Abstract
Permethrin is the most widely used pediculicide, but evidence of resistance from several countries and anecdotal reports from Germany suggest that permethrin lotion is now less effective. We designed a randomized, controlled, parallel group trial involving 100 participants with active head louse infestation to investigate the activity of a coconut and anise spray and to see whether permethrin lotion is still effective, using two applications of product 9 days apart. The spray was significantly more successful (41/50, 82.0%) cures compared with permethrin (21/50, 42.0%; p < 0.0001, difference 40.0%, 95% confidence interval of 22.5% to 57.5%). Per-protocol success was 83.3% and 44.7%, respectively. Thirty-three people reported irritant reactions following alcohol contact with excoriated skin. We concluded that, although permethrin lotion is still effective for some people, the coconut and anise spray can be a significantly more effective alternative treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The insecticide permethrin is probably the most widely used active ingredient for treatments designed to eliminate head louse infestation and is found in products from North and South America, Asia, Australia, and most countries in Europe. Several studies have now shown acquired resistance to this insecticide in head lice, and in most cases, this has been identified as being primarily mediated by a recessive gene mutation known as “knockdown” resistance (kdr) [1–5], although this is not the only mechanism for resistance to these insecticides, which may also be degraded metabolically [5, 11]. However, the impact of resistance is variable depending upon the intensiveness of selection pressure through extensive and frequent use of pyrethroid insecticides for treatment of infestation. Effectiveness of treatment is also influenced by the dosage form used for different products and whether active formulation excipients are present [6, 7]. Consequently, some preparations with permethrin as the active ingredient may be more effective than others when used in the same community. It is for this reason that 0.43% permethrin alcoholic lotion is one of the most used preparations in Germany because alcohol is believed to enhance the penetration of insecticides into the lice.
Coconut and anise spray has been shown to be effective in killing laboratory reared lice and their eggs (E. Brunton, unpublished data) and has been evaluated in two previous clinical investigations with good success rates [8, 9]. However, the first study used a treatment regimen different from the one currently used for the product in Europe and experienced approximately 10% drop-out rate [8]. The other evaluated only 12 subjects [9]. Overall, these studies indicated that the product is likely to have a treatment success rate of around 90%, which would make it an acceptable alternative in areas where resistance is an issue with conventional insecticides like permethrin.
We have conducted a randomized, assessor-blinded (single-blinded) clinical trial to evaluate the efficacy of coconut and anise spray in comparison with that of permethrin lotion and to compare the products for safety and acceptability to consumers.
Materials and methods
Objectives
This study was designed to compare the efficacy of a coconut and anise spray with 0.43% permethrin lotion with sufficient power to detect if the activity of either product was superior to that of the other.
Participants
Participants to this study were recruited by advertising in newspapers or parish magazines and from direct contact with families who had participated in previous clinical studies and who had expressed a wish to be included in any future research. In each case, an information booklet was delivered to the family, and an appointment was arranged for an investigator to visit. Potential participants were screened for head lice using a standard detection comb used in previous studies (“PDC”, KSL Consulting, Denmark). The level of infestation was graded on an analog scale (heavy infestation is equal to more than one louse found with a single stroke of the comb, medium infestation is equal to one louse found with the first stroke of the comb, and light infestation is equal to one louse found after several strokes of the comb). In practice, most people with heavy infestation had at least 25 lice of all stages, and some were estimated to have in excess of 500 mobile lice of all development stages present, as well as viable eggs.
Those people with lice who conformed to the study eligibility requirements were conducted through a standard informed consent and assent procedure. All family members over the age of 2 years who had lice and were otherwise eligible could be enrolled.
All participants agreed to be available for the 14-day duration of the study prior to enrolment. Anyone who had a known sensitivity to any component of the products; had used hair bleach, permanent colorants, permanent waves, or undergone treatment with trimethoprim or co-trimoxazole within the past 4 weeks; or who had used a pediculicide within the previous 2 weeks was excluded. Also excluded was anyone with a secondary scalp infection (impetigo), with a chronic scalp condition (e.g., psoriasis), was pregnant or nursing, had participated in a clinical trial within the previous 4 weeks, or had previously participated in this trial.
