Abstract
The aim of the surveys conducted by the Idiopathic Nephrotic Syndrome Working Group of the ESPN was to study the possible variability of treatment in Europe at different stages of the disease by means of questionnaires sent to members of the Working Group. Four surveys have been completed: treatment of the first flare, treatment of the first relapse and the issue of steroid dependency, use of rituximab, and the management of steroid-resistant patients. A uniform treatment of the first flare was applied in only three countries, and ten additional centers have adopted one of the three main protocols. Reported treatment of the first relapse was relatively uniform, whereas the use of additional immunosuppressants in steroid dependency was widely variable. Rituximab had already been used in hundreds of patients, although the formal evidence of efficiency in steroid dependency was relatively recent at the time of the survey. The definition of steroid resistance was variable in the European centers, but strikingly, the first-line treatment was uniform throughout the centers and included the combination of prednisone plus calcineurin antagonists.
Conclusion: The variability in the approach of idiopathic nephrotic syndrome is unexpectedly large and affects treatment of the first flare, strategies in the case of steroid dependency, as well as the definitions of steroid resistance.
What is Known: • Steroids and immunosuppressants are the universal treatment of idiopathic nephrotic syndrome. |
What is New: • The variability of treatments and strategy of treatment in European centers of pediatric nephrology |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
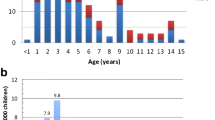
Idiopathic nephrotic syndrome (INS) is not a frequent disease, but not an orphan disease. The annual incidence in the population below 16 years of age is between 1.2 and 3.4 new cases per 100,000 [6]. It means that 1000 to 1500 new cases are occurring yearly in the European Union. Roughly half of them will be steroid-dependent and will have a median course of 10 years, meaning that 6000 to 16,000 pediatric patients (equivalent to 6 to 18 per 100,000 of the general population <16 years of age) are currently treated with steroids or immunosuppressive drugs. One of the main difficulties in gathering multicenter data for clinical studies on INS is due to the adoption of different treatment protocols as well as the definition of outcomes and resistance to treatment. This issue is particularly important in INS, where elements of the diagnosis and the prognosis are based on the response to the very initial phase of treatment.
The aim of the surveys conducted by the Idiopathic Nephrotic Syndrome Working Group (WG) of the European Society of Pediatric Nephrology (ESPN) was to study the possible variability of treatment in Europe at different stages of the disease by means of questionnaires sent to members of the WG. These questionnaires aimed at exploring different debated issues on INS treatment. The global conclusions are that the variability is unexpectedly large and not always understandable, even when a general consensus had apparently been reached.
Methods
Four surveys have been completed from 2013 to 2015 and sent to the 52 members of the INS Working Group.
Survey 1: first flare
Treatment of the first flare was investigated using a template where the classical protocols were recalled along with a space for the single center’s individual approach. Each participant was asked to fill out the available cells of the column space entitled “your protocol” with the local protocol of treatment of the first flare.
Survey 2: first relapse and steroid dependency
Treatment of the first relapse and the management of steroid-dependent patients were investigated using a clinical case. The first query aimed at describing the treatment of the first relapse in each center. According to the answer, a second query was on the timing and choice of additional immunosuppressive treatment in each center.
Survey 3: rituximab
The use of rituximab was investigated using two successive questionnaires. The first questionnaire mainly aimed at defining the criteria to treat with rituximab (steroid dependency, duration, or severe complication of the disease), and the second questionnaire was dedicated to the technical points: dose, number of infusions for the initial cure, duration of B cell depletion, antimicrobial prophylaxis, and withdrawal of conventional immunosuppressive drugs and steroids.
Survey 4: steroid-resistant forms
The management of steroid-resistant patients was investigated using a template to fill out. The template contained open criteria of the definition, use of renal biopsy, and access to genetic testing first-line treatment, duration of the treatment prior to considering failure, and criteria of success.
Results
The surveys were sent to 52 centers and answered by 40 centers from 19 countries. There were 29, 16, 27, and 18 answers for surveys 1, 2, 3, and 4, respectively (Table 1).
