. 2012; Noël et al. 2012). Biomarkers that reflect these changes could have great clinical potential. Such biomarkers may be found by investigating the proteases and the protein fragments they release to the circulation, where they can be detected in the blood.
Elastin is a signature ECM protein of the lungs. Elastic fibers are key in maintaining structure and function of tissues. They provide elasticity, which is critical for the function of tissues such as the lungs, skin or arteries. Elastic fibers comprise primarily of elastin, forming the core, and microfibrils forming a sheath on the outside of the fiber. Elastin is formed by crosslinking of its precursor tropoelastin, which is catalyzed by lysyl oxidase (Mithieux and Weiss 2005). In healthy tissue, there is very little turnover of the mature cross-linked elastin; this is altered in cancer and a link to lung cancer has already been suggested (Wise and Weiss 2009; Starcher et al. 2013). For example, the release of amino acids desmosine and isodesmosine as markers for degradation of mature cross-linked elastin are elevated in the urine of lung cancer patients (Starcher et al. 2013). Cleavage of elastin not only affects tissue structure, but can also generate bioactive peptides, called matrikines, that can modulate diverse cellular processes (Ricard-Blum and Vallet 2016). The three serine proteases neutrophil elastase (NE), cathepsin G (CG) and proteinase 3 (PR3) as well as MMP-7, -9 and -12 can all generate bioactive peptides from elastin cleavage (Taddese et al. 2008; Heinz et al. 2010, 2011, 2012).
The aim of this study was to validate an elastin degradation assay specific to MMP-9 and -12 cleaved elastin, named ELM12. Along with ELM12, an MMP-7-specific elastin fragment [ELM7, (Kristensen et al. 2015b)], a NE-fragment [EL-NE, (Kristensen et al. 2015a)], CG-fragment [EL-CG, (Gudmann et al. 2018)] and PR3-fragment [ELP-3, (Gudmann et al. 2018)] were evaluated in serum from NSCLC patients for their potential as non-invasive lung cancer biomarkers.
Methods
Patient samples
The NSCLC cohort was obtained from the commercial vendor Proteogenex (Culver City, CA, USA). It included 40 patients with NSCLC in stages I, II, III and IV. Tumor stage and the histological subtypes adenocarcinoma (AC) and squamous cell carcinoma (SCC) were defined according to the criteria of the American Joint Committee on Cancer (AJCC) and International Union against Cancer (IUCC). The controls (n = 30) included colonoscopy-negative individuals with no symptomatic or chronic disease from Proteogenex, as well as healthy volunteers from the commercial vendor Valley Biomedical (Winchester, VA, USA). According to the vendors, an appropriate Institutional Review Board/Independent Ethical Committee approved sample collection, and all the patients filed informed consent. All investigations were carried out in accordance with the Helsinki Declaration.
ELISA protocols for assessment of elastin degradation fragments in serum of NSCLC patients
All the ELISA assays used a monoclonal antibody targeting a protein fragment generated by a specific protease. ELM7 (generated by MMP-7), EL-NE (generated by neutrophil elastase), EL-CG (generated by cathepsin G) and ELP-3 (generated by proteinase 3) were measured as previously described (Kristensen et al. 2015a, b; Gudmann et al. 2018). Generation of monoclonal antibodies to target the ELM12 neo-epitope and characterization of the clones has been described previously (Skjøt-Arkil et al. 2013). The antibodies used in this study are sub-cloned variants of the previously described antibodies. The final ELISA protocol for measuring ELM12 is described below. All samples that measured below the limit of measurement range (LLMR) were stated as the value of LLMR.
Technical validation of ELM12 assay
Optimization of assay buffer and incubation time and temperature was determined, as well as optimal antibody and coater peptide concentrations. Antibody specificity was determined by twofold dilutions of the standard peptide (GVAPGIGPGG), elongated peptide (GVAPGIGPGGV), truncated peptide (GVAPGIGPG), non-sense standard peptide (LLARDFEKNY) and a non-sense coater peptide (Biotin-ADWGQSRDAEEAISQ). The inter- and intra-assay variation was determined by ten independent runs using five quality control samples and two kit controls. Each sample was run in double-determinations. Three of the quality control samples were human serum and two were standard peptide in assay buffer. Intra-assay variation was calculated as the mean coefficient of variance (CV%) of each of the ten runs. Inter-assay variation was calculated as the CV% across the ten runs. Lower limit of measurement range (LLMR) and Upper limit of measurement range (ULMR) was calculated based on the ten inter- and intra-assay runs. Linearity was assessed by performing twofold dilutions of human serum or plasma samples. Linearity was calculated as the percentage recovery of the undiluted sample. Accuracy was determined by spiking cleaved elastin into a healthy human serum sample. Spiking recovery was calculated as the percentage recovery of the measured value and the serum sample concentration plus the spiking analyte. Interference was measured in human serum spiked with high or low amounts of hemoglobin (high = 0.310 mM, low = 0.155 mM), lipid (high = 10.98 mM, low = 4.83 mM) or biotin (high = 90 ng/ml, low = 30 ng/ml). Interference was calculated as the percentage recovery of the non-spiked sample. Analyte stability was determined for three human serum samples incubated at 4 °C or 20 °C for 2, 4, 24 or 48 h. Stability was calculated by the percentage variation from the control sample, kept at − 20 °C (0 h sample). Additionally, the stability of samples exposed to 1–4 freeze–thaw cycles was evaluated. Stability was calculated by the percentage variation from the sample that underwent one freeze–thaw cycle.
