Abstract
Purpose
The aim of the present study was to assess the prognostic significance of serum soluble interleukin-2 receptor (sIL-2R) in aggressive non-Hodgkin’s lymphoma (NHL).
Methods
One hundred and thirteen consecutive patients with previously untreated aggressive NHL (diffuse large B-cell lymphoma, 96; peripheral T-cell lymphoma, 17) prospectively participated in this study between 1995 and 2001. The patients were treated with 6–8 cycles of a CHOP or THP (pirarubicin)-COP regimen.
Results
A high serum sIL-2R level (2,000 U/ml and over) at onset was associated with a low complete remission rate. Patients with high sIL-2R had significantly lower survival rates (5-year, 24%) than those with low sIL-2R (under 2,000 U/ml) (74%) (P<0.01). Multivariate analysis employing sIL-2R levels and conventional prognostic factors demonstrated that high sIL-2R, presence of B-symptoms, and advanced age (60 years and older) were significantly unfavorable variables for overall survival. In addition, we attempted to use sIL-2R in combination with the International Prognostic Index (IPI). The patients in the high (H) risk group and those with high sIL-2R in the low-intermediate (LI)/high-intermediate (HI) risk group had significantly lower survival rates than the patients in the low (L) risk group and those with low sIL-2R in the LI/HI risk group (P<0.001).
Conclusion
The results suggest that a high serum sIL-2R level predicts a poor prognosis in aggressive NHL and may be a useful biomarker for selecting appropriate treatment when used in combination with the IPI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recently, many investigators have attempted to identify the prognostic factors in non-Hodgkin’s lymphoma (NHL) (Nicolaides et al. 1998). Age, performance status (PS), clinical stage (CS), serum lactate dehydrogenase (LDH) activity, and the number of extranodal lesions are recognized as conventional prognostic factors, and have been incorporated in the International Prognostic Index (IPI) for intermediate NHL (The International non-Hodgkin’s Lymphoma Prognostic Factors Project 1993). Some investigators have suggested that serum-soluble interleukin-2 receptor (sIL-2R) level may also be a prognostic factor for NHL (Niitsu et al. 2001; Kono et al. 2000). IL-2R is expressed not only on the surface of activated T or B lymphocytes, but also on parts of lymphoid malignancies. sIL-2R is released from the cell membrane by cleavage of IL-2R (Rubin et al. 1985; Rubin and Nelson 1990) and its the serum level rises in patients with some malignancies, including malignant lymphoma. In clinical practice, we attempt to devise a therapeutic plan according to expected prognosis, and thus need prognostic factors that can be used to categorize patients with aggressive NHL. Here, we examined whether serum sIL-2R evaluation would help to achieve this aim.
Prognostic factors often differ among clinical studies due to the use of different chemotherapeutic protocols. Accordingly, for prognostic analysis, uniform chemotherapy should be performed where possible. In the present study, we enrolled patients who underwent almost uniform chemotherapy, including a CHOP regimen consisting of cyclophosphamide (CPA), doxorubicin (DOX), vincristine (VCR), and prednisolone (PSL) or a THP-COP regimen consisting of CPA, pirarubicin (THP), VCR, and PSL (Kitamura and Takaku 1990; Tsurumi et al. 2003).
Materials and methods
Patients
We used a prospective, consecutive entry design. Between October 1995 and December 2001, previously untreated patients with aggressive NHL confirmed by biopsy participated in this study. Between 1995 and 2000 the histology of aggressive NHL was defined according to the Working-Formulation (The non-Hodgkin’s lymphoma pathologic classification project 1982), and thereafter it was reclassified based on the new WHO classification (Jaffe et al. 2001). Follicular large cell lymphoma, which is included in aggressive NHL, was excluded because rituximab became available for its treatment in Japan. Therefore, in the present study, no patient received rituximab. In addition, patients with human immunodeficiency virus or human T-cell lymphotropic virus type I were excluded. Clinical stage (CS) of the disease was evaluated according to the Ann Arbor classification (Carbone et al. 1971). Patients who did not receive chemotherapy due to any reason were also excluded. All patients gave written informed consent according to institutional guidelines and the Declaration of Helsinki.