First flare
The questionnaire was returned by 26 individual centers (Table 2). In addition, three countries—Denmark, Germany, and France—that applied a uniform nationwide treatment were considered as one answer while representing dozens of individual centers. Surprisingly, those three protocols were relatively similar, but differed by the cumulative dose of prednisone (3360 mg/m2 for Denmark and Germany and 3990 mg/m2 for France), the use of intravenous methylprednisolone in the case of oral steroid resistance (Germany and France), and the tapering sequence (only in France). In other centers, the variability of the cumulative dose ranged from 2240 to 4245 mg/m2. Consistently, the duration of treatment also varied from 8 to 24 weeks. Other important results showed that (1) all centers gave 60 mg m−2 day−1 of prednisone (n = 14) or prednisolone (n = 15) to start the treatment; (2) all centers were limiting the daily dose during the first weeks of treatment, 18 of them to less than 60 mg/day, meaning that patients over 1 m2 (about 30 kg body weight) were receiving less than the nominal cumulative dose mentioned in Table 1; (3) 20 of 29 protocols included a sequence of several steps of steroid tapering before withdrawal; and (4) 20 of 29 were using an intravenous (IV) methylprednisolone test in the case of steroid resistance at the end of the period of full oral daily dose. Another unexpected fact was the variability of the protocols within large countries (Italy, Russia, Spain, and Turkey) as well as within smaller countries (Belgium, Croatia, and Serbia). Finally, half of the centers (13/26) were following one of the three main protocols emerging from the literature (Table 4): two centers (nos. 01 and 02; Table 1) had a protocol close to the model of the International Study of Kidney Diseases in Children (ISKDC; Table 4), seven centers (nos. 13–19; Table 1) had a protocol close to the model of the German Society for Pediatric Nephrology (GPN; Table 4), and four (nos. 24–27; Table 1) had a protocol close to that of the French Société de Néphrologie Pédiatrique (SNP; Table 4).
First relapse and steroid dependency
The survey adopted the form of a clinical quiz that was compiled by 16 centers. The clinical case presented a typical steroid-dependent patient relapsing 5 days after the withdrawal of prednisone. Reported treatment of the first relapse was relatively uniform and consisted of a short period of daily prednisone limited to the time to obtain a remission in one center, plus 3 days in 9 of 16 centers, and plus 5–7 days in five centers. Only one center reported treating the first relapse similarly to a first flare in the absence of significant steroid toxicity. A single treatment with prednisone lasting from 1 to 6 months without any prevention of further relapses was the choice of seven centers. A systematic prevention of further relapses was undertaken as soon as the first early relapse by eight centers: five gave long-lasting alternate day prednisone therapy, one levamisole, one cyclosporine, and one an unconventional combination of levamisole, mycophenolate, and subcutaneous polyclonal immunoglobulins. In the last center, treatment with mycophenolate was given only in the case of significant signs of steroid toxicity. Three centers also mentioned that cyclophosphamide or rituximab could be an option as soon as the first relapse in the case of relapse prior to the withdrawal of steroids.
At the second relapse, immunosuppressant drugs were systematically given to patients in nine centers. Mycophenolate was the first option in the majority of those centers, and only two considered cyclophosphamide or rituximab at this stage. Four centers did not consider any systematic prevention of further relapses at this stage of the disease, but mycophenolate or levamisole was conditioned to steroid toxicity in three out of four centers and cyclophosphamide in one out of four. The last three centers reported no answer for the second relapse and beyond.
Rituximab
The questionnaire was sent in two parts. Twenty-seven centers answered the first part and 13 the second part. One center had no experience at all. In contrast, several hundreds of patients have been treated with rituximab in the other 26 centers. Three centers reported more than 50 patients each and four other centers reported 20 to 50 patients each. The last 18 centers had a more marginal experience with less than ten patients. The major indication of treatment was steroid dependency. Other frequent indications included steroid resistance (eight centers) and long-lasting treatment with immunosuppressants (eight centers). A minimum of at least a 3-year duration of nephrotic syndrome was reported by seven centers, but two centers had clearly no lower limit for prescription. Rituximab was the last line of treatment for three centers. Either non-compliance or complications were an indication in six centers. Strikingly, costs of rituximab were not covered by healthcare insurance in Belgium and Poland in 2015.
