Abstract
Approximately 15–20% of patients with Kawasaki disease (KD) are not responsive to high-dose intravenous gammaglobulin (IVIG). We have previously reported a predictive method for identifying IVIG-non-responsive patients (high-risk KD patients). We determined the safety and effectiveness of pulse methylprednisolone with high-dose IVIG (mPSL+IVIG) as a primary treatment for high-risk KD patients. Sixty-two high-risk KD patients were treated with pulse methylprednisolone 30 mg/kg over 2 h, followed by IVIG 2 g/kg over 24 h (mPSL+IVIG group) and were compared with a historical control group of 32 high-risk patients treated with IVIG 2 g/kg alone at the participating hospitals before this study was opened (IVIG group). High-risk patients were identified with at least two of three predictors (C-reactive protein ≥7 mg/dL, total bilirubin ≥0.9 mg/dL or aspartate aminotransferase ≥200 IU/L). Sixty-six percent (95% confidence interval [CI] 54–78%) of patients had a prompt defervescence in the mPSL+IVIG group compared with 44% (95% CI 26–62%) for the IVIG group (p = 0.048). Coronary artery lesions were observed in 24.2% (95% CI 13.2–35.2%) and 46.9% (95% CI 28.6–65.2%) of patients in the mPSL+IVIG and IVIG groups, respectively (p = 0.025). This is the first report showing that mPSL+IVIG is effective and safe as a primary treatment for high-risk KD patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Kawasaki disease (KD) is a systemic inflammatory disease characterised by fever and systemic vasculitis [8]. The most severe problem with this disease is vasculitis and subsequent remodelling of the major arteries, including coronary arteries. Although abnormalities of coronary arteries have been highlighted, these are only representative and silent injuries occur in many systemic arteries. Such injuries may lead to serious problems in former patients during middle age. Indeed, some reports suggested that children with KD were at high risk for coronary artery disease, even in patients without development of coronary artery abnormalities [1, 3, 8]. Therefore, the aim of KD treatment is the prompt termination of systemic inflammation as early as possible and inhibition of the development of systemic vasculitis.
Current standard primary therapy for KD is a large dose of intravenous gammaglobulin (IVIG) 2 g/kg [5, 8] with aspirin 30–50 mg/kg/day, which can reduce the prevalence of coronary artery lesions to approximately 5% [8]. However, approximately 15–20% of patients with KD have been reported as IVIG-non-responsive [4, 8, 11], even though standard high-dose IVIG therapy was appropriately initiated. In these patients, coronary artery lesions frequently developed, despite the use of additional treatments, including further IVIG and steroids [4, 10], indicating that current alternative treatments are ineffective after the failure of the initial IVIG treatment. In other words, an earlier and more effective primary therapy is required for non-responsive patients.
Hence, we proposed the prediction of IVIG-non-responsive patients before starting an initial treatment [10]. Patients with at least two of three predictors (C-reactive protein [CRP] ≥7 mg/dL, total bilirubin ≥0.9 mg/dL or aspartate aminotransferase [AST] ≥200 IU/L) are predicted to be non-responsive to initial IVIG treatment (sensitivity=77%, specificity=86%, and positive and negative predictive values of 59% and 94%, respectively) [10]. We defined these patients as having high-risk KD. According to these criteria, approximately 20% of KD patients are predicted to be resistant to IVIG. We examined the effectiveness and safety of pulse methylprednisolone combined with IVIG as a primary treatment in patients with high-risk KD in a prospective, multicentre study and the results were compared with a historical control group.
Patients and methods
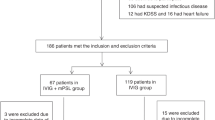
Between April 2002 and March 2005, 62 patients with newly diagnosed high-risk KD (17% of all KD patients) were enrolled in this study. Patients aged ≥3 months with fever of ≤5 days duration at the time of diagnosis were eligible. Exclusion criteria included a previous diagnosis of KD or the presence of a dilated coronary artery (≥3SD internal diameter). The Institutional Review Board of each participating hospital approved this study, and informed consent was obtained from the guardians of all patients.
The historical control group included 32 patients who were treated with IVIG 2 g/kg alone at the participating hospitals before this study was opened. They were diagnosed as high-risk KD in the same way, and the eligibility criteria were identical.
Patients received pulse methylprednisolone 30 mg/kg over 2 h followed by the administration of IVIG (2 g/kg over 24 h). We used heparin (10 U/kg/h, continuous infusion) concomitantly from 2 h before the start of methylprednisolone for 48 h. Aspirin (30 mg/kg/day, three times daily) was given from the end of heparin administration, and it was reduced to 10 mg/kg/day after defervescence. We considered the treatment to be effective when a patient had defervescence within 24 h after the completion of IVIG administration. Rebound was defined as a transient fever after the defervescence.
