Abstract
We investigated dwell times and risk of non-elective removal of 975 single-lumen 1-French peripherally inserted central catheters (1FR-PICC) according to tip position in a cohort of very preterm infants with a mean (SD) gestational age of 27+6 (2+1) weeks and a mean (SD) birth weight of 988 (294) g over an eight-year period. Infants with a 1FR-PICC inserted for continuous infusion of intravenous fluids within the first 30 days of life were eligible. Dwell times of PICC with elective versus non-elective removal, risk of non-elective removal of PICC according to tip position, and differences between upper versus lower limb catheter insertion were analysed. 33.8% PICC were removed non-electively. Median (IQR) dwell time was 193 (142–287) versus 154 (102–260) h for elective versus non-elective removal (p < 0.001). Non-elective removal was more common for lower limb insertion sites: 41 versus 31% (p = 0.002). PICC were significantly more likely to be removed non-electively when located in the axillary (odds ratio (OR) 2.08), cephalic (OR 8.93), external iliac (OR 4.99), and femoral (OR 10.31) vein.
Conclusion: In this cohort, dwell times of 1FR-PICC lines removed non-electively were similar to 1.9- or 2.0FR-PICC. PICC tips positioned in the axillary, cephalic, external iliac, and femoral veins had a higher risk of non-elective removal.
What is Known: |
•Peripherally inserted central catheters (PICC) are widely used in neonatal intensive care. |
•Previous studies focused on 2-French PICC and newborns of all gestational ages. |
What is New: |
•Dwell times of 1-French PICC removed non-electively were similar to 2-French PICC. |
•1-French PICC tips positioned more peripherally had a higher risk of non-elective removal. |
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Peripherally inserted central catheters (PICC) are widely used in neonatal intensive care for the provision of parenteral nutrition and intravenous drugs in even the tiniest preterm infants. Commercially available catheters are as small as a size of 1FR/28G, translating into an external diameter of one third of a millimetre. Commonly used veins for PICC insertion are the basilic vein or the saphenous vein, although other veins are suitable as long as the PICC can be advanced easily. The most preferred PICC tip positions are centrally in the superior and inferior cava vein (SVC, IVC), but other catheter tip positions are usually tolerated if the PICC cannot be advanced any further in view of limited venous access options in the very preterm infant. Previous studies, however, have shown ambiguous results regarding the optimal PICC tip position and associated complications. Hoang et al. reported a lower complication rate for lower extremity PICC insertion, whereas Wrightson did not demonstrate a difference between upper and lower extremity insertion [4, 7]. Colacchio et al. analysed PICC tip positions and found more complications in PICC with a non-central tip position [1]. Similarly, Jain et al. reviewed PICC tip positions in central or non-central position and reported a higher complication rate for non-central PICC, predominantly because of PICC with the tip lying in a mid-clavicular position [6]. In contrast, Costa et al. did not demonstrate a difference in non-elective removal rates of PICC according to their tip position [2].
All of these studies enrolled neonates of all gestation ages and used preferably 2-French (FR) PICC lines, where stated. The aim of our study was to investigate exclusively the smallest available PICC lines (1FR) in a large cohort of preterm infants born less than 32 weeks gestation or less than 1500 g birth weight. The study outcomes focused on dwell time of PICC lines with elective versus non-elective removal, risk of non-elective removal of PICC according to tip position, and differences between upper versus lower limb catheter insertion for this specific PICC size.
Methods
Setting
This retrospective cohort study was conducted at the neonatal intensive care unit (NICU) of the Mercy Hospital for Women, one of three tertiary perinatal centres in Melbourne, Australia, with approximately 6000 births and 180–200 very low birth weight infants cared for in the NICU per year. The study was approved by the institutional Human Research Ethics Committee (Mercy Health Inc., Melbourne, Victoria, Australia). The need for written consent was waived as the study was considered a low-risk, quality assurance project, and all data were reviewed de-identified.
Patients
Preterm infants born less than 1500 g birth weight or less than 32 weeks gestation were eligible if they had a PICC inserted within the first 30 days of life for the purpose of a continuous infusion of IV fluids. Only single-lumen PICC insertions with a size of 1FR/28G were included into the study. Patients with other PICC lines inserted, or PICC inserted in other NICUs, were excluded.
