Abstract
Pediculosis capitis occurs worldwide. Children in the age group of 5–13 years are the ordinary victims. Population-based studies show that the prevalence of pediculosis is 1.6–13.4% in various regions of Iran. In this observer-blinded trial, we conducted a study to evaluate the comparative efficacy and safety of permethrin 1% and lindane 1% shampoos and dimeticone 4% lotion to cure head lice infestation in children aged 7–13 years in female primary schools in Ahvaz City, Iran. Children with head lice were randomized to receive each treatment. Two applications of permethrin 1% or dimeticone 4% were done, 1 week apart. However, lindane 1% was used just once for treatment cases. Data analysis was done using SPSS software. Recovery differences between the groups were tested using the chi-squared test. Four hundred forty-four louse-infested schoolgirls were randomly treated with them. Permethrin, lindane, dimeticone, and placebo produced the recovery rates 56.8, 31.5, 51.4, and 10.8% on day 2 post-treatment, respectively. Cure rates were in the permethrin group on days 8 and 15, respectively, 69.4 and 90.1%. The success rates were in the lindane group on days 8 and 15, respectively, 73 and 86.5%. The success rates were in the dimeticone group on days 8 and 15, respectively, 60.4 and 94.6%. It is recommended dimeticone lotion (4%) as a very effective and safe pediculicide for pediculosis control. With proper application, dimethicone can rapidly cure head lice infestation with minimal reinfestation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Head lice are external and obligatory parasites of humans and nymphs and adults feed on the blood of both sexes. Infestation with the head louse is a significant public health challenge involving children aged between 5 and 13 years old (Moosazadeh et al. 2015; Pilger et al. 2010). It is caused by Pediculus capitis De Geer, 1767 (Phthiraptera: Pediculidae), found out on the scalp and hair, and is commonly transmitted via direct contact, or through indirect contact (devices such as comb, towels, and infested clothing) (Kassiri and Esteghali 2016; Burkhart and Burkhart 2006). The main risk factors for the spread of head lice are the following: use of shared clothing and bedding, hair washing habits, number of children in the family, local habits, social contacts, lack of health care services in schools, socio-economic status. Pediculosis capitis is widespread all over the globe but is more prevalent in developing countries. Unfortunately, in some parts of Iran, different factors, including excessive population growth, urbanization, marginality, and establishment of satellite towns with minimum health and welfare facilities, have contributed to the emergence and prevalence of head lice infestation (Kassiri et al. 2015). Every day, a head louse can lay up to 10 nits, provides a lifetime potential of till 300 nits in its life span, i.e., 30–40 days. A new generation of human head louse is produced in 18–24 days (Mac-Mary et al. 2012). The female head louse pastes the nits to the hair (nearly 1–3 cm from the scalp), with priority on behind the ears or the neck, using powerful water-proof glue (Kassiri et al. 2020).
Head louse prevalence rates of 5.8–35% have been reported from different areas in the world (Amirkhani et al. 2011). Notwithstanding spending a lot of annual budget (Salimi et al. 2020), head lice infestation is as yet common in multitude regions of Iran (Firoozfar et al. 2019; Nejati et al. 2018; Adham et al. 2020). In Iran, its prevalence was reported between 1.6 and 13.4% from certain regions with various socio-economic and demographic situations (Amirkhani et al. 2011).
The head louse infestation can cause secondary microbial infections (like impetigo), discomfort, pruritus, lymphadenopathy on the back of the neck and ears, sleep loss, and irritation (Kassiri et al. 2020). By the way, it can occasionally cause mental disturbances (emotional distress, anxiety, and feelings of being ashamed), because children imagine that they are the result of being filthy. By the way, pediculosis capitis can cause social stigma, psychological distress, and absence from school and work for both schoolchildren and their parents (Kassiri and Esteghali 2016; Oh et al. 2010; Roux and Raoult 1999 ). Head lice have been reported to carry Rickettsia prowazekii in Asia, South America, and Africa. In addition, evidences have been indicated from Ethiopia that Bartonella quintana and Borrelia recurrentis were present in 7% and in 23% of head lice, respectively (Veracx and Raoult 2012; Angelakis et al. 2011; Boutellis et al. 2013).
In fight with pediculosis capitis, physical techniques such as combing, removing the lice from hair, personal hygiene, health education, shaving, separation of infected patients, availability to sufficient healthy water resources, collaboration of teachers and parents, and quick detection and treatment of cases have an important role (Shahraki et al. 2013).