After consent was taken, baseline demographic data were collected on gender, age, hair characteristics, previous pediculicide use, and success of previous treatments. Appointments were made for subsequent visits to the participants in their homes for treatment and assessments. No payment was offered for participation. Anyone who had lice but was ineligible to participate was offered treatment using 4% dimeticone lotion as a standard of care treatment and to prevent reinfestation of study participants.
Ethics
Ethical approval for the study was granted by Leeds (West) Research Ethics Committee (EudraCT 2007-006190-87). The study was conducted in conformity with the principles of the Declaration of Helsinki and of European Union Directive 2001/20/EC. Prior to giving consent, all participants stated that they understood the purpose and requirements of the investigation after having read the participation information booklet. Parents or guardians gave written consent for children younger than 16 years. Children also provided written or verbal assent, according to age, witnessed by the parent or guardian.
Treatments
Coconut and anise spray (Paranix spray/Lyclear SprayAway, Omega Pharma NV, Nazareth, Belgium; fractionated coconut oil (caprylic capric triglyceride), propan-1-ol, anise oil (from star anise), and ylang-ylang flower oil, the proportions of which are proprietary information) was supplied in 60-ml plastic bottles with a finger pump spray head. The permethrin lotion was supplied as 100-ml glass bottles with a sprinkler opening containing an alcohol solution with 430 mg per 100 ml (0.43% w/v) permethrin (permethrin, ethanol, propan-2-ol, water, propylene glycol, and sodium dihydrogen phosphate; InfectoPedicul lotion, InfectoPharm GmbH, Heppenheim, Germany).
In order to ensure a correct treatment, each of the products was applied in exact conformity with the instructions for use supplied in the package. The coconut and anise spray was applied to dry hair over its full length until wetted. When the permethrin lotion was applied, the hair was first shampoo-washed and then towel-dried, after which, the lotion was applied drop by drop until all the hair was soaked with the fluid to the point of running off. In each case, the investigators spread the fluid through the hair using their fingers to ensure thorough coverage.
The coconut and anise spray was left in place for 15 min before washing out using shampoo and water. The permethrin lotion was left for 45 min, after that period, it was removed by rinsing with water alone. The washing process was performed by carers who were advised of the time to remove the product, which in many cases, while the investigator was still present. They were also advised not to divulge the identity of the treatment to investigators conducting assessments in order to maintain blinding. Those participants, treated using the permethrin lotion, were also asked not to shampoo their hair for 3 days.
For both products, a second treatment was applied 9 days later. Participants were advised not to use nit combs or other pediculicide preparations during the course of the study.
Outcome measures
The primary outcome measure for the study was elimination of infestation, i.e., no lice present, using two applications of the product. Previous studies have shown that it is possible to effect a cure using this treatment regimen but, because the background prevalence of lice in the population is currently high [10, 11], it is possible for participants to be reinfested after the second treatment. To address this problem, an algorithm used in past studies able to distinguish moderate levels of reinfestation from cases of treatment failure [12, 13] was applied to this study also.
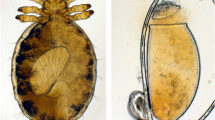
Post-treatment assessments were conducted by dry detection combing using the “PDC” comb on days 2, 7, 11, and 14 after the day of first treatment. The aim of these assessments was to determine whether any lice were still present, and if any were found, they were collected in the case record and examined by microscope to determine the development stage and, if appropriate, the gender. Day 14 assessment was considered the most important, so, a more thorough combing examination was made on this day. A successful treatment was achieved if no lice were found on days 11 and 14, following the second application of treatment. Outcomes of treatment were therefore categorized as cure, reinfestation following cure, or treatment failure.