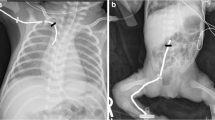
PICC placement and care
In our NICU, all PICC are inserted by advanced neonatal trainees or consultant neonatologists, following the unit’s standard PICC insertion procedure. The standard PICC line used in very preterm infants is the 1FR/28G Premicath (Vygon GmbH & Co. KG, Aachen, Germany) without stylet. The PICC position is confirmed on X-ray using contrast medium (Ultravist®, Bayer Australia Ltd., Pymble, NSW, Australia) prior to final fixation of the catheter. All X-rays are immediately reviewed by the consultant neonatologist on duty, and subsequently by a consultant paediatric radiologist. A central PICC tip position in the SVC or IVC outside the heart is preferred; however, less central tip positions are acceptable if the PICC could not be more advanced further during the procedure in view of limited venous access in very preterm infants. Care and access of the PICC line is performed in a strictly sterile fashion according to the unit’s standard operating procedure. The NICU’s total parenteral nutrition solution contains heparin (1 unit/ml). In case of suspected or true PICC line infection, the line would be removed promptly.
Classification of tip position
For this study, the final X-ray report of the consultant paediatric radiologist was reviewed for each PICC included. The tip positions were classified according to the report as the tip of the catheter lying in the SVC, brachiocephalic vein, subclavian vein, axillary vein, and cephalic vein for the upper limb, and IVC, common iliac vein, external iliac vein, and femoral vein for the lower limb. In the event an X-ray report was ambiguous about the tip position of the PICC, the X-ray was retrieved and reviewed.
Data collection
The following data were collected from the departmental database: gestational age, birth weight, sex, day of life of PICC insertion, day of life of PICC removal, PICC duration, and elective or non-elective removal.
Outcome measures and statistical analysis
The aim of this study was to identify the risk of non-elective PICC removal according to the PICC tip position, including the potential association of gestational age, birth weight, sex, and upper versus lower limb PICC insertion. Elective removal was defined as removal of the PICC line because it was no longer required (e.g. cessation of parenteral nutrition/IV fluids). Non-elective removal included all causes for premature removal prior to its intended duration, including true or suspected infection, inflammation or leakage at the insertion site, line occlusion, and kinked or obstructed lines.
Data analysis was performed using Stata 11.2 (StataCorp, College Station, Texas, USA). Multiple logistic regression (allowing for gestation, birth weight, and sex) and χ2 test were used for categorical data. T test and Wilcoxon’s rank sum test were used for continuous variables. A p value <0.05 was considered significant.
Results
Study cohort
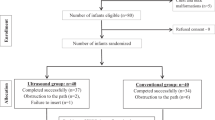
Between 2004 and 2011, a total of 975 PICC inserted fulfilled the inclusion criteria. The study cohort had a mean (SD) gestational age of 27+6 weeks (2+1 weeks) and a mean (SD) birthweight of 988 g (294 g). Fifty-six percent were male. Table 1 shows the number of PICC per pre-specified PICC tip position.
Elective versus non-elective PICC removal
The median (IQR) insertion time was day 4 of life (3–6) for PICC electively removed and day 5 of life (3–7) for PICC with non-elective removal (p = 0.039). PICC removed electively were in situ for longer time a follows: median (IQR) 193 h (142–287) versus 154 h (102–260) h for non-elective removal (p < 0.001).
Association of gestational age, birth weight, and sex with elective and non-elective PICC removal
On average, subjects with non-elective removal of PICC were 6 days younger than those with elective PICC removal. Mean (SD) gestational age for elective removal was 28+0 weeks (2+1 weeks) versus 27+1 weeks (2+1 weeks) for non-elective removal (p < 0.001). Mean (SD) birth weight for elective removal was 1050 g (11 g) versus 895 g (15 g) for non-elective PICC removal (p < 0.001). Gender was not significantly associated with elective PICC removal, with 66% elective PICC removal in both males and females (p = 0.83).