Multitude researches have been done on the assessment of various formulations of chemical pediculicides in the treatment of head louse infestation in various parts of the globe (Karami Jooshin et al. 2019). The results obtained from different studies display that pediculicides accessible in the types of formulations have different rates of efficacy in different regions of the world, whereas the findings acquired in a particular region or country have no worthiness for another region or country (Shahraki et al. 2013; Zahirnia et al. 2001). Selecting an appropriate pediculicide formulation depends on efficacy, priority of the infected patients, expense, and access to a particular production. Shampoo for treatment of head lice is well embraced among infected people, easy to utilize and shows greater killing nits efficacy than lotion formulations (Shahraki et al. 2013).
In the first-line head louse infestation therapies, permethrin (1%, an organophosphate, toxicity at LD50 = 2000 mg/kg), there is increasing resistance (Canyon and Speare 2007). The short-generation stage of P. capitis, the contact of whole life-cycle steps, and any used pediculosis capitis treatment are providing factors to resistance development. The main medicine is commonly permethrin, which has been found to have the greatest efficacy and the greatest of safety , but the general abundance of local irritating symptoms observed with permethrin ranges from 2.1 to 5.9%. The second-line pediculicides, lindane (1% gamma benzene hexachloride, an organochloride, dermal toxicity at LD50 = 900–1000 mg/kg ), possess worries and limitations regarding unpleasant odor, flammability, and safety. A second-line medication means it may just be prescribed when the rest of first-line medications cannot be applied or have closed out. In Europe since 2007, medicines comprising lindane have been removed from the pharmacies (Mac-Mary et al. 2012; Pariser et al. 2012). Resistance to lindane has been reported (Brandenburg et al. 1986).
Dimeticones (linear polydimethylsiloxanes of differing chain length) are silicone oils with a little surface tension and characteristic creeping and diffusing features (Heukelbach et al. 2008). They are a new class of pediculicides with a physical mode of action. Dimeticone shampoo is a new medicine, with no normal insecticide function. It possesses 4% long-chain linear silicone in a fugacious silicone base (cyclomethicone). Both compounds are utilized broadly in toiletries and cosmetics, and a shorter chain dimeticone is applied as an anti-flatulent for infant stomach ache. Dimeticon is an odorless, clear liquid substance which is used in the same way as other shampoos for pediculosis capitis, by wearing scalp and the full length of the hair. The compound becomes dry by evaporation of the cyclomethicone solvent (Burgess et al. 2005). The dimeticone pediculicide is safe and very effective. Because of its physical mode of action (discontinuity of the louse’s oxygen supply of the central nervous system), the development of resistance is improbable (Heukelbach et al. 2008). Lately, the use of herbal shampoos has been proposed due to increased resistance of the head lice to chemical shampoos (Watcharawit and Soonwera 2013). Treatment with any shampoo needs reusing application after 7 days to destroy eggs (Brandenburg et al. 1986).
The efficacy of anti-head lice compounds varies largely in field status. Shahraki et al. 2013 found that shampoo treatment on 1242 head louse–infested girls in primary schools at Yasuj, Iran, resulted in only 52.9% overall recovery. With lindane, it was 50.96% and with permethrin 54.29% (Shahraki et al. 2013). Two applications of dimeticone or 1% permethrin was applied, 1 week apart, on 145 children aged 5–15 years with pediculosis capitis in Brazil. Overall cure rates were as follows: day 2 – dimeticone 94.5% and permethrin 66.7%; day 7 – dimeticone 64.4% and permethrin 59.7%; day 9 – dimeticone 97.2% and permethrin 67.6% (Heukelbach et al. 2008). Tashakori et al. (2018) aimed to compare two pediculosis capitis control methods, vinegar wet combing and dimethicone lotion (4 %) with permethrin shampoo (1%) on schoolchildren infested with head lice in Mashhad City, Iran, during 2015 and 2016. Application times of permethrin, dimethicone, and vinegar were 8–10 min, 8 h, and 20-30 min, respectively. The dimethicone treated group showed the largest control levels (86% and 74%). The therapeutic rates at first endpoint were 86, 64.2, and 60.8%, and at the second endpoint were 74, 45.3, and 45.1% for dimethicone, permethrin, and vinegar, respectively (Tashakori et al. 2018). In a study in governmental primary schools in Kerman, southern Iran, the 721 children with head lice infestation were treated with lindane shampoo (1%). At 2 weeks after the primary therapy, the cure rates were 49% (Tashakori et al. 2018).
