Abstract
Purpose
To evaluate the efficacy, safety and pharmacokinetic profiles of S-1, which composed of tegafur (FT, a prodrug of 5-FU), 5-chloro-2,4-dihydroxypyridine and potassium oxonate (Oxo), in Taiwanese advanced gastric cancer (AGC) patients.
Methods
Patients with chemo-naïve, histologically confirmed AGC were eligible. S-1 was given orally at dose of 40, 50 or 60 mg, twice daily for patients with body surface <1.25, 1.25–1.5 and >1.5 m2, respectively, on day 1–28 every 42 days/cycle.
Results
Thirty-four patients were included. On intent-to-treat analysis, the overall response rate, median progression-free and overall survival were 35.3% [95% confidence interval (CI): 19.2–51.3%], 2.9 (95% CI: 2.4–5.8) months and 9.8 (95% CI: 6.1–NA) months, respectively. The most common grade 3–4 toxicities were anemia 23.5% and neutropenia 11.8%. There were two treatment-related mortality, which occurred in patients with suboptimal renal function underestimated by serum creatinine level at study entry. Single-dose pharmacokinetic study showed trend toward lower AUC5–FU, and higher AUCFT and AUCOxo comparing to most Western reports.
Conclusions
The efficacy, toxicity and pharmacokinetic profiles of S-1 in current study are compatible with those from other Asian populations. Accurate renal function assessment and more closely monitoring is mandatory for S-1 therapy in patients with low body mass. Literature review suggests that, besides AUC5–FU, AUCOxo may also attribute to the difference in the compliance to S-1 between Asian and Caucasian populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer is the fourth most common cancer, with an estimated more than one million new cases diagnosed in 2007, and the second most common cause of cancer death (more than 800,000 deaths annually) worldwide [1]. In Taiwan, gastric cancer ranks the fifth of all cancer-related mortality and is responsible for approximately 2,400 deaths per year in 2006 [2]. One-third or more of patients presented with unresectable locally advanced or metastatic diseases at time of diagnosis, while many patients who were able to receive curative surgical resection would eventually relapse [3]. Thus, majority of gastric cancer patients require palliative treatment at certain time-points. 5-fluorouracil (5-FU) is one of the most active and least toxic chemotherapeutic agents for advanced gastric cancer (AGC). Protracted intravenous infusion at dose of 200–300 mg/m2/day or 5-days infusion at dose of 800–1,000 mg/m2/day every 3 weeks, or 24–48 h infusion of 2,400–3,000 mg/m2 every 1–2 weeks are the favorable schedules for 5-FU administration. These infusional 5-FU regimens, with and without folinic acid modulation, can achieve up to 15–30% of objective response and are commonly used as the backbone of current “standard” combination regimens in AGC [4, 5]. Several randomized trials have demonstrated that infusion 5-FU—based chemotherapy could significantly improve the quality of life and overall survival of AGC patients comparing to best supportive care [4].
S-1 is a third generation of oral fluoropyrimidine composed of tegafur (FT, a prodrug of 5-FU), 5-chloro-2,4-dihydroxypyridine (CDHP) and potassium oxonate (Oxo) in 1:0.4:1 M ratio [6]. Tegafur is converted to 5-FU by cytochrome CYP2A6 enzyme, which then rapidly catabolized by dihydropyrimidine dehydrogenase (DPD) in the liver and certain types of tumor. CDHP, a competitive antagonist of DPD, may enhance the concentration of 5-FU in both plasma and tumor tissues to potentate the antitumor activity of 5-FU, as demonstrated in subcutaneous xenograft animal model [6]. Oxo is a potent biochemical modulator of pyrimidine phosphoribosyl transferase, an enzyme responsible for the phosphorylation of 5-FU. Because preferentially localizes in the gut after absorption, Oxo may selectively inhibit the formation of 5-FU nucleotides in the gut and theoretically reduce gastrointestinal side effects of S-1 [6].
