Abstract
Purpose
The aim of this study was to assess the prognostic factors of peripheral T-cell lymphoma, unspecified (PTCL-U).
Patients and methods
We retrospectively analyzed 30 cases fulfilling the criteria of PTCL-U defined by the World Health Organization classification. The patients were treated with 6–8 cycles of a CHOP or THP (pirarubicin)-COP regimen.
Results
A high serum sIL-2R level (≥2,000 U/ml) at onset was associated with a low complete remission rate. Patients with high sIL-2R had significantly lower survival rates (5 year, 15.1%) than those with low sIL-2R (<2,000 U/ml) (100%) (P < 0.005). Factors associated with worse overall survival in a univariate analysis were high sIL-2R (P < 0.005), high age (>60 years) (P < 0.05), poor performance status (P < 0.01) and poor international prognostic index (P < 0.05). No correlation was observed between sIL-2R and other markers. Multivariate analysis showed that only sIL-2R was a prognostic factor for overall survival (P < 0.01).
Conclusion
The results suggest that a high serum sIL-2R level predicts a poor prognosis in PTCL-U.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Peripheral T-cell lymphoma, unspecified (PTCL-U) is characterized by disseminated disease, with systemic symptoms, bone marrow involvement, and extranodal disease. Although high-dose sequential chemotherapy followed by autologous hematopoietic stem cell transplantation (ASCT) has been successful (Zaja et al. 1997; Haioun et al. 1997), Zaja et al. (1997) have shown there is no benefit of ASCT in a subset of PTCL-U.
Many investigators have examined prognostic factors in non-Hodgkin’s lymphoma (NHL), of which the International Prognostic Index (IPI) (The International Non-Hodgkin’s Lymphoma Prognostic Factors Project 1993), based on patient characteristics directly associated with their condition, is the most reliable and well known. Examination of prognostic factors is extremely important in attempting patient stratification. We have previously reported that serum concentrations of soluble Fas (sFas) (Hara et al. 2000), soluble tumor necrosis factor receptor 2 (Goto et al. 2006), and soluble interleukin-2 receptor (sIL-2R) (Goto et al. 2005) predict the clinical outcome of patients with aggressive NHL. These analyses were mainly for diffuse large B-cell lymphoma (DLBCL). Here, we report the results of prognostic analysis using sIL-2R in patients with PTCL-U.
Patients and methods
Patient selection
We investigated all patients with PTCL diagnosed between January 1995 and December 2006. To be eligible for this study, patients needed a histologically confirmed diagnosis of PTCL-U, according to the World Health Organization classification (Harris et al. 1999), with T-cell phenotype proven either by flow cytometry or immunohistochemistry. A complete set of clinical data for an accurate clinical staging was also required for inclusion. A simple set of clinical data including age, sex, complete blood count, serum lactate dehydrogenase (LDH) level, serum sIL-2R level, Ann Arbor stage, international prognostic index (IPI), prognostic index for PTCL-U (PIT) (Gallamini et al. 2004), number and sites of extranodal disease, bone marrow (BM) involvement, systemic symptoms (B symptoms), bulky disease, performance status (PS), date of diagnosis, type of treatment, response to therapy, date of assessment of response, date of relapse, date of and status at last follow-up, and, if deceased, date and cause of death was collected. Bulky disease was defined as a mediastinal mass with a maximum diameter greater than one-third of the maximum chest diameter or any other mass at least 10 cm in diameter. B symptoms were defined, according to Ann Arbor criteria, as recurrent fever (>38°C), night sweats, or loss of more than 10% of body weight.
