Abstract
Purpose
We retrospectively examined the efficacy and safety of S-1 alone or S-1 plus cisplatin (SP) for elderly patients with advanced gastric cancer because the benefit of adding cisplatin in these patients still remains unclear.
Patients and methods
Among 175 patients aged 70 years or older who received S-1 alone or SP as a first-line therapy between April 2000 and November 2010 at our institution, 104 patients who met eligibility criteria were examined. We investigated safety and efficacy of S-1 and SP.
Results
Among these 104 patients, 73 patients received S-1 and 31 patients received SP. The median age was 75 years in the S-1 group and 74 years in the SP group. The response rate was 26.3 % in the S-1 group and 44.0 % in the SP group. Major grade 3 or higher adverse events were observed as follows (S-1 vs. SP): nausea (1.4 vs. 16.1 %), anorexia (16.4 vs. 41.9 %), neutropenia (4.1 vs. 35.5 %), and febrile neutropenia (0 vs. 9.7 %). The median overall survival (OS) was 10.4 months in the S-1 group and 17.8 months in the SP group. Treatment of SP and histology of intestinal type were detected as independent, good prognostic factors in multivariate analysis.
Conclusion
SP might improve OS with some added toxicity compared to S-1 alone in elderly patients with advanced gastric cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer is the fourth most frequent malignant disease and the second most common cause of cancer-related deaths in the world (Parkin et al. 2005). In Japan, gastric cancer has caused the second most frequent cancer-related deaths, behind lung cancer, since 1999. A total of 23 % of the Japanese population were aged 65 years or older in 2010, and 39.9 % of the population will be 65 years or older by 2060. In the last decades, despite the overall decrease in the rate of gastric cancer, the proportion of elderly among gastric cancer patients is increasing (Kitamura et al. 1996). The elderly comprise the most rapidly growing segment of the population that requires chemotherapy for the treatment of cancer.
The development of systemic chemotherapy has improved the survival and quality of life in patients with gastric cancer compared with best supportive care alone (Murad et al. 1993; Pyrhonen et al. 1995; Glimelius et al. 1997). In Japan, the JCOG9912 trial showed S-1 to be non-inferior to continuous infusion of fluorouracil (Boku et al. 2009), and the SPIRITS trial showed a survival benefit of S-1 plus cisplatin (SP) over S-1 alone (Koizumi et al. 2008). From the results of these phase III trials, SP was recognized as a standard treatment for advanced gastric cancer. A subset analysis of the SPIRITS trial reported that the hazards ratio (HR) for overall survival (OS) among patients aged 70 years or older was 0.95 (95 % CI 0.71–1.27), but this age group comprised only 17 % of all the patients. To date, although several phase II trials and retrospective studies on elderly patients have been reported, the most appropriate standard chemotherapy for elderly patients remains unclear (Lee et al. 2008; Koizumi et al. 2010; Xiang et al. 2012; Fonck et al. 2011; Seol et al. 2009; Tsushima et al. 2013).
Therefore, we retrospectively examined the efficacy and safety of S-1 alone or SP for elderly patients with advanced gastric cancer.
Patients and method
Patients
Patients over 70-year old with advanced gastric cancer who received S-1 or SP as a first-line therapy between April 2000 and November 2010 at our institution were enrolled. The eligibility criteria were as follows: Eastern Cooperative Oncology Group (ECOG) performance status of 0–2; adequate organ function with the following laboratory data: 20,000/mm3 > leukocyte count > 4,000/mm3, platelet count > 100,000/mm3, hemoglobin >8.0 g/dL, aspartate aminotransferase (AST) and alanine aminotransferase (ALT) <100 U/L, total bilirubin <1.5 mg/dL, serum creatinine < the upper limit of normal (ULN) and creatinine clearance (Ccr) >50 mL/min, and alkaline phosphatase (ALP) <ULN × 2.
Toxicity and response criteria
We obtained all the clinical data retrospectively from the medical records. Adverse events were evaluated according to the National Cancer Institute Common Terminology Criteria for Adverse Events, version 4.0. The tumor response was evaluated according to Response Evaluation Criteria in Solid Tumours (RECIST) version 1.0 (Therasse et al. 2000).
