Abstract
Background
We recently found an elevation in the pre-operative peritoneal lavage carcinoembryonic antigen (CEA) level to be associated with an earlier detection of recurrent peritoneal dissemination and a poor prognosis.
Method
Two hundred and twenty-nine patients with gastric cancer were intraoperatively measured for tumor markers, CEA and CA125 based on peritoneal lavage using a chemiluminescent enzyme immunoassay.
Results
The patients were divided into four groups. (A) The peritoneal lavage CEA (−) CA125 (−) group (CEA < 0.4 ng/ml, CA125 < 200 ng/ml, n = 129); (B) the peritoneal lavage CEA (−) CA125 (+) group (CEA < 0.4 ng/ml, CA125 ≧ 200 ng/ml, n = 50); (C) the peritoneal lavage CEA (+) CA125 (−) group (CEA ≧ 0.4 ng/ml, CA125 < 200 ng/ml, n = 18); and (D) the peritoneal lavage CEA (+) CA125 (+) group (CEA ≧ 0.4 ng/ml, CA125 ≧ 200 ng/ml, n = 32). The 5-year survival of the patients in groups C and D was 40 and 26%, respectively, which was lower than that of the patients in any other group (group A, B; p < 0.0001). Recurrent sites were both peritoneal dissemination and lymph node/liver in group C, while those were only peritoneal dissemination in group D.
Conclusion
This combined analysis of these markers is therefore considered to be helpful method to accurately estimate the recurrent sites and prognosis for advanced gastric cancer patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Carcinoembryonic antigen (CEA) is the most commonly used tumor marker for gastric cancer, and the levels of CEA in peritoneal lavage have been reported to accurately predict peritoneal recurrence after a curative resection of gastric cancer (Asao et al. 1991). Serum CA 125, a sensitive tumor marker for ovarian cancer reported by Bast et al. (1981), has also been shown to be a sensitive marker for the peritoneal dissemination of gastric cancer (Nakata et al. 1998; Haga et al. 1986).
The sites of recurrence in patients following a curative resection of advanced gastric cancer are hematogenesis, peritoneal dissemination, lymph node metastasis, local recurrence and multiple recurrences (Maehara et al. 2000). In particular, over 50% patients who have recurrences recognized the tumor at the peritoneum. It is difficult to detect the recurrent peritoneal carcinomatosa in an early stage. It is therefore necessary to establish a more sensitive marker to detect micrometastasis from gastric cancer due to find recurrent patients at an earlier stage. In many patients with gastric cancer with marked serosal cancer invasion, microscopic peritoneal metastasis has already been established at the time of curative surgery (Kiyasu et al. 1981). Other investigators have reported that patients with gastrointestinal or gynecological malignant disease had an unfavorable prognosis if any free cancer cells are observed in the peritoneal cavity (Moore et al. 1961; Creasman and Rutledge 1971). An analysis of the pre-operative peritoneal lavage fluid thus appears to result in an improved accuracy for predicting of peritoneal metastasis, thus allowing patients at high risk of peritoneal recurrence to be identified pre-operatively. A pre-operative assay of peritoneal lavage is thus considered to be a reliable method for selecting patients at an earlier stage of the peritoneal dissemination for whom systemic chemotherapy can be expected to have a beneficial effect (Sugerbeker and Yonemura 2000; Fujimoto et al. 2002; Yu et al. 1998; Baba et al. 2003).
This study was carried out to examine the peritoneal lavage CEA and CA125 levels in gastric cancer patients with respect to the sites of tumor recurrence.
Materials and methods
Patients and assay of tumor markers
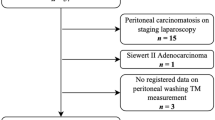
Two hundreds twenty-nine patients with gastric cancer who underwent a gastrectomy at National Kyushu Cancer Center were included in this study from April 1996 to March 2001. Immediately after performing a laparotomy, about 100 ml normal saline was administered into the Douglas pouch and then was collected for both a cytological examination and to measure for tumor markers (CEA, CA125). We selected two tumor markers, because we previously reported that CEA and CA125 in the peritoneal lavage were found to be independently related to peritoneal dissemination including CY(+) (Yamamoto et al. 2004). The preparation of samples and the judgments used the same method of the previous report (Yamamoto et al. 2004). The cutoff level for peritoneal lavage tumor markers was shown by a ROC curve in all patients. The cutoff level of CEA and CA125 in peritoneal lavage was 0.4 and 200 ng/ml, respectively. Previously, some investigators discussed the cutoff levels were set at levels divided actual levels for the peritoneal lavage tumor markers by serum protein levels (Asao et al. 1991; Nishiyama et al. 1995), however, we determined the actual levels for the peritoneal lavage tumor markers because the almost same results in our data were obtained when the cutoff level for the peritoneal lavage tumor markers was determined to be at levels divided actual levels by serum protein levels. All resected specimens were microscopically examined regarding the histologic type, the depth of invasion, lymphatic and vascular invasion, and lymph node metastasis according to the TNM Classification of the Stomach (UICC)-5th English Edition (Sobin and Wittekind 1997).