Treatment strategies
Patients aged under 70 were assigned to receive eight cycles of CHOP or THP-COP therapy (Tsurumi et al. 2004). Each regimen consisted of cyclophosphamide (CPA: 750 mg/m2, given as a 2-h intravenous drip infusion on day 1), doxorubicin (DOX) or tetrahydropyranyl-adriamycin (THP: 50 mg/m2, given as a 30-min intravenous drip infusion on day 1), vincristine [VCR: 1.4 mg/m2 (maximum dose 2.0 mg), given intravenously in a bolus over 5 min on day 1], and prednisolone (PSL: 100 mg daily, given orally on days 1–5). THP, an anthracyclin derivative of DOX with reportedly lower cardiotoxicity (Miller and Salewski 1994; Takagi and Oguro 1987), was used instead of DOX in the THP-COP regimen. No significant differences were observed for remission rate and survival between CHOP and THP-COP therapy in our prospective randomized study (Tsurumi et al. 2004). Patients aged 70 and over were assigned to receive six cycles of THP-COP therapy, which is often used for elderly NHL patients (Tsurumi et al. 2007). The regimen consisted of CPA (650 mg/m2, given as a 2-h intravenous drip infusion on day 1), THP (40 mg/m2, given as a 30-min intravenous drip infusion on day 1), VCR [1.4 mg/m2 (maximum dose 2.0 mg), given intravenously in a bolus over 5-min on day 1], and PSL (40 mg daily, given orally on days 1–5). Granulocyte colony-stimulating factor (G-CSF) was administered subcutaneously at 2 μg/kg from day 7 until recovery from neutropenia, where necessary. The CHOP and THP-COP chemotherapy cycles were repeated at 14-day intervals in patients aged under 70, and the THP-COP chemotherapy cycles were repeated at 21-day intervals in patients aged 70 and over. Patients with a bulky mass received radiotherapy ranging from 30 to 40 Gy after chemotherapy. Upfront high-dose chemotherapy followed by ASCT was performed in six cases after complete remission (CR) was achieved.
Patients who relapsed or had disease progression after CHOP or THP-COP, and patients who were resistant to CHOP or THP-COP, received the P-IMVP-16/CBDCA regimen (Sawada et al. 2002) (consisting of methylprednisolone, ifosfamide, methotrexate, etoposide, and carboplatin) second line. Patients aged under 70 with refractory or relapsed NHL who responded to P-IMVP-16/CBDCA received high-dose chemotherapy followed by ASCT.
Response criteria
Tumor response to chemotherapy was evaluated after the second, fourth, sixth, and final courses of chemotherapy. Therapy was considered to have failed at those time points for tumors that showed progressive disease. Response to treatment was categorized using repeated physical examination, radiological studies, gallium scintigraphy, fluorodeoxyglucose-positron emission tomography (FDG-PET) and bone-marrow aspiration, according to the response criteria defined by Cheson et al. (1999).
Statistical analyses
Data are expressed as medians and range. Differences in median values were tested using the nonparametric Mann–Whitney U-test. OS was measured from the time of initiation of chemotherapy until death from any cause. Univariate analyses of several pretreatment characteristics for their effect on attaining CR were performed using the chi-squared test. Univariate analyses of several pretreatment characteristics including sIL-2R for their effect on survival were performed using the log-rank test based on the method of Kaplan and Meier. Multivariate analysis was performed using the Cox’s proportional-hazards regression technique to define the prognostic significance of selected covariates including sIL-2R. P-values < 0.05 were taken to indicate significance. All follow-up data were updated on 1 December 2007.
Results
Characteristics of enrolled patients
We recruited a consecutive series of 30 patients with previously untreated PTCL-U. The characteristics of the patients at entry are summarized in Table 1. The median age was 59 years (range 14–79 years), and the male-to-female ratio was 23:7. Bulky disease was present in four patients (13.3%). Nearly half of the patients presented with B symptoms (13 of 30, 43.3%). LDH levels were elevated in 22 patients (73.3%). IPI scoring was available in all patients, five (16.7%) were classified as low risk (L), ten (33.3%) as low-intermediate (LI), six (20.0%) as high-intermediate (HI), and nine (30.0%) as high risk (H). According to PIT, 4 (13.3%) were classified as group 1 (no adverse factors), 14 (46.7%) as group 2 (1 factor), 6 (20.0%) as group 3 (2 factors), and 6 (20.0%) as group 4 (3 factors or more).
Serum sIL-2R levels at entry
The median serum sIL-2R level (all patients) was 2,801 U/ml (range 176–80,450) (Table 1). Various poor prognostic features, such as age over 60 years, sex, poor PS, elevated LDH, and extranodal sites were not associated with serum sIL-2R level (Table 1). Advanced disease (CS III/IV) was related significantly with a high serum sIL-2R level (P < 0.05) (Table 1). The median (range) serum sIL-2R levels of the different IPI risk groups were as follows: 367 (176–3,400) U/ml for the L risk group, 2,701 (423–72,800) U/ml for the LI risk group, 4,076 (570–58,900) U/ml for the HI risk group, and 11,050 (2,398–80,450) U/ml for the H risk group (P overall < 0.001) (Table 1).