Treatment dose and schedule
Patients received S-1 or SP according to the investigators’ choice. The patients receiving SP were administered S-1 orally twice daily for the first 3 weeks of a 5-week cycle, and cisplatin on day 8 of each cycle. The patients receiving S-1 alone were administered S-1 orally twice daily for the first 4 weeks of a 6-week cycle. In each group, the dose of S-1 was generally decided according to the patient’s body surface area as follows: less than 1.25 m2, 40 mg; 1.25–1.5 m2, 50 mg; and greater than 1.5 m2, 60 mg. Cisplatin was given as an intravenous infusion of 60 mg/m2. The dose of chemotherapy was allowed to be reduced according to the physician’s judgment after the first cycle. Treatment for both groups was continued until progressive disease, unacceptable toxicity, withdrawal of consent by the patient, or termination of the treatment by the treating physician.
Statistical analysis
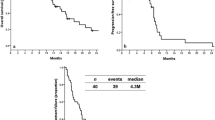
OS was defined as the time from the date of the first administration of S-1 to the date of death from any cause. Progression-free survival (PFS) was defined as the time from the date of the first administration of S-1 to the date of progressive disease or death from any cause. Survival curves were estimated using the Kaplan–Meier method.
OS was compared between S-1 and SP with baseline prognostic factors adjusted, using Cox proportional hazards model. Baseline prognostic factors, used as adjusting factors, were as follows: age (<75 vs. ≥75 years), sex (male vs. female), performance status (0 vs. 1–2), alkaline phosphatase (ALP) (≤359 vs. >359 U/L), disease status (recurrence vs. stage IV), histological type (intestinal type vs. diffuse type), and the number of metastatic sites (1 vs. ≥2). Statistical analysis was performed using SPSS software (SPSS, Inc, Chicago, IL). A p value <0.05 was considered to be statistically significant.
Results
Patient characteristics
A total of 175 patients over 70-year old received S-1 or SP. Among them, 104 patients who met the eligibility criteria of the SPIRITS trial were evaluated (Fig. 1). A total of 73 patients received S-1, and 31 patients received SP. Patient characteristics are shown in Table 1. The median age was 76 years (range 70–84 years) in the S-1 group and 74 years (range 70–78 years) in the SP group. In the S-1 group, 14 patients were over 80-year old, but none in the SP group (p = 0.007) was that old. More patients in the S-1 group than in the SP group had ECOG performance status of 1 or 2 (64.4 vs. 35.5 %, p = 0.07).
Treatment and dose of drugs
The median number of treatment cycles was 3 (1–22) in S-1 and 2 (1–9) in SP. In both groups, 25 % of patients had a dose reduction after the first cycle due to low creatinine clearance or older age. The main reason for treatment failure was disease progression in both groups (n = 44, 60.3 % and n = 13, 41.9 % in S-1 and SP, respectively), and the second most frequent reason was adverse events (n = 11, 15.1 % and n = 11, 35.1 % in S-1 and SP, respectively). The details of the adverse events that caused treatment failure were as follows: anorexia (n = 4), diarrhea (n = 1), rash (n = 2), stomatitis (n = 2), abdominal pain (n = 1), and pneumonia (n = 1) in the S-1 group and renal dysfunction (n = 2), anorexia (n = 5), diarrhea (n = 1), rash (n = 1), and neuropathy (n = 2) in the SP group.
Adverse events
Table 2 shows adverse events. The SP group had a higher incidence of grade 3 or 4 hematological toxicity than did the S-1 group. Severe anorexia and anemia occurred often in the SP group (anorexia, S-1 16.4 %/SP 41.9 %; and nausea, S-1 1.4 %/SP 16.1 %). There was no treatment-related death in either group.