Laboratory tests were performed at least once weekly until the CRP became normal. The cardiovascular sequellae were evaluated by serial cardiac ultrasound studies. Two-dimensional echocardiographic measurements of coronary artery dimensions, the left main, proximal right and proximal left anterior descending coronary arteries (LMCA, RCA and LAD, respectively), were obtained at least three times during the early phase: before the treatment, immediately after the treatment and a short time later. The diameter of the coronary artery was expressed as a z-score and the value of the standard deviation from a standardised coronary artery dimension was calculated from the body surface area [10]. Dilation of the coronary artery was defined as a z-score ≥3.0 and coronary aneurysm as a z-score ≥5.0.
Statistical analysis for differences in the mean values was performed with Student’s t-test. Gender, effectiveness and the incidence of coronary artery lesions were compared by means of χ2 analysis.
The authors had full access to the data and take responsibility for its integrity. All authors have read and agreed to the manuscript as written.
Results
Patient characteristics
The patient cohort included 35 boys and 27 girls with a median age of 2.8 years (range 0.3–7.0). The mean coronary artery z-score was 1.18 (range −1.08 to 2.87) at diagnosis. The difference was not significant between patients in the study group (mPSL+IVIG group) and historical control group (IVIG group) (Table 1).
Effectiveness of pulse methylprednisolone with high-dose IVIG
The treatment was effective in 66% (95% confidence interval [CI] 54–78%) of patients in the mPSL+IVIG group compared with 44% (95% CI 26–62%) of those in the IVIG group (Table 2). The combination of pulse methylprednisolone and IVIG was significantly more effective (p = 0.048).
Table 3 shows the distribution of the maximum z-score for each patient. Coronary artery lesions (z-score ≥3.0) were observed in 24.2% (95% CI 13.2–35.2%) of patients in the mPSL+IVIG group, compared with 46.9% (95% CI 28.6–65.2%) of those in the IVIG group (p = 0.025). Moreover, the incidence of coronary artery aneurysm (z-score ≥5.0) was significantly lower in the mPSL+IVIG group (p = 0.002). The mean maximum z-score was also significantly decreased in the mPSL+IVIG group compared with the IVIG group (2.28 vs. 4.31, p = 0.008).
The AST and total bilirubin levels were normalised promptly after the treatment. However, some patients developed transient AST elevation, which seemed to be adverse events. The CRP levels were normalised within two weeks in almost all patients, though one month was required for the normalisation of CRP levels in three refractory or rebound patients.
Rebound or refractory patients after pulse methylprednisolone with high-dose IVIG
Seven patients were refractory and 14 patients had rebound after mPSL+IVIG treatment. Nine of them had coronary artery lesions (Table 4). The incidence of coronary artery lesions was significantly higher in rebound or refractory patients than in responsive patients (p = 0.049). Although 19 of 21 rebound or refractory patients received additional treatments, including corticosteroids and/or IVIG, coronary artery lesions developed in six patients and these treatments seemed to be insufficient (Fig. 1). Two patients without further treatments also developed coronary artery lesions.
Adverse events
Nine patients developed hypothermia (<36.0°C), nine transaminase elevation, four bradycardia (<60/min) and one hypertension. These adverse events were transient and disappeared in a few days. There were no serious adverse events.
Discussion
The addition of pulse methylprednisolone to standard high-dose IVIG treatment was safe and proved to be significantly more effective in decreasing the frequency and severity of coronary artery lesions in high-risk KD patients compared with a historical group of similar patients treated with high-dose IVIG alone. Thus, this study showed, for the first time, that the early termination of systemic inflammation as soon as possible is key in preventing the progression of vasculitis.
In recent years, corticosteroid treatments have been reviewed in various reports describing the treatment of IVIG-resistant patients [2, 12]. Furthermore, two prospective studies suggested that corticosteroids were safe and effective as the initial treatment for the early termination of inflammation [7, 9]. However, both studies failed to show the substantial difference in the most important issue of coronary artery abnormalities. The present study is the first report demonstrating the usefulness of corticosteroids for preventing the development of coronary artery injury with respect to both frequency and severity. A randomised trial conducted by Newburger et al. [9] examined an identical regimen to ours in KD patients. However, no significant differences between treatment groups were noted in the coronary artery dimensions. We speculate that their result differs from ours because the frequency of coronary artery abnormalities in the unselected KD patients that they targeted was low. In contrast, the subjects of our study were limited to high-risk patients who frequently show the development of coronary artery lesions.
Although this combination treatment accomplished successful results, it failed in 34% of high-risk patients. Half of these cases had coronary artery lesions, despite the use of some additional therapies, including IVIG and/or corticosteroids. These results suggest that a more potent anti-inflammatory treatment, for example, two courses of pulse methylprednisolone therapy with high-dose IVIG, may be required.