In two late phase II clinical studies, S-1 monotherapy at mean dose of 35–40 mg/m2 achieved 44.6% (45/101) of objective response rate (ORR), 244 days of median overall survival (OS) time and 37% of 1-year survival rate, and a low incidence of grade 3–4 toxicities [7, 8]. Recent randomized 3-arm trial (JCOG9912) showed that S-1 monotherapy, 5-day infusion of 5-FU and irinotecan/cisplatin combination could achieve compatible overall survival time in AGC patients [9]. However, earlier studies showed there were potential ethnic differences for S-1 in AGC patients, in terms of pharmacokinetic parameters, toxicity profile and maximum tolerated dose [10–15]. The recommended dose of S-1 for Caucasians was 30–35 mg/m2 twice daily when compared to the 35–40 mg/m2 twice daily for Asians [7–10, 16]. Herein, we reported the results of a phase II study evaluating the efficacy, safety and pharmacokinetics of S-1 in Taiwanese AGC patients.
Patients and methods
Patient eligibility
Patients with histologically or cytologically confirmed unresectable locally advanced, recurrent or metastatic gastric adenocarcinoma, age ≥20 years, Eastern Cooperative Oncology Group (ECOG) performance status score ≤2, at least 4 weeks from prior surgery or radiotherapy, measurable lesion(s) defined by Response Evaluation Criteria in Solid Tumors (RECIST) Guidelines [17], no prior chemotherapy except postoperative adjuvant chemotherapy that was associated with tumor relapse >6 months after end of treatment and adequate hematologic, hepatic and renal functions, i.e., absolute neutrophil counts (ANC) ≥1,500/μl, hemoglobin ≥9 g/dl, platelets ≥100,000/μl, and serum level of creatinine ≤1.5 × upper limit of normal (ULN), total bilirubin ≤1.5 × ULN were eligible. The eligible criterion for serum level of creatinine was amended to ≤1.0 × ULN after the occurrence of two treatment-related mortality.
Exclusion criteria included life expectancy less than 3 months, evidence of central nervous system metastasis, pregnancy or breast feeding, active infection, history of active cardiac diseases (e.g., angina or myocardial disease) within 6 months before study entry, history of other malignancy except for curatively treated non-melanoma skin cancer or cervical carcinoma in situ, mental status unfit for clinical trials or intestinal obstruction, mal-absorption or any other condition that precluded taking oral study medication. This study has been approved by the institutional review board of each participating hospital and Department of Health, Executive Yuen, Taiwan, and signed informed consent was obtained from all patients.
Treatment schedule
S-1 capsules (Taiho Pharmaceutical Co., Ltd., Tokyo, Japan) in the forms of 20 and 25 mg capsule containing 20 and 25 mg tegafur, respectively. S-1 was given orally twice daily (bid) on day 1–28 in a 42-day cycle. For patient whose body surface area (BSA) was <1.25, 1.25–1.5 and >1.5 m2 would receive S-1 at dose of 40, 50 and 60 mg bid, respectively. In the presence of ANC <1,000/μl, platelet <50,000/μl, creatinine >1.5× ULN and/or any grade 3–4 non-hematologic toxicity after treatment, the dose of S-1 would be reduced by one level in subsequent cycle of treatment. If a patient with BSA <1.25 m2 experienced the above toxicities, or who required a more than 4 week rest to recover toxicities, then the patient would be of-studied. We monitored patients’ compliance by their diaries. The treatment was repeated until disease progression, intolerable toxicity, consent withdrawal or death.
Evaluation of response and toxicity
Physical examination and symptoms, as well as complete blood count with differential count, serum biochemistry and electrolytes, prothrombin time/activated partial thromboplastin time (PT/aPTT), and urine analysis were evaluated before each treatment cycle. Adverse effect was assessed according to National Cancer Institute Common Toxicity Criteria, version 3.0 (NCI-CTC version III, 2003), from study entry until 30 days after the last dose of study medication. Computed tomography (CT) scan and/or magnetic resonance imaging (MRI) examination was conducted after every 6 weeks (one cycle) of treatment to evaluated tumor response according to RECIST criteria [17].
Pharmacokinetic measurements
Blood sampling for pharmacokinetics (PK) evaluation was obtained at before dosing and 0.5, 1, 2, 4, 6, 8, 12, 24 and 48 h after drug administration on day 1 and day 28 during the first cycle of treatment. Peripheral blood samples were collected into a heparinized tube at a volume of 5 ml at each sampling time and centrifuged, and the plasma was frozen at −20°C. The plasma concentrations of S-1 components (FT, CDHP and Oxo) and 5-FU were determined by either high-performance liquid chromatography (HPLC) or gas chromatography with mass spectrometric detection (GC–MS), in FALCO Biosystems Ltd., Kyoto, Japan. The following PK parameters were determined, including maximum plasma concentration (C max), time to maximum plasma concentration (T max), half-life (T 1/2), the area under the serum concentration–time curve from time 0 to infinity (AUC0–inf) and time 0 to the last quantifiable concentration, (AUC0–last) and (AUC0–last,ss). The AUC were computed from the raw concentration–time data by the linear trapezoidal method.