To the best of our knowledge, no comprehensive study has so far focused on the treatment of head lice infestation in Ahvaz County, Khuzestan Province, southwestern Iran. Due to the importance of fighting the spread of infestation to prevent its harmful health, economic, and social outcomes, this study was done. This study was carried out to compare the effect of 1% permethrin (in a 60-mL tube, manufactured by Gilaranco, Rasht, Iran), 1% lindane (in a 60-mL tube, manufactured by Gilaranco, Rasht, Iran), and 4% dimeticone, a lotion with no conventional insecticide activity (in a 60-mL tube, manufactured by Reyhan, Tehran, Iran) on pediculosis capitis of 7–13-year-old students (median age: 7 years ) in girls’ primary schools in Ahvaz City.
Materials and methods
This research was carried out in Ahvaz (31° 192 133 N 48° 402 093 E) as a part of the central coordination Khuzestan (31.3273° N 48.6940° E), capital of Khuzestan, a southwestern province of Iran. Given its hot and humid climate and high population density, Khuzestan Province (Iran) is considered a favorable environment for lice population growth. Ahvaz is a county with a hot and arid climate located at the center of Khuzestan Province. Ahvaz area is estimated to be 528 km. Its elevation is 17 m above sea level. In 2016, its population was 1,302,000. Ahvaz had the world’s worst air pollution according to a survey by the World Health Organization in 2011. It is a subtropical area and the environmental temperatures reach its maximum during March to September.
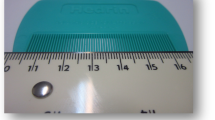
This randomized, double-blinded clinical trial was conducted during autumn 2015–2016. At the start, a training program was distributed among all individuals discussing methods of prevention and control and so directions for use of shampoos. The training program was done by using methods of lecture with asking and answering during the two sessions and each session of 20 min and distribution of pamphlets. Several data (including demography data) were recorded in a questionnaire that was made by researchers using interviews. We included students in the study who had not taken any medication in the previous 3 weeks. We also had to make sure that these students would not take any medication during treatment. Exclusion criteria were subjects affected by scalp disorders (such as eczema, impetigo, dermatitis, and psoriasis), treatment with a lousicide within 2 weeks prior to the trial, history of irritation to hair care products or lousicides, use permanent wave, hair dyes, bleaches, or relaxing solutions within the research or during the previous 2–3 weeks, and whose parents assured not to apply any other head louse infestation treatment during the study. The recognition of pediculosis capitis was confirmed by visual clinical trial of hair and scalp (with a × 10 magnifying lens), using a head lice detection comb, for the presence of each of the adult, nymph, or nit stages of the head louse, under the supervision of the health specialists and the investigators (Kassiri et al. 2020). Because adult and nymph lice are very small and move fast and avoid light, they may be difficult to find. They are flat, wingless, and gray insects about 2–4 mm in length. Nits are tiny and translucent. Applying a fine-toothed comb may facilitate the diagnosis of live head lice.
The method of infestation detection was that each person’s hair was exposed to natural light for 7 min. The emphasis was on the hair behind the ears and neck. All individuals that met inclusion criteria received treatment. Cure was defined as the absence of live adult lice/viable nymphs/hatching nymphs/nits (one or more) on 2, 8, and 15 days after the first post-application, and signs are usually associated with head lice infestation. The outcome measure was the cure rate, defined as the percentage of patients cured after application of the first treatment.
The sample size was calculated as per the following formula:
Considering loss to follow-up (14%) during the study period, a study size of about 444 participants was considered to be sufficient. Therefore, the population included 444 cases with head lice infestation that were confirmed through interview and clinical inspections. They in 31 girls’ primary schools were randomly treated with the shampoos (111 students with lindane 1%, 111 students with permethrin 1%, and 111 students with dimeticone 4%). Meanwhile, one hundred eleven infested schoolgirls were treated with placebo shampoo. According to the protocol (Tashakori et al. 2018), 1% permethrin was applied to the clean-washed wet hair and scalp for 10 min, followed by thorough rinsing with water and repeated fine tooth combing. On the other hand, 4% dimeticone was applied to dry hair and scalp and kept for 8 h (overnight) to dry naturally, followed by steps of rinsing and fine tooth combing. Meanwhile, 1% lindane was applied to wet hair, left for 4 min, and thereafter washed out in the same method as dimeticone and permethrin. Treatment with permethrin shampoo and dimeticone lotion was repeated after 1 week. But, treatment with lindane was performed only once. All compounds were applied onto the hair from the hair shafts to the tips, and an ordinary comb was used to spread them uniformly. At first, the head was washed with ordinary shampoo and dried. Then, the hair again was washed and massaged using a formulation containing anti-lice. All personal items, such as scarves, caps, combs, clothing, bedding, and brushes, had to be deloused as well (by washing items on a hot cycle or by deep-freezing). Moreover, parents were warned not to remove head lice by combing after the therapy. Clinical pathology included the presence of inflammation, irritation, or itching of scalp and ocular irritation. The severity of itching was evaluated in mild, moderate, and severe.
