Abstract
Background
Breast cancer is a clinically heterogeneous disease. Approximately 10–15 % of breast cancer patients develop distant metastases within 2 years of diagnosis with a poor 5-year survival rate of 21 %. Little data have been gathered about how some breast cancer metastasizes earlier than expected. The study aimed to identify predictors of distant metastases among breast cancer patients in relation to their clinical and tumour characteristics. The results of the study may have important implications in our understanding of the disease process allowing more aggressive treatment and monitoring of certain subgroups of patients.
Methodology
Retrospective review of 215 patients (54 % early stage and 46 % locally advanced stage) who fulfilled the specified criteria was performed. Twelve variables were considered. Univariate and multivariate logistic regression analyses were performed to identify independent predictors of developing distant metastasis within 24 months after surgery and adjuvant therapy.
Results
Of the 215 patients, 27.9 and 17.7 % developed bone and visceral metastasis, respectively. Bone metastasis was significantly dependent on stage, tumour size, lymph node involvement, lymphovascular invasion, estrogen receptor, progesterone receptor and Her/2-neu pattern (p < 0.05). Visceral metastasis was significantly dependent on age, menopausal status, stage, tumour size, lymph node involvement, estrogen receptor, progesterone receptor and Her-2/neu pattern (p < 0.05). Among patients with bone and visceral metastases, 67 and 43 % have triple negative pattern, respectively. Logistic regression provided an accurate model for predicting bone but not visceral metastasis.
Conclusion
A significant fraction of breast cancer patients experienced early metastasis. Our data suggest that tumour stage, size and lymph node involvement are major predictors of metastasis. Her-2/neu over-expression alone is not a strong predictor of early metastasis but triple negative breast cancers belong to an aggressive subgroup with early metastatic capacity. Young, premenopausal patients may benefit from aggressive surveillance and treatment since they tend to present with early visceral spread.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common cancer in the Philippines. About 3 out of 100 Filipino women will develop breast cancer in their lifetime. Although breast cancer has one of the highest 5-year survival rate compared to other malignancies in the country, it is still about 40–50 % which is much lower than the 80–98 % 5-year survival rate in developed countries (Ngelangel and Wang 2002). The relatively low survival rate of breast cancer in a low resource country like the Philippines is due to lack of awareness and lack of adequate diagnosis and treatment leading to progression of the disease (Ngelangel and Wang 2002; El Saghir et al. 2011). Distant metastasis is the most common form of recurrence and the main cause of death in patients with breast cancer (Gluck 2007). Patients with metastatic breast cancer have a median survival of 18–24 months (Gennari et al. 2005). Hence it is important to distinguish subset of patients with aggressive disease at risk for early progression and metastasis.
The original model in cancer metastasis reflects the view that metastatic capacity is a late acquired event in the natural history of majority of cancers. The original hypothesis by Halsted (Halstedian Paradigm) proposed that breast cancer was a local disease and tumour dissemination occurred via regional nodes. Aggressive loco-regional control prevents local recurrence which is a determinant of distant metastasis. This hypothesis was later displaced by Fisher (Fisherian Paradigm) which proposed that women with early stage disease may already have distant micro-metastasis at the time of diagnosis increasing their later risk of developing overt distant metastasis irrespective of the extent of loco-regional treatment. This view switched the emphasis from aggressive local control to the importance of effective systemic therapy (Gluck 2007; Rabinovitch and Kavanagh 2009).
Currently, the prevailing model of tumour pathogenesis combined earlier theories as proposed by Harris and Hellman (Spectrum Theory). Tumour cells spread via lymphatic vessels in early stage breast cancer and via hematogenous route in late stage disease (Rabinovitch and Kavanagh 2009). Breast cancer is a clinically heterogeneous disease with metastatic capacity as an inherent feature of breast tumours. Half of all breast cancer recurrences occur >5 years after initial therapy. However, approximately 10–15 % of patients with breast cancer develop early distant metastasis. Early metastasis is defined as relatively short period of time (less than 2 years) that elapsed between the diagnosis of the primary tumour and the development of distant spread. Also, this heterogeneity makes it difficult not only to define cure for the disease, but also assess the risk factors predictive of metastasis (Cardoso et al. 2011; De Vita et al. 2008; Giordano 2003; Popoola et al. 2012; Jensen et al. 2011).