Response and survival
A total of 57 patients in the S-1 group and 25 patients in the SP group had measurable lesions. The response rate was 26 % in the S-1 group (95 % CI 15–40 %) and 44 % in the SP group (95 % CI 24–65 %; Table 3). The median follow-up period was 10.4 months (95 % CI 8.5–12.3 months) in the S-1 group and 19.6 months (95 % CI 16.8–22.5 months) in the SP group. The median OS tended to be longer in the SP group than in the S-1 group (10.4 months [95 % CI 8.4–12.4 months] in the S-1 group vs. 17.8 months [95 % CI 15.0–20.6 months] in the SP group; Fig. 2). The median PFS was 5.6 months [95 % CI 4.6–6.7 months] in the S-1 group and 7.7 months [95 % CI 4.2–11.1 months] in the SP group (Fig. 3). Subsequent chemotherapy was given to 39 patients (53.4 %) in the S-1 group: paclitaxel (n = 20), irinotecan plus cisplatin (n = 10), methotrexate plus fluorouracil (n = 3), fluorouracil (n = 3), and other (n = 3), and to 17 patients (54.8 %) in the SP group: S-1 (n = 8), paclitaxel (n = 4), irinotecan (n = 3), and others (n = 2). Two patients in the SP group who had only para-aortic lymph node metastasis received curative surgery.
Clinical factors predicting OS were analyzed (Table 4). All clinical parameters were included in a multivariate analysis. Treatment and histology were detected as an independent prognostic factor.
Discussion
This retrospective study showed that SP may provide increased efficacy compared to S-1 alone in advanced gastric cancer patients aged 70 years or older. The median OS was 10.4 months for the S-1 group and 17.8 months for the SP group.
Several phase II studies and retrospective studies on elderly gastric cancer patients have been reported. Among these studies, oral fluoropyrimidine alone provided a median PFS of 3.9–5.2 months and a median OS of 8.1–15.7 months (Lee et al. 2008; Koizumi et al. 2010; Tsushima et al. 2013). Combination therapy with fluoropyrimidine and platinum provided a median PFS of 5.0–7.0 months, with a median OS of 9.6–14.4 months (Xiang et al. 2012; Fonck et al. 2011; Seol et al. 2009; Tsushima et al. 2013). Combination chemotherapy with fluoropyrimidine and platinum may provide better benefit compared to fluoropyrimidine alone for both elderly and young patients.
More patients in the SP than in the S-1 group had grade 3 or higher hematological and gastrointestinal adverse events. In our study, elderly patients in both the S-1 and SP groups developed more frequently hematological and gastrointestinal adverse events than did patients aged 20–74 years in the SPIRITS trial. The percentage of patients withdrawn from SP due to adverse events was slightly higher in the present study than it was in the SPIRITS trial (35 % in our study and 28 % in the SPIRITS trial; Koizumi et al. 2008). Elderly cancer patients generally have reduced renal function (Launay-Vacher et al. 2007). It has been reported that patients with low creatinine clearance had serious adverse events because S-1 is a renally excreted drug, and cisplatin is a well-known nephrotoxic drug (Chen et al. 2011; Nagashima et al. 2005).
According to the results of a multivariate analysis of OS, histology was also detected as an independent prognostic factor. The diffuse type is generally considered to be an unfavorable factor related to shorter survival in advanced gastric cancer. In the subset analysis of the JCOG 9912 trial, the patients with diffuse type who received S-1 or cisplatin plus irinotecan had shorter survival than did those with the intestinal type (Boku et al. 2009). However, in subgroup analyses of the SPIRITS trial, both S-1 and SP were effective without regard to histological type. This study was retrospective, so patient characteristics were not well balanced between the two groups. In this study, 44 patients had intestinal type (33/11; S-1/SP) and 59 patients had diffuse type (39/20; S-1/SP) of advanced gastric cancer. This study also demonstrated the significance of histology as an independent poor prognostic factor in elderly patients.