Serum sIL-2R determination
To evaluate serum levels of sIL-2R, venous blood samples were drawn from patients immediately before the initiation of treatment. Serum sIL-2R was determined using a sandwich enzyme-linked immunosorbent assay (ELISA) kit (Cell-free Interleukin-2 Receptor Test Kit, T cell Science, Cambridge, Mass., USA) based on two monoclonal antibodies raised against two different epitopes of the p55 alpha-chain of the IL-2R complex, according to the manufacturer’s instructions
Treatment
Patients aged under 70 were assigned to receive eight cycles of CHOP or THP-COP therapy (Tsurumi et al. 2003). Each regimen consisted of CPA (750 mg/m2 on day 1), DOX or THP (50 mg/m2 on day 1), VCR [1.4 mg/m2 (maximal dose, 2.0 mg), on day 1], and PSL (100 mg, on days 1–5). THP, a derivative of DOX, is reportedly an anthracyclin with less cardiotoxicity than DOX (Miller and Salewski 1994; Takagi and Oguro 1987). THP was used instead of DOX in the THP-COP regimen. No significant difference was observed for remission rate and survival in our prospective randomized study between CHOP and THP-COP therapy (Tsurumi et al. 2003). Patients aged 70 and over were assigned to receive six cycles of THP-COP therapy, which is often used for elderly NHL patients (Kitamura and Takaku 1990). The regimen consisted of CPA (650 mg/m2 on day 1), THP (40 mg/m2 on day 1), VCR [1.4 mg/m2 (maximal dose, 2.0 mg) on day 1], and PSL (40 mg on days 1–5). The CHOP and THP-COP chemotherapy cycles were repeated at 14-day intervals in patients aged under 70, and the THP-COP chemotherapy cycles were repeated at 21-day intervals in elderly patients aged 70 and over, using granulocyte colony-stimulating factor (G-CSF). Patients with a bulky mass received radiotherapy ranging from 30 Gy to 40 Gy after chemotherapy. Patients who relapsed or had disease progression after CHOP or THP-COP, and patients who were resistant to CHOP or THP-COP received the P-IMVP-16/CBDCA regimen (Sawada et al. 2002), consisting of methylprednisolone, ifosfamide, methotrexate, etoposide, and carboplatin, as a second-line regimen. Some patients aged under 70 with refractory or relapsed NHL who responded to the P-IMVP-16/CBDCA received high-dose chemotherapy followed by autologous hematopoietic stem cell transplantation (HSCT).
Response criteria
After the completion of chemotherapy, response to treatment was categorized according to the International Workshop for NHL (Cheson et al. 1999). The disappearance of all disease evidence for at least 1 month qualified as complete remission (CR). Patients with residual masses were classified as uncertain CR (CRu), which denotes the disappearance of all disease apart from residual radiologic abnormalities (less than 25% of initial volume) of uncertain significance. A decrease in tumor mass by more than 50% for at least 1 month qualified as partial remission (PR). In this study, CRu was also included in CR.
Statistical analyses
Data are expressed as the median and range. Differences in median values were tested using the nonparametric Mann Whitney U-test (Stat View 4.01). Overall survival (OS) was measured from the time of chemotherapy until death from any cause. In patients who obtained CR, disease-free survival (DFS) was measured from the time of achievement of CR until relapse or death from any cause. Univariate analyses of several pretreatment features for their effect on attaining CR were performed using the chi-squared test. Univariate analyses of several pretreatment features including sIL-2R for their effect on survival were performed using the log-rank test based on the method of Kaplan and Meier (Kaplan and Meier 1958). Multivariate analysis was performed using Cox’s proportional-hazards regression technique to define the prognostic significance of selected covariates including sIL-2R (Cox 1972). P-values less than 0.05 were taken to indicate significance. All follow-up data were updated on 1 December 2002.
Results
Characteristics of enrolled patients with aggressive NHL and their serum sIL-2R levels
We measured serum sIL-2R levels (Table 1) in a consecutive series of 113 (69 males, 44 females; age, 14–92 years; median, 66 years) patients with aggressive NHL. Of these 113 patients, 96 had diffuse large B-cell lymphoma (DLBCL) and 17 had peripheral T-cell lymphoma (PTCL). The median of serum sIL-2R level in all patients was 1,748 U/ml (range 123–42,900). Various poor prognostic features, such as poor PS, an elevated LDH, extranodal sites, advanced disease (CS III/IV), existence of B-symptoms, and elevated CRP were strongly associated with high serum sIL-2R levels. The mean serum sIL-2R level of T-cell lymphoma (PTCL) was higher than that of B-cell lymphoma (DLBCL) (P<0.05). Neither sex, age, nor the existence of bulky mass was associated with serum sIL-2R levels. The median serum sIL-2R levels of the respective IPI risk group was as follows: 494 (range: 123–1,760) U/ml for the L risk group, 809 (181–7,620) U/ml for the LI risk group, 1,940 (459–17,120) U/ml for the HI risk group, and 7,694 (502–42,900) U/ml for the H risk group (P<0.001).