Statistical methods
This was an open-label, non-comparative phase II and pharmacokinetic study with primary endpoint of objective response rate. Secondary endpoints were progression-free and overall survival, toxicity profiles and PK. The Simon optimal two-stage design was used [18]. The response rate of interest and non-interest was P1 30% and P0 10%, respectively. If objective tumor responses were observed in more than two of 10 evaluable patients in the first stage, an additional 19 evaluable patients would be enrolled in the second stage. If there were more than six responders at the end of the second stage, this treatment would be considered as effective and deserving further investigation, with an a-value of 0.05 and a b-value of 0.20. Progression-free survival was defined as the duration from the date of starting protocol treatment to the date of disease progression or any cause of death, while the data of patients who loss of follow-up before progression would be censored at the date of last follow-up. Overall survival represented the duration from the date of starting protocol treatment to the date of death from any cause. Survival was estimated by Kaplan–Meier analysis [19]. Significance level was defined as P < 0.05. All statistics were two-sided and performed using SAS software (version 9.1.3, SAS Inc., Cary, NC).
Results
Patient and demographic characteristics
Between February 2006 and November 2006, a total of 34 patients were enrolled from at six participating centers. There were 9 women and 25 men (median age, 66.5 years; range, 37–84), 31 with ECOG performance status of 0–1 and 15 with prior history of gastrectomy. Patient characteristics were as shown in Table 1.
Efficacy
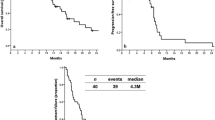
The median treatment cycle was 2 cycles (range, 1–17). Three patients were not evaluable for tumor responses because of protocol violation in one, and early death in two. Among the 31 evaluable patients, best tumor response was complete response (CR) in 1, partial response (PR) in 11, stable disease (SD) in 4 and progressive disease (PD) in 15. On an intent-to-treat analysis, the ORR was 35.3% (95% CI: 19.2–51.3%). Upon the end of December 2008, the median follow-up time of ITT population was 7.1 (range: 0.7–28.4) months. The median PFS and OS were 2.9 (95% CI: 2.4–5.8) months and 9.8 (95% CI: 6.1–NA) months, respectively. The median duration of response of the 12 responders was 11.0 (95% CI: 5.8–NA) months and, the cumulative 12-month survival rate was 40%. The Kaplan–Meier estimated PFS and OS curves are shown in Fig. 1.
Safety
The median initial actual dose and median relative dose intensity per patients of S-1 were 37.0 mg/m2 (range, 32.4–39.7) bid and 94.6% (range, 48.6–100), respectively. Adverse events (AE) were assessed in all 34 patients (Table 2). The major grade III/IV of hematologic toxicity were anemia in 23.5%, neutropenia in 11.7% and thrombocytopenia in 8.8%, while of non-hematologic toxicity were anorexia 17.6%, creatinine increased 5.9%, stomatitis 5.9%, hand–foot syndrome 5.9%, diarrhea 5.9%, asthenia 5.9% and nausea 2.9%. There were three deaths while on protocol treatment: one died of cerebrovascular events and the other two deaths were caused by treatment-related grade 4 neutropenia and concomitant infection. Both patients were men and thin with body mass index of 15.8 and 15.6 kg/m2, respectively. Despite serum creatinine level fulfilled eligibility criteria ≤1.5 × ULN at study entry, both patients were found to have moderate to severe renal function impairment with calculated glomerular filtration rate (GFR) of 27.8 and 44.8 ml/min, respectively, by Cockcroft-Gault equation [GFR = (140 − age) × body weight/(72 × serum creatinine level)] in retrospective safety monitoring. After the two events, the protocol was amended to change the inclusion criterion for renal function from creatinine ≤1.5 × ULN to ≤1.0 × ULN, and there were no more grade 4 neutropenia afterward. There toxicity profiles were not significantly different between gastrectomy and non-gastrectomy subgroups (data not shown).