Of the 13 centers that answered the second part of the questionnaire, 12 were initiating the treatment by one (eight centers) or two infusions at 1 week distance (four centers), while only one center followed the classic protocol consisting of four infusions in 4 weeks. The dose of one infusion was 375 mg/m2 for all centers, except one that reported a unitary dose of 750 mg/m2. Reinfusion was performed if B cell repletion was observed within 6 months after the first infusion in six centers and only in the case of relapse in four centers. A systematic long-lasting B cell depletion of 12 and 18 months was achieved in two centers. An alternate protocol adopted by one center was to treat any relapses with rituximab in steroid-dependent patients, allowing to rapidly stop the oral treatment. A reinfusion was never done in one center. A withdrawal of all oral drugs was attempted by all centers, with a delay varying from 1 month (in three centers) to 12 months.
Steroid-resistant forms
Eighteen centers answered the survey. The heterogeneity of the definition of steroid resistance is shown in Table 3. The first-line treatment that was adopted by the 18 centers was the association of calcineurin inhibitors, either cyclosporine (15 centers) or tacrolimus (three centers). A patient was considered multidrug-resistant in the case of no response to the association of calcineurin inhibitor and prednisone for a period of 3 months (two centers), 6 months (eight centers), or 9 months (five centers; three centers did not answer the question). Partial response to treatment was considered 50% proteinuria reduction by most centers and combined to serum albumin increase in three centers. In the case of partial response, mycophenolate was added as a second-line treatment in 13 centers. Only isolated centers propose a third-line treatment with apheretic techniques, intravenous high-dose immunoglobulin, and rituximab. One center had no additional treatment in the case of multidrug resistance. All centers decided to withdraw immunosuppressive therapies, shifting to exclusive supportive care based on unequivocal genetic results (all centers) or the development of renal failure (all centers).
Discussion
Idiopathic nephrotic syndrome affects children all over the globe, and one should expect that they should be treated with common and shared protocols. Here, we report the results of surveys that concern the treatment of children with INS in the European area. The data come from a sample of European centers of Pediatric Nephrology belonging to the INS Working Group of the ESPN and that answered the four surveys. Despite the relatively low number of participating centers compared to the total number of centers in Europe, which is clearly a limitation of the study, the surveys show large variations of treatment strategies at all steps of the management of idiopathic nephrotic syndrome in the European area, as already reported elsewhere in the world [16, 21].
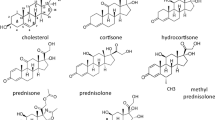
Numerous guidelines, meta-analyses [9], and follow-up series on the treatment of the first flare of nephrotic syndrome have been released in the literature by Pediatric Nephrology societies, consortium of centers, or single centers [7, 8, 12, 18, 25]. At least seven randomized prospective trials have tested different protocols of steroid therapy [8]. The fact is that the literature shows substantial differences in the treatment of the first flare according to countries and centers. In addition to the protocol described in the literature as the International Study of Kidney Disease in Childhood [3], the GPN (formerly named Arbeitgemeinshaft für Pädiatrische Nephrologie, APN) protocol [5], and the protocol of the Société de Néphrologie Pédiatrique [2], the US and India guidelines recommend a protocol that is very similar to that of the GPN [1, 8]. The protocol recommended by the Kidney Disease Improving Global Outcomes (KDIGO) is less well defined in terms of duration of treatment and is composed of different sources [14]. The main details of the protocols that are used in Europe are shown in Table 4. They are quite different in terms of duration and cumulated dose of steroid therapy, the tapering protocol, and the option of intravenous methylprednisolone in the case of oral steroid resistance. As a matter of fact, out of the European Centers of Pediatric Nephrology, one half of the centers reported using the ISKDC or the APN or the SNP protocol, while the other half have a local protocol that is more or less a mix of the three main protocols. The variability in the dose and duration of prednisone (or prednisolone) has already been reported in Italy, not only in General Pediatrics Units but also in those specialized in Pediatric Nephrology [20]. Noteworthy is that two centers using the classical ISKDC protocol have reported the use of IV methylprednisolone in the case of oral steroid resistance while this option is not classically included in those protocols.. The most surprising finding is that, according to this survey, a total of 13 European centers are treating patients below the KDIGO recommendations of minimum steroid therapy: less than 12 weeks of duration or less than 3360 mg/m2 of cumulative dose corresponding to the sum of 4 weeks at 60 mg m−2 day−1 and 6 weeks at 40 mg/m2 e.o.d. [14]. Nevertheless, two recent prospective randomized trials have shown that a cumulative prednisone dose of 2240 mg/m2 had the same effect on the outcome as doses of 3500 and 3900 mg/m2 [24, 26]. In contrast, a less recent prospective trial from Japan also showed that patients under 4 years of age had a strong benefit from a high cumulative dose of prednisolone [11]. At the other end, none of the centers participating in this survey reported steroid overtreatment, contrasting with a recent Italian report where patients in two pediatric nephrology units are treated with a cumulative prednisone dose of over 5000 mg/m2 [20]. However, our data clearly highlight the need to discuss common and shared European guidelines aimed at optimizing steroid therapy according to one protocol with different options. Based on the data of the literature and on the experience of centers, European guidelines should at least state about a uniform dose of steroids and define one option for the tapering protocol and the test with IV methylprednisolone.