The final ELM12 assay protocol was performed as follows: a 96-well streptavidin-coated ELISA plate was coated with 100 µl of 5.83 ng/ml biotinylated GVAPGIGPGG peptide dissolved in assay buffer [50 mM PBS, 1% BSA (w/v), 0.1% Tween-20 (w/v), pH 7.4, 4 g/l NaCl] and incubated for 30 min at 20 °C with shaking at 300 rpm. Following a washing cycle, 20 µl of sample was added in duplicates followed by 100 µl of 29.2 ng/ml monoclonal antibody in assay buffer and incubated for 1 h at 20 °C with shaking. Following a washing cycle, 100 µl of goat anti-mouse HRP-antibody (Thermo Scientific, Waltham, MA, USA, cat# 31437) diluted to a final concentration of 130 ng/ml was added and incubated for 1 h at 20 °C with shaking. Following a washing cycle, 100 µl of 3,3′,5,5′-tetramethylbenzidine (TMB) (Kem-En-Tec, cat# 438OH) was added and incubated for 15 min at 20 °C with shaking. Finally, the TMB reaction was stopped by adding 100 µl 1% H2SO4. Absorbance was measured at 450 nm and 650 nm as reference. During each washing cycle, the plate was washed five times with washing buffer (20 mM Tris, 50 mM NaCl, pH 7.2). Addition of 20 µl of 250 ng/ml GVAPGIGPGG peptide, serially diluted 1:2 was used to generate a standard curve plotted by a four-parametric mathematical fit model. Each plate included two kit controls to monitor intra- and inter-assay variation.
Cleavage of soluble elastin from human lung
Solubilized elastin purified from human lung (Sigma-Aldrich, cat# E7277) was diluted in MMP buffer (50 mM Tris–HCl, 150 mM NaCl, 10 mM CaCl2, 10 µM ZnCl, 0.05% Brij-35, pH 7.5) or NE buffer (50 mM Tris–HCl, 150 mM NaCl, pH 7.5) to a final concentration of 100 µg/ml. The elastin and protease solutions were incubated at 37 °C for 4 or 24 h with or without the following: MMP-12 (Giotto cat# G04MP12Cm), MMP-9 (Giotto, cat# G04MP09C), MMP-7 (Giotto, cat# G04MP07C), human NE (Abcam, cat# ab91099), CG (Sigma-Aldrich, cat# C5108) and PR3 (Sigma-Aldrich, cat# SRP6309). MMP-12, -9 and -7 were added in an enzyme:protein ratio of 1:10 (weight/weight). NE was added in a ratio of 1:50. Lastly, CG and PR3 were added in a ratio of 1:15. The MMP buffer was used for the MMP cleavage and the NE buffer for the cleavage by NE, CG and PR3. Proteases in buffer without elastin were used as negative controls. Carboxymethylated-transferrin was used as a positive control, as it is a protein cleaved by these proteases. The reaction was stopped by adding EDTA to a final concentration of 1 µM and samples were stored at − 80 °C until analysis by ELISA.
Statistics
Serum levels of ELM12, ELM7, EL-NE, EL-CG and ELP-3 were assessed for normality by D’Agostino–Pearson omnibus test. Comparison of NSCLC and healthy control biomarker levels, histological subtype (AC vs. SCC) and age was done using unpaired, two-tailed Mann–Whitney test. Comparison of NSCLC stages was assessed by unpaired, non-parametric Kruskal–Wallis test adjusted for Dunn’s multiple comparisons. Diagnostic power of biomarkers was assessed by the area under the receiver operating characteristics (AUROC) curve. Sensitivity and specificity were determined for the estimated optimal cut-off value, as determined by the Youden Index. Comparison of gender was done using fisher’s exact test. A p value below 0.05 was considered significant. Asterisks indicate the following significance levels: *p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001. Statistical analysis and graphs were done in GraphPad Prism version 7 (GraphPad Software, Inc., La Jolla, CA, USA) and MedCalc (MedCalc Statistical Software version 16.8.4 (MedCalc Software bvba, Ostend, Belgium; https://www.medcalc.org; 2016).
Results
Validation of the ELM12 assay
Specificity of the ELM12 assay was assessed by the reactivity of the antibody towards the standard peptide (GVAPGIGPGG), elongated peptide (GVAPGIGPGGV), truncated peptide (GVAPGIGPG), non-sense peptide (LLARDFEKNY) and finally a non-sense coater peptide (Biotin-ADWGQSRDAEEAISQ) (Fig. 1). The standard peptide dose-dependently inhibited the signal, whereas the other peptides did not. No signal could be detected using the non-sense coater peptide. This all suggests that the assay is specific for the epitope of interest, ELM12.