Sample size
A total sample size of 100 participants (50 in each of the treatment groups) was considered sufficient to detect a difference of 35% between groups in the success rate at 14 days, with 90% power and 95% confidence. This 35% difference represented the difference between a 35% success rate in one product group and a 70% rate in the other group. The actual sample size required was 47 per group, so, recruitment of 50 per group made allowance for dropout.
Randomization and blinding
Treatment allocation was in balanced blocks of ten derived from a computer generated list (http://www.randomization.com, seed 2348, 19 March 2008). Allocation at the point of delivery was made from instruction sheets enclosed in opaque, sealed, sequentially numbered envelopes distributed to investigators in batches of ten. A duplicate set was prepared in case an emergency code break was required. As each participant was enrolled, the investigators selected the next available numbered envelope available to them from the allocation. Randomization was by individual, so, when more than one member of a family was enrolled, it was possible for them to receive different treatments.
Application of treatment could not be blinded due to the different physical and chemical natures of the study treatments. This study was therefore single-blinded with post-treatment assessments performed by different investigators unaware of which treatment products had been used (assessor blinded).
Statistics
Statistical analyses were performed by an independent statistical consultant. Fisher exact tests were used for presence/absence variables. Differences in success rates were measured by the 95% confidence interval (CI) calculated using a normal approximation to the binomial distribution. Quantitative variables were compared by using an unpaired t test or the Mann–Whitney U test.
Results
Participants
This study was performed between March and July 2008 in the counties of Cambridgeshire and Suffolk, UK. During this time, 139 people from 49 households were screened for head louse infestation, and a further 117 household members either declined screening or were unavailable. Our aim was to eliminate lice from each household to minimize the risk of reinfestation, so, any person who had head lice but was ineligible to join the study was offered a standard of care treatment (Hedrin® 4% lotion) for self-administration. The most common household sizes were six (23 participants) or four (20 participants). From those found infested, consent to participate was obtained for 85 children and 15 adults between the ages of two and 49, median 10 years. Most participants (78) lived in households with more than one family member participating in the study, ten families having two participants in the study, 12 families three participants, two families four, and one family each having five and seven participants.
The study group was divided equally between the two treatments (50 per group), and 96 participants completed the study (Fig. 1). Two dropped out from the permethrin lotion group, requesting a rescue treatment following day 6 assessment on ground of lack of efficacy. One participant from the same family was lost to follow-up from the coconut and anise spray group, and one child from the spray group was excluded from per-protocol analysis because the wrong second treatment was applied. Data from these participants were included in the intention to treat analyses. All other participants had complete data sets with two treatments 9 days apart and follow-up checks on days 2, 7, 11, and 14.
Demographic data
Table 1 shows that there were no differences between the groups in respect of age; gender (in both groups, the majority were female); hair length, thickness, dryness/oiliness, or degree of curl; intensity of infestation; or previous experience using head louse products. There was also no difference with regard to medical history.
Outcomes
The main outcome analysis was the comparison of rates of cure or reinfestation after cure in the total population of 100 participants analyzed. According to these criteria, success was achieved by 21/50 (42.0%) of the participants in the permethrin lotion group and by 41/50 (82.0%) of the participants in the coconut and anise spray group. In both groups, all outcomes were counted as cures (no lice following the second treatment), with only one case of reinfestation in each. The difference in rate of success between the two treatments was estimated as 40.0% (95% CI of 22.5% to 57.5%) which meant that the coconut and anise spray was highly significantly (p < 0.001) more effective than permethrin lotion in the population tested.
Elimination of protocol violators from the analysis gave per-protocol success rates of 44.7% for the permethrin lotion group and 83.3% for the coconut and anise spray group, a difference of 39.6%, which was also highly significant (p < 0.001).