Standard statistical method (chi-squared test) was applied in order to analyze the information. Statistical analysis of findings was done using SPSS software version 20.0. Differences between groups were noticed to be statistically significant when P values were less than 0.05.
Ethics statement
The study was approved by the Committee of Ethics in Research, Ahvaz Jundishapur University of Medical Sciences and registered as R.AJUMS.REC.1394.558.
This trial was registered with Iranian Registry of Clinical Trials (Registration ID in IRCT: IRCT2016013026266N1). This project was done in accordance with the ethical principles and the national norms and standard for conducting medical research in Iran.
No photographs or names of cases are found in the paper. The confidentiality of the records of patients was assured. Participation was fully voluntary and written signed informed consent (after getting the data and after a verbal description of the objectives and the method of the research) was gotten from all the parents of eligible children under study. There was no consequence for non-participation. The college research review committee revised the paper according to the rule and regulation. Ahvaz Health Services Center administrative authorities were informed about the study and their consent was obtained with the letter. The students in the control group were all treated with medication (4% dimeticone or 1% permethrin) at the end of the study.
Results
We randomly assigned 444 people aged 7 to 13 years in 8 girls’ primary schools to receive pediculicide and placebo shampoo. Of the 441 patients, 14.6, 8.6, 22.5, 28.6, 13.1, 10.4, and 2.2% were included at the ages of 7, 8, 9, 10, 11, 12, and 13 years old, respectively. According to the educational grades, 15.3, 10.1, 22.5, 27.7, 14.9, and 9.5% were in grades 1, 2, 3, 4, 5, and 6, respectively. The mean age in permethrin, lindane, dimeticone, and control groups was 9.75, 9.82, 9.58, and 9.14, respectively. The study participants were in different educational levels, i.e., grades 1 (15.3%), 2 (10.1%), 3 (22.5%), 4 (27.7%), 5 (14.9%), and 6 (9.5%). Based on the mothers’ educational level, 13.3% were illiterate, 59.9% with primary/elementary education, 22.7% with diploma, and 4.1% with university education. Also, 7, 55.6, 27.5, and 9.9% of the fathers of infested children were illiterate or had primary/elementary education, diploma, or academic literacy, respectively. In terms of the occupation of the fathers of the children, 4.1, 54.5, 16.2, 10.8, 1.1, 9.7, and 3.6% were unemployed, self-employment, government employee, diver, military, worker, and etc., respectively.
The findings showed significant differences among the treated groups of cases on days 2 (x2 = 75, P < 0.001), 8 (x2 = 80, P < 0.001), and 15 (x2 = 219.5, P < 0.001) post-application. On the other hand, permethrin outcome was not significantly different from that of dimeticone on day 2 after post-application (x2 = 0.63, P = 0.42), which means the similar success of these two pediculicides. The results showed a significant P value (x2 = 8.98, P = 0.003) for dimeticone treatment compared with application of lindane on day 2 post-application. The result of chi-squared test at primary endpoint indicated significant P value which prove meaningful difference between permethrin and lindane (x2 = 14.3, P < 0.001). The statistical analyses showed no meaningful difference between permethrin and lindane (x2 = 0.35, P = 0.55), also permethrin and dimeticone (x2 = 1.97, P = 0.16), as well as lindane and dimeticone (x2 = 3.97, P = 0.43) on day 8 post-treatment. Furthermore, the statistical analysis indicated no significant difference between permethrin and lindane (x2 = 0.7, P = 0.4), also permethrin and dimeticone (x2 = 1.59, P = 0.21), as well as lindane and dimeticone (x2 = 4.26, P = 0.39) at the third endpoint on day 15 post-treatment (Table 1).
Permethrin, lindane, and dimethicone groups recorded the best recovery rate of 90.1, 86.5, and 94.6% on day 15 post-application, respectively. Lindane shampoo recorded the minimum success rate of approximately 31.5% on day 2 post-treatment. Permethrin, lindane, and dimeticone groups recorded the best cure rates of 56.8, 73, and 94.6% at the first, second, and third endpoints of days 2, 8, and 15 post-application, respectively (Table 1 and Fig. 1).
The highest level of recovery rates was observed among primary school girls in grades 2 (100%), 3 (100%), and 2/4 (100%) for permethrin, lindane, and dimeticone on day 15 post-application, respectively. Table 2 shows recovery rates in relation to class/grade. Moreover, the highest percentage of efficacy rates was observed in grades 1, 2, and 6 children (Table 3).