Objective and significance of the study
The objective of the study was to identify predictors of early distant metastasis in women with breast cancer in relation to their clinical and tumour characteristics. There are established prognostic markers of survival in breast cancer but there is paucity of published data correlating risk factors predicting the likelihood of early metastasis. The primary tumour size, lymph node involvement, tumour histology, estrogen and progesterone receptor status (ER and PR) and Her-2/neu gene amplification are well-known prognostic markers but there seems to be a more varied correlation between these factors and the probability of metastasis. For example, approximately one-third of breast cancer patients without lymph node involvement develop distant metastasis. Likewise, one-third of breast cancer patients with lymph node involvement remain free of distant metastasis (Cardoso et al. 2011; De Vita et al. 2008).
The postulated hypothesis was that a combination of inherent tumour features determines metastatic capacity of breast cancers and not just a direct function of its size and local invasion. This investigation may have important implications in our understanding of the disease process. The outcome of the study could identify patients at risk for metastasis from the onset of breast cancer. More aggressive treatment and follow-up may be justified in certain subgroups of patients.
Methodology
This was a retrospective single-centre analytical study conducted at the University of Santo Tomas Hospital. The institutional review board of the hospital approved the study design. Eligible subjects were selected from female patients with breast cancer seen from January 2009 to December 2010 at the cancer institute and clinics. The records of patients were reviewed from the time of diagnosis of their breast cancer and surgery. A 2-year period was specified as the observation period for either metastasis-free interval or occurrence of distant metastasis. Occurrence of distant metastasis was defined as period between first diagnosis of breast cancer and first recurrence of bone or visceral metastasis. Metastasis-free interval was defined as freedom from metastasis within the 2-year observation period. The sample size (215 subjects) exceeded the minimum requirement (127 subjects) for the regression study given the desired probability level (0.05), number of predictors (12), effect size (0.15) and statistical power (0.8).
The subjects included were adult (≥19 years old) females diagnosed with breast adenocarcinoma established by histopathology result. They have undergone surgery (modified radical mastectomy or breast conservation therapy) followed by standard adjuvant chemotherapy and radiotherapy if recommended by their particular stage. The hospital cancer institute followed the recommendations of the National Comprehensive Cancer Network (NCCN) guidelines. Distant metastases were ruled out before surgery by physical examination, abdominal ultrasound, chest radiograph and bone scintigraphy. Of the 349 records of breast cancer patients reviewed, 215 satisfied the inclusion and exclusion criteria. The exclusion criteria and the reasons for exclusion of 134 subjects were as follows: inadequate follow-up of less than 24 months (33 %), unable to receive standard treatment specifically surgery, chemotherapy and radiotherapy if warranted for their particular stage (28 %), insufficient data (16 %), presence of distant metastasis at the time of diagnosis (10 %), local or soft tissue recurrence (6 %), carcinoma in situ, inflammatory breast cancer or non-adenocarcinoma (4 %), and presence of a second primary malignancy (1 %).
Data gathered were age, menopausal status, histologic subtype, pathologic stage, primary tumour, lymph node involvement, lymphovascular invasion, histologic grade, estrogen and progesterone receptor, Her-2/neu over-expression and presence of triple negative status. The data were obtained from medical records of patients. The staging were divided into early (stage I and II) and locally advanced (stage III) disease. Based on the tumour node metastasis (TNM) staging classification of the American Joint Committee on Cancer (AJCC) and the International Union for Cancer Control (IUCC), the primary tumour was classified as T1 if ≤20 mm, T2 if 21–50 mm, T3 if >50 mm or T4 if with chest wall or skin extension (American Joint Committee on Cancer 2010). Likewise, the regional lymph node involvement was categorized as N0 if none, N2 if with 1–3 lymph nodes, N3 if with 4–9 lymph nodes or N4 if with 10 or more lymph nodes. The lymphovascular invasion and histological grade were reviewed from the histopathological result after surgery. Estrogen and progesterone receptor status was defined by immunohistochemistry, and staining of 10 % or more of tumour cells was adopted as positive. For Her-2/neu, immunohistochemistry reaction of 3+ was considered positive while immunohistochemistry reaction of 0 or 1+ was considered negative. Fluorescence-in situ hybridization (FISH) was needed to verify over-expression if immunohistochemistry reaction was 2+. Data which were not available or uncertain were recorded as unknown. Although surgery and adjuvant therapy were absolute inclusion criteria, the study did not take into consideration the type of treatment received by the patient.