Follow-up
After being discharged from the hospital, all patients were followed up with both physical and blood examinations every 2 weeks and a combination of chest X-ray, computed tomography and ultrasonography of the abdomen every 3–6 months for the first year and then at intervals ranging from 6 to 12 months. The site of recurrence and causes of death were carefully investigated. In some cases, the mode of recurrence was determined by cytology, biopsy or surgery. The type of recurrence was classified as hepatic metastasis, peritoneal recurrence, lymph node recurrence or other types of recurrence. The median length of follow-up for the patients in this study was 58 months (ranging from 27 to 111 months).
Thirty-eight of 200 patients with curative operations had been treated as adjuvant chemotherapy with the oral administration of 5′-DFUR, 5-FU, UFT etc. Twenty of 29 patients with non-curative operations had been treated as the chemotherapy with the administration of TS-1, Irinotecan, Methotrexate/5-FU etc.
Statistical assessment
Non-parametric approximation was applied to estimate the cutoff levels. The non-parametric Mann–Whitney test was used for comparisons between the different groups. The long-rank test was used for comparisons of the survival rates. A finding of p < 0.05 was regarded as significant.
Results
Correlation of peritoneal lavage both CEA and CA125 levels
Figure 1 shows the distribution of the peritoneal lavage CEA and CA125 levels of the 229 patients; no correlations were observed among these peritoneal lavage tumor markers (r = 0.058).
Clinicopathological factors
The clinicopathological findings of the 229 patients are given in Table 1. The peritoneal lavage CEA (+) CA125 (+) group (group D) differed significantly from the peritoneal lavage CEA (−) CA125 (−) group (group A) regarding the following variables: stage (p < 0.0001), serosal invasion (p < 0.0001), lymph node metastasis (p < 0.001), lymphatic involvement (p < 0.001) and curability (p < 0.0001). The peritoneal lavage CEA (+) CA125 (+) group (group D) differs significantly from the peritoneal lavage CEA (−) CA125 (+) group (group B) regarding stage (p < 0.0001), serosal invasion (p < 0.0001), lymph node metastasis (p < 0.01), lymphatic involvement (p < 0.001), vascular involvement (p < 0.05) and curability (p < 0.0001). Group C and group D differed regarding curability (p < 0.01). In addition, the patients who were peritoneal lavage CEA (+) CA125 (+) group (Group D) tended to demonstrate more advanced cancer than the patients in other groups.
The different sites of the recurrent regions
Table 2 shows the recurrent sites of each group. Recurrence was recognized in 23 of the 32 patients (71.9%), and the recurrent site of all patients was only peritoneal dissemination in the peritoneal lavage CEA (+) CA125 (+) group (group D). Recurrence was recognized in 12 of the 18 patients (66.7%), and the recurrent sites in 6 of the 18 patients (33.3%) were peritoneal dissemination, while 6 of the 18 patients (33.3%) showed recurrence in the liver or lymph node etc. in the peritoneal lavage CEA (+) CA125 (−) group (group C). On the other hand, the recurrence rate was 16.0% (8 of 50 patients) in the peritoneal lavage CEA (−) CA125 (+) group (group B), and 11.6% (15 of 129 patients) in the peritoneal lavage CEA (−) CA125 (−) group (group A).
The survival rates
The mean follow-up time at the time of analysis was 5 years for the 156 patient survivors out of the total 229 patients. The post-operaive survival curve among the groups was also compared (Fig. 2). The 5-year survivals for patients in the peritoneal lavage CEA (+) group (group C and D) were worse than that of patients for the peritoneal lavage CEA (−) (groups A and B). In particular, the 5-year survival for patients in the peritoneal lavage CEA (+) CA125 (+) group (group D) was worse than that of patients for the peritoneal lavage CEA (+) CA125 (−) group (group C) (p < 0.0001).