In contrast with the treatment of the first flare, the steroid therapy of the first relapse, which has never been the objective of a randomized prospective trial, is very homogenous in Europe. All but one center treat the first relapse with a shortened duration of daily prednisone and a rapid tapering of the dose from 0 to 7 days after the remission of proteinuria, consistent with the KDIGO recommendations [14]. At this point, differences between centers concern the duration of steroid therapy and the use of an additional second-line treatment. Prevention of relapses by either long-lasting steroid therapy or levamisole was reported by seven centers as soon as the first relapse. Beyond the first relapse, KDIGO recommendations are vague, particularly on the chronology of each possible steroid-sparing treatment. No differences are suggested between the treatments that prevent relapses as long as they are continued but have no remnant effect after withdrawal (levamisole, mycophenolate, and calcineurin inhibitors) and those that clearly show the ability to disrupt the course of the disease in long-term follow-up series (cyclophosphamide and rituximab) [14]. At the second relapse, nine European centers considered an additional treatment and four reported using an additional treatment only in the case of steroid toxicity. Among the nine centers that reported an additional treatment, only two reported the early use of cyclophosphamide or rituximab. The duration of the disease was never explicitly mentioned as an indication of additional treatment.
Rituximab has now been fully recognized as an efficient treatment in steroid-dependent patients, with a high rate of evidence since the end of 2014 and the release of the first randomized controlled trial [13]. Nevertheless, the efficiency of rituximab has been empirically recognized by clinicians for several years [4], while more than 300 patients have been reported in the survey at the end of 2014. Variations in the use of rituximab are somehow limited: most of the centers reported the same unitary dose of 375 mg/m2, and the number of initial infusion was 1 or 2. Long-lasting B cell depletion [22] has been used by two centers, but one should recall that the risk of life-threatening infections might be proportional to the duration of B cell depletion [23]. An alternative way might be to systematically treat relapses in steroid-dependent patients with one infusion of rituximab in order to stop oral treatments rapidly and to delay the next relapse. Nevertheless, the best way to use rituximab remains to be defined in the near future.
Steroid resistance is a condition of high morbidity leading to end-stage renal failure or to long-lasting and heavy immunosuppressive drug therapy [10, 17, 27]. The definition of steroid resistance is very heterogeneous in the survey. Whereas the prevalence of steroid sensitivity is proportional to the duration and the cumulative dose of steroids [19], the resistance after 4 weeks of oral prednisone might have a different significance in terms of difficulty to treat than the resistance after 8 weeks of oral prednisone plus three intravenous methylprednisolone pulses. Nevertheless, the first-line treatment is similar in all centers regardless of the definition. All centers reported using a first line of prednisone and calcineurin antagonists, consistent with the KDIGO recommendations [15]. Mycophenolate is a common drug included in maintenance treatment, especially in partial response. Positive genetic testing is a major cause of immunosuppressive treatment withdrawal in all centers, suggesting that the first-line treatment is systematically started before genetic results are likely to be delayed in most cases. The other criterion that leads to withdrawal of immunosuppressive therapy is the time to unresponsiveness, which ranges between 3 and 9 months, defining multidrug resistance. In this case, experimental therapeutic options using plasma exchange or immunoglobulin removal are a choice for only two centers.