Pharmacokinetics study
Twelve patients had single-dosing pharmacokinetic study on day 1, while 7 of them participated multiple dosing PK study on day 28. The changes of plasma 5-FU, FT, CDHP and Oxo levels after single dosing of S-1 were shown in Fig. 2, while their PK parameters after single and multiple dosing were listed in Table 3. PK parameters of plasma 5-FU after single administration were C max 143.8 ± 49.5 ng/ml, T max 2.83 ± 1.03 h, AUC0–inf 846.4 ± 330.0 ng × h/ml and T 1/2 2.52 ± 0.89 h, while the C max and AUC0–inf of FT were 2,551.8 ± 589.1 ng/ml and 32,126.2 ± 6,352.7 ng × h/ml, respectively. The corresponding parameters for CDHP and Oxo were 347.2 ± 165.8 ng/ml and 1,719.7 ± 773.6 ng × h/ml, and 78.1 ± 79.9 ng/ml and 471.0 ± 343.2 ng × h/ml, respectively. The PK parameters of 5-FU, CDHP and Oxo after multiple dosing at day 28 were nearly coincident with those after single-dose administration, as shown in Table 3. The results indicated the steady-state PK of 5-FU, CDHP and Oxo could be predicted from single-dose PK study. Furthermore, the PK parameters were not significantly different between patients with and without prior gastrectomy (six patients in each subgroup, supplement table 1).
Discussion
In this study, S-1, at median initial dose of 37.0 mg/m2 twice daily, could achieved 35.3% (95% CI: 19.8–53.5%) of response rate, 9.8 (95% CI: 6.1–NA) months of median OS time and 40% of 1-year survival rate in Taiwanese AGC patients. The results are comparable with previously reported phase II studies with the corresponding parameters being 19.3–49.0%, 250–265 days and 34–37%, respectively [7–10]. With similar median initial actual dose of S-1, ranged from 36.5–40 mg/m2, the incidence of grade 3–4 non-hematologic toxicity of S-1 monotherapy in our study were generally <10% (except anorexia) and largely compatible with the phase II reports from Japan and Korea [6–8, 10]. However, the incidence of grade 3–4 anemia in our study was 23.5%, when compared to the 8.5 and 16.1% reported from Japan and Korea, respectively [6, 10]. The mechanism for the higher incidence of anemia in Taiwanese and Korean populations was not clear. However, Jeung et al. ever performed a micro-array-based comparative genomic hybridization study and suggested that baseline hemoglobin level combined with three genetic copy number variations (HIST1H2BL, C10orf127, and XPNPEP2) may provide a predictive model for the development of severe hemoglobin reduction in patients receiving S-1 monotherapy. Unfortunately, such pharmacogenetic study was not preplanned in our study, and we were not able to validate the findings of our Korean colleagues [10].
The 11.8% of grade 3–4 neutropenia in our study was similar to the 4.8–11.1% observed in other Asian studies [6, 9]. However, the cause of grade 4 neutropenia in two of our patients who experienced and died of severe neutropenia with concomitant infection in early study period was considered to result from underestimation of renal functional impairment by serum creatinine level in patients with low body mass. Such events were ameliorated after protocol amendment to include only patients with more adequate serum creatinine level. Although both of the patients did not participate PK study, however, earlier reports had shown that impaired renal function would reduce CDHP clearance to result in prolonged exposure to high concentration of plasma 5-FU and thus more severe myelosuppression [7, 11]. These findings highlight that accurate renal function assessment is critical for patients going to receive S-1 and concurs with the report of Ikeda et al. that patients with impaired renal function may need individualized dosing of S-1 and pharmacokinetic monitoring [20].