Discussion
Carcinoembryonic antigen is a useful marker for both monitoring patients with gastrointestinal malignancies, and predicting recurrences (Maehara et al. 1990). Serum CA 125, a sensitive tumor marker for ovarian cancer reported by Bast et al. (1981), has also been shown to be a sensitive marker for the peritoneal dissemination in gastric cancer. An intraoperative peritoneal lavage cytological examination is important for predicting survival and peritoneal recurrence in gastric cancer (Moore et al. 1961). We recently demonstrated the sensitivity of the peritoneal lavage CEA level and CA125 for peritoneal dissemination including CY(+) (Yamamoto et al. 2004). This study demonstrated the recurrence sites and prognosis by the combined peritoneal lavage CEA and CA125 levels (Table 2).
The peritoneal lavage CEA and CA125 levels are a good screening method for predicting peritoneal dissemination including CY(+). As shown in Fig. 1, the distribution of these two markers did not correlated. As a result, there may be some difference in the characteristics of the tumors in patients with higher peritoneal lavage CEA levels and those with higher peritoneal lavage CA125 levels. Accordingly, we separated our patients into four groups—the peritoneal lavage CEA (−) CA125 (−) (group A), the peritoneal lavage CEA (−) CA125 (+) (group B), the peritoneal lavage CEA (+) CA125 (−) (group C) and the peritoneal lavage CEA (+) CA125 (+) (group D), so as to obtain a more precise assessment of the prognosis. In addition, only recurrent peritoneal dissemination was assumed to occur in group D, while recurrences including both peritoneal dissemination and lymph node metastasis etc. were seen in group C.
The 5-year survival for patients in group D was 26%, while that of the patients in the other group was 40% in group C (p < 0.0001), and the 5-year survival for patients in group B was 77%, while those in group A was 80%. The prognosis and recurrent regions between the peritoneal lavage CA125 (+) and (−) in cases of the peritoneal lavage CEA (−) were not differ, while there are the differences of the prognosis and recurrent regions between the peritoneal lavage CA125 (+) and (−) in cases of the peritoneal lavage CEA (+). In particular, the combination of two markers is useful to distinguish the differences of recurrent regions and the prognosis.
The higher specificity for free tumor cells indicates by the combination of higher peritoneal lavage CEA and CA125 than by peritoneal lavage CEA alone or CA125 alone. Though the presence of higher peritoneal lavage CEA and CA125 levels are thought to indicate the micrometastasis of peritoneal dissemination (group D), our data also recognized other metastasis, such as lymph node metastasis etc. (group C). Actually, histological types in gastric cancer determined the recurrence sites, most cases of undifferentiated adenocarcinoma lead to the peritoneal dissemination and differentiated adenocarcinoma lead to the liver and lymph node metastasis (Maehara et al. 2000). The reason for the occurrence of lymph node metastasis in patients with free tumor cells in the peritoneal lavage is unknown. We often encounter patients who have both peritoneal dissemination and lymph node metastasis (Yamamoto et al. 2006). The high levels of peritoneal lavege tumor markers may indicate free tumor cells originated from lymph nodes leading to the peritoneal dissemination (Rosenberg et al. 2002). The combination of peritoneal lavage CEA and CA125 levels thus help us to predict the sites of recurrence for all sites except for peritoneal dissemination.
As residual or occult tumor cells in gastric cancer may grow rapidly in the post-operative period, any delay in the ingestion of anti-cancer drugs may reduce the potential for controlling residual tumors (Gunduz et al. 1979; Schabel 1987). We made a multivariate analysis concerning curability, liver metastasis, peritoneal dissemination, serosal invasion, lymph node metastasis and found evidence for independent prognostic factors in gastric cancer patients (Maehara et al. 1991a, b). As these factors and peritoneal lavage CEA and CA125 levels can be determined at the time of surgery, we can perform the intensive chemotherapy at the intraoperative and early post-operation.
We thus concluded that the use of the combined peritoneal lavage CEA and CA125 assay is useful for determining the outcome of patients with gastric cancer. The administration of intensive chemotherapy and a close follow-up are recommended for such patients with high levels of peritoneal lavage tumor markers.