Assay specificity. Inhibition curve for the standard peptide (GVAPGIGPGG), elongated (GVAPGIGPGGV), truncated (GVAPGIGPG), non-sense standard peptide (LLARDFEKNY) and a non-sense coater peptide (Biotin-ADWGQSRDAEEAISQ). Shown as percentage of background absorbance, which is assay buffer, as a function of peptide concentration on a linear scale. Error bars indicate standard deviation from duplicate measures
Technical performance of the ELM12 assay is summarized in Table 1. The measurement range (LLMR-ULMR) was determined to be 2.92–133 ng/ml. The intra- and inter-assay variation was 10 and 15%, respectively. Linearity was achieved from undiluted to fourfold dilution for both human serum and heparin plasma with a mean recovery of 100.9% for human serum and 99.6% for human heparin plasma (Fig. 2). Spiking recovery of cleaved elastin in healthy human serum resulted in a mean recovery of 94% in the linear range of the assay. Analyte stability was acceptable for up to 48 h at both 4 °C and 20 °C (mean recovery of 114% and 112%, respectively), as well as for multiple freeze–thaw cycles (mean recovery of 111%). Lastly, hemoglobin, lipids and biotin did not interfere with the ELM12 assay.
Assay linearity. Inhibition curve for the standard peptide and human serum samples, diluted twofold until samples measured below lower limit of measurement range (LLMR). Shown as percentage of background absorbance, which is assay buffer, as a function of peptide concentration on a log(10) scale. Error bars indicate standard deviation from duplicate measures
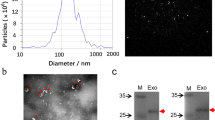
Degradation of elastin and generation of the ELM12 fragment
To investigate the different proteases ability to degrade elastin and generate the ELM12 epitope, MMP-7, -9 and -12 as well as NE, CG and PR3 were incubated with soluble elastin from human lung. Only MMP-9 and MMP-12 generated considerable amounts of the ELM12 neo-epitope (Fig. 3). MMP-12 generated more than double the amount of ELM12 compared to MMP-9 and no ELM12 generation was seen for MMP-7, NE, CG or PR3 demonstrating that ELM12 is generated by MMP-9 and -12.
Elastin cleavage. Soluble elastin from human lung was incubated 4 or 24 h with the specified protease. Cleavage by NE, CG, PR3 and MMP-7, -9 and -12 was analyzed by ELM12 ELISA, presented with mean and standard deviation. Data are based on two independent experiments with duplicate measures performed for each condition in each experiment. Error bars indicate standard deviation from the two experiments. Background reactivity of elastin and proteases in buffer were subtracted
Assessment of elastin degradation in serum from NSCLC patients and healthy controls
The five elastin degradation markers ELM12, ELM7, EL-NE, EL-CG and ELP-3 were assessed in a cohort of stage I-IV NSCLC patients and healthy controls. There was no significant difference in age or gender (Table 2). ELM12, ELM7, EL-NE and EL-CG were significantly elevated in NSCLC patients (Table 2; Fig. 4). There was no significant difference in ELP-3 levels. When evaluating differences in biomarker levels according to TNM tumor stage, and histological subtype (AC vs. SCC), no significant differences were detected expect for the EL-P3 levels in stage 1 vs. stage 4 (Fig. 5).
Assessment of elastin degradation markers in NSCLC vs. healthy controls. The levels of ELM12, ELM7, EL-NE, EL-CG and ELP-3 were measured in serum from NSCLC patients (n = 40) and healthy controls (n = 30) by ELISA, presented with mean and standard deviation. Samples measuring below LLMR were given the value of LLMR, as determined in the validation of each assay. Differences in biomarker levels were evaluated by Mann–Whitney test. ****Indicates a p value below 0.0001. *Indicates a p value below 0.05
Assessment of elastin degradation markers in NSCLC patients according to TNM stage (top) and histological subtype (bottom). The levels of ELM12, ELM7, EL-NE, EL-CG and ELP-3 are presented with mean and standard deviation. Samples measuring below LLMR were given the value of LLMR, as determined in the validation of each assay Comparison of histological subtype was evaluated by Mann–Whitney test. Comparison of NSCLC stages was evaluated by Kruskal–Wallis test adjusted for Dunn’s multiple comparisons.*Indicates a p value below 0.05. AC adenocarcinoma, SCC squamous cell carcinoma
ELM7, EL-CG and EL-NE correlated positively with each other, whereas ELM12 did not correlate with any of the other markers (Table 3). The AUROC indicated that ELM12 could discriminate between NSCLC and controls with an AUROC of 0.663 (p = 0.013) with a sensitivity of 67.5% and specificity of 60% using an estimated optimal cut-off value (Table 4). ELM7 had an AUROC of 0.779 (p < 0.0001) with a sensitivity of 85% and specificity of 63.3%. EL-NE had an AUROC of 0.770 (p < 0.0001) with a sensitivity of 75% and specificity of 76.7%. Lastly, EL-CG had an AUROC of 0.833 (p < 0.0001) with a sensitivity of 95% and specificity of 53.3%. These results indicate that the elastin degradation markers can distinguish between NSCLC patients and healthy controls and demonstrates their biomarker potential. Combining the ELM12 marker with either ELM7, EL-NE or EL-CG yielded minimal increases in AUROC, suggesting that these biomarkers do not supplement each other in NSCLC diagnosis (Table 4).