Data were analysed using Statistical Package for Social Sciences (SPSS) version 17.0. Univariate analyses were performed to identify independent predictors. A cut-off p value of <0.05 was considered significant. A multivariate logistic regression model was derived for each set of predictors found to be significant in the univariate analyses.
Results
The characteristics of 215 cases of breast cancer seen at our institution are summarized in Table 1. The median age of the subjects was 49 years, with a range from 31 to 67 years. The predominant tumour type was invasive ductal carcinoma (79.5 %) followed by invasive lobular carcinoma (13 %). Of the 215 subjects, 60 (27.9 %) developed bone metastasis and 38 (17.7 %) developed visceral metastasis within 2 years after detection of primary tumour and surgery. Visceral metastases were distributed as follows: fifteen to the liver (39.5 %), twelve to the lung parenchyma (31.8), seven to the brain (18.4 %) and two to the pleura (5.3 %). The median time to occurrence of metastasis within the specified observation period was 14 months, with the earliest seen after 4 months.
Table 2 shows the distribution of the 12 variables with the proportion of subjects in each category with bone metastasis. The odds ratios for the presence of bone metastasis and p value derived from the univariate analysis were also shown.
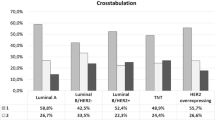
Bone metastasis was found to be significantly dependent (p < 0.05) on 7 variables: stage, primary tumour size, lymph node involvement, lymphovascular invasion, estrogen and progesterone receptor status and pattern. Among breast cancer patients with bone metastasis, 67 % have triple negative status (negative estrogen receptor and progesterone receptors and Her-2/neu non-over-expression or non-amplification).
Table 3 shows the distribution of the 12 variables with the proportion of subjects in each category with visceral metastasis. The odds ratios for the presence of visceral metastasis and p value derived from the univariate analysis were also shown.
Visceral metastasis was found to be significantly dependent (p < 0.05) on 8 variables: age, menopausal status, stage, primary tumour size, lymph node involvement, estrogen and progesterone receptor status and pattern. Among breast cancer patients with visceral metastasis, 43 % have triple negative status (negative estrogen and progesterone receptors and Her-2/neu non-over-expression or non-amplification).
The multivariate regression model for early bone metastasis was found to be significant (p = 0.046). The logistic regression provided an accurate model for predicting early bone metastasis. The sensitivity and specificity of the prediction model were 74 and 97 %, respectively.
On the other hand, the multivariate regression model for early visceral metastasis was not significant (p = 0.671). Although individual predictors were identified in the univariate logistic regression analysis, their combined effect did not provide an accurate model for predicting early visceral metastasis. The high specificity (96 %) of the model was offset by its low sensitivity (26 %).
Discussion
We were able to identify factors that independently predict the development of early distant metastasis. Bone metastasis and visceral metastasis were analysed separately because patients who had bone metastasis as their first and only site of metastasis are known to have a longer survival than those who present first with visceral metastasis with or without bone involvement (Solomayer et al. 2000). In general, skeletal metastasis has a more favourable prognosis than visceral metastasis (Kuru et al. 2008). Breast cancer patients remain at risk for recurrence for many years even after receiving standard treatment. Nevertheless, the greatest risk of recurrence is in the first 2–3 years after detection of primary tumour and subsequent surgery (De Vita et al. 2008). Those with early relapse are considered to have high-risk features that put them to such disadvantage.