Treatment-related events included itching in the scalp (15 in permethrin group, 10 in lindane group, and 13 in dimeticone group), inflammation/irritation in the eyes (1 in permethrin group, 11 in lindane group, and 0 in dimeticone group), and inflammation/irritation in the scalp (2 in permethrin group, 10 in lindane group, and 1 in dimeticone group) (Table 4).
Degree of itching (on an ordinal scale severe, moderate, and mild) was reduced in both treatment groups lindane and dimeticone during the study period. Bacterial infection and cervical lymphadenopathy were not observed during the study. The symptoms associated with pediculosis like itch, flakiness, and scalp dryness/irritation were largely and quickly reduced by the therapy.
Discussion
Notwithstanding the application of various chemical agents for the treatment of pediculosis, the prevalence of head lice infestation remains great due to the lack of efficacy of applied lousicides in many countries all over the world (Kassiri et al. 2020; Tashakori et al. 2018). There are various aspects we must figure out when investigating a treatment, like safety, ease of use, price, application guidance, toxicity, mechanism, and prevalence of resistance. The reduced property of pediculicides can be attributed to lice resistance, undesirable use, and inefficient dose-applied formulation (Tashakori et al. 2018; AL-Megrin 2015; Zhu et al. 2016 ). However in the 1980s, pyrethrins were almost 100% effective, but recent researches propose that their efficacy evaluation has reduced until 50%. Similarly, clinical failure measures of more than 50% have been obtained with permethrin in the world (Karami Jooshin et al. 2019; Mac-Mary et al. 2012; Heukelbach and Feldmeier 2004; Maunder 1971). Mumcuoglu et al. (1995) observed a 4-fold decrease in susceptibility to permethrin between 1989 and 1994 (Mac-Mary et al. 2012; Mumcuoglu et al. 1995). Moreover, cross-resistance between several pediculicides like DDT and bioallethrin or permethrin has developed. On the whole, resistance has been reported to insecticides such as malathion, DDT, pyrethroids (permethrin and pyrethrins), sevin, and lindane (Mac-Mary et al. 2012; Mumcuoglu 1999). Resistance to dimeticone (silicone compound) is improbable due to its physical mode of action (Verma and Namdeo 2015). At the same time, reinfestation is frequent even with therapies that demonstrate successful if relatives of the cured individual are not cured simultaneously. This issue is especially common in small societies, where persons are in close contact for long term. Actually, reinfestation remains an important risk factor of heal lice infestation as determined by investigators (Ferrara et al. 2013; Saghafipour et al. 2017; Moradiasl et al. 2018).
In this study, we purposed to compare recovery of three pediculicides to control pediculosis among 333 primary school girls in Ahvaz City. A control group of 111 girls from primary levels was treated with placebo shampoo. Our findings show a 86.5–94.6% decline in pediculosis patients following the application of pediculicides. Overall cure rates were 46.6% on day 2, 67.6% on day 8, and 90.4% on day 15 post-treatment. Permethrin shampoo produced a 90.1% recovery, lindane shampoo a 86.5% recovery, and dimeticone lotion a 94.6 recovery on day 15 post-treatment. In contrast to the high cure rates on day 15, cure rates on day 8 post-application in the permethrin, lindane, and dimeticone groups were 69.4%, 73%, and 60.4%, respectively. These findings are in the range of researches done by Shahraki et al. (2013) (54.21% and 50.96% using permethrin and lindane shampoos, respectively), Brandenburg et al. (1986) (43% using lindane shampoo), Fan et al. (1991) (71% using gamma benzene shampoo), Khazaie (1998) (72.62% using gamma benzene hexachloride shampoo), Stoug et al. (2009) (44.9% using permethrin 1% with combing), Ha et al. (2000) (93.5% using lindane shampoo), Budak et al. (1996) (67.5% with lindane shampoo), and Motovali-Emmami et al. (2008) (49% using lindane shampoo). In a research by Tashakori et al. in Mashhad City, the dimethicone cured group showed the largest control levels (86 and 74%). The success rates at day 7 post-application were 86, 64.2, and 60.8%, and at day 30 post-application were 74, 45.3, and 45.1% for dimethicone lotion, permethrin shampoo 1%, and vinegary shampoo, respectively. Dimethicone was 4.3 times more potent than either of vinegar or permethrin (Tashakori et al. 2018). In a study in Rome (Italy) between April 2008 and June 2008, Ferrara et al. reported, after 7 days of treatment with dimeticone shampoo 4%, 7/23 (30.4%) positive children still had head lice infestation, with a recovery rate of 69.6% (16/23). At 30 days, 26/131 children (19.9%) were infested with head lice (Ferrara et al. 2013). Heukelbach et al. (2008) in their research in Brazil reported that overall cure rates were as follows: day 2 – dimeticone 94.5% and permethrin 66.7%; day 7 – dimeticone 64.4% and permethrin 59.7%; day 9 – dimeticone 97.2% and permethrin 67.6%.