Discussion
In this study, we present the technical validation of an ELISA measuring elastin degradation by MMP-9 and -12. The assay was specific, only recognizing the intended neo-epitope, and was technically robust. Additionally, the biomarker potential of the ELM12 neo-epitope was demonstrated in the context of other elastin degradation markers in serum from NSCLC patients. Four elastin degradation markers were elevated in serum from NSCLC patients as compared to healthy controls: ELM12, generated by MMP-9 and -12; ELM7, generated by MMP-7; EL-NE, generated by NE; EL-CG, generated by CG. ELP-3, generated by proteinase 3 showed no significant difference between NSCLC patients and healthy controls.
As part of the matrix metalloprotease family, MMP-7, -9 and -12 are zinc-dependent endopeptidase that can cleave a diverse set of substrates and are implicated in a variety of cellular processes (Ra and Parks 2007). MMPs are well-established actors in the remodeling of the tumor microenvironment that promote tumor progression (Brown and Murray 2015). Previous studies reveal that MMP-12 is upregulated in NSCLC and correlates with metastatic potential and relapse of NSCLC tumors, as well as poor survival (Kettunen et al. 2004; Hofmann et al. 2005; Woenckhaus et al. 2006; Ella et al. 2018). Interestingly, MMP-12 is highly expressed by epithelial cells of the NSCLC tumors (Ella et al. 2018). In addition, tumor-derived rather than host-derived MMP-12 was shown to promote lung tumor growth in mice injected with lewis lung carcinoma (LLC) (Ella et al. 2018). Other studies have contrastingly demonstrated that MMP-12 is antitumorigenic: in mice injected with LLC cells, the presence of MMP-12 from tumor-associated macrophages (TAM) led to fewer lung metastases and an angiostatic tumor microenvironment (Houghton et al. 2006). These studies highlight the importance of MMP-12’s cellular origin and present a balance between pro- and anti-tumorigenic effects of MMP-12 activity. It is possible that the elevated MMP-12-derived elastin fragment, ELM12, detected in the serum from NSCLC patients originates from tumor epithelial cells and not host-derived macrophages. MMP-9 is also upregulated in NSCLC and levels are twofold higher in lung tumor tissue compared to healthy lung tissue (Hofmann et al. 2005). High MMP-9 levels have also been associated with lung cancer recurrence (Shah et al. 2010). In addition, high MMP-9 levels of both the tumor and surrounding stroma are associated with aggressive NSCLC, suggesting MMP-9 has prognostic value (Leinonen et al. 2006a; Gong et al. 2016). Our results support the finding that MMP-9 or -12 activity is elevated in NSCLC patients. In summary, the link between MMP-9 and -12 and lung cancer is well established and supports our current findings.
High MMP-7 expression is also observed in NSCLC patients (Leinonen et al. 2006b; Safranek et al. 2009). High MMP-7 expression is associated with dedifferentiated tumors and lymph node metastasis (Han et al. 2015; Sun et al. 2015). Additionally, MMP-7 is higher in AC as compared to SCC and is mostly tumor-derived, with minimal MMP-7 expression in the surrounding stroma (Leinonen et al. 2006b; Stenvold et al. 2012; Han et al. 2015). There are also ethnic differences in the effect of MMP-7 expression, as evidenced by the seemingly positive impact on survival in Caucasians and negative in Asians (Stenvold et al. 2012; Liang et al. 2014; Sun et al. 2015). In the current study, ELM7 was also elevated in serum from NSCLC patients as compared to healthy controls, exhibiting modest diagnostic capacity in this regard. A modest performance in diagnostics is not surprising considering most studies associate MMP-7 expression with NSCLC aggressiveness and metastasis. This marker could therefore be more useful in a prognostic setting. Indeed, we did see a trend towards higher ELM7 levels in later cancer stages, although not significant. Additionally, there was no significant difference between ELM7 levels in AC or SCC despite previous reports demonstrating this. Lastly, all patient samples in this cohort were Caucasian. Investigating ELM7 levels in an Asian cohort could yield an interesting comparison.
Altogether, these studies support the present findings of elevated elastin fragments generated by MMP-7, -9 and -12. It appears knowledge of the cellular origin of MMP activity is important to assert if activity is pro- or anti-tumorigenic, however that is not known in this study. Likewise, although MMP activity seems to have prognostic value, the lack of follow-up data in the current study prevents evaluation of this. Further investigation into the cellular origin of the MMP-derived elastin fragments and their potential prognostic value is warranted.
NE, CG and PR3 are serine proteases from the chymotrypsin family and are stored in the granules of polymorphonuclear neutrophils (Korkmaz et al. 2008). These cells are some of the first to reach a site of inflammation and the proteases they release are involved in remodeling of the ECM and diverse disease pathologies, including lung disease such as chronic obstructive pulmonary disorder (COPD) (Korkmaz et al. 2008; Bihlet et al. 2017). Inflammation in the lung microenvironment, characterized by neutrophil invasion, promotes metastasis to the lung from distant organs, in part accomplished by NE and CG proteolytic activity (El Rayes et al. 2015). With regard to the cellular origin of NE and CG, a previous study suggest that lung cancer cells do not express the proteases themselves, but that they are secreted to the tumor microenvironment by tumor-associated neutrophils (TAN) or TAMs (Peters et al. 2017). The activity of neutrophils and their release of proteases such as NE has been linked to tumor growth and invasiveness (Houghton 2010). These observations support our finding of elevated levels of CG- and NE-generated fragments in serum of NSCLC patients. In this study, EL-NE and EL-CG levels correlated, indicating that EL-NE and EL-CG generation stems from the same pathologic process.