In this study, the PK study showed trend toward lower AUC5–FU and higher AUCFT comparing to the PK data from Western countries [12–15, 21], as did in reports from other Asian studies, as shown in Table 4 [10–15]. The incidence of grade 3–4 diarrhea in our study was 5.9%, which are also comparable with that observed in other Asian studies [9, 10, 22, 23]. On the other hand, diarrhea has been the major principal dose-limiting toxicity of S-1 in Caucasian population [12–15]. In the studies of Ajani et al. and Van Groningen et al., the occurrence of severe diarrhea was significantly correlated with AUC5–FU, with P values of 0.004 and 0.034, respectively [12, 24]. Based on the results, the discrepancy in incidence of severe diarrhea between the Asian and Caucasian has been considered to result from the higher AUC5–FU/AUCFT ratio secondary to higher incidence of CYP2A6 extensive metabolizer phenotype in Caucasian population [24]. However, recent data suggested that ethnicity and AUC5–FU might not be the only factors attributed to the high incidence of severe diarrhea observed in some Western studies. Of the three phase I studies of S-1 monotherapy conducted in Europe and US, all achieved comparable AUC5–FU (ranging from 894 ± 151 to 1,134 ± 332 ng × h/ml) [12–15]. In the studies of Zhu et al. and Hoff et al., the MTD of S-1 for pretreated cancer patients in US was 30 mg/m2 bid [14, 15]. In the latter study, grade 3–4 diarrhea was the major DLT and observed in 50 and 100% of patients receiving 35 mg/m2 and 40 mg/m2 bid, respectively [15]. On the other hand, in an EORTC phase I study, van Groningen et al. showed the MTD of patients with chemo-naïve and heavily pretreated advanced solid tumor was 40 and 35 mg/m2 bid, respectively [12]. In subsequent EROTC phase II study, Chollet et al. showed that grade 3–4 diarrhea in AGC patients receiving 35–40 mg/m2 bid of S-1 was 5 out of 30 (16.7%) patients [16]. It appears that factor(s) other than AUC5-FU may be attributed to the intra-ethnic difference in the incidence of severe diarrhea after S-1 in Caucasian population.
In the study of Adjani et al., the occurrence of severe diarrhea was significantly correlated with AUC5–FU but not AUCOxo [18]. However, comparing the pharmacokinetic data after S-1 monotherapy, we noted that the mean AUCOxo in European, Asian (including current study) and US studies was 566, 337–471 and 206–280 ng × h/ml, respectively. Since the role of Oxo, an inhibitor of orotate phosphoribosyl transferase, as a component of S-1 is to reduce the phosphorylation of 5-FU in gastrointestinal tissues and hence to reduce the gastrointestinal toxicity of S-1. The impact of AUCOxo on the occurrence of S-1 associated severe diarrhea still deserves exploration in future study [10, 25, 26].
Sakuramoto et al. recently showed that adjuvant S-1 therapy could effectively prolong the overall survival of patients with D2 dissected stage II-III gastric cancer [27]. However, among the 517 patients in S-1 arm, 143 (27.6%) patients could not complete the 12 months assigned treatment due to poor compliance and/or adverse events. Furthermore, dose reduction was required in 46.5% of patients who received S-1 for 12 months. These observations raised the concern regarding the effect of gastrectomy on the pharmacokinetics of 5-FU after oral administration of S-1. Our data, as shown in supplement Table 1, concurs with most of previous reports to show the pharmacokinetics of 5-FU and S-1 components were not significant different between patients with and without prior gastrectomy [15, 28–30]. The finding indicates that S-1 can be safely administered in adjuvant setting.
Recently, two large-scale, multinational, randomized phase III trials demonstrated that, while in combination with cisplatin alone (ML 17032) or with epirubicin plus one platinum analogue (REAL-2 study), capecitabine is significantly non-inferior to infusional 5-FU in advanced gastric cancer [31, 32]. On the other hand, JCOG 9912 and SPIRITS trials from Japan showed that S-1 is non-inferior to infusional 5-FU alone and S-1/cisplatin combination is significantly superior to S-1 monotherapy for AGC, respectively [9, 22]. It appears oral fluoropyrimidine plus either cisplatin or oxaliplatin would be the standard or backbone for future chemotherapy in AGC. Lee et al. prospectively compared the activity and safety of capecitabine/cisplatin and S-1/cisplatin combinations in a randomized phase II in elderly AGC patients in Korea [23]. The therapeutic efficacies, in terms of overall response rate, median TTP and overall survival, and hematologic and non-hematologic toxicity profiles in the two study arms are largely compatible. However, the relative dose intensity of capecitabine steadily decreased during treatment, which was mainly caused by treatment delays or dose reductions secondary to hand–foot syndrome, whereas that of S-1 remained steady (86.7 vs. 96.3%, P = 0.003) [23]. The higher incidence of hand–foot syndrome after capecitabine/cisplatin comparing to S-1/cisplatin combination has also been reported in one retrospective study [33]. However, the better tolerability of S-1/cisplatin versus capecitabine/cisplatin may require further validation in prospective randomization trials.
In conclusion, our study demonstrated that the efficacy, toxicity and pharmacokinetics profiles of S-1 in Taiwanese AGC population are compatible with those reported from other Asian studies. The findings support the use of S-1 as an alternative for 5-FU, either alone or in combination with platinum analogue, in the management of AGC in Taiwan. However, accurate renal function assessment and cautious administration with more closely monitoring of adverse events in patients with low body mass are mandatory.