Cases treated with dimeticone lotion stated a less incidence of irritant detrimental effects. Its high cure rate, lack of odor, safety, and relative simplicity of applying make this product an appropriate alternative to conventional therapies. These days, the American Academy of Pediatrics advises permethrin 1% as first-line treatment for head lice infestation (Ferrara et al. 2013). Lindane (gamma benzene hexachloride 1% shampoo) is greatly applied as lousicide in Iran (as the second-line treatment). However, it has limited ovicidal activity. That is why it is important to repeat treatment with lindane. Due to the potentially increasing side effects of lindane, including bone marrow suppression and neurotoxicity, resistance to lindane is common in populations all over the world (Motovali-Emmami et al. 2008). It is important that government officials support and cooperate with school authorities and health services centers for successful and effective control pediculosis in primary and elementary schools. There is an immediate necessity to find novel, safe pediculicides for effective control. Doing training programs by teachers, health services centers, and physicians is useful for pediculosis control.
The limitations of this study were as follows: (I) The sample size was limited to primary school students. (II) Although the families included are felt to represent the social-economic diversity within a county, they were not randomly selected. (III) The role of other factors such as active support by the family members is equally significant and should be addressed in future studies. (IV) One more limitation of our study is the lack of clear guideline for comparative efficacy of pediculicides. (V) The last clear limitation is the relatively high number of excluded cases.
The strengths of this study were as follows: (I) To our knowledge, this study is one of the first studies to describe comparative efficacy of three pediculicides for the treatment of head louse infestation in southwestern Iran. (II) All the parents and evaluators of children instructed to apply the pediculicides accurately, following suitable instructions of use. (III) All evaluators were trained before the study in the technique for head lice assessment (which included combing and detecting head lice in infested cases). (IV) The control group improved the sensitivity of the study design. (V) Their family members were treated with a pediculicide to reduce the occurrence of reinfestation.
The highlights of this study were as follows: (I) Permethrin, lindane, and dimethicone groups recorded the best recovery rate of 90.1, 86.5, and 94.6% on day 15 post-application, respectively. (II) The highest level of recovery rates was observed among primary school girls in grades 2 (100%), 3 (100%), and 2/4 (100%) or permethrin, lindane, and dimeticone on day 15 post-application, respectively. (III) Given the better effects of dimethicone, it is recommended as the drug of choice for head lice infestation control. (IV) The symptoms associated with pediculosis like itch, flakiness, and scalp dryness/irritation were largely and quickly reduced by the therapy.
Conclusions
Based on the results of this study, treatment with pediculicides could be effective in controlling head lice infestation. But given the better effects of dimethicone lotion, it is recommended as the drug of choice for head lice infestation control. Owing to its physical mode of action, the development of resistance is implausible. Educating students about caring for healthy hair and preventing head lice infestation as well as its treatment is absolutely essential. Because infestation spreads so quickly in students and can infest their family, it is recommended that the parents be examined and trained to prevent and treat it.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Adham D, Moradi-Asl E, Abazari M, Saghafipour A, Alizadeh P (2020) Forecasting head lice (Pediculidae: Pediculus humanus capitis) infestation incidence hotspots based on spatial correlation analysis in Northwest Iran. Vet World 13(1):40–46
AL-Megrin WAI (2015) Assessment of the prevalence of pediculosis capitis among primary school girls in Riyadh, Saudi Arabia. Res J Environ Sci 9(4):193–199
Amirkhani MA, Alavian SM, Maesoumi H, Aminaie T, Dashti T, Ardalan T, Ziaoddini H, Mirmoghtadaee P, Poursafa P, Kelishadi R (2011) A nationwide survey of prevalence of pediculosis in children and adolescents in Iran. Iran Red Crescent Med J 13(3):167–170