PR3 is very similar to both NE and CG, both in terms structure and substrate specificities (Korkmaz et al. 2008). In the present study, EL-P3 was significantly elevated in stage 4 NSCLC compared to earlier stages, whereas EL-NE and EL-CG was not. This finding suggests that EL-P3 could have prognostic potential in NSCLC, warranting further investigations into the link between PR3 activity and metastatic potential. The cellular context of PR3 is important for PR3 function and differs from NE and CG. For example, although secreted PR3 is associated with tissue degradation, cytosolic PR3 is associated with apoptosis of both neutrophils and endothelial cells via procaspase-3 (Yang et al. 2001; Korkmaz et al. 2016). In addition, PR3 is found in a proteolytically inactive state on the surface of quiescent neutrophils and upon neutrophil activation, the amount of inactive PR3 increases (Korkmaz et al. 2016). This could mean that the proteolytic activity of PR3 decreases near neutrophils (Guarino et al. 2014). With that said, proteolytic activity of PR3 is known to cause tissue injury and emphysema in COPD and this may reveal another case where the two diseases differ (Guyot et al. 2014).
COPD patients have a high risk of developing lung cancer and the emphysema component of COPD, characterized by inflammation and destruction of ECM components such as elastin, has been linked to lung cancer risk. MMP-12, -9 and NE have all been linked to emphysema (Hautamaki et al. 1997; Atkinson et al. 2011; Houghton 2013; McGarry Houghton et al. 2015). Additionally, overexpression of MMP-12 in a murine model drove the transition of emphysema to lung cancer as facilitated by inflammation (Qu et al. 2009). However, previous investigations into the ELM12 neo-epitope revealed no elevated levels in either idiopathic pulmonary fibrosis (IPF) or COPD (Skjøt-Arkil et al. 2013). In the context of our results, this could indicate that ELM12 generation is more associated with lung cancer rather than being a result of general pulmonary disorders or tissue destruction. In comparison, the ELM7 and EL-NE neo-epitopes have been found elevated in serum from IPF patients, lung cancer patients and were heightened during acute exacerbations of COPD (Kristensen et al. 2015a, b; Sand et al. 2015). Given the correlation of EL-CG with ELM7 and EL-NE, the EL-CG neo-epitope may also be a generated in other lung disorders such as IPF and COPD.
Since ELM12 did not correlate with the other elastin degradation markers, it was investigated if the other markers could supplement ELM12 in terms of diagnostic power. Combination of the ELM12 biomarker with the other elastin fragments did improve the diagnostic power, however only minimally. Likewise, pairwise combinations of the other markers did not perform significantly better. Lastly, combining all four significant markers (ELM12, ELM7, EL-NE and EL-CG) did not perform significantly better than EL-CG alone, the best performing marker. Furthermore, there was no association with histological subtypes or cancer stages for any of the fragments. This suggest that the elastin markers investigated here, alone and in combination, may have limited diagnostic applicability, but may have more potential for phenotyping patients, and as mentioned above may have prognostic value.
The fact that bioactive elastin-derived peptides (EDPs) have been linked to tumor progression could support prognostic capacity of the measured markers. EDPs can drive tumor progression in several ways, for example by increasing secretion of proteases, facilitating migration or enabling metastasis by chemotactic activity (Scandolera et al. 2016). EDPs can also stimulate proliferation of cells in vitro, as seen in melanoma, astrocytoma and glioma cells (Jung et al. 1998; Hinek et al. 1999; Devy et al. 2010). In addition, they modulate invasiveness and migration of lung cancer cell lines (Blood et al. 1988; Toupance et al. 2012). EDPs are reportedly elevated in the serum of lung cancer patients as compared to healthy controls (Gminski et al. 1993). Indeed, some of the neo-epitope sequences investigated in the present study include known bioactive sequences. This presents the possibility that the fragments measured are not only biomarkers but have an active role in disease progression. The archetypal EDP is the VGVAPG hexapeptide, which holds the GxxPG motif, enabling recognition by the elastin receptor complex (ERC) (Ricard-Blum and Vallet 2016; Scandolera et al. 2016). The GxxPG motif is found throughout the tropoelastin sequence and repeated many times in the 24th exon, which can be considered one large matrikine. The cleavage site for the ELM12 neo-epitope is found near the end of the 24th exon, making it conceivable that cleavage at this site can leave bioactive sequences exposed and free to interact with the ERC. There are also GxxPG sequences near the EL-NE cleavage site, where a GFGPG sequence could also interact with the ERC.