A cut-off value of serum sIL-2R
We determined an appropriate cut-off value of 2,000 U/ml to discriminate one group from another for OS and DFS. The value is nearest to the median sIL-2R level in all NHL patients.
Serum sIL-2R on achievement of CR
The CR rate of patients with sIL-2R levels of less than 2,000 U/ml and 2,000 U/ml and over was 85% and 64%, respectively (P<0.01) (Table 2). In addition, the CR rate was significantly worse in patients with aged 60 years and older, high serum LDH levels, poor PS (>1), many extranodal involvements (>1), unfavorable IPI (HI and H risk groups), B-symptoms, and high CRP levels (>3 mg/dl) (Table 2).
Univariate analyses for various factors on overall survival and disease-free survival
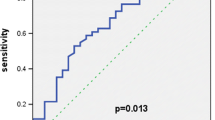
The 5-year OS rates for patients with sIL-2R levels of less than 2,000 U/ml and 2,000 U/ml and over were 74% and 24%, respectively (P<0.001), with respective DFS rates of 79% and 28% (P<0.01) (Fig. 1, Table 2). The OS rate was significantly worse in patients aged 60 years and older, poor PS (>1), high serum LDH levels, many extranodal involvements (>1), advanced CS (III, IV), unfavorable IPI (HI and H risk groups), B-symptoms, high CRP levels (>3 mg/dl), and no achievement of CR (Table 2). The DFS rate was significantly worse in patients with high serum LDH levels, many extranodal involvements (>1), advanced CS (III, IV), and unfavorable IPI (HI and H risk groups) (Table 2). Figure 2 shows the difference in OS and DFS according to IPI. Regarding OS, no significant difference was observed between the LI and HI group (Fig. 2a). As to DFS, no significant differences were observed among the LI, HI, and H group (Fig. 2b).
Combination of IPI and sIL-2R on survival
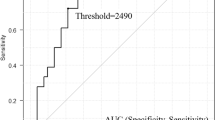
Risk categories of IPI were then divided into low and high sIL-2R groups (Table 3). The OS and DFS of high sIL-2R in the LI group were almost equivalent to those of high sIL-2R in the HI group. The OS and DFS of low sIL-2R in the LI group were also almost equivalent to those of low sIL-2R in the HI group. Thus, the LI and HI groups were combined and then divided into two groups; the low sIL-2R group and the high sIL-2R group. As shown in Fig. 3a, the OS of the L group and the OS of the low sIL-2R group in LI/HI were almost equivalent, while the OS of the high sIL-2R group in LI/HI and the OS of the H group were also almost equivalent. Hence, a strong significant difference was observed between the former (L and low sIL-2R group in LI/HI) and the latter (high sIL-2R group in LI/HI and H) (P<0.001) (Fig. 3b).
Overall survival curves for patients with aggressive non-Hodgkin’s lymphoma classified according to the combination of the International Prognostic Index (IPI) and serum sIL-2R level. The LI and HI risk groups were combined and then divided into two groups; the low sIL-2R group in LI/HI and the high sIL-2R group in LI/HI. Hence, the patients were classified into four groups; a the L risk group, the low sIL-2R group in LI/HI, the high sIL-2R group in LI/HI, and the H risk group. The former two groups and the latter two groups were combined, respectively, and all patients were then divided into two groups; the L and low sIL-2R group in LI/HI, and the H and high sIL-2R group in LI/HI. b Between the two groups, there was a strongly significant difference
Multivariate analyses on overall survival and disease-free survival
Multivariate analyses employing these factors demonstrated that high serum sIL-2R, presence of B-symptoms, and advanced age were independent prognostic factors for OS (sIL-2R: relative risk 3.2, 95% confidence interval 1.574–7.089, P=0.0011; B-symptoms: 2.0, 1.011–3.956, 0.0463; age: 2.0, 1.008–4.736, 0.0473,). High sIL-2R and advanced CS were independent prognostic factors for DFS (sIL-2R: relative risk 3.0, 95% confidence interval 1.685–5.523, P=0.0001; CS: 2.8, 1.105–4.559, 0.0208).