References
Garcia M, Jemal A, Ward EM et al (2007) Global cancer facts & figures 2007. American Cancer Society, Atlanta, GA
Hsu PY (2008) Statistics on causes of death. In: Health statistics in Taiwan 2006 Department of Health, Executive Yuan, R.O.C. (Taiwan), Taipei, pp 12–43
Hunahl SA, Menck HR, Mansour EG, Winchester DP (1997) The National Cancer Data Base report on gastric carcinoma. Cancer 80:2333–2341
Wagner AD, Grothe W, Haerting J, Kleber G, Grothey A, Fleig WE (2006) Chemotherapy in advanced gastric cancer: a systematic review and meta-analysis based on aggregate data. J Clin Oncol 24:2903–2909
Ohtsu A (2005) Current status and future prospects of chemotherapy for metastatic gastric cancer: a review. Gastric Cancer 8:95–102
Shirasaka T (2009) Development history and concept of an oral anticancer agent S-1 (TS-1). Its clinical usefulness and future vistas. Jpn J Clin Oncol 39:2–15
Sakata Y, Ohtsu A, Horikoshi N, Sugimachi K, Mitachi Y, Taguchi T (1998) Late phase II study of novel oral fluoropyrimidine anticancer drug S-1 (1M Tegafur-0.4M Gimestat-1M Otastat Potassium) in advanced gastric cancer patients. Eur J Cancer 34:1715–1720
Koizumi W, Kurihara M, Nakano S, Hasegawa K (2000) The S-1 Cooperative Gastric Cancer Study Group. Phase II study of S-1, a novel oral derivative of 5-fluorouracil, in advanced gastric cancer. Oncology 58:191–197
Boku N, Yamamoto S, Fukuda H et al (2009) Fluorouracil versus combination of irinotecan plus cisplatin versus S-1 in metastatic gastric cancer: a randomised phase 3 study. Lancet Oncol 10:1063–1069
Jeung HC, Rha SY, Kim HK et al (2007) Multi-Institutional phase II study of S-1 monotherapy in advanced gastric cancer with pharmacokinetic and pharmacogenomic evaluations. Oncologist 12:543–554
Hirata K, Horikoshi N, Aiba K et al (1999) Pharmacokinetic study of S-1, a novel oral fluorouracil antitumor drug. Clin Cancer Res 5:2000–2005
Van Groeningen CJ, Peters GJ, Schornagel JH et al (2000) Phase I clinical and pharmacokinetic study of oral S-1 in patients with advanced solid tumors. J Clin Oncol 18:2772–2779
Chu QS, Hammond LA, Schwartz G et al (2004) Phase I and pharmacokinetic study of the oral fluoropyrimidine S-1 on a once-daily-for-28-day schedule in patients with advanced malignancies. Clin Cancer Res 10:4913–4921
Zhu AX, Clark JW, Ryan DP et al (2007) Phase I and pharmacokinetic study of S-1 administered for 14 days in a 21-day cycle in patients with advanced upper gastrointestinal cancer. Cancer Chemother Pharmacol 59:285–293
Hoff PM, Saad ED, Ajani JA et al (2003) Phase I study with pharmacokinetics of S-1 on an oral daily schedule for 28 days in patients with solid tumors. Clin Cancer Res 9:134–142
Chollet P, Schoffski P, Weigang-Kohler K et al (2003) Phase II trial with S-1 in chemotherapy-naïve patients with gastric cancer. A trial performed by the EORTC Early Clinical Studies Group (ECSG). Eur J Cancer 39:1264–1270
Therasse P, Arbuck SG, Eisenhauer EA et al (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92:205–216
Simon R (1998) Optimal two-stage design for phase II clinical trials. Control Clin Trials 10:1–10
Kaplan EL, Meier P (1958) Nonparametric estimation from incomplete observation. J Am Stat Assoc 53:457–481
Ikeda M, Furukawa H, Imamura H et al (2002) Pharmacokinetic study of S-1, a novel oral fluorouracil antitumor agent in animal model and in patients with impaired renal function. Cancer Chemother Pharmacol 50:25–32
Peters GJ, Noordhuis P, Van Kuilenburg AB et al (2003) Pharmacokinetics of S-1, an oral formulation of ftorafur, oxonic acid and 5-chloro-2, 4-dihydroxypyridine (molar ratio 1:0.4:1) in patients with solid tumors. Cancer Chemother Pharmacol 52:1–12