To conclude, a lot of work remains to be done in order to homogenize the treatment of idiopathic nephrotic syndrome based on high-quality evidence. The choice of treatment remains largely dependent on each physician’s clinical experience at all steps. This variability of therapeutic approaches deserves some attention and supports the commitment of the INS Working Group of the ESPN to build guidelines and consensus.
Abbreviations
- APN:
-
Arbeitgemeinshaft für Pediatrische Nephrologie
- ESPN:
-
European Society of Pediatric Nephrology
- GPN:
-
German Society for Pediatric Nephrology
- KDIGO:
-
Kidney Disease Improving Global Outcomes
- INS:
-
Idiopathic Nephrotic Syndrome
- ISKDC:
-
International Study of Kidney Disease in Childhood
- IVMP:
-
Intravenous methylprednisolone
- MP:
-
Methylprednisolone
- SNP:
-
Société de Néphrologie Pédiatrique
- WG:
-
Working Group
References
Bagga A, Ali U, Banerjee S, Kanitkar M, Phadke KD, Senguttuvan P, Sethi S, Shah M (2008) Management of steroid sensitive nephrotic syndrome: revised guidelines. Indian Pediatr 45:203–214
Berard E, Broyer M, Dehennault M, Dumas R, Eckart P, Fischbach M, Loirat C, Martinat L (2005) Corticosensitive nephrotic syndrome (or nephrosis) in children. Therapeutic guideline proposed by the Pediatric Society of Nephrology. Nephrol Ther 1:150–156. doi:10.1016/j.nephro.2005.06.003
Brodehl J, Ehrich JHH (1988) Short versus standard prednisone therapy for initial treatment of idiopathic nephrotic syndrome in children. Arbeitsgemeinschaft fur Padiatrische Nephrologie. Lancet 1:380–383
Cara-Fuentes G, Kairalla JA, Ishimoto T, Rivard C, Johnson RJ, Garin EH (2014) Rituximab in idiopathic nephrotic syndrome: does it make sense? Pediatr Nephrol 29:1313–1319. doi:10.1007/s00467-013-2534-4
Ehrich JH, Brodehl J (1993) Long versus standard prednisone therapy for initial treatment of idiopathic nephrotic syndrome in children. Arbeitsgemeinschaft fur Padiatrische Nephrologie. Eur J Pediatr 152:357–361
El Bakkali L, Rodrigues Pereira R, Kuik DJ, Ket JC, van Wijk JA (2011) Nephrotic syndrome in the Netherlands: a population-based cohort study and a review of the literature. Pediatr Nephrol 26:1241–1246. doi:10.1007/s00467-011-1851-8
Gellermann J, Ehrich JH, Querfeld U (2012) Sequential maintenance therapy with cyclosporin A and mycophenolate mofetil for sustained remission of childhood steroid-resistant nephrotic syndrome. Nephrol Dial Transplant Off Pub Eur Dial Trans Assoc - Eur Renal Assoc 27:1970–1978. doi:10.1093/ndt/gfr572
Gipson DS, Massengill SF, Yao L, Nagaraj S, Smoyer WE, Mahan JD, Wigfall D, Miles P, Powell L, Lin JJ, Trachtman H, Greenbaum LA (2009) Management of childhood onset nephrotic syndrome. Pediatrics 124:747–757. doi:10.1542/peds.2008-1559
Hahn D, Hodson EM, Willis NS, Craig JC (2015) nephrotic syndrome in children. Cochrane Database Syst Rev (1):CD001533. doi: 10.1002/14651858.CD001533.pub5
Hamasaki Y, Yoshikawa N, Nakazato H, Sasaki S, Iijima K, Nakanishi K, Matsuyama T, Ishikura K, Ito S, Kaneko T, Honda M (2013) Prospective 5-year follow-up of cyclosporine treatment in children with steroid-resistant nephrosis. Pediatr Nephrol 28:765–771. doi:10.1007/s00467-012-2393-4
Hiraoka M, Tsukahara H, Matsubara K, Tsurusawa M, Takeda N, Haruki S, Hayashi S, Ohta K, Momoi T, Ohshima Y, Suganuma N, Mayumi M (2003) A randomized study of two long-course prednisolone regimens for nephrotic syndrome in children. Am J Kidney Dis 41:1155–1162