Discussion
In recent years, intensive chemotherapies for the treatment of NHL, including HSCT, have been investigated. Some of these therapies have been shown to yield a better outcome in some populations of NHL. However, in the low-risk group of patients with NHL, such intensive therapy might result in overtreatment. Therefore, discrimination of risk groups needs to be clarified. Under these circumstances, various studies on prognostic factors of NHL have been performed, and the IPI is now considered as the most reliable index. The HI and H groups have been thought to be suitable for HSCT in aggressive NHL in the first CR (Shipp et al. 1999; Haioun et al. 1997). However, even in the L and LI groups, the outcome of some patients is sometimes poor, whereas some patients in the HI and H groups sometimes have a good outcome. Thus, there may be no marked difference in prognosis of aggressive NHL between the LI and HI groups. At least , in our series, a significant difference was not observed between the LI and HI groups (Fig. 2). Thus, the IPI alone may not always be sufficient to categorize patients with aggressive NHL in order to determine the therapeutic strategy.
The IPI is based on patients’ characteristics directly associated with their condition, such as age and PS, and variables indirectly reflecting the tumor biology such as CS, LDH, and extranodal sites. Thus, the examination of biological prognostic factors has recently been focused on by many researches. For instance, in aggressive NHL patients, the p53 mutation, the nm23-HI protein, and serum soluble Fas level were associated with prognosis (Ichikawa et al. 1997; Niitsu et al. 1999; Hara et al. 2000). Moreover, many prognostic factors such as basic fibroblast growth factor (Salven et al. 1999), IL-6 (Preti et al. 1997), IL-10 (Stasi et al. 1994), soluble CD44 variant 6 (Sasaki and Niitsu 2000), and survivin (Adida et al. 2000) have also been investigated. In addition, using gene expression analysis with DNA microarrays, DLBCL was recently classified into the two different groups of germinal center B-like DLBCL and activated B-like DLBCL. When these two types were compared, the prognosis of activated B-like DLBCL was significantly worse (Alizadeh et al. 2000). Thus, in the future, prognostic analysis of NHL will be performed at the genomic level. However, a prediction of prognosis should be available prior to treatment in order to assist in selecting appropriate treatment. At the present time, it is important to ensure that these analyses can be performed quickly and easily.
Serum sIL-2R levels have been clinically investigated in a variety of human diseases such as myelodysplastic syndrome (Ogata et al. 1996), Hodgkin’s disease (Viviani et al. 1998), B-chronic lymphocytic leukemia (Semenzato et al. 1987), lymphoblastic lymphoma (Wagner et al. 1987), and adult T-cell leukemia/lymphoma (Yasuda et al. 1988).However, unexpectedly, there have been few prospective studies that have evaluated the prognostic significance of serum sIL-2R in adult aggressive NHL patients (Niitsu et al. 2001; Kono et al. 2000). In the present study, we showed that sIL-2R was closely associated with the prognosis of aggressive NHL. The indications of up-front HSCT for aggressive NHL in the first CR remain to be clarified. Here, in selecting the appropriate therapeutic strategy for aggressive NHL, we tried to make use of sIL-2R in combination with IPI. Our study showed that the OS of the L and the low sIL-2R group in the LI/HI group was significantly better than that of the H and the high sIL-2R group in the LI/HI group. The latter group is considered to be unfavorable, and might be a good indication of the need for high-dose chemotherapy with HSCT. Thus, the requirement for high-dose chemotherapy with HSCT might be well indicated in patients with high sIL-2R irrespective of IPI, and in H risk patients.
In conclusion, serum sIL-2R might be a significant prognostic factor for aggressive NHL and a useful tool for selecting the appropriate therapeutic strategy in patients with aggressive NHL. The most reliable prognostic factor and the best combination of some prognostic factors for aggressive NHL should be further clarified in order to assist in selection of appropriate treatment.