Analysis of response
Overall, the CR rate was 70.0% (21 of 30); partial responses were observed in 6.7% of patients (2 of 30) and failures in 23.3% (7 of 30). The patients were divided into two groups by sIL-2R level using a cut-off value of 2,000 U/ml, which was almost the median sIL-2R level in these patients and is the value we also used in a previous report (Goto et al. 2005). The CR rate was significantly worse in patients with a sIL-2R level of ≥2,000 U/ml (P < 0.01) (Table 2). There was no significant difference in CR rate between PIT group 1 or 2 and PIT group 3 or 4 (Table 2).
Treatment regimens
Seven cases were treated with the CHOP regimen, and 19 with the THP-COP regimen. The CR rates with CHOP and THP-COP were 85.7 and 73.7%, respectively, and the 5-year OS rates were 41.7 and 63.4%. There was no significant difference in CR rate and OS between the two regimens. ASCT was performed in ten cases after CR was achieved, and the 5-year OS rates of patients treated with and without ASCT were 33.3 and 37.6%, respectively.
Univariate analyses for the effects of various factors on overall survival
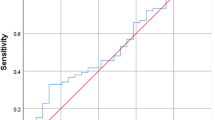
After a mean follow-up of 137 months, 12 (40.0%) of 30 patients had died, and the cumulative probability of survival at 5 years was 42.1% (Table 2; Fig. 1). The OS rate was significantly worse in patients aged over 60 years (P < 0.05), poor PS (>1) (P < 0.01) or unfavorable IPI (HI and H risk groups) (P < 0.05) (Table 2; Fig. 2). The 5-year OS rates for patients with sIL-2R levels of <2,000 and ≥2,000 U/ml were 100 and 15.1%, respectively (P < 0.005) (Table 2; Fig. 3). PIT also reflected the overall survival of PTCL-U, when we divided he patients into favorable (group 1 or 2) and unfavorable groups (group 3 or 4) (P < 0.005) (Table 2).
Multivariate analyses on overall survival
Multivariate analyses demonstrated that only high serum sIL-2R was an independent prognostic factor for OS (P < 0.01).
Discussion
PTCL is a heterogeneous group of neoplasms presenting as an advanced disease characterized by widespread dissemination, aggressive behavior, and a very poor outcome. For treatment selection, discrimination of risk groups needs to be clarified, and the IPI is now considered to be the most reliable index. In a good agreement with previous studies using IPI, the OS rates of the L and LI groups was better than that of the HI and H groups, also in our results.
In recent years, intensive chemotherapies for the treatment of NHL, including hematopoietic stem cell transplantation (HSCT), have been investigated. Some of these therapies have been shown to have better outcomes in some populations of NHL. Although the utility of HSCT for PTCL has not been established, the HI and H groups have been thought to be suitable for HSCT in aggressive NHL in the first CR (Haioun et al. 1997; Shipp et al. 1999).
The IPI is based on patient characteristics directly associated with their condition, such as age and PS, and variables indirectly reflecting tumor biology such as CS, LDH, and extranodal sites. Thus, examination of biological prognostic factors has recently been the focus of research. For instance, in patients with aggressive NHL, Ichikawa et al. (1997) reported that the p53 mutation was associated with a poor prognosis, and Niitsu et al. (1999, 2001, 2003) reported that the nm23-HI protein was also associated with prognosis. Moreover, many prognostic factors such as CRP (Legouffe et al. 1998), basic fibroblast growth factor (Salven et al. 1999), IL-6 (Preti et al. 1997), IL-10 (Stasi et al. 1994), soluble CD44 variant 6 (Sasaki and Niitsu 2000), and survivin (Adida et al. 2000) have also been investigated. Most previous studies comparing outcomes between patients with PTCL and patients with DLBCL have been limited by the heterogeneity encountered within each disease category (Gisselbrecht et al. 1998). There are many differences between PTCL-U and DLBCL, and the clinical difference between B-cell and T-cell lymphoma becomes more clearly after the introduction of rituximab to treat B-cell lymphoma. Therefore, it is necessary to examine the prognostic factors in PTCL separately from DLBCL, since prediction of prognosis is necessary to select the most appropriate treatment.