Secondary analyses
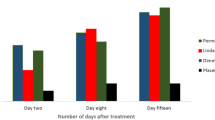
In both treatment groups, some lice were found after the first application of treatment. However, the numbers of lice on each day and the range of developmental stages recovered at each of the assessments were generally greater in the permethrin lotion treated group compared with the coconut and anise spray treated group (Table 2). Examination for the presence of live lice on days 2 and 7, which is related to immediate activity of the treatments and to the ability of the treatments to inhibit louse eggs from hatching, found that 35 (70%) of the participants in the permethrin lotion group and 26 (52%) of the participants in the coconut and anise group had lice at one or more developmental stages on either of these two days. In most cases, these lice were newly emerged nymphs. In the group treated using the coconut and anise spray, the number of people with lice approximately doubled between days 2 and 7 due to hatching of eggs, although the actual number of young nymphs found on participants treated using the spray was significantly lower than on those treated using permethrin lotion (p < 0.05), which indicates that it was more effective to prevent louse eggs from hatching than the permethrin lotion. This means that for both treatments, the second application is generally necessary for elimination of infestation because some louse eggs may not be adequately coated with product during the treatment process. However, 16 (32%) of those treated using permethrin lotion showed all developmental stages of lice on one or both assessment days following the first treatment, compared with just two (4%) of those treated with the spray, indicating that the efficacy of the permethrin product was significantly lower (p < 0.01) and possibly affected by resistance to the insecticide.
All participants treated using permethrin lotion reported not shampooing hair until at least 3 days after treatment. Of these, 27/50 (54%) had not shampooed their hair by day 6 examination. In the per-protocol group, a non-significant trend was found in which those who delayed shampoo use until day 6 (9/25 = 36%) were less likely to be cured than those who shampooed between days 3 and 6 (12/23 = 52%).
The quantity of treatment applied varied with the thickness (density) and length of the hair on each participant, longer and/or thicker hair requiring more product than shorter and/or finer hair. If required, a second bottle of product was available for use on long or thick hair in order to ensure adequate coverage, but in practice, this was found to be unnecessary.
Weighing of the bottles before and after treatment allowed an estimation of the quantity of product applied at each treatment. Generally, approximately twice as much permethrin lotion was used as coconut and anise spray. Mean estimates of permethrin lotion used were 46 g (range from 13.8 to 85.1) for the first application and 44 g (range from 6.7 to 84.2) for the second application. Quantities of coconut and anise spray used were 30.6 g (range from 8.9 to 49.5) for the first application and 25.7 g (range from 6.8 to 49.7) for the second application.
The two products were comparable in their ease of application and of spreading the preparations through the hair. However, there were some significant differences between the products with regard to the feeling of the product on the hair and scalp. The coconut and anise spray was more likely to feel itchy or warm rather than cool (p < 0.01). The odor of the spray was considered strong compared with that of the lotion (p < 0.001) but was acceptable for both products, and the spray was considered more difficult to wash out, mainly because the hair was greasier after use (p < 0.001). Nevertheless, a majority of participants said they would prefer to use the spray again compared with the lotion (86% vs 58%, p < 0.004).
Adverse events
There were 55 adverse events reported, and 37 participants reported one or more adverse events, 20 in the permethrin lotion group, and 17 in the coconut and anise spray group. Of these, 44 adverse events were recorded in 33 participants in relationship to study treatment. The remainder (11 events) were related to concomitant illness or minor accidents. In the permethrin lotion group, 12 of the 50 participants analyzed had a single adverse event, six had two adverse events, one had three adverse events, and one had four events (20 participants experiencing an adverse event and 31 adverse events in total). In the coconut and anise spray group, 12 of the 50 participants had one adverse event, three had two adverse events, and two had three adverse events (17 participants with an adverse event and 24 adverse events in total).
Adverse events related to treatment were mostly stinging or burning sensations on the scalp or neck or both during and after treatment. Most of these events were apparently related to intensity of infestation and the number of bite reactions on the scalp. However, it was clear that the cause of the adverse events in each case was the level of alcohol in the products, with a possible effect from essential oil in the spray, these components being likely irritants to broken or excoriated skin. Such events were more or less evenly distributed between the two treatment groups.
No subject had a serious adverse event, and there was no evidence of any difference between groups in respect of frequency, outcome, action taken, relationship to study treatment, relationship to concomitant illness or drug, or severity.