Hodson EM, Willis NS, Craig JC (2007) Corticosteroid therapy for nephrotic syndrome in children. Cochrane Database Syst Rev. doi:10.1002/14651858.CD001533.pub4
Iijima K, Sako M, Nozu K, Mori R, Tuchida N, Kamei K, Miura K, Aya K, Nakanishi K, Ohtomo Y, Takahashi S, Tanaka R, Kaito H, Nakamura H, Ishikura K, Ito S, Ohashi Y (2014) Rituximab for childhood-onset, complicated, frequently relapsing nephrotic syndrome or steroid-dependent nephrotic syndrome: a multicentre, double-blind, randomised, placebo-controlled trial. Lancet 384:1273–1281. doi:10.1016/S0140-6736(14)60541-9
KDIGO (2012) KDIGO clinical practice guideline for glomerulonephritis. Kidney Int Suppl 2:143–153. doi:10.1038/kisup.2012.13
Lombel RM, Gipson DS, Hodson EM (2013) Treatment of steroid-sensitive nephrotic syndrome: new guidelines from KDIGO. Pediatr Nephrol 28:415–426. doi:10.1007/s00467-012-2310-x
MacHardy N, Miles PV, Massengill SF, Smoyer WE, Mahan JD, Greenbaum L, Massie S, Yao L, Nagaraj S, Lin JJ, Wigfall D, Trachtman H, Hu Y, Gipson DS (2009) Management patterns of childhood-onset nephrotic syndrome. Pediatr Nephrol 24:2193–2201. doi:10.1007/s00467-009-1282-y
Mekahli D, Liutkus A, Ranchin B, Yu A, Bessenay L, Girardin E, Van Damme-Lombaerts R, Palcoux JB, Cachat F, Lavocat MP, Bourdat-Michel G, Nobili F, Cochat P (2009) Long-term outcome of idiopathic steroid-resistant nephrotic syndrome: a multicenter study. Pediatr Nephrol 24:1525–1532. doi:10.1007/s00467-009-1138-5
Nakanishi K, Iijima K, Ishikura K, Hataya H, Nakazato H, Sasaki S, Honda M, Yoshikawa N (2013) Two-year outcome of the ISKDC regimen and frequent-relapsing risk in children with idiopathic nephrotic syndrome. Clin J Am Soc Nephrol CJASN 8:756–762. doi:10.2215/CJN.09010912
Nakayama M, Katafuchi R, Yanase T, Ikeda K, Tanaka H, Fujimi S (2002) Steroid responsiveness and frequency of relapse in adult-onset minimal change nephrotic syndrome. Am J Kidney Dis 39:503–512. doi:10.1053/ajkd.2002.31400
Pasini A, Aceto G, Ammenti A, Ardissino G, Azzolina V, Bettinelli A, Cama E et al (2015) Best practice guidelines for idiopathic nephrotic syndrome: recommendations versus reality. Pediatr Nephrol 30:91–101. doi:10.1007/s00467-014-2903-7
Samuel S, Morgan CJ, Bitzan M, Mammen C, Dart AB, Manns BJ, Alexander RT, Erickson RL, Grisaru S, Wade AW, Blydt-Hansen T, Feber J, Arora S, Licht C, Zappitelli M (2013) Substantial practice variation exists in the management of childhood nephrotic syndrome. Pediatr Nephrol 28:2289–2298. doi:10.1007/s00467-013-2546-0
Sellier-Leclerc AL, Baudouin V, Kwon T, Macher MA, Guerin V, Lapillonne H, Deschenes G, Ulinski T (2012) Rituximab in steroid-dependent idiopathic nephrotic syndrome in childhood—follow-up after CD19 recovery. Nephrol Dial, Trans Off Pub Eur Dial Trans Assoc - Eur Renal Assoc 27:1083–1089. doi:10.1093/ndt/gfr405
Sellier-Leclerc AL, Belli E, Guerin V, Dorfmuller P, Deschenes G (2013) Fulminant viral myocarditis after rituximab therapy in pediatric nephrotic syndrome. Pediatr Nephrol 28:1875–1879. doi:10.1007/s00467-013-2485-9
Sinha A, Saha A, Kumar M, Sharma S, Afzal K, Mehta A, Kalaivani M, Hari P, Bagga A (2015) Extending initial prednisolone treatment in a randomized control trial from 3 to 6 months did not significantly influence the course of illness in children with steroid-sensitive nephrotic syndrome. Kidney Int 87:217–224. doi:10.1038/ki.2014.240
Tarshish P, Tobin JN, Bernstein J, Edelmann CM Jr (1997) Prognostic significance of the early course of minimal change nephrotic syndrome: report of the International Study of Kidney Disease in Children. Clin J Am Soc Nephrol JASN 8:769–776