Gallamini et al. (2004) proposed PIT as a prognostic model for PTCL-U, but as indicated in Table 2, we found that PIT did not affect remission rate. When we divided the patients into two, i.e., favorable and unfavorable, groups based on PIT, it reflected the overall survival of PTCL-U, but a significant difference was not seen among four groups according to original PIT classification (data not shown). Based on these results, PIT appears to be a useful model for PTCL-U, but it is uncertain whether prognosis of PTCL-U can be predicted only with PIT.
Mature T cells produce IL-2 in response to stimulation by antigens and IL-2 promotes the growth of T cells bearing IL-2R (Robb 1982). Membrane-bound IL-2R is present on all normal activated T cells (Cantrell and Smith 1983). IL-2R consists of three chains: α, β, and γ. The α chain appears on the surface of the T cell when it is activated, separates from the cell, and exists as a soluble form in the serum. It has been demonstrated that IL-2R is released from the cell surface in a soluble form (sIL-2R) under particular conditions in vitro and in vivo (Rubin et al. 1985). High serum levels of sIL-2R have been demonstrated in several diseases (Rubin et al. 1985; Ogata et al. 1996; Wasik et al. 1996). The sIL-2R molecules can bind to IL-2, although it is not known whether malignant or normal activated T cells produce sIL-2R, both cell types have the capacity to release sIL-2R into the serum. In vivo, sIL-2R might be produced by normal lymphoid cells responding to stimulation by malignant cells, which we believe is a likely process in B cell lymphoma. Activated T cells produce sIL-2R in B cell lymphoma. Similarly, it is thought that both activated T cells and lymphoma cells produce sIL-2R in PTCL-U. Therefore, sIL-2R reflects the prognosis more clearly in patients with PTCL-U than those with DLBCL.
Soluble IL-2R can be measured quickly and easily using ELISA. It decreased when the treatment succeeded and when CR was achieved in patients with high serum sIL-2R at onset, and increased again at relapse (data not shown). Thus, the sIL-2R level correlates with the condition of lymphoma, and also reflects the activity of PTCL-U. Although the number of patients in our study was too small to be meaningful, sIL-2R clearly reflects the prognosis of PTCL-U. Thus, it should be used as a biological prognostic factor alongside IPI in stratification of patients with PTCL-U.
THP is reported to be particularly effective for T-cell lymphoma. However, our study showed no significant differences between CHOP and THP-COP in CR rate and OS. In addition, we could not demonstrate a benefit for upfront auto PBSCT when the patient achieved first CR. This study is not a randomized trial, so we have to consider the bias of each case and further studies, in particular randomized trials, should be considered. In conclusion, although we have to consider the modification of activating T cells by such factors as viral infection, serum sIL-2R is a useful as a significant prognostic factor for PTCL-U. The most reliable prognostic factor and the best combination of prognostic factors for aggressive NHL should be further clarified in order to facilitate selection of appropriate treatment.