Upper versus lower limb PICC insertion
There was no difference in the PICC duration between upper and lower limb insertion: upper limb median (IQR) 186 h (129–269) versus lower limb median (IQR) 172 h (122–183) (p = 0.56). Day of PICC insertion was also similar between upper and lower limb insertion sites: median (IQR) day of life 4 (3–6) for upper limb insertion versus median (IQR) day of life 4 (3–10) for lower limb insertion (p = 0.11). However, non-elective removal was more common for lower limb PICC: 41% of lower limb PICC were removed non-electively versus 31% of upper limb PICC (p = 0.002). Gestational age was not significantly associated with upper versus lower limb insertion of PICC (mean 276 weeks gestation upper limb, 274 weeks gestation lower limb, p = 0.16). Similarly, birth weight was not significantly associated with upper versus lower limb insertion of PICC (1003 g upper limb, 983 g lower limb, p = 0.32). Table 2 shows the median (IQR) PICC duration for non-electively removed PICC per tip position.
Risk of non-elective removal per tip position
Table 3 shows the odds ratios for non-elective PICC removal per tip position, correcting for birth weight, gestational age, and sex, using the tip in the SVC as reference position. A PICC tip located in the axillary, cephalic, external iliac, and femoral vein were significantly more likely to be removed non-electively.
Discussion
We investigated the dwell time of 1FR single-lumen PICC lines according to their catheter tip position in this retrospective study. To the best of our knowledge, this is the first study to exclusively report on PICC of this size in a large cohort of very preterm infants. This and the previously published studies give an overview of dwell times of PICC removed non-electively in newborns. Isemann et al. report a median PICC duration of 6 days for 1.9FR PICC lines until non-elective removal of the catheter. This is close to our population where the median dwell time of PICC removed non-electively was 6.4 days (154 h) [5]. Jain et al. reviewed 1.9FR and 2.0FR PICC and discriminated between PICC with a central tip position versus non-central tip position; the median duration was 11.4 and 6.2 days, respectively [6]. The largest and most recently published study by Greenberg et al. investigated dwell times of PICC and the related risk of infection in preterm infants. Almost 15,000 PICC were studied, however, the PICC size and tip position was not reported, and PICC removed within the first 2 days following insertion were excluded. The study revealed no increased risk for central line associated bloodstream infections with prolonged PICC dwell time. The authors concluded clinicians should not routinely replace uninfected PICC [3] (Table 4, electronic supplementary material).
Jain et al. argued against the use of PICC with the tip in subclavian veins in their study. Our study confirms a shorter dwell time for PICC with the tip in the subclavian vein, however when calculating the odds ratio for non-elective removal, this did not reach statistical significance. Only PICC tips lying in the axillary, cephalic, external iliac, and femoral veins had a significantly increased risk of premature, non-elective removal. Our results agree with Jain et al.’s with regards to PICC tip positions in the superior and inferior vena cava and in brachiocephalic veins. In addition, we also found no increased risk for non-elective removal for PICC tips positioned in the common iliac vein [6].
There was no significant difference in PICC duration between upper versus lower limb insertion; however, more PICC were removed non-electively from the lower limb: 41 versus 31%. This is in contrast to the study by Hoang et al. who reported a lower complication rate and longer duration for PICC lines inserted in the lower extremity [4]. There are several differences between Hoang’s and our study. Firstly, our sample size is more than double of Hoang’s study. Secondly, the type of PICC line is different. Hoang et al. only used 2FR PICC lines in their cohort, whereas our study only included 1FR PICC in this study. Wrightson also investigated PICC complications related to upper or lower limb insertion site [7]. In contrast to Hoang et al., no difference in complications according to limb insertion site was reported. A total of 626 PICC were reviewed in a cohort of preterm and term infants. It is noted that the mean birth weight of enrolled infants was much higher in Wrightson’s cohort compared to Hoang’s and our study.
Our study has several strengths. We limited inclusion to very preterm infants who commonly require central venous access for parenteral nutrition and administration of intravenous drugs. Due to the limited number of appropriate veins for insertion, PICC lines are the preferred option of central venous access in this population. We also did not include PICC lines inserted in other veins than upper and lower limb veins such as femoral PICC line insertion or scalp veins as these are not standard procedure in our NICU. In contrast to other studies published previously, this is the first study only including preterm infants who had a 1FR/28G PICC line inserted. The number of PICC lines analysed is large with almost a thousand catheters reviewed.
