Abstract
Congenital diaphragmatic hernia (CDH) occurs in approximately 1 in 2500 to 5000 infants. The use of lung ultrasound (LUS) for its diagnosis has been reported in only two case reports. The aim of this study was to report the LUS pattern of CDH in a case series of infants with respiratory distress. This case series was part of a cohort enrolled in a larger prospective observational study. LUS was performed at the point-of-care during the first 24 h of life of the neonates and its operation time was measured. Seven cases (six left and one right CDH) were diagnosed. We found that the pattern of LUS for CDH diagnosis includes (1) partial absence of the hyperechoic line representing the normal diaphragmatic profile, (2) partial absence of the pleural line in the affected hemithorax, (3) absence of A lines in the affected area, (4) presence of multi-layered area with hyperechoic contents in motion (normal gut), and (5) possible presence of parenchymatous organs inside the thorax (i.e., liver or spleen).
Conclusion: A description of LUS pattern in infants with CDH is provided. LUS at the point-of-care may allow the prompt diagnosis of CDH and this is particularly useful in cases of missed prenatal diagnosis.
What is Known: | |
• Congenital diaphragmatic hernia occurs in approximately 1 in 2500 to 5000 infants but the use of lung ultrasound for its diagnosis has been reported in only two case reports. | |
What is New: | |
• Research provided a description of lung ultrasound pattern in infants with congenital diaphragmatic hernia. | |
• Lung ultrasound at the point-of-care may allow a prompt diagnosis of congenital diaphragmatic hernia, particularly useful in cases of missed prenatal diagnosis. |
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Congenital diaphragmatic hernia (CDH) occurs in approximately 1 in 2500 to 5000 newly born infants [7] with mortality rates as high as 30% [12]. Two main types of CDH can occur: Bochdalek (posterolateral) which is more frequent and Morgagni (anteromedial) hernias [3].
The ultrasonographic features of CDH during fetal life are widely described [8], but neonatal cases of CDH undetected in utero may happen. The fetal ultrasound detection rate reported in the literature is 60% [6].
Lung ultrasound (LUS) is a rapidly evolving technique in neonatology and increasing evidences are available on its use, both as a descriptive and functional application. [9]
The use of LUS at the point-of-care for the diagnosis of neonatal CDH has been reported in only two case reports performed in pediatric emergency departments [5, 10]. On the other hand, the use of LUS could be particularly useful for quick discovery of missed prenatal diagnosis due to its availability at infants’ bedside.
Thus, the aim of our study is to report a case series of LUS diagnosis of CDH in late-preterm and term infants with respiratory distress and document the ultrasound pattern of this pathology.
Methods
Study design and setting
This case series is part of the study population of a previous larger prospective observational study [4] on the diagnostic abilities of LUS in neonatal respiratory distress performed in the Neonatal Intensive Care Unit of Careggi University Hospital of Florence, from September 2015 to December 2016, after approval from the local Ethics Committee. The enrolling facility is one of the regional referral center for congenital disorders of neonates.
In the companion study, all eligible neonates admitted to the neonatal intensive care unit for respiratory distress during the first 24 h of life underwent chest x-ray (CXR) and LUS at the point-of-care. All enrolling neonatologist sonographers were blinded to any prenatal diagnosis and CXR results while performing LUS scan. LUS was performed with a Philips CX50 (Philips, Eindhoven, the Netherlands) ultrasound machine using a high-frequency (7–15 MHz) linear transducer with infants placed in a supine or lateral recumbent position to scan the anterior, lateral, and posterior chest walls and a curvilinear transducer (5–8 MHz) to explore the diaphragm. Images of longitudinal and transverse sections were obtained and recorded. Trans-abdominal scanning for lung bases was done by trans-hepatic and trans-splenic views. The subcostal view was also used to investigate the diaphragm.
CXRs were obtained in anterior-posterior view and lateral views were performed when required by neonatologists. CXR interpretation, diagnosis, and management decisions were up to senior neonatologists who were blinded to the results of the LUS exam and the prenatal diagnosis as per study protocol.
We compared the LUS findings of neonates with CDH with the LUS findings of all the neonates with respiratory distress enrolled in the companion study [4] with a different diagnosis than CDH and who served as a control group. Comparison was made using Fisher’s exact test.
The operation time for LUS, defined as the interval between the decision to perform the diagnostic test and the final report, was measured and compared to CXR operation time using Wilcoxon matched pairs test due to the non-normal data distribution.
Results
During the study period, we enrolled 124 preterm, late-preterm and term infants with respiratory distress. CDH was identified in 7/124 (6%) patients; six cases were of left CDH and one was a case of right CDH.
All described patients had a prenatal diagnosis of CDH but sonographers were blinded to the prenatal diagnosis. Demographics and clinical features of the patients are detailed in Table 1.
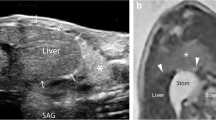
Figure 1 shows the images of a normal transverse scan of the abdomen with diaphragm profile and a normal LUS (panels a and b respectively).