The stage of malignancy, primary tumour size and lymph node involvement were established prognostic factors affecting over-all survival of patients with breast cancers (Gluck 2007; De Vita et al. 2008; Kuru et al. 2008). The results of our study showed that stage III disease was predictive for metastasis compared to earlier stages. With regard to primary tumour size, early bone and visceral metastases were observed once tumour size exceeded 20 mm. Likewise, even 1–3 regional lymph node involvement predicted early bone and visceral metastases. However, there was no correlation between the number of positive lymph nodes and the likelihood of whether there would be bone or visceral metastasis. Hormone receptor status and Her-2/neu over-expression pattern were independent variables associated with early metastasis.
Locally advanced breast cancers at diagnosis were predisposed to early bone and visceral metastasis (44 and 29 %, respectively) as compared to early stage breast cancers (14 and 8 %, respectively). Tumour size is an established predictor of lymph node metastasis in prior studies (Gajdos 1999). Our investigation supports the relationship between primary tumour size and the probability of early distant metastasis. The larger the tumour size the greater was the probability of distant recurrence as observed in the frequency of bone and visceral metastasis in T2 and T3 tumours (>20 mm) compared to T1 tumours.
Greater than 3 axillary lymph node involved predicts the greater probability of metastasis but there is no direct correlation between the number of lymph nodes and proportion of subjects with metastasis. Coleman et al. pointed out that patients with ≥4 axillary lymph nodes were more likely to develop disease outside the skeleton, and tumours with 1–3 or no axillary lymph node are more likely to remain confined to the skeleton (Kuru et al. 2008; Coleman et al. 1998). However, the current findings agree with those of Solomayer et al. (2000) who suggested that number of lymph nodes involved does not directly correlate with bone or visceral metastasis. The plausible reason is that bone and visceral metastases were analysed separately in this study instead of bone and bone plus visceral metastasis. If simultaneous bone and visceral metastases were analysed concurrently and were categorized under visceral metastasis, 4 or more positive regional lymph nodes would favour early visceral metastasis rather than bone metastasis. Nevertheless, lymph node status is an independent predictor of metastasis.
Earlier studies associated bone metastasis with lobular carcinoma but this was not observed in our study (Coleman et al. 1998). The histology of the tumour did not predict the early bone or visceral metastasis. Histologic grade of tumour was not a significant predictor of early metastasis in our investigation. Existing studies support the theory that tumour grade only becomes significant predictor in young patients wherein the grade of the tumour determines the probability of aggressive disease. Lymphovascular invasion was a significant predictor of early metastasis in the bones but not in visceral organs. The drainage of blood to the skeleton via vertebral venous plexus, which drains blood from the chest wall, explains the tendency of breast to produce metastasis in the axial skeleton and limb girdles (Coleman et al. 1998). This result supports our hypothesis that metastatic capacity to visceral organs especially of the more aggressive breast cancers may be an inherent feature of the tumour and not just a function of size and local invasion.
More estrogen receptor (ER) and progesterone receptor (PR)-positive tumours present with bone metastasis rather than visceral metastasis. This finding is in accordance with previous studies which demonstrated that there was significant association between ER-positive tumours and bone metastasis (Coleman et al. 1998). Patients with ER- and PR-positive tumours have independently favourable prognosis and this feature may also explain the more indolent course of patients with bone metastasis compared to visceral metastasis (Jensen et al. 2011; Gajdos 1999). Contrary to previous studies by Clark et al. that ER-positive tumours were likely to recur in the bone and ER-negative tumours were likely to recur in the viscera (Clark et al. 1987), our findings maintain that both bone and visceral metastases are associated with ER-negative tumours. In contrast with the study cited, bone and visceral metastasis are analysed independently in this study.
Younger age and premenopausal status appeared to be predictors of early visceral metastasis. This is complementary to earlier reports that elderly postmenopausal patients were more likely to have confined to the skeleton than those who are premenopausal. Breast tumours in women under 40 are more likely to be associated with high-risk tumour features and poorer prognosis including incidence of metastasis (Gajdos 1999). Of the 20 premenopausal subjects with visceral metastasis in this study, 6 over-expressed Her-2/neu gene, 5 were estrogen and progesterone receptor-negative and 4 were triple negative breast cancers.