References
Adida C, Haioun C, Gaulard P, Lepage E, Morel P, Briere J, Dombret H, Reyes F, Diebold J, Gisselbrecht C, Salles G, Altieri DC, Molina TJ (2000) Prognostic significance of survivin expression in diffuse large B-cell lymphomas. Blood 96:1921–1925
Alizadeh AA, Eisen MB, Davis RE, Ma C, Lossos IS, Rosenwald A, Boldrick JC, Sabet H, Tran T, Yu X, Powell JI, Yang L, Marti GE, Moore T, Hudson Jr J, Lu L, Lewis DB, Tibshirani R, Sherlock G, Chan WC, Greiner TC, Weisenburger DD, Armitage JO, Warnke R, Levy R, Wilson W, Grever MR, Byrd JC, Botstein D, Brown PO, Staudt LM (2000) Distinct types of diffuse large B-cell lymphoma identified by gene expression profiling. Nature 403:503–511
Carbone PP, Kaplan HS, Musshoff K, Smithers DW, Tubiana M (1971) Report of the committee on Hodgkin’s disease staging classification. Cancer Res 31:1860–1861
Cheson BD, Horning SJ, Coiffier B, Shipp MA, Fisher RI, Connors JM, Lister TA, Vose J, Grillo-Lopez A, Hagenbeek A, Cabanillas F, Kippensten D, Hiddemann W, Castellino R, Harris NL, Armitage JO, Carter W, Hoppe R, Canellos GP (1999) Report of an International Workshop to standardize response criteria for non-Hodgkin’s lymphomas. J Clin Oncol 17:1244–1253
Cox DR (1972) Regression models and life-tables (with discussions). J R Stat Soc (Series B) 34:187–220
Haioun C, Lepage E, Gisselbrecht C, Bastion Y, Coiffier B, Brice P, Bosly A, Dupriez B, Nouvel C, Tilly H, Lederlin P, Biron P, Briere J, Gaulard P, Reyes F for the Group d’Etude des Lymphomes de I’Adulte (1997) Benefit of autologous bone marrow transplantation over sequential chemotherapy in poor-risk aggressive non-Hodgkin’s lymphoma: updated results of the prospective study LNH87–2. J Clin Oncol 15:1131–1137
Hara T, Tsurumi H, Takemura M, Goto H, Yamada T, Sawada M, Takahashi T, Moriwaki H (2000) Serum-soluble Fas level determines clinical symptoms and outcome of patients with aggressive non-Hodgkin’s lymphoma. Am J Hematol 64:257–261
Ichikawa A, Kinoshita T, Watanabe T, Kato H, Nagai H, Tsushita K, Saito H, Hotta T (1997) Mutation of the p53 gene as a prognostic factor in aggressive B-cell lymphoma. N Engl J Med 337:529–534
The International Non-Hodgkin’s Lymphoma Prognostic Factors Project (1993) A predictive model for aggressive non-Hodgkin’s lymphoma. N Engl J Med 329:987–994
Jaffe ES, Harris NL, Stein H, Vardiman JW, eds (2001) World health organization classification of tumors, pathology and genetics tumors of haematopoietic and lymphoid tissues. IARC, Lyon, 109–236
Kaplan EL, Meier P (1958) Non-parametric estimation from incomplete observations. J Am Stat Assoc 53:457–481
Kitamura K, Takaku F (1990) Pirarubicin, a novel derivative of doxorubicin. THP-COP therapy for non-Hodgkin’s lymphoma in the elderly. Am J Clin Oncol 13 [Suppl 1]:S15-S19
Kono N, Kanda Y, Yamamoto R, Chizuka A, Suguro M, Hamaki T, Arai C, Matsuyama T, Takezako N, Miwa A, Togawa A (2000) Prognostic significance of serum soluble interleukin-2 receptor level in non-Hodgkin’s lymphoma: a single center study in Japan. Leuk Lymphoma 37:151–156
Miller AA, Salewski E (1994) Prospects for pirarubicin. Med Pediatr Oncol 22:261–268
Nicolaides C, Dimou S, Pavlidis N (1998) Prognostic factors in aggressive non-Hodgkin’s lymphomas. Oncologist 3:189–197
Niitsu N, Okabe-Kado J, Kasukabe T, Yamamoto-Yamaguchi Y, Umeda M, Honma Y (1999) Prognostic implications of the differentiation inhibitory factor nm23-H1 protein in the plasma of aggressive non-Hodgkin’s lymphoma. Blood 94:3541–3550
Niitsu N, Iijima K, Chizuka A (2001) A high serum-soluble interleukin-2 receptor level is associated with a poor outcome of aggressive non-Hodgkin’s lymphoma. Eur J Haematol 66:24–30
The non-Hodgkin’s lymphoma pathologic classification project (1982) National Cancer Institute-sponsored study of classifications of non-Hodgkin’s lymphomas. Summary and description of a working formulation for clinical usage. Cancer 49:2112–2135