This study has multiple limitations. Firstly, NSCLC patients in this study were exclusively Caucasian, so further investigation is needed to determine if extrapolation to populations of different ethnicities is possible. Secondly, although not significant, the difference in mean age between NSCLC patients and controls was considerable at 10 years. An increase in the elastin degradation markers during aging is conceivable, since the loss of elasticity and increased activity of elastases has already been linked to aging (Baud et al. 2013). In the case of ELM7 though, there does not seem to be an increase when comparing young and old rats (Karsdal et al. 2016). The link between the elastin degradation markers and age needs further investigation. Thirdly, clinical and pathological characteristics of patients were limited and with no follow-up data. Fourthly, the single small cohort utilized here limits the statistical power of the analysis, casting doubt on the diagnostic usefulness of the biomarkers, if any. Additionally, our findings should be validated in a second cohort.
In conclusion, the current study demonstrates that elastin degradation fragments generated by MMP-7, -9 and -12, as well as NE and CG were elevated in serum of NSCLC patients. The PR3-specific fragment showed no significant difference. The MMP-9 and -12 specific fragment, ELM12, did not correlate with either ELM7, EL-NE or EL-CG suggesting that generation of ELM12 is driven by different pathological mechanisms, although combinations of the biomarkers yielded limited diagnostic benefit. These preliminary findings demonstrate the biomarker potential of elastin degradation assays and future studies should investigate their clinical usefulness as phenotypic and/or prognostic markers in the lung cancer setting.
References
Atkinson JJ, Lutey BA, Suzuki Y et al (2011) The role of matrix metalloproteinase-9 in cigarette smoke-induced emphysema. Am J Respir Crit Care Med 183:876–884. https://doi.org/10.1164/rccm.201005-0718OC
Balkwill FR, Capasso M, Hagemann T (2012) The tumor microenvironment at a glance. J Cell Sci 125:5591–5596. https://doi.org/10.1242/jcs.116392
Baud S, Duca L, Bochicchio B et al (2013) Elastin peptides in aging and pathological conditions. Biomol Concepts 4:65–76. https://doi.org/10.1515/bmc-2011-0062
Bihlet AR, Karsdal MA, Sand JMB et al (2017) Biomarkers of extracellular matrix turnover are associated with emphysema and eosinophilic-bronchitis in COPD. Respir Res 18:22. https://doi.org/10.1186/s12931-017-0509-x
Blood CH, Sasse J, Brodt P, Zetter BR (1988) Identification of a tumor cell receptor for VGVAPG, an elastin-derived chemotactic peptide. J Cell Biol 107:1987–1993. https://doi.org/10.1083/jcb.107.5.1987
Brown GT, Murray GI (2015) Current mechanistic insights into the roles of matrix metalloproteinases in tumour invasion and metastasis. J Pathol 237:273–281. https://doi.org/10.1002/path.4586
Devy J, Duca L, Cantarelli B et al (2010) Elastin-derived peptides enhance melanoma growth in vivo by upregulating the activation of Mcol-A (MMP-1) collagenase. Br J Cancer 103:1562–1570. https://doi.org/10.1038/sj.bjc.6605926
El Rayes T, Catena R, Lee S et al (2015) Lung inflammation promotes metastasis through neutrophil protease-mediated degradation of Tsp-1. Proc Natl Acad Sci USA 112:16000–16005. https://doi.org/10.1073/pnas.1507294112
Ella E, Harel Y, Abraham M et al (2018) Matrix metalloproteinase 12 promotes tumor propagation in the lung. J Thorac Cardiovasc Surg 155:2164–2175.e1. https://doi.org/10.1016/j.jtcvs.2017.11.110
Gminski J, Mykala-Ciesla J, Machalski M, Drozdz M (1993) Elastin metabolism parameters in sera of patients with lung cancer. Neoplasma 40:41–44
Gong L, Wu D, Zou J et al (2016) Prognostic impact of serum and tissue MMP-9 in non-small cell lung cancer: a systematic review and meta-analysis. Oncotarget 7:18458–18468. https://doi.org/10.18632/oncotarget.7607
Guarino C, Legowska M, Epinette C et al (2014) New selective peptidyl di(chlorophenyl) phosphonate esters for visualizing and blocking neutrophil proteinase 3 in human diseases. J Biol Chem 289:31777–31791. https://doi.org/10.1074/jbc.M114.591339
Gudmann NS, Manon-Jensen T, Sand JMB et al (2018) Lung tissue destruction by proteinase 3 and cathepsin G mediated elastin degradation is elevated in chronic obstructive pulmonary disease. Biochem Biophys Res Commun. https://doi.org/10.1016/j.bbrc.2018.07.038
Guyot N, Wartelle J, Malleret L et al (2014) Unopposed cathepsin G, neutrophil elastase, and proteinase 3 cause severe lung damage and emphysema. Am J Pathol 184:2197–2210. https://doi.org/10.1016/j.ajpath.2014.04.015