Angelakis E, Diatta G, Abdissa A, Trape JF, Mediannikov O, Richet H et al (2011) Altitude-dependent Bartonella quintana genotype C in head lice, Ethiopia. Emerg Infect Dis 17(12):2357–2359
Boutellis A, Mediannikov O, Bilcha KD, Ali J, Campelo D, Barker SC et al (2013) Borrelia recurrentis in head lice, Ethiopia. Emerg Infect Dis 19(5):796–798
Brandenburg K, Deinard AS, DiNapoli J, Englender SJ, Orthoefer J, Wagner D (1986) 1% permethrin cream rinse vs 1% lindane shampoo in treating pediculosis capitis. Am J Dis Child 140:894–896
Budak S, Ilhan F, Guruz AY (1996) A comparative study on the efficacy of 0.4% Sumithrine and 1% Lindane in the treatment of Pediculus humanus capitis in Turkey. J Egyp Soc Parasitol 26:237–241
Burgess IF, Brown CM, Lee PN (2005) Treatment of head louse infestation with 4% dimeticone lotion: randomised controlled equivalence trial. BMJ:1–4. https://doi.org/10.1136/bmj.38497.506481.8F
Burkhart CG, Burkhart CN (2006) Safety and efficacy of pediculicides for head lice. Expert Opin Drug Saf 5(1):169–179
Canyon DV, Speare R (2007) A comparison of botanical and synthetic substances commonly used to prevent head lice (Pediculus humanus var. capitis) infestation. Int J Dermatol 46(4):422–426
Fan P, Chung W, Kuo C, Hsu H, Chow C (1991) Present status of head louse (Pediculus capitis) infestation among school children in Yunlin County, Taiwan. Gaoxiong Yi Xue Ke Xue Za Zhi (Kaohsiung J Med Sci) 7:151–159
Ferrara P, Del Bufalo F, Romano V, Tiberie E, Bottqro G, Romani L, Malamisura M, Ianniello F, Ceni L, Mottini G, Gatto A (2013) Efficacy and safety of dimeticone in the treatment of lice infestation through prophylaxis of classmates. Iranian J Publ Health 42(7):700–706
Firoozfar F, Moosa-Kazemi SH, Bahrami A, Ahmed Yusuf M, Saghafipour A et al (2019) Head Lice Infestation (Pediculus humanus capitis) Prevalence and its associated factors, among the Kormanj Tribes in North Khorasan Province. Shiraz E-Med J. 20(2):e80292
Ha YC, Heo JM, Kim HJ, Go GM, Lee SJ, Jeong SH et al (2000) Infestation status of head louse and treatment with lindane shampoo in children of primary school and kindergarten in Chinju-shi, Kyongsangnam-do, Korea. Kisaengchunghak Chapchi (Korean J Arasitol) 38:41–43
Heukelbach J, Feldmeier H (2004) Ectoparasites—the underestimated realm. The Lancet. 363(9412):889–891
Heukelbach J, Pilger D, Oliveira FA, Adak Khakban A, Ariza L, Feldmeier H (2008) A highly efficacious pediculicide based on dimeticone: randomized observer blinded comparative trial. BMC Infect Dis 8:115
Karami Jooshin M, Izanloo H, Saghafipour A, Ghafoori Y (2019) Study on efficacy of 1% permethrin shampoo and 4% dimethicone lotion as pediculicide products used in Iran: a clinical trial. Tehran Univ Med J 77(1):41–46
Kassiri H, Esteghali E (2016) Prevalence rate and risk factors of Pediculus capitis among primary school children in Iran. Arch Pediatr Infect Dis 4(1):e26390
Kassiri H, Kasiri A, Kasiri N, Moeininejad F (2015) Epidemiology and morbidity of head lice infestation in Khorram-shahr County, Iran (2006-2009). J Health Sci Surveillance 3(2):83–87
Kassiri H, Mehraghaei M, Lotfi M, Kasiri R (2020) Head lice prevalence and associated factors in primary schools in Karun County, Khuzestan Province, Iran. Med Sci 24(104):2280–2290
Khazaie F (1998) Survey on knowledge of primary school about pediculosis and comparative evaluation of Gamma-banzene and kopex pediculicides in Arak city. In: Dissertation. Tehran University of Medical Science, Tehran
Mac-Mary S, Messikh R, Jeudy A, Lihoreau T, Sainthillier JM, Gabard B, Schneider C, Auderset P, Humbert P (2012) Assessment of the efficacy and safety of a new treatment for head lice. ISRN. Dermatology 2012:460467
Maunder JW (1971) Resistance to organochlorine insecticides in head lice and trials using alternative compounds. Medical Officer’s 125:27–29
Moosazadeh M, Afshari M, Keianian H, Nezammahalleh A, Enayati AA (2015) Prevalence of head lice infestation and its associated factors among primary school students in Iran: a systematic review and meta-analysis. Osong Public Health Res Perspect 6(6):346–356
Moradiasl E, Habibzadeh S, Rafinejad J, Abazari M, Sadeghieh Ahari S, Saghafipour A et al (2018) Risk factors associated with head lice (Pediculosis) infestation among elementary school students in Meshkinshahr County, North West of Iran. Int J Pediatr 6(3):7383–7392