This study had some limitations. First, the number of patients who received SP was too small to compare with those in the S-1 group. The result of the SPIRITS trial was reported at the 2007 Annual Meeting of the American Society of Clinical Oncology, whereas our study was conducted during a period (from 2000 to 2010) where SP had not been established as a standard first-line therapy. Second, the patients’ ages were different in the two groups. SP was not selected for patients aged 80 years or older (p = 0.007). Finally, patients with performance status of 1 or 2 tended to be selected to S-1 alone more frequently than to SP because physicians judged that SP was too toxic for patients with poor performance status.
The individual’s level of functioning is an important factor to consider when weighing the risks and benefits of a treatment for elderly patients with cancer. In our institution, patients who had good performance status were selected. However, the important parameters for elderly cancer patients are not only performance status but also complications, cognitive function, and physical condition. Recently, geriatricians performed a comprehensive geriatric assessment (CGA) that measured independent clinical predictors of morbidity and mortality in older adults with cancer (Hurria et al. 2005, 2011; Extermann and Hurria 2007). It is expected that CGA typically will be used in daily oncology practice to assist in decision-making. Hence, assessment of CGA in a clinical trial is expected to result in the administration of standard chemotherapy to elderly and eligible patients with cancer.
In conclusion, SP tended to improve PFS and OS in elderly patients compared to S-1 alone, although the toxic effects of SP were more serious than those of S-1 alone. We think that SP treatment should be limited to elderly patients who have performance status of 0 or 1 because there are few data about the safety of SP treatment for elderly patients with performance status of 2. A feasible regimen that would not decrease the efficacy was needed for elderly patients. A multicenter phase II study that validates a modified SP treatment based on creatinine clearance is ongoing.
References
Boku N, Yamamoto S, Fukuda H, Shirao K, Doi T, Sawaki A, Koizumi W, Saito H, Yamaguchi K, Takiuchi H, Nasu J, Ohtsu A, Gastrointestinal Oncology Study Group of the Japan Clinical Oncology Group (2009) Fluorouracil versus combination of irinotecan plus cisplatin versus S-1 in metastatic gastric cancer: a randomised phase 3 study. Lancet Oncol 10:1063–1069
Chen JS, Chao Y, Hsieh RK, Cheng AL, Chen PM, Chiou TJ, Chao TY, Yeh KH, Chen LT, Whang-Peng J (2011) A phase II and pharmacokinetic study of first line S-1 for advanced gastric cancer in Taiwan. Cancer Chemother Pharmacol 67:1281–1289
Extermann M, Hurria A (2007) Comprehensive geriatric assessment for older patients with cancer. J Clin Oncol 25:1824–1831
Fonck M, Brunet R, Becouarn Y, Legoux JL, Dauba J, Cany L, Smith D, Auby D, Terrebonne E, Traissac L, Mertens C, Soubeyran P, Bellera C, Rainfray M, Mathoulin-Pélissier S (2011) Evaluation of efficacy and safety of FOLFIRI for elderly patients with gastric cancer: a first-line phase II study. Clin Res Hepatol Gastroenterol 35:823–830
Glimelius B, Ekström K, Hoffman K, Graf W, Sjödén PO, Haglund U, Svensson C, Enander LK, Linné T, Sellström H, Heuman R (1997) Randomized comparison between chemotherapy plus best supportive care with best supportive care in advanced gastric cancer. Ann Oncol 8:163–168
Hurria A, Gupta S, Zauderer M, Zuckerman EL, Cohen HJ, Muss H, Rodin M, Panageas KS, Holland JC, Saltz L, Kris MG, Noy A, Gomez J, Jakubowski A, Hudis C, Kornblith AB (2005) Developing a cancer-specific geriatric assessment: a feasibility study. Cancer 104:1998–2005