Discussion
We have found that coconut oil and anise spray gave superior efficacy for elimination of head louse infestation than 0.43% permethrin lotion, both products applied on two occasions 9 days apart.
Coconut and anise spray is a class I medical device that acts by coating lice in an oily film, obstructing the respiratory system in a similar way to several other medical device products for control of head lice [12, 14]. However, as the application time is relatively short, it is likely that triglycerides persisting on the hair and lice subsequent to washing contribute to the efficacy. As the mode of action appears to be mainly due to the physical effects of coconut oil coating the louse surface, it is not envisaged that lice may develop resistance to the product unlike pharmacologically active insecticides like permethrin. Resistance to permethrin has been shown to cause treatment failure in the UK [10, 15]. We would therefore expect to encounter a proportion of cases in every community with lice resistant to permethrin.
In practice, we found approximately one third of our participants did not respond to treatment using permethrin lotion, and that the alcohol in the lotion does not appear to contribute to the activity of the product to ensure its effectiveness in use. In contrast, the coconut and anise spray was not only effective in most households, even where other family members treated using permethrin had experienced treatment failure; it was also more cost effective. Based on the weights of product used in our study, we estimate that for an average application of 0.43% permethrin lotion, the cost would be approximately €10.94 per application (€2.43 per cl). In contrast, the cost of an average application of coconut and anise spray would be approximately €9.64 (€3.32 per cl).
We were unable to detect any age-related trend for obtaining a successful treatment using either product, which indicates that success, or lack of it, in eliminating lice was not related to a likely increased risk of reinfestation in children as they played with their peers.
We found a higher incidence of “stinging at the site of application” adverse events to treatment in this study than in our previous investigations [12, 13], and this can only be attributed to alcohol components of treatment. However, none of the experiences lasted more than about 20 min and ceased when the alcohol had evaporated. We did not observe any subsequent Draize-type reactions. There are no reported incidents of sensitization or allergy caused by any of the ingredients of either product, and we found no evidence such reactions in our study.
Both previous studies evaluating the coconut and anise spray, one in Israel [8] and the other in Italy [9], used three applications with 5 days between each, and one study [9] also required all parents/carers to comb the hair with a nit comb to remove eggs and lice daily. Therefore, the level of intervention in those studies was greater than we employed, yet the intention to treat cure rate for the Israeli study (60/70, 85.7%) was not significantly different from our result using only two applications 9 days apart. We cannot draw a comparison with the Italian study because the combing component of treatment clearly contributed much of the successful outcome as nearly all participants, including those treated using a relatively weak comparator product, were effectively cured by removal of all lice and eggshells before the second application of product [9].
Physiological resistance to insecticide-based products is now considered widespread in Europe and North America [2–8, 11, 13–15] and affects not only pyrethroid insecticides like permethrin but also the organophosphate malathion [2, 3, 5, 8] and previously used chemicals like the cyclodiene hexachlorocyclohexane (HCH or lindane). The extent of this resistance varies not only with the country but also with the region, district, town, or even street [2, 3, 5, 8, 13]. Consequently, there are no clear figures indicating the proportion of cases in a population likely to experience resistance, but resistance in some form has been found in more than 80% of lice in some populations [8, 13], or to influence the outcome of treatment in between 70% and 90% of cases of infestation [3–5, 8] in affected areas. As a result, physically acting preparations like coconut and anise spray are now the treatment of choice for many consumers, especially as they are not affected by resistance, and there is no recognized mechanism whereby lice might develop tolerance of these materials. As a result, we believe that coconut and anise spray should remain a viable treatment option for most people well into the future.
