Abstract
Human polyomavirus BK virus (BKV) is a double-stranded DNA virus that infects approximately 90 % of the general population as a subclinical or mild infection. In immunosuppressed patients, such as HIV cases, BKV may be reactivated resulting hemorrhagic cystitis and tubulointerstitial nephritis. However, there are limited studies on prevalence and molecular epidemiology of BKV in Iran. We therefore aimed to evaluate the prevalence and subtypes of BKV in Iranian HIV patients. A total of 99 patients with HIV infection were enrolled in the study. Presence of BKV DNA in plasma was evaluated by nested PCR. PCR products were sequenced directly, and phylogenetic analysis was performed. BKV DNA was detected in 8.08 % of HIV patients. BKV viremia presented in 4 out of 25 patients (16 %) not receiving antiretroviral therapy in comparison with 4 out 74 of HAART-treated patients (5.4 %) (P = 0.023). In patients with CD4 counts ≥200 cells/mm3, viremia was found more commonly (7/80 = 8.8 %) than in those with lower counts (1/19 = 5.2 %) (not significant). All sequenced BKV isolates belonged to subtype Ib-2. Our findings indicated that the prevalence of BKV viremia is relatively prevalent in patients with HIV infection and significantly higher in naïve than HAART-treated cases. Therefore, HAART can eliminate BKV infection from plasma and reduce