Koizumi W, Narahara H, Hara T et al (2008) S-1 plus cisplatin versus S-1 alone for first-line treatment of advanced gastric cancer (SPIRITS trial): a phase III trial. Lancet Oncol 9:215–221
Lee JL, Kang YK, Kang HJ et al (2008) A randomized multicentre phase II trial of capecitabine vs S-1 as first-line treatment in elderly patients with metastatic or recurrent unresectable gastric cancer. Br J Cancer 99:584–590
Ajani JA, Faust J, Ikeda K et al (2005) Phase I pharmacokinetic study of S-1 plus cisplatin in patients with advanced gastric carcinoma. J Clin Oncol 23:6957–6965
Shirasaka T, Shimamoto Y, Fukushima M (1993) Inhibition by oxonic acid of gastrointestinal toxicity of 5-fluorouracil without loss of its antitumor activity in rats. Cancer Res 53:4004–4009
Takechi T, Nakano K, Uchida J et al (1997) Antitumor activity and low intestinal toxicity of S-1, a new formulation of oral tegafur, in experimental tumor models in rats. Cancer Chemother Pharmacol 39:205–211
Sakuramoto S, Sasako M, Yamaguhi T et al (2007) Adjuvant chemotherapy for gastric cancer with S-1, an oral fluoropyrimidine. N Engl J Med 357:1810–1820
Tsuruoka Y, Kamano T, Kitajima M et al (2006) Effect of gastrectomy on the pharmacokinetics of 5-fluorouracil and gimeracil after oral administration of S-1. Anticancer Drug 17:393–399
Kochi M, Fujii M, Kanamori N et al (2007) Effect of gastrectomy on the pharmacokinetics of S-1, an oral fluoropyrimidine, in resectable gastric cancer patients. Cancer Chemother Pharmacol 60:693–701
Kim WY, Nakata B, Hirakawa K (2007) Alternative pharmacokinetics of S-1 components, 5-fluorouracil, dihydrofluorouracil and α-fluoro-β-alanine after oral administration of S-1 following total gastrectomy. Cancer Sci 98:1604–1608
Cunningham D, Starling N, Rao S et al (2008) Capecitabine and oxaliplatin for advanced esophagogastric cancer. N Engl J Med 358:36–46
Kang YK, Kang WK, Shin DB et al (2009) Capecitabine/cisplatin versus 5-fluorouracil/cisplatin as first-line therapy in patients with advanced gastric cancer: a randomised phase III noninferiority trial. Ann Oncol 20:666–673
Seol YM, Song MK, Choi YJ et al (2009) Oral fluoropyrimidines (capecitabine or S-1) and cisplatin as first-line treatment in elderly patients with advanced gastric cancer: a retrospective study. Jpn J Clin Oncol 39:43–48
Acknowledgments
The authors wish to thank the centres and physicians participating in the study: National Taiwan University Hospital (Chih-Hung Hsu, M.D., Ph.D.); Veterans General Hospital, Taipei (Chung-Pin Li, M.D. Ph.D.); Chang-Gung Memorial Hospital, Linkou (Tsai-Shen Yang, M.D.); National Institute of Cancer Research, Tainan (Her-Shyong Shiah, M.D., Jang-Yang Chang, M.D.); Mackay Memorial Hospital, Taipei (Tsang-En Wang, M.D.); Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung (Chang-Ming Jan, M.D.). The study was funded by TTY Biopharm Co., Ltd., Taipei, Taiwan, and Taiho Pharmaceutical Co., Ltd., Tokyo, Japan.
Conflict of interest
Jen-Shi Chen, Yee Chao and Li-Tzong Chen received honoraria from TTY Biopharm Co., Ltd, Taipei, Taiwan. Li-Tzong Chen received research funding from TTY Biopharm Co., Ltd and Taiho Pharmaceutical Co., Ltd, Tokyo, Japan.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Jen-Shi Chen and Yee Chao contributed equally to the manuscript.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chen, JS., Chao, Y., Hsieh, RK. et al. A phase II and pharmacokinetic study of first line S-1 for advanced gastric cancer in Taiwan. Cancer Chemother Pharmacol 67, 1281–1289 (2011). https://doi.org/10.1007/s00280-010-1416-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-010-1416-8