References
Burgess IF (1999) Dermatopharmacology of antiparasitics and insect repellents. In: Gabard B, Elsner P, Surber C, Treffel P (eds) Dermatopharmacology of topical preparations. Springer-Verlag, Heidelberg, pp 157–178
Burgess IF, Brown CM (1999) Management of insecticide resistance in head lice, Pediculus capitis (Anoplura: Pediculidae). Proceedings of the 3rd International Conference on Control of Urban Pests, Prague, pp 249–253
Burgess IF, Lee PN, Matlock G (2007) Randomised, controlled, assessor blind trial comparing 4% dimeticone lotion with 0.5% malathion liquid for head louse infestation. PLoS ONE 2(11):e1127. doi:10.1371/journal.pone.0001127
Burgess IF, Lee PN, Brown CM (2008) Randomised, controlled, parallel group clinical trials to evaluate the efficacy of isopropyl myristate/cyclomethicone solution against head lice. Pharm J 280:371–375
Downs AMR, Stafford KA, Coles GC (1999) Head lice: prevalence in schoolchildren and insecticide resistance. Parasitol Today 15:1–3. doi:10.1016/S0169-4758(98)01361-1
Durand R, Millard B, Bouges-Michel C et al (2007) Detection of pyrethroid resistance gene in head lice in schoolchildren from Bobigny, France. J Med Entomol 44:796–798. doi:10.1603/0022-2585(2007)44[796:DOPRGI]2.0.CO;2
Hemingway J, Miller J, Mumcuoglu KY (1999) Pyrethroid resistance mechanisms in the head louse Pediculus capitis from Israel: implications for control. Med Vet Entomol 13:89–96. doi:10.1046/j.1365-2915.1999.00141.x
Kristensen M (2005) Identification of sodium channel mutations in human head louse (Anoplura: Pediculidae) from Denmark. J Med Entomol 42:826–829. doi:10.1603/0022-2585(2005)042[0826:IOSCMI]2.0.CO;2
Mumcuoglu KY, Miller J, Zamir C et al (2002) The in vivo pediculicidal efficacy of a natural remedy. Isr Med Assoc J 4:790–793
Oliveira FAS, Speare R, Heukelbach J (2007) High in vitro efficacy of Nyda®L, a pediculicide containing dimeticone. J Eur Acad Dermatol Venereol 21:1325–1329. doi:10.1111/j.1468-3083.2007.02258.x
Picollo MI, Vassena CV, Casadio AA et al (1998) Laboratory studies of susceptibility and resistance to insecticides in Pediculus capitis (Anoplura; Pediculidae). J Med Entomol 35:814–817
Scanni G, Bonifazi E (2005) Efficacy and safety of a new non-pesticide lice removal product. Eur J Pediatr Dermatol 15:49–52
Thomas DR, McCarroll L, Roberts R et al (2006) Surveillance of insecticide resistance in head lice using biochemical and molecular methods. Arch Dis Child 91:777–778. doi:10.1136/adc.2005.091280
Yoon KS, Gao JR, Lee SH et al (2003) Permethrin-resistant human head lice, Pediculus capitis, and their treatment. Arch Dermatol 139:94–1000. doi:10.1001/archderm.139.8.994
Yoon KS, Gao JR, Lee SH et al (2004) Resistance and cross-resistance to insecticides in human head lice from Florida and California. Pestic Biochem Physiol 80:192–201. doi:10.1016/j.pestbp.2004.07.008
Acknowledgements
This study was supported financially by Omega Pharma NV, Nazareth, Belgium, which played no active role in the design of the study, interpretation of the results, or the writing of the manuscript. We wish to thank Dr Marc Dams and Isabelle Dedeken for administrative support. Thanks also to Laurence Noiroux of S-Clinica, Brussels, Belgium for statistical analyses. Investigation team members who contributed to the study but were not named as authors were Ian Jones, Audrey Pepperman, and Christine Sullivan. Medical supervision for clinical queries was provided by Dr Paul Silverston.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Burgess, I.F., Brunton, E.R. & Burgess, N.A. Clinical trial showing superiority of a coconut and anise spray over permethrin 0.43% lotion for head louse infestation, ISRCTN96469780. Eur J Pediatr 169, 55–62 (2010). https://doi.org/10.1007/s00431-009-0978-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-009-0978-0