There are limitations. It is a retrospective study design. Although a central tip position is preferred, the unit follows a pragmatic approach tolerating less central catheter positions in favour of fewer PICC insertion attempts to minimize the impact of pain and discomfort for the baby. This is reflected in the higher number of PICC lines with tips in non-central positions. Other neonatal units may prefer a more restrictive approach with regard to non-central catheter tip positions. There might be some variance in the insertion technique based on the individual experience of the medical practitioner. Trainees in their advanced neonatal training are supervised for several PICC insertions until they are deemed capable; however, it obviously requires more experience to achieve sufficient routine for the procedure. PICC tip positions were assessed on a plain X-ray performed immediately following PICC insertion. It is known that PICC move with limb motion; hence, we cannot exclude tip migration at the time of catheter removal.
We conclude that dwell times of 1FR PICC lines removed non-electively are similar to 1.9 or 2.0FR PICC. PICC tips positioned in the axillary, cephalic, external iliac, and femoral veins had a higher risk of non-elective removal.
Authors’ contributions
DME, SN, DMC, and KK conceived the study. KK and DMC wrote the study protocol and ethics application. DME and SN collected all data. DME, SN, KJG, DMC, and KK reviewed and analysed all data. KJG and DMC performed all statistical analyses. DME and KK wrote the first version of the manuscript. All authors edited the first and subsequent versions of the manuscript and approved the submitted manuscript.
Abbreviations
- FR:
-
French
- IQR:
-
Interquartile range
- IVC:
-
Inferior vena cava
- NICU:
-
Neonatal intensive care unit
- PICC:
-
Peripherally inserted central catheter
- SD:
-
Standard deviation
- SVC:
-
Superior vena cava
References
Colacchio K, Deng Y, Northrup V, Bizzarro MJ (2013) Complications associated with central and non-central venous catheters in a neonatal intensive care unit. J Perinatol 32:941–946
Costa P, Bueno M, Aparecida Alves AM, Kimura AF (2013) Incidence of nonelective removal of percutaneously inserted central catheters according to tip position in neonates. J Obstet Gynecol Neonatal Nurs 42:348–356
Greenberg RG, Cochran KM, Smith PB et al (2015) Effect of catheter dwell time on risk of central line-associated bloodstream infection in infants. Pediatrics 136:1080–1086
Hoang V, Sills J, Chandler M, Busalani E, Clifton-Koeppel R, Modanlou HD (2008) Percutaneously inserted central catheter for total parenteral nutrition in neonates: complications rates related to upper versus lower extremity insertion. Pediatrics 121:e1152–e1159
Isemann B, Sorrels R, Akinbi H (2015) Effect of heparin and other factors associated with complications of peripherally inserted central venous catheters in neonates. J Perinatol 32:856–860
Jain A, Deshpande P, Shah P (2013) Peripherally inserted central catheter tip position and risk of associated complications in neonates. J Perinatol 33:307–312
Wrightson DD (2013) Peripherally inserted central catheter complications in neonates with upper versus lower extremity insertion sites. Adv Neonatal Care 13:198–204
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this study.
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the institutional Human Research Ethics Committee (Mercy Health Inc., Melbourne, Victoria, Australia). The need for written consent was waived by the Committee as the study was considered a low-risk, quality assurance project, and all data were reviewed de-identified.
Additional information
Communicated by Patrick Van Reempts
Revisions received: 05 December 2016; 03 January 2017
Electronic supplementary material
Supplementary Table 4
(DOCX 20 kb)
Rights and permissions
About this article
Cite this article
Erhard, D.M., Nguyen, S., Guy, K.J. et al. Dwell times and risk of non-elective removal of 1-French peripherally inserted central catheters according to catheter tip position in very preterm infants. Eur J Pediatr 176, 407–411 (2017). https://doi.org/10.1007/s00431-017-2854-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-017-2854-7