Yoshikawa N, Nakanishi K, Sako M, Oba MS, Mori R, Ota E, Ishikura K, Hataya H, Honda M, Ito S, Shima Y, Kaito H, Nozu K, Nakamura H, Igarashi T, Ohashi Y, Iijima K (2015) A multicenter randomized trial indicates initial prednisolone treatment for childhood nephrotic syndrome for two months is not inferior to six-month treatment. Kidney Int 87:225–232. doi:10.1038/ki.2014.260
Zagury A, Oliveira AL, Montalvao JA, Novaes RH, Sa VM, Moraes CA, Tavares Mde S (2013) Steroid-resistant idiopathic nephrotic syndrome in children: long-term follow-up and risk factors for end-stage renal disease. Jornal brasileiro de nefrologia: ′orgao oficial de Sociedades Brasileira e Latino-Americana de Nefrologia 35:191–199. doi:10.5935/0101-2800.20130031
*Working Group on Idiopathic Nephrotic Syndrome—list of coauthors
Marmara University Medical Faculty, Istanbul, Turkey harika.alpay@gmail.com
Hospital Vall d’Hebron, Barcelona, Spain amadrid@vhebron.net
Aarhus University Hospital, Aarhus, Denmark rfa@clin.au.dk
Olgahospital, Stuttgart, Germany m.bald@klinikum-stuttgart.de
Department of Woman’s and Child’s Health, AOP-University of Padova, Italy elisabene@libero.it
Hôpitaux pédiatriques universitaires de Nice, Nice, France berard.e@chu-nice.fr
Great Ormond Street Hospital, London, UK d.bockenhauer@ucl.ac.uk
Hôpital Necker, APHP, Université Paris-Descartes, Paris, France olivia.boyer@aphp.fr
Haukeland University Hospital, Bergen, Norway damien.marie.michel.brackman@helse-bergen.no
APHP Robert-Debré, Paris France claire.dossier@aphp.fr
Kocaeli Çocuk Nefroloji ve Romatoloji Bilim Dalı, Umuttepe, Türkiye zekinci@outlook.com
Bambino Gesù Children’s Hospital and Research Institute, Roma, Italy francesco.emma@opbg.net
KU Leuven and University Hospitals Leuven, Leuven, Belgium, benedicte.eneman@uzleuven.be
Paediatric Nephrology, Hospital Universitario La Paz, Madrid, Spain lespinosar@salud.madrid.org
Hôpital Arnaud de Villeneuve, Montpellier, France m-fila@chu-montpellier.fr
U.O.C. Nefrologia e Dialisi Pediatrica - Fondazione IRCCS Cà Granda, Milan, Italy luciana.ghio@policlinico.mi.it
Emma Children’s Hospital, Amsterdam, the Netherlands j.w.groothoff@amc.uva.nl
Limoges University Hospital, Limoges, France v.guigonis@gmail.com
Pediatric Center, Vilnius University, Vilnius, Lithuania augustina.jankauskiene@mf.vu.lt
Orenburg Regional Children’s Hospital, Orenburg, Russia mkaganorenburg@yahoo.com
Institute for Child and Youth Health Care in Novi Sad, Serbia dr.maja.kovacevic@gmail.com
University Medical Center Hamburg-Eppendorf, Hamburg, Germany kemper@uke.de
KU Leuven and University Hospitals Leuven, Leuven, Belgium elena.levtchenko@uzleuven.be
Ospedale dei Bambini “G. Di Cristina” A.R.N.A.S., Palermo, Italy s.maringhini@ospedalecivicopa.org
Ege University Faculty of Medicine, İzmir, Turkey sevgi.mir@ege.edu.tr
P. & A. Kyriakou Children’s Hospital, Athens, Greece amitsioni@icloud.com
Medical University of Warsaw, Warsaw, Poland wasiaczki@wp.pl
Jagiellonian University Medical College, Cracow, Poland amoczulska@cm-uj.krakow.pl
University of Milan, Ospedale Maggiore Policlinico, Milan, Italy giovanni.montini@unimi.it
Department of Woman’s and Child’s Health, AOP-University of Padova, Padua, Italy. luisa.murer@sanita.padova.it
Department of Pediatrics, University of Oulu, Oulu, Finland mnuutine@cc.oulu.fi
Research Institute of Pediatrics and Children Surgery, Moscow, Russia obuhova.v@mail.ru
University Medical Center Hamburg-Eppendorf, Hamburg, Germany j.oh@uke.de