The results showed that triple negative breast cancer (TNBC) is an aggressive breast cancer subtype with propensity for early metastasis both in the bone and in the viscera (Ossovskaya et al. 2011). The metastatic potential of this subgroup of patients is usually manifest within 5 years of primary tumour diagnosis (Yau et al. 2010). However, it was also postulated in evidence available that early triple negative breast cancers are sensitive to standard chemotherapy and distant metastasis after 5–10 years becomes less common than in other breast cancers (Ossovskaya et al. 2011; Yau et al. 2010; Cianfrocca and Goldstein 2004).
Based on the current NCCN guidelines, routine systemic staging is not recommended especially for early breast cancers in the absence of symptoms, that is, bone scan in the presence of localized bone pain or elevated alkaline phosphatase, chest CT scan in the presence of pulmonary symptoms and abdominal/pelvic CT scan or MRI in the presence of abdominal symptoms, abnormal physical examination or abnormal liver function tests (Carlson et al. 2012). The results of the study justify a more comprehensive work-up for breast cancer patients who are put to disadvantage because of poor predictors of early distant metastasis.
In earlier studies, Diel et al. (1998) demonstrated that bisphosphonates can reduce the incidence and number of new skeletal metastasis. Our result revives the potential role of bisphosphonates as prophylaxis to prevent skeletal metastasis. Likewise, patients with high risk of developing early bone or visceral metastasis should receive anthracycline and taxane-based treatments at the onset since these are considered the most active agents in treatment of metastatic breast cancer (De Vita et al. 2008).
To the best of our knowledge, the present study is the first to address predictors of early distant metastasis among stage I to III breast cancers after surgery and adjuvant treatment. Our study has some limitations. Although loco-regional and adjuvant therapy were absolute inclusion criteria, the study did not take into consideration the particular treatment received by each subject. As in other retrospective study, selection bias and data sufficiency should be taken into consideration.
In future studies, validation of the regression models may be pursued in bigger prospective cohorts of patients. Treatment received by the subjects may be included in the analysis. If sample size would permit, subanalyses of predictors per stage can be done to determine variables unique to a particular stage. New methods such as measurement of proliferation markers like S-phase fraction and genetic profiling by micro-array analyses show great promise in improving our predictive accuracy since certain tumour biological subtypes and tumour proteins were associated with distant spread of breast cancer cells (Sihto et al. 2011).
Conclusion
A significant fraction of breast cancer patients experienced early metastasis to the bones and visceral organs. Our data emphasized that tumour stage, size and lymph node involvement are major predictors of distant metastasis. Lymphovascular invasion was a distinct predictor of bone metastasis while young age and premenopausal status were predictors exclusive to visceral metastasis. Estrogen and progesterone-receptor positive tumours have independently favourable prognosis. Her-2/neu over-expression alone is not a strong predictor of early metastasis but triple negative breast cancers belong to an aggressive subgroup with early metastatic capacity. Certain subgroups such as the young premenopausal patients as well as those with triple negative status may benefit from more aggressive work-up, treatment and surveillance thereafter. Likewise, early recognition of metastasis will allow rapid institution of effective palliative treatment. In this situation, for which the present study was relevant, a prediction model can be useful.
References
American Joint Committee on Cancer Staging Manual, 7th, Edge SB, Byrd DR, Compton CC, et al (Eds) (2010) S. Giordano. Update on Locally Advanced Breast Cancer. Springer, New York
Cardoso F, Fallowfield L, Costa A, Castiglione M, Senkus E (2011) Locally recurrent or metastatic breast cancer: ESMO clinical practice guidelines for diagnosis treatment and follow-up. Annal Oncol 22(suppl 6):vi25–vi30
Carlson R, Craig A, Anderson B, Burstein H, Carter WB, Edge S, Erban J et al (2012) Breast cancer. National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines in Oncology 7:122–129
Cianfrocca M, Goldstein LJ (2004) Prognostic and predictive factors in early stage breast cancer. Oncologist 9(6):606–616
Clark GM, Sledge GW, Osborne CK, McGuire WL (1987) Survival from first recurrence: relative importance of prognostic factors in 1,015 breast cancer patients. J Clin Oncol 5(1):55–61
Coleman RE, Smith P, Rubens RD (1998) Clinical course and prognostic factors following bone recurrence from breast cancer. Brit J Cancer 77(2):336–340
De Vita V, Lawrence T, Rosenberg S. De Vita (2008) Hellman and rosenberg’s cancer: principles and practice of oncology, 8th Ed.