References
Adida C, Haioun C, Gaulard P, Lepage E, Morel P, Briere J et al (2000) Prognostic significance of survivin expression in diffuse large B-cell lymphomas. Blood 96:1921–1925
Cantrell DA, Smith KA (1983) Transient expression of interleukin 2 receptors. Consequences for T cell growth. J Exp Med 158:1895–1911. doi:10.1084/jem.158.6.1895
Cheson BD, Horning SJ, Coiffier B, Shipp MA, Fisher RI, Connors JM et al (1999) Report of an international workshop to standardize response criteria for non-Hodgkin’s lymphomas. NCI Sponsored International Working Group. J Clin Oncol 17:1244–1253
Gallamini A, Stelitano C, Calvi R, Bellei M, Mattei D, Vitolo U, Morabito F, Martelli M, Brusamolino E, Iannitto E, Zaja F, Cortelazzo S, Rigacci L, Devizzi L, Todeschini G, Santini G, Brugiatelli M, Federico M (2004) Intergruppo Italiano Linfomi. Peripheral T-cell lymphoma unspecified (PTCL-U): a new prognostic model from a retrospective multicentric clinical study. Blood 103:2474–2479. doi:10.1182/blood-2003-09-3080
Gisselbrecht C, Gaulard P, Lepage E, Coiffier B, Brière J, Haioun C et al (1998) Prognostic significance of T-cell phenotype in aggressive non-Hodgkin’s lymphomas. Groupe d’Etudes des Lymphomes de l’Adulte (GELA). Blood 92:76–82
Goto H, Tsurumi H, Takemura M, Ino-Shimomura Y, Kasahara S, Sawada M et al (2005) Serum-soluble interleukin-2 receptor (sIL-2R) level determines clinical outcome in patients with aggressive non-Hodgkin’s lymphoma: in combination with the International Prognostic Index. J Cancer Res Clin Oncol 131:73–79. doi:10.1007/s00432-004-0600-9
Goto N, Tsurumi H, Takemura M, Hara T, Sawada M, Kasahara S et al (2006) Serum-soluble tumor necrosis factor receptor 2 (sTNF-R2) level determines clinical outcome in patients with aggressive non-Hodgkin’s lymphoma. Eur J Haematol 77:217–225. doi:10.1111/j.1600-0609.2006.00702.x
Haioun C, Lepage E, Gisselbrecht C, Bastion Y, Coiffier B, Brice P et al (1997) Benefit of autologous bone marrow transplantation over sequential chemotherapy in poor-risk aggressive non-Hodgkin’s lymphoma: updated results of the prospective study LNH87–2. Groupe d’Etude des Lymphomes de l’Adulte. J Clin Oncol 15:1131–1137
Hara T, Tsurumi H, Takemura M, Goto H, Yamada T, Sawada M et al (2000) Serum-soluble fas level determines clinical symptoms and outcome of patients with aggressive non-Hodgkin’s lymphoma. Am J Hematol 64:257–261. doi:10.1002/1096-8652(200008)64:4<257::AID-AJH4>3.0.CO;2-2
Harris NL, Jaffe ES, Diebold J, Flandrin G, Muller-Hermelink HK, Vardiman J et al (1999) World Health Organization classification of neoplastic diseases of the hematopoietic and lymphoid tissues: report of the Clinical Advisory Committee meeting-Airlie House, Virginia, November 1997. J Clin Oncol 17:3835–3849
Ichikawa A, Kinoshita T, Watanabe T, Kato H, Nagai H, Tsushita K et al (1997) Mutations of the p53 gene as a prognostic factor in aggressive B-cell lymphoma. N Engl J Med 337:529–534. doi:10.1056/NEJM199708213370804
Legouffe E, Rodriguez C, Picot MC, Richard B, Klein B, Rossi JF et al (1998) C-reactive protein serum level is a valuable and simple prognostic marker in non Hodgkin’s lymphoma. Leuk Lymphoma 31:351–357
Miller AA, Salewski E (1994) Prospects for pirarubicin. Med Pediatr Oncol 22:261–268. doi:10.1002/mpo.2950220410
Niitsu N, Okabe-Kado J, Kasukabe T, Yamamoto-Yamaguchi Y, Umeda M, Honma Y (1999) Prognostic implications of the differentiation inhibitory factor nm23-H1 protein in the plasma of aggressive non-Hodgkin’s lymphoma. Blood 94:3541–3550
Niitsu N, Okamoto M, Okabe-Kado J, Takagi T, Yoshida T, Aoki S et al (2001) Serum nm23-H1 protein as a prognostic factor in aggressive non-Hodgkin lymphoma. Blood 97:1202–1210. doi:10.1182/blood.V97.5.1202
Niitsu N, Honma Y, Iijima K, Takagi T, Higashihara M, Sawada U et al (2003) Clinical significance of nm23-H1 proteins expressed on cell surface in non-Hodgkin’s lymphoma. Leukemia 17:196–202. doi:10.1038/sj.leu.2402699