Halaoui R, McCaffrey L (2015) Rewiring cell polarity signaling in cancer. Oncogene 34:939–950. https://doi.org/10.1038/onc.2014.59
Han J-C, Li X-D, Du J et al (2015) Elevated matrix metalloproteinase-7 expression promotes metastasis in human lung carcinoma. World J Surg Oncol 13:5. https://doi.org/10.1186/1477-7819-13-5
Hautamaki RD, Kobayashi DK, Senior RM, Shapiro SD (1997) Requirement for macrophage elastase for cigarette smoke-induced emphysema in mice. Science 277:2002–2004
Heinz A, Jung MC, Duca L et al (2010) Degradation of tropoelastin by matrix metalloproteinases—cleavage site specificities and release of matrikines. FEBS J 277:1939–1956. https://doi.org/10.1111/j.1742-4658.2010.07616.x
Heinz A, Taddese S, Sippl W et al (2011) Insights into the degradation of human elastin by matrilysin-1. Biochimie 93:187–194. https://doi.org/10.1016/j.biochi.2010.09.011
Heinz A, Jung MC, Jahreis G et al (2012) The action of neutrophil serine proteases on elastin and its precursor. Biochimie 94:192–202. https://doi.org/10.1016/j.biochi.2011.10.006
Hinek A, Jung S, Rutka JT (1999) Cell surface aggregation of elastin receptor molecules caused by suramin amplified signals leading to proliferation of human glioma cells. Acta Neuropathol 97:399–407
Hofmann H-S, Hansen G, Richter G et al (2005) Matrix metalloproteinase-12 expression correlates with local recurrence and metastatic disease in non-small cell lung cancer patients. Clin Cancer Res 11:1086–1092
Houghton AM (2010) The paradox of tumor-associated neutrophils: fueling tumor growth with cytotoxic substances. Cell Cycle 9:1732–1737. https://doi.org/10.4161/cc.9.9.11297
Houghton AM (2013) Mechanistic links between COPD and lung cancer. Nat Rev Cancer 13:233–245. https://doi.org/10.1038/nrc3477
Houghton AM, Grisolano JL, Baumann ML et al (2006) Macrophage elastase (Matrix Metalloproteinase-12) suppresses growth of lung metastases. Cancer Res 66:6149–6155. https://doi.org/10.1158/0008-5472.CAN-04-0297
Jung S, Rutka JT, Hinek A (1998) Tropoelastin and elastin degradation products promote proliferation of human astrocytoma cell lines. J Neuropathol Exp Neurol 57:439–448. https://doi.org/10.1097/00005072-199805000-00007
Karsdal MA, Genovese F, Madsen EA et al (2016) Collagen and tissue turnover as a function of age: implications for fibrosis. J Heptol 64:103–109. https://doi.org/10.1016/j.jhep.2015.08.014
Kettunen E, Anttila S, Seppänen JK et al (2004) Differentially expressed genes in nonsmall cell lung cancer: expression profiling of cancer-related genes in squamous cell lung cancer. Cancer Genet Cytogenet 149:98–106. https://doi.org/10.1016/S0165-4608(03)00300-5
Korkmaz B, Moreau T, Gauthier F (2008) Neutrophil elastase, proteinase 3 and cathepsin G: physicochemical properties, activity and physiopathological functions. Biochimie 90:227–242. https://doi.org/10.1016/j.biochi.2007.10.009
Korkmaz B, Lesner A, Guarino C et al (2016) Inhibitors and antibody fragments as potential anti-inflammatory therapeutics targeting neutrophil proteinase 3 in human disease. Pharmacol Rev 68:603–630. https://doi.org/10.1124/pr.115.012104
Kristensen JH, Karsdal MA, Sand JM et al (2015a) Serological assessment of neutrophil elastase activity on elastin during lung ECM remodeling. BMC Pulm Med 15:53. https://doi.org/10.1186/s12890-015-0048-5
Kristensen JH, Larsen L, Dasgupta B et al (2015b) Levels of circulating MMP-7 degraded elastin are elevated in pulmonary disorders. Clin Biochem 48:1083–1088. https://doi.org/10.1016/j.clinbiochem.2015.07.009
Landskron G, De la Fuente M, Thuwajit P et al (2014) Chronic inflammation and cytokines in the tumor microenvironment. J Immunol Res 2014:149185. https://doi.org/10.1155/2014/149185
Leinonen T, Pirinen R, Böhm J et al (2006a) Expression of matrix metalloproteinases 7 and 9 in non-small cell lung cancer. Lung Cancer 51:313–321. https://doi.org/10.1016/j.lungcan.2005.11.002
Leinonen T, Pirinen R, Böhm J et al (2006b) Expression of matrix metalloproteinases 7 and 9 in non-small cell lung cancer. Relation to clinicopathological factors, beta-catenin and prognosis. Lung Cancer 51:313–321. https://doi.org/10.1016/j.lungcan.2005.11.002
Liang Y, Guo S, Zhou Q (2014) Prognostic value of matrix metalloproteinase-7 expression in patients with non-small cell lung cancer. Tumour Biol 35:3717–3724. https://doi.org/10.1007/s13277-013-1491-7
McGarry Houghton A, Houghton AM, McGarry Houghton A (2015) Matrix metalloproteinases in destructive lung disease. Matrix Biol 44–46:167–174. https://doi.org/10.1016/j.matbio.2015.02.002
Mithieux SM, Weiss AS (2005) Elastin. In: Advances in protein chemistry. Academic Press, Cambridge, pp 437–461