Figure 2 presents the CXR and the LUS findings for cases of left and right CDH. All patients had similar ultrasound findings. It was possible to identify in the subcostal view the partial absence of part of the affected hemi-diaphragm (Fig. 2 panels b and e, left and right CDH respectively) which normally appears as a bright curved line that moves with respiration as shown in Fig. 1 panel a and in Supplemental video 1.
Ultrasonographic findings of CDH. Panel a Chest X-ray of term infant with left CDH. b Transverse scan of the abdomen; note the absence in the left hemithorax of the hyperechoic line (dashed line) representing the normal diaphragm. c Absence of the hyperechoic line that represents the pleura and the absence of the normal A lines. It is possible to see the presence of a multi-layered area with hyperechoic contents typical of the normal gut (white arrows) instead of the normal pulmonary parenchyma. d Chest X-ray of neonate affected by right CDH. e Transverse scan of the abdomen; note the absence in the right hemithorax of the hyperechoic line (dashed line) representing the normal diaphragm. f Absence of the hyperechoic line that represents the pleura and absence of the normal A lines. The presence of the parenchymatous organ (liver) (white arrows) instead of the normal pulmonary parenchyma can be appreciated
The scans of the affected hemithorax showed partial absence of the pleural line and associated absence of pleural sliding; absence of A lines in the affected area; multi-layered area with hyperechoic contents in motion, typical of the normal gut and its peristalsis (Fig. 2 panel c) (Supplemental video 2). In the case of right-sided CDH, it was possible to identify the liver in the thorax (Fig. 2 panel f) (Supplemental video 3). In all our reported cases, there was the dislocation of mediastinum and heart in the opposite hemithorax.
None of the other 117/124 (94%) neonates enrolled in the companion study presented contemporaneously all the ultrasound signs we described in patients with CDH (p < 0.05). [4]
The LUS diagnosis of CDH took 15 min (interquartile range (IQR) 15–16 min) in comparison with 53 min (IQR 47–64 min) for CXR (p < 0.05).
Discussion
In this paper, we described the LUS findings in a case series of late-preterm and term infants with CDH to identify the ultrasound pattern of CDH.
We found that the LUS pattern of CDH is represented by (1) partial absence of the hyperechoic line representing the normal diaphragmatic profile; (2) partial absence of the pleural line and therefore of the pleural sliding in part of the affected hemithorax; (3) absence of A lines in the affected area; (4) presence, in the affected hemithorax, of multi-layered area with hyperechoic contents in motion, typical of the normal gut and its peristalsis; and (5) possible presence of parenchymatous organs in the thorax (i.e., liver, spleen). This pattern can be easily recognized with subcostal and trans-thoracic views and, therefore, we suggest that evaluation of the diaphragm from a subcostal view should be added to the traditional trans-thoracic view in all infants in whom a LUS was performed.
Therefore, LUS plays an important role in the diagnosis of congenital diseases that can affect the lung. Recently, LUS characteristics for the diagnosis of congenital pulmonary airway malformation (CPAM) have been described. [11]
The LUS characteristics that we described are in agreement with the two case reports on the use of LUS in the emergency department for late diagnosis of CDH [5, 10]. The authors reported the partial absence of pleural sliding and the presence of intestinal loops that can be seen inside the thorax in the affected side and the absence of a part of the diaphragm line.
In developing countries, antenatal care of pregnancy is often insufficient or absent and failure to diagnose CDH can frequently occur. Thus, in these settings, LUS can contribute to an early diagnosis of CDH and, possibly, improving its prognosis.
In developed countries with adequate antenatal care, the majority of CDHs are prenatally diagnosed. However, in some cases, the condition can still missed [8] and diagnosis can come late. Baglaj et al. [1] reported that CDH can be discovered late in 25% of cases. It is worthy to note that when the diagnosis of CDH is late, CXR can lead to a relatively large number of cases with incorrect diagnoses [2] and consequent incorrect medical management. A revision of 349 patients with delayed CDH diagnosis detailed that CXR misdiagnosis occurred in 88 children (25%), the most frequent misdiagnoses being pneumothorax (14 cases), pleural effusion (10 cases), hydropneumothorax (3 cases), and pneumonia with effusion (10 cases)[2]. Unfortunately, misdiagnoses were followed by improper treatment, such as antibiotic treatment or chest drainage placement, in addition to the detrimental effects of the delayed treatment of CDH.
We found that in our setting, neonatologists were able to diagnose CDH more rapidly using LUS compared to CXR, which allowed treatment of the disease as soon as possible and thus optimizing CDH prognosis. However, our results on the shorter duration of execution of LUS compared to CXR must be critically evaluated and contextualized within the organization of a single department. Many NICU have on-site X-ray facilities that may reduce the time of completion and diagnosis. For this reason, our results may not significant for other neonatal setting and therefore not be generalizable.
The limitation of this study is the small number of reported cases. In the reported cases, the dimension of the diaphragmatic defects was significant. Smaller defects might be more difficult to diagnose also by ultrasound; thus, studies with an adequate sample size should be conducted to obtain generalizable results.
However, considering the lack of other larger studies, we are confident that the proposed criteria for the LUS diagnosis of CDH are very accurate, although it cannot be excluded that smallest CDHs might be missed by LUS.