Fatih Sultan Mehmet Training and Research Hospital, Istanbul, Turkey ozanozkaya@yahoo.com
Azienda Ospedaliera, Cosenza, Italy teresapapalia@alice.it
BEL MEDIC General Hospital, Belgrade, Serbia amira@udk.bg.ac.rs
Nephrology and Dialysis, Children Hospital Santobono-Pausilipon, Naples, Italy pecoraro@unina.it
Hospital Universitario La Paz, Madrid, Spain antonia.pena@salud.madrid.org
Russian National Research Medical University, Moscow, Russia ed3565@ya.ru
Centre Hospitalier Universitaire de Reims, France cpietrement@chu-reims.fr
Pirogov Russian National Research Medical University, Moscow, Russia lprikhodina@yahoo.com
Charité Universitätsmedizin, Berlin, Germany uwe.querfeld@charite.de
Aarhus University Hospital, Aarhus, Denmark rittig@clin.au.dk
School of Clinical Sciences, University of Bristol, UK m.saleem@bristol.ac.uk
School of Medicine, University of Split, Split, Croatia msaraga@kbsplit.hr
Saint-Petersburg State Pediatric Medical University, St Petersburg, Russia savenkova.n.spb@mail.ru
İstanbul University Cerrahpaşa Faculty of Medicine, İstanbul, Turkey severlale@hotmail.com
Great Ormond Street Hospital, London, UK Kjell.Tullus@gosh.nhs.uk
Armand-Trousseau Hospital, Paris, France tim.ulinski@aphp.fr
Safepedrug, University Hospital Gent, Gent, Belgium Johan.VandeWalle@uzgent.be
Martin Hospital Universitario 12 de Octubre, Madrid, Spain julia.vara@salud.madrid.org
University of Manchester, Manchester Academic Health Science Centre, Royal Manchester Children’s Hospital, Manchester, UK Nicholas.Webb@cmft.nhs.uk
University Hospital of Cologne, Cologne, Germany lutz.weber@uk-koeln.de
Medical University Gdansk, Poland azur@gumed.edu.pl
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Consortia
Contributions
Georges Deschênes and Licia Peruzzi conceived the questionnaires and wrote the paper.
Marina Vivarelli wrote the paper with LP and GD.
Coauthors of the ESPN Working Group on Idiopathic Nephrotic Syndrome answered the surveys.
Among coauthors, Olivia Boyer, Detlef Bockenhauer, Etienne Berard, Lutz Weber, and Lale Sever kindly reviewed the paper.
Corresponding author
Ethics declarations
Funding
This study has been supported by a grant of 1000€ from the European Society of Pediatric Nephrology
Conflicts of interest
The authors declare that they have no conflict of interest and no financial relationship with the ESPN.
The coauthors in the list declare no conflict of interest and no financial relationship with the ESPN.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
It is clear that this paper obviously reports the routine clinical experience of medical teams on the treatment of human patients affected of a human disease, but this article does not contain any experimental studies with human participants or animals performed by any of the authors. It is also clear that several thousand human patients are the core of this clinical experience, but this paper does not report any specific information contained in patient files. Consequently, informed consent has not been obtained from individual participants.
Additional information
Communicated by Mario Bianchetti
Revisions received: 13 February 2017; 24 February 2017
Rights and permissions
About this article
Cite this article
Deschênes, G., Vivarelli, M., Peruzzi, L. et al. Variability of diagnostic criteria and treatment of idiopathic nephrotic syndrome across European countries. Eur J Pediatr 176, 647–654 (2017). https://doi.org/10.1007/s00431-017-2891-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-017-2891-2