Abbreviations
- 1CEA:
-
Carcinoembryonic antigen
- 2CY(+):
-
Peritoneal lavage cytological positive
References
Asao T, Fukuda T, Yazawa S, Nagamachi Y (1991) Carcinoembryonic antigen levels in peritoneal washings can predict peritoneal recurrence after curative resection of gastric cancer. Cancer 68:44–47
Baba H, Yamamoto M, Endo K, Ikeda Y, Toh Y, Kohnoe S, Okamura T (2003) Clinical efficacy of S-1 combined with cisplatin for advanced gastric cancer. Gastric Cancer 6:45–49
Bast RC, Freeney M, Lazarus H, Nadler LM, Colvin RB, Knapp RC (1981) Reactivity of a monoclonal antibody with human ovarian carcinoma. J Clin Invest 68:1331–1337
Creasman WT, Rutledge F (1971) The prognostic value of peritoneal cytology in gynecological malignant disease. Am J Obestet Gynecol 110:773–781
Fujimoto T, Zhang B, Minami S, Wang X, Takahashi Y, Mai M (2002) Evaluation of intraoperative intraperitoneal cytology for advanced gastric cancer. Oncology 62:201–208
Gunduz N, Fisher B, Saffer EA (1979) Effect of surgical removal on the growth and kinetics of residual tumour. Cancer Res 39:3861–3865
Haga Y, Sakamoto K, Egami H, Yoshimura R, Mori K, Akagi M (1986) Clinical significance of serum CA125 value in patients with cancers of the digestive system. Am J Med Sci 292:30–34
Kiyasu Y, Kaneshima S, Koga S (1981) Morphogenesis of peritoneal metastasis in human gastric cancer. Cancer Res 41:1236–1239
Maehara Y, Sugimachi K, Akagi M, Kakegawa T, Shimuzu H, Tomita M (1990) Serum carcinoembryonic antigen level increase correlate with tumour progression in patients with differentiated gastric carcinoma following non-curative resection. Cancer Res 50:3952–3955
Maehara Y, Moriguchi S, Yoshida M, Takahashi I, Korenaga D, Sugimachi K (1991a) Splenectomy does not correlate with length of survival in patients undergoing curative total gastrectomy for gastric carcinoma. Cancer 67:3006–3009
Maehara Y, Moriguchi S, Kakeji Y, Orita H, Haraguchi M, Korenaga D, Sugimachi K (1991b) Prognostic factors in adeoncarcinoma in the upper third of the stomach. Surg Gynecl Obstet 173:223–226
Maehara Y, Hasuda S, Koga T, Tokunaga E, Kakeji Y, Sugimachi K (2000) Postoperative outcome and sites of recurrence in patients following curative resection of gastric cancer. Br J Surg 87:353–357
Moore GE, Sako K, Kondo T, Badillo J, Burke E (1961) Assessment of the exfoliation of tumour cells into the body cavities. Surg Gynecol Obestet 112:469–474
Nakata B, Hirakawa K, Kato Y, Yamashita Y, Maeda K, Onoda N, Sawada T, Sowa M (1998) Serum CA125 level as a predictor of peritoneal dissemination in patients with gastric carcinoma. Cancer 83:2488–2492
Nishiyama M, Takashima I, Tanaka T, Yoshida K, Toge T, Nagata N, Iwamori S, Tamura Y (1995) Carcinoembryonic antigen levels in the peritoneal cavity: useful gide to peritoneal recurrence and prognosis for gastric cancer. World J Surg 19:133–137
Rosenberg R, Hoos A, Mueller J, Baier P, Stricker D, Werner M, Nekarda H, Siewert JR (2002) Prognostic significance of cytokeratin-20 reverse transcriptase polymerase chain reaction in lymph nodes of node-negative colorectal cancer patients. J Clin Oncol 20:1049–1055
Schabel FM (1987) Concepts for systemic treatment of micrometastasis. Oncoloy 44:240–244
Sobin LH, Wittekind CH (1997) Internatinal Union Against Cancer: TNM classification of malignant tumors, 5th edn. Wiley-Liss, New York
Sugarbeker PH, Yonemura Y (2000) Clinical pathway for the management of resectable gastric cancer with peritoneal seeding: best palliation with a ray of hope of cure. Oncology 58:96–107
Yamamoto M, Baba H, Kakeji Y, Endo K, Ikeda Y, Toh Y, Kohnoe S, Okamura T, Maehara Y (2004) Prognostic significance of tumour markers in peritoneal lavage in advanced gastric cancer. Oncology 67:19–26
Yamamoto M, Taguchi K, Baba H, Endo K, Kohnoe S, Okamura T, Maehara Y (2006) The features of peritoneal dissemination with early gastric cancer. Surg Today 36(9):835–838
Yu W, Whang I, Suh I, Averbach A, Chang D, Sugerbaker PH (1998) Prospective randomized trial of early postoperative intraperitoneal chemotherapy as an adjuvant to resectable gastric cancer. Ann Surg 228:347–354
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yamamoto, M., Baba, H., Toh, Y. et al. Peritoneal lavage CEA/CA125 is a prognostic factor for gastric cancer patients. J Cancer Res Clin Oncol 133, 471–476 (2007). https://doi.org/10.1007/s00432-006-0189-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-006-0189-2