Noël A, Gutiérrez-Fernández A, Sounni NE et al (2012) New and paradoxical roles of matrix metalloproteinases in the tumor microenvironment. Front Pharmacol 3:140. https://doi.org/10.3389/fphar.2012.00140
Peters HL, Tripathi SC, Kerros C et al (2017) Serine proteases enhance immunogenic antigen presentation on lung cancer cells. Cancer Immunol Res 5:319–329. https://doi.org/10.1158/2326-6066.CIR-16-0141
Qu P, Du H, Wang X, Yan C (2009) Matrix metalloproteinase 12 overexpression in lung epithelial cells plays a key role in emphysema to lung bronchioalveolar adenocarcinoma transition. Cancer Res 69:7252–7261. https://doi.org/10.1158/0008-5472.CAN-09-0577
Ra H-J, Parks WC (2007) Control of matrix metalloproteinase catalytic activity. Matrix Biol 26:587–596. https://doi.org/10.1016/j.matbio.2007.07.001
Ricard-Blum S, Vallet SD (2016) Matricryptins network with matricellular receptors at the surface of endothelial and tumor cells. Front Pharmacol 7:11. https://doi.org/10.3389/fphar.2016.00011
Safranek J, Pesta M, Holubec L et al (2009) Expression of MMP-7, MMP-9, TIMP-1 and TIMP-2 mRNA in lung tissue of patients with non-small cell lung cancer (NSCLC) and benign pulmonary disease. Anticancer Res 29:2513–2517
Sand JMB, Knox AJ, Lange P et al (2015) Accelerated extracellular matrix turnover during exacerbations of COPD. Respir Res 16:69. https://doi.org/10.1186/s12931-015-0225-3
Scandolera A, Odoul L, Salesse S et al (2016) The elastin receptor complex: a unique matricellular receptor with high anti-tumoral potential. Front Pharmacol 7:1–10. https://doi.org/10.3389/fphar.2016.00032
Shah SA, Spinale FG, Ikonomidis JS et al (2010) Differential matrix metalloproteinase levels in adenocarcinoma and squamous cell carcinoma of the lung. J Thorac Cardiovasc Surg 139:984–990. https://doi.org/10.1016/j.jtcvs.2009.12.016
Siegel RL, Miller KD, Jemal A (2018) Cancer statistics, 2018. CA Cancer J Clin 68:7–30. https://doi.org/10.3322/caac.21442
Skjøt-Arkil H, Clausen RE, Rasmussen LM et al (2013) Acute myocardial infarction and pulmonary diseases result in two different degradation profiles of elastin as quantified by two novel ELISAs. PLoS One. https://doi.org/10.1371/journal.pone.0060936
Starcher B, Sauter E, Ho C (2013) Elastin turnover in malignant solid tumors. Connect Tissue Res 54:313–318. https://doi.org/10.3109/03008207.2013.820723
Stenvold H, Donnem T, Andersen S et al (2012) Overexpression of matrix metalloproteinase-7 and -9 in NSCLC tumor and stromal cells: correlation with a favorable clinical outcome. Lung Cancer 75:235–241. https://doi.org/10.1016/j.lungcan.2011.06.010
Sun Y, Li D, Lv X-H et al (2015) Roles of osteopontin and matrix metalloproteinase-7 in occurrence, progression, and prognosis of nonsmall cell lung cancer. J Res Med Sci 20:1138–1146. https://doi.org/10.4103/1735-1995.172980
Taddese S, Weiss AS, Neubert RHH, Schmelzer CEH (2008) Mapping of macrophage elastase cleavage sites in insoluble human skin elastin. Matrix Biol 27:420–428. https://doi.org/10.1016/j.matbio.2008.02.001
Toupance S, Brassart B, Rabenoelina F et al (2012) Elastin-derived peptides increase invasive capacities of lung cancer cells by post-transcriptional regulation of MMP-2 and uPA. Clin Exp Metastasis 29:511–522. https://doi.org/10.1007/s10585-012-9467-3
Wise SG, Weiss AS (2009) Tropoelastin. Int J Biochem Cell Biol 41:494–497. https://doi.org/10.1016/j.biocel.2008.03.017
Woenckhaus M, Klein-Hitpass L, Grepmeier U et al (2006) Smoking and cancer-related gene expression in bronchial epithelium and non-small-cell lung cancers. J Pathol 210:192–204. https://doi.org/10.1002/path.2039
Yang JJ, Preston GA, Pendergraft WF et al (2001) Internalization of proteinase 3 is concomitant with endothelial cell apoptosis and internalization of myeloperoxidase with generation of intracellular oxidants. Am J Pathol 158:581–592. https://doi.org/10.1016/S0002-9440(10)64000-X
Zamay T, Zamay G, Kolovskaya O et al (2017) Current and prospective protein biomarkers of lung cancer. Cancers (Basel) 9:155. https://doi.org/10.3390/cancers9110155
Acknowledgements
We acknowledge the Danish Research Foundation for supporting this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors are employed at Nordic Bioscience involved in biomarker discovery and assay development.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Thorlacius-Ussing, J., Kehlet, S.N., Rønnow, S.R. et al. Non-invasive profiling of protease-specific elastin turnover in lung cancer: biomarker potential. J Cancer Res Clin Oncol 145, 383–392 (2019). https://doi.org/10.1007/s00432-018-2799-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-018-2799-x