Diel IJ, Solomayer EF, Costa SD, Gollan C, Goerner R, Wallwiener D, Kauffmann M, Bastert G (1998) Reduction in new metastases in breast cancer with adjuvant clodronate treatment. N Engl J Med 339(6):357–363
El Saghir NS, Adebamowo CA, Anderson BO, Carlson RW, Bird PA, Corbex M, Badwe RA, Bushnaq MA (2011) Breast cancer management in low resource countries (LRCs): consensus statement from the breast health global initiative. The Breast 20:S3–S11
Gajdos C, Tartter PI, Bleiweiss IJ (1999) Lymphatic invasion, tumor size, and age are independent predictors of axillary lymph node metastases in women with T1 breast cancers. Ann Surg 230:692–696
Gennari A, Conte P, Rosso R, Orlandini C, Bruzzi P (2005) Survival of metastatic breast carcinoma patients over a 20-year period: a retrospective analysis based on individual patient data from six consecutive studies. Cancer 104(8):1742
Giordano SH (2003) Update on locally advanced breast cancer. Oncologist 8:521
Gluck S (2007) Importance of distant metastasis and its impact on survival rates on early stage hormone receptor positive breast cancer. US Oncol Dis 1(1):22–25
Jensen A, Jacobsen J, Norgaard M, Yong M, Fryzek J, Sorensen H (2011) Incidence of bone metastases and skeletal-related events in breast cancer patients: a population-based cohort study in Denmark. BioMed Cent 11:29
Kuru B, Camlibel M, Dinc S, Gulcelik MA, Gonollu D, Alagol H (2008) Prognostic factors for survival in breast cancer patients who developed distant metastasis subsequent to definitive surgery. Singap Med J 49(11):904
Ngelangel CA, Wang EHM (2002) Cancer in the Philippine Cancer Control Program Japanese. J Clin Oncol 32(suppl 1):S52–S61
Ossovskaya V, Wang Y, Budoff A, Xu Q, Lituev A, Potapova O, Vansant G, Monforte J, Darasella N (2011) Exploring molecular pathways of triple negative breast cancer. Genes Cancer 2(9):870–879
Popoola AO, Ibrahim NA, Omodele FO, Oludara MA, Adebowale SA, Igwilo AI (2012) Pattern of spread of breast cancer among patients attending cancer unit of Lagos State University Teaching Hospital. Asian J Med Sci 4(3):89–94
Rabinovitch R, Kavanagh B (2009) Double helix of breast cancer therapy: intertwining the Halsted and Fisher Hypotheses. J Clin Oncol. Vol. 27. No. 15
Sihto H, Lundin J, Lundin M, Lehtimaki T, Ristimaki A, Holli K, Sallas L, Kataja et al (2011) Breast cancer biological subtypes and protein expression predict for the preferential distant metastasis: a nationwide cohort. Breast Cancer Res 13:R87
Solomayer EF, Diel JJ, Meyberg GC, Gollan C, Basterg G (2000) Metastatic breast cancer: clinical course, prognosis and therapy related to the first site of metastasis. Breast Cancer Res Treat 59(3):271–278
Yau C, Esserman L, Moore DH, Waldman F, Sninsky J, Benz CC (2010) Multigene predictor of metastatic outcome in early stage hormone receptor negative and triple negative breast cancer. Breast Cancer Res 12(5):R85
Conflict of interest
We certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rosa Mendoza, E.S., Moreno, E. & Caguioa, P.B. Predictors of early distant metastasis in women with breast cancer. J Cancer Res Clin Oncol 139, 645–652 (2013). https://doi.org/10.1007/s00432-012-1367-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-012-1367-z