Motovali-Emmami M, Aflatoonian MR, Fekri A, Yazdi M (2008) Epidemiological aspects of pediculosis capitis and treatment evaluation in primary- school children in Iran. Pakistan. J Bio Sci 11(2):260–264
Mumcuoglu KY (1999) Prevention and treatment of head lice in children. Paediatric Drugs 1(3):211–218
Mumcuoglu KY, Hemingway J, Miller J et al (1995) Permethrin resistance in the head louse Pediculus capitis from Israel. Med Vet Entomol 9(4):427–447
Nejati J, Keyhani A, Tavakoli Kareshk A, Mahmoudvand H, Saghafipour A, Khoraminasab M, Tavakoli Oliaee R, Mousavi SM (2018) Prevalence and risk factors of pediculosis in primary school children in south west of Iran. Iran J Public Health 47(12):1923–1929
Oh JM, Lee IY, Lee WJ, Seo M, SA. SA, Lee SH, et al. (2010) Prevalence of pediculosis capitis among Korean children. Parasitol Res 107(6):1415–1419
Pariser DM, Meinking TL, Bell M, Ryan WG (2012) Topical 0.5% ivermectin lotion for treatment of head lice. N Engl J Med 367(18):1687–1693
Pilger D, Heukelbach J, Khakban A, Oliveira FA, Fenglerc G, Feldmeiera H (2010) Household-wide ivermectin treatment for head lice in an impoverished community: randomized observer-blinded controlled trial. Bull World Health Organ 88:90–96
Roux V, Raoult D (1999) Body lice as tools for diagnosis and surveillance of reemerging diseases. J Clin Microbiol 37(3):596–599
Saghafipour A, Nejati J, Zahraei-Ramazani A, Vatandoost H, Mozaffari E, Rezaei F (2017) Prevalence and risk factors associated with head louse (Pediculus humanus capitis) in Central Iran. Int J Pediatr 5(7):5245–5254
Salimi M, Saghafipour A, Hamidi Parsa H, Khosravi M (2020) Economic burden associated with head louse (Pediculus humanus capitis) infestation in Iran. Iran J Public Health 49(7):1348–1354
Shahraki GH, Fararooie M, Karimi A (2013) Controlling head lice in Iranian primary schools for girls. Asian Biomed 7(2):281–285
Stoug D, Shellabarger S, Quiring J, Gabrielsen AA Jr (2009) Efficacy and safety of spinosad and permethrin crème rinses for pediculosis capitis (head lice). Pediatrics 124:e389–e395
Tashakori G, Dayer MS, V ( M–G (2018) Comparative efficacy of three control protocols of head lice (Pediculus Humanus Capitis) infesting schoolchildren in Mashhad City, Iran. Int J Pediatr 6(6):7803–7814
Veracx A, Raoult D (2012) Biology and genetics of human head and body lice. Trends Parasitol 28:563–571
Verma P, Namdeo C (2015) Treatment of pediculosis capitis. Indian J Dermatol 60:238–247
Watcharawit R, Soonwera M (2013) Pediculicidal effect of herbal shampoo against Pediculus humanus capitis in vitro. Trop Biomed 30(2):315–324
Zahirnia AH, Taherkhani H, Bathaii SJ (2001) Comparative study on the effectiveness of three different shampoos in treatment of head lice (Pediculus capitis) in primary school-children in Hamadan province. J Mazandaran Uni Med Sci 15:16–24 [Abstract in English]
Zhu F, Lavine L, O’Neal S, Lavine M, Foss C, Walsh D (2016) Insecticide resistance and management strategies in urban ecosystems. Insects 7(1):2–26
Acknowledgments
This study is subject of M.Sc thesis of Mrs. Atefe Ebrahimi Fahdani. The authors’ deep gratitude goes to the health staffs of Ahvaz Jundishapur University of Medical Sciences for their collaboration.
Funding
Special thanks to Research Health Vice-Chancellery of Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran, for the financial support of this work (Project Number: U-94166).
Author information
Authors and Affiliations
Contributions
Hamid Kassiri provided the research idea, searched for previous relevant articles, prepared the paper, and edited the paper and references. Atefe Ebrahimi did field operations. Bahman Cheraghian analyzed the information obtained.
Corresponding author
Ethics declarations
The study was approved by the Committee of Ethics in Research, Ahvaz Jundishapur University of Medical Sciences and registered as R.AJUMS.REC.1394.558.
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kassiri, H., Fahdani, A.E. & Cheraghian, B. Comparative efficacy of permethrin 1%, lindane 1%, and dimeticone 4% for the treatment of head louse infestation in Iran. Environ Sci Pollut Res 28, 3506–3514 (2021). https://doi.org/10.1007/s11356-020-10686-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-020-10686-3