Hurria A, Togawa K, Mohile SG, Owusu C, Klepin HD, Gross CP, Lichtman SM, Gajra A, Bhatia S, Katheria V, Klapper S, Hansen K, Ramani R, Lachs M, Wong FL, Tew WP (2011) Predicting chemotherapy toxicity in older adults with cancer: a prospective multicenter study. J Clin Oncol 29:3457–3465
Kitamura K, Yamaguchi T, Taniguchi H, Hagiwara A, Yamane T, Sawai K, Takahashi T (1996) Clinicopathological characteristics of gastric cancer in the elderly. Br J Cancer 73:798–802
Koizumi W, Narahara H, Hara T, Takagane A, Akiya T, Takagi M, Miyashita K, Nishizaki T, Kobayashi O, Takiyama W, Toh Y, Nagaie T, Takagi S, Yamamura Y, Yanaoka K, Orita H, Takeuchi M (2008) S-1 plus cisplatin versus S-1 alone for first-line treatment of advanced gastric cancer (SPIRITS trial): a phase III trial. Lancet Oncol 9:215–221
Koizumi W, Akiya T, Sato A, Sakuyama T, Sasaki E, Tomidokoro T, Hamada T, Fujimori M, Kikuchi Y, Shimada K, Mine T, Yamaguchi K, Sasaki T, Kurihara M (2010) Phase II study of S-1 as first-line treatment for elderly patients over 75 years of age with advanced gastric cancer: the Tokyo Cooperative Oncology Group study. Cancer Chemother Pharmacol 65:1093–1099
Launay-Vacher V, Chatelut E, Lichtman SM, Wildiers H, Steer C, Aapro M, International Society of Geriatric Oncology (2007) Renal insufficiency in elderly cancer patients: International Society of Geriatric Oncology clinical practice recommendations. Ann Oncol 18:1314–1321
Lee JL, Kang YK, Kang HJ, Lee KH, Zang DY, Ryoo BY, Kim JG, Park SR, Kang WK, Shin DB, Ryu MH, Chang HM, Kim TW, Baek JH, Min YJ (2008) A randomised multicentre phase II trial of capecitabine vs S-1 as first-line treatment in elderly patients with metastatic or recurrent unresectable gastric cancer. Br J Cancer 99:584–590
Murad AM, Santiago FF, Petroianu A, Rocha PR, Rodrigues MA, Rausch M (1993) Modified therapy with 5-fluorouracil, doxorubicin, and methotrexate in advanced gastric cancer. Cancer 72:37–41
Nagashima F, Ohtsu A, Yoshida S, Ito K (2005) Japanese nationwide post-marketing survey of S-1 in patients with advanced gastric cancer. Gastric Cancer 8:6–11
Parkin DM, Bray F, Ferlay J, Pisani P (2005) Global cancer statistics, 2002. CA Cancer J Clin 55:74–108
Pyrhonen S, Kuitunen T, Nyandoto P, Kouri M (1995) Randomised comparison of fluorouracil, epidoxorubicin and methotrexate (FEMTX) plus supportive care with supportive care alone in patients with nonresectable gastric cancer. Br J Cancer 71:587–591
Seol YM, Song MK, Choi YJ, Kim GH, Shin HJ, Song GA, Chung JS, Cho GJ (2009) Oral fluoropyrimidines (Capecitabine or S-1) and cisplatin as first line treatment in elderly patients with advanced gastric cancer: a retrospective study. Jpn J Clin Oncol 39:43–48
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92:205–216
Tsushima T, Hironaka S, Boku N, Machida N, Yamazaki K, Yasui H, Fukutomi A, Todaka A, Taniguchi H, Onozawa Y, Taku K (2013) Comparison of safety and efficacy of S-1 monotherapy and S-1 plus cisplatin therapy in elderly patients with advanced gastric cancer. Int J Clin Oncol 18:10–16
Xiang XJ, Zhang L, Qiu F, Yu F, Zhan ZY, Feng M, Yan J, Zhao JG, Xiong JP (2012) A phase II study of capecitabine plus oxaliplatin as first-line chemotherapy in elderly patients with advanced gastric cancer. Chemotherapy 58:1–7
Conflict of interest
The authors indicated no potential conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Terazawa, T., Iwasa, S., Takashima, A. et al. Impact of adding cisplatin to S-1 in elderly patients with advanced gastric cancer. J Cancer Res Clin Oncol 139, 2111–2116 (2013). https://doi.org/10.1007/s00432-013-1537-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-013-1537-7