Ogata K, Yokose N, An E, Kamikubo K, Tamura H, Dan K, Sakamaki H, Onozawa Y, Hamaguchi H, Nomura T (1996) Plasma soluble interleukin-2 receptor level in patients with primary myelodysplastic syndrome: a relationship with disease subtype and clinical outcome. Brit J Haematol 93:45–52
Preti HA, Cabanillas F, Talpaz M, Tucker SL, Seymour JF, Kurzrock R (1997) Prognostic value of serum interleukin-6 in diffuse large-cell lymphoma. Ann Intern Med 127:186–194
Rubin LA, Kurman CC, Fritz ME, Biddison WE, Boutin B, Yarchoan R, Nelson DL (1985) Soluble interleukin 2 receptors are released from activated human lymphoid cells in vitro. J Immunol 135:3172–3177
Rubin LA, Nelson DL (1990) The soluble interleukin-2 receptor: biology, function, and clinical application. Ann Intern Med 113:619–627
Salven P, Teerenhovi L, Joensuu H (1999) A high pretreatment serum basic fibroblast growth factor concentration is an independent predictor of poor prognosis in non-Hodgkin’s lymphoma. Blood 94:3334–3339
Sasaki K, Niitsu N (2000) Elevated serum levels of soluble CD44 variant 6 are correlated with shorter survival in aggressive non-Hodgkin’s lymphoma. Eur J Haematol 65:195–202
Sawada M, Tsurumi H, Yamada T, Hara T, Fukuno K, Goto H, Shimizu M, Kasahara S, Yoshikawa T, Kanemura N, Oyama M, Takami T, Moriwaki H (2002) A prospective study of P-IMVP-16/CBDCA: a novel salvage chemotherapy for patients with aggressive non-Hodgkin’s lymphoma who previously received CHOP therapy as first-line chemotherapy. Eur J Haematol 68:354–361
Semenzato G, Foa R, Agostini C, Zambello R, Trentin L, Vinante F, Benedetti F, Chilosi M, Pizzolo G (1987) High serum levels of soluble interleukin-2 receptor in patients with B chronic lymphocytic leukemia. Blood 70:396–400
Shipp MA, Abeloff MD, Antman KH, Carroll G, Hagenbeek A, Loeffler M, Montserrat E, Radford JA, Salles G, Schmitz N, Symann M, Armitage JO, Philip T, Coiffier B (1999) International consensus conference on high-dose therapy with hematopoietic stem cell transplantation in aggressive non-Hodgkin’s lymphoma: Report of the July. J Clin Oncol 17:423–429
Stasi R, Zinzani PL, Galieni P, Lauta VM, Damasio E, Dispensa E, Dammacco F, Papa G, Tura S (1994) Prognostic value of serum IL-10 and soluble IL-2 receptor levels in aggressive non-Hodgkin’s lymphoma. Brit J Haematol 88:770–777
Takagi T, Oguro M (1987) (2”-R)-4’-o-Tetrahydropyranyladriamycin, a new anthracyclin derivative; its effectiveness in lymphoid malignancies. Cancer Chemother Pharmacol 20:151–154
Tsurumi H, Yamada T, Sawada M, Kasahara S, Kanemura N, Kojima Y, Fukuno K, Hara T, Saio M, Takahashi T, Oyama M, Ozawa K, Takami T, Moriwaki H (2004) Biweekly CHOP or biweekly THP-COP regimens in the treatment of aggressive non-Hodgkin’s lymphoma: a comparison of doxorubicin and pirarubicin: a randomized phase II study. J Cancer Res Clin Oncol 130:107–113
Viviani S, Camerini E, Bonfante V, Santoro A, Balzarotti M, Fornier M, Devizzi L, Verderio P, Valagussa P, Bonadonna G (1998) Soluble interleukin-2 receptors (sIL-2R) in Hodgkin’s disease: outcome and clinical implications. Brit J Cancer 77: 992–997
Wagner DK, Kiwanuka J, Edwards BK, Rubin LA, Nelson DL, Magrath IT (1987) Soluble interleukin-2 receptor levels in patients with undifferentiated and lymphoblastic lymphomas: correlation with survival. J Clin Oncol 5:1262–1274
Yasuda N, Lai PK, Ip SH, Kung PC, Hinuma Y, Matsuoka M, Hattori T, Takatsuki K, Purtilo DT (1988) Soluble interleukin-2 receptors in sera of Japanese patients with adult T cell leukemia mark activity of disease. Blood 71:1021–1026
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Goto, H., Tsurumi, H., Takemura, M. et al. Serum-soluble interleukin-2 receptor (sIL-2R) level determines clinical outcome in patients with aggressive non-Hodgkin’s lymphoma: in combination with the International Prognostic Index. J Cancer Res Clin Oncol 131, 73–79 (2005). https://doi.org/10.1007/s00432-004-0600-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-004-0600-9