Ogata K, Yokose N, An E, Kamikubo K, Tamura H, Dan K et al (1996) Plasma soluble interleukin-2 receptor level in patients with primary myelodysplastic syndromes: a relationship with disease subtype and clinical outcome. Br J Haematol 93:45–52. doi:10.1046/j.1365-2141.1996.4641003.x
Preti HA, Cabanillas F, Talpaz M, Tucker SL, Seymour JF, Kurzrock R (1997) Prognostic value of serum interleukin-6 in diffuse large-cell lymphoma. Ann Intern Med 127:186–194
Robb RJ (1982) Human T-cell growth factor: purification and interaction with a cellular receptor. Lymphokine Res 1:37–43
Rubin LA, Kurman CC, Fritz ME, Biddison WE, Boutin B, Yarchoan R et al (1985) Soluble interleukin 2 receptors are released from activated human lymphoid cells in vitro. J Immunol 135:3172–3177
Salven P, Teerenhovi L, Joensuu H (1999) A high pretreatment serum basic fibroblast growth factor concentration is an independent predictor of poor prognosis in non-Hodgkin’s lymphoma. Blood 94:3334–3339
Sasaki K, Niitsu N (2000) Elevated serum levels of soluble CD44 variant 6 are correlated with shorter survival in aggressive non-Hodgkin’s lymphoma. Eur J Haematol 65:195–202. doi:10.1034/j.1600-0609.2000.065003195.x
Sawada M, Tsurumi H, Yamada T, Hara T, Fukuno K, Goto H et al (2002) A prospective study of P-IMVP-16/CBDCA: a novel salvage chemotherapy for patients with aggressive non-Hodgkin’s lymphoma who had previously received CHOP therapy as first-line chemotherapy. Eur J Haematol 68:354–361. doi:10.1034/j.1600-0609.2002.01654.x
Shipp MA, Abeloff MD, Antman KH, Carroll G, Hagenbeek A, Loeffler M et al (1999) International consensus conference on high-dose therapy with hematopoietic stem cell transplantation in aggressive non-Hodgkin’s lymphomas: report of the jury. J Clin Oncol 17:423–429
Stasi R, Zinzani PL, Galieni P, Lauta VM, Damasio E, Dispensa E et al (1994) Prognostic value of serum IL-10 and soluble IL-2 receptor levels in aggressive non-Hodgkin’s lymphoma. Br J Haematol 88:770–777. doi:10.1111/j.1365-2141.1994.tb05116.x
Takagi T, Oguro M (1987) (2″-R)-4′-o-tetrahydropyranyladriamycin, a new anthracycline derivative; its effectiveness in lymphoid malignancies. Cancer Chemother Pharmacol 20:151–154. doi:10.1007/BF00253970
The International Non-Hodgkin’s Lymphoma Prognostic Factors Project (1993) A predictive model for aggressive non-Hodgkin’s lymphoma. N Engl J Med 329:987–994. doi:10.1056/NEJM199309303291402
Tsurumi H, Yamada T, Sawada M, Kasahara S, Kanemura N, Kojima Y et al (2004) Biweekly CHOP or THP-COP regimens in the treatment of newly diagnosed aggressive non-Hodgkin’s lymphoma. A comparison of doxorubicin and pirarubicin: a randomized phase II study. J Cancer Res Clin Oncol 130:107–113. doi:10.1007/s00432-003-0508-9
Tsurumi H, Hara T, Goto N, Kanemura N, Kasahara S, Sawada M et al (2007) A phase II study of a THP-COP regimen for the treatment of elderly patients aged 70 years or older with diffuse large B-cell lymphoma. Hematol Oncol 25:107–114. doi:10.1002/hon.815
Wasik MA, Vonderheid EC, Bigler RD, Marti R, Lessin SR, Polansky M et al (1996) Increased serum concentration of the soluble interleukin-2 receptor in cutaneous T-cell lymphoma. Clinical and prognostic implications. Arch Dermatol 132:42–47. doi:10.1001/archderm.132.1.42
Zaja F, Russo D, Silvestri F, Fanin R, Damiani D, Infanti L et al (1997) Retrospective analysis of 23 cases with peripheral T-cell lymphoma, unspecified: clinical characteristics and outcome. Haematologica 82:171–177
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kitagawa, Ji., Hara, T., Tsurumi, H. et al. Serum-soluble interleukin-2 receptor (sIL-2R) is an extremely strong prognostic factor for patients with peripheral T-cell lymphoma, unspecified (PTCL-U). J Cancer Res Clin Oncol 135, 53–59 (2009). https://doi.org/10.1007/s00432-008-0440-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-008-0440-0