Conclusions
This paper provides description of the LUS findings in neonates with CDH. We found that CDH has an ultrasound pattern that allows a prompt diagnosis and that the proposed technique can contribute to early discovery of missed prenatal diagnoses and to the improvement of its prognosis.
Abbreviations
- CDH:
-
Congenital diaphragmatic hernia
- CXR:
-
Chest X-ray
- IQR:
-
Interquartile range
- LUS:
-
Lung ultrasound
References
Bagłaj M (2004) Late-presenting congenital diaphragmatic hernia in children: a clinical spectrum. Pediatr Surg Int 20:658–669
Bagłaj M, Dorobisz U (2005) Late-presenting congenital diaphragmatic hernia in children: a literature review. Pediatr Radiol 35:478–488
Clifton MS, Wulkan ML (2017) Congenital diaphragmatic hernia and diaphragmatic eventration. Clin Perinatol 44:773–779
Corsini I, Parri N, Gozzini E, Coviello C, Leonardi V, Poggi C, Giacalone M, Bianconi T, Tofani L, Raimondi F, Dani C (2019) Lung ultrasonography for the differential diagnosis of respiratory distress in neonates. Neonatology 115:77–84. https://doi.org/10.1159/000493001
Desjardins MP, Weerdenburg KD, Fischer JW (2016) Emergency point-of-care ultrasound diagnosis of diaphragmatic hernia in the pediatric emergency department. Pediatr Emerg Care 32(10):685–687
Gallot D, Coste K, Francannet C, Laurichesse H, Boda C, Ughetto S, Vanlieferinghen P, Scheye T, Vendittelli F, Labbe A, Dechelotte PJ, Sapin V, Lemery D (2006) Antenatal detection and impact on outcome of congenital diaphragmatic hernia: a 12-year experience in Auvergne (France). Eur J Obstet Gynecol Reprod Biol 125:202–205
Garne E, Haeusler M, Barisic I, Gjergja R, Stoll C, Clementi M (2002) Congenital diaphragmatic hernia: evaluation of prenatal diagnosis in 20 European regions. Ultrasound Obstet Gynecol 19:329–333. https://doi.org/10.1046/j.1469-0705.2002.00635.x
Oluyomi-Obi T, Van Mieghem T, Ryan G (2017) Fetal imaging and therapy for CDH-current status. Semin Pediatr Surg 26:140–146
Raimondi F, Yousef N, Migliaro F, Capasso L, De Luca D (2018) Point-of-care lung ultrasound in neonatology: classification into descriptive and functional applications. Pediatr Res. https://doi.org/10.1038/s41390-018-0114-9.
Rankin JH, Elkhunovich M, Seif D, Chilstrom M (2016) Point-of-care ultrasound diagnosis of diaphragmatic hernia in an infant with respiratory distress. Pediatr Emerg Care 32:731–733
Yousef N, Mokhtari M, Durand P, Raimondi F, Migliaro F, Letourneau A, Tissières P, de Luca D (2018 Oct) Lung ultrasound findings in congenital pulmonary airway malformation. Am J Perinatol 35(12):1222–1227. https://doi.org/10.1055/s-0038-1645861
Zalla JM, Stoddard GJ, Yoder B (2015) Improved mortality rate for congenital diaphragmatic hernia in the modern era of management: 15 year experience in a single institution. J Pediatr Surg 50:524–527. https://doi.org/10.1016/j.jpedsurg.2014.11.002
Author information
Authors and Affiliations
Contributions
Dr. Iuri Corsini and Dr. Niccolò Parri has equally contributed to the paper, serve as guarantors of the paper, and were responsible for study conception, design, execution, data analysis, and writing the manuscript.
Dr. Caterina Coviello and Dr. Valentina Leonardi enrolled patients, designed the data collection instruments, collected data reviewed, and revised the manuscript.
Prof. Carlo Dani supervised the project, provided oversight of the study, refined the study design and the design of the study protocol and data form, and critically reviewed the manuscript for important intellectual content.
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the local Ethical Committee. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Communicated by Patrick Van Reempts
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplemental video 1
Transverse subcostal view of the abdomen. Note the absence of the hyperechoic line representing the diaphragm in a neonate with left CDH. (MOV 418 kb)
Ultrasonographic findings of CDH. Note the absence of the hyperechoic line that represents the pleura and the absence of the normal A lines. The presence of a multi-layered area with hyperechoic contents typical of the normal intestine instead of the normal pulmonary parenchyma can be seen. (MOV 13597 kb)
Supplemental video 3
Ultrasonographic findings of CDH. Note the absence of the hyperechoic line that represents the pleura and the absence of the normal A lines. It is possible to see the parenchymatous organ (liver) instead of the normal pulmonary parenchyma. (MOV 19280 kb)
Rights and permissions
About this article
Cite this article
Corsini, I., Parri, N., Coviello, C. et al. Lung ultrasound findings in congenital diaphragmatic hernia. Eur J Pediatr 178, 491–495 (2019). https://doi.org/10.1007/s00431-019-03321-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-019-03321-y