Our study indicates that pulse methylprednisolone therapy is a safe and powerful initial treatment for KD. The power of the prediction of non-responsiveness to initial therapy with IVIG alone is limited, and the late sequellae of systemic vasculitis are unknown in KD patients, even in patients without acute coronary artery injury. Moreover, a recent study reported that a combination of prednisolone and IVIG in primary therapy for all KD patients improved coronary artery outcome [6]. Hence, it seems appropriate that methylprednisolone pulse therapy combined with high-dose IVIG is applied to all KD patients without coronary artery dilations at diagnosis.
Abbreviations
- IVIG:
-
Intravenous gammaglobulin
- KD:
-
Kawasaki disease
- mPSL:
-
Methylprednisolone
References
Cheung YF, Yung TC, Tam SC, Ho MH, Chau AK (2004) Novel and traditional cardiovascular risk factors in children after Kawasaki disease: implications for premature atherosclerosis. J Am Coll Cardiol 43:120–124
Dale RC, Saleem MA, Daw S, Dillon MJ (2000) Treatment of severe complicated Kawasaki disease with oral prednisolone and aspirin. J Pediatr 137:723–726
Dhillon R, Clarkson P, Donald AE, Powe AJ, Nash M, Novelli V, Dillon MJ, Deanfield JE (1996) Endothelial dysfunction late after Kawasaki disease. Circulation 94:2103–2106
Durongpisitkul K, Soongswang J, Laohaprasitiporn D, Nana A, Prachuabmoh C, Kangkagate C (2003) Immunoglobulin failure and retreatment in Kawasaki disease. Pediatr Cardiol 24:145–148
Furusho K, Kamiya T, Nakano H, Kiyosawa N, Shinomiya K, Hayashidera T, Tamura T, Hirose O, Manabe Y, Yokoyama T, Kawarano M, Baba K, Mori C (1984) High-dose intravenous gammaglobulin for Kawasaki disease. Lancet 2:1055–1058
Inoue Y, Okada Y, Shinohara M, Kobayashi T, Kobayashi T, Tomomasa T, Takeuchi K, Morikawa A (2006) A multicenter prospective randomized trial of corticosteroids in primary therapy for Kawasaki disease: clinical course and coronary artery outcome. J Pediatr 149:336–341
Jibiki T, Terai M, Kurosaki T, Nakajima H, Suzuki K, Inomata H, Terashima I, Honda T, Yasukawa K, Hamada H, Kohno Y (2004) Efficacy of intravenous immune globulin therapy combined with dexamethasone for the initial treatment of acute Kawasaki disease. Eur J Pediatr 163:229–233
Newburger JW, Takahashi M, Gerber MA, Gewitz MH, Tani LY, Burns JC, Shulman ST, Bolger AF, Ferrieri P, Baltimore RS, Wilson WR, Baddour LM, Levison ME, Pallasch TJ, Falace DA, Taubert KA; Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease; Council on Cardiovascular Disease in the Young; American Heart Association (2004) Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Pediatrics 114:1708–1733
Newburger JW, Sleeper LA, McCrindle BW, Minich LL, Gersony W, Vetter VL, Atz AM, Li JS, Takahashi M, Baker AL, Colan SD, Mitchell PD, Klein GL, Sundel RP; Pediatric Heart Network Investigators (2007) Randomized trial of pulsed corticosteroid therapy for primary treatment of Kawasaki disease. N Engl J Med 15:663–675
Sano T, Kurotobi S, Matsuzaki K, Yamamoto T, Maki I, Miki K, Kogaki S, Hara J (2007) Prediction of non-responsiveness to standard high-dose gamma-globulin therapy in patients with acute Kawasaki disease before starting initial treatment. Eur J Pediatr 166:131–137
Wallace CA, French JW, Kahn SJ, Sherry DD (2000) Initial intravenous gammaglobulin treatment failure in Kawasaki disease. Pediatrics 105:E78
Wright DA, Newburger JW, Baker A, Sundel RP (1996) Treatment of immune globulin-resistant Kawasaki disease with pulsed doses of corticosteroids. J Pediatr 128:146–149
Acknowledgements
We thank Shigetoyo Kogaki, Reiko Yabuta, Nobuhiro Kawakami, Masaru Iwaki and Kazuki Tanaka for the acquisition of the clinical data, and Tokuko Okuda for assistance.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Okada, K., Hara, J., Maki, I. et al. Pulse methylprednisolone with gammaglobulin as an initial treatment for acute Kawasaki disease. Eur J Pediatr 168, 181–185 (2009). https://doi.org/10.1007/s00431-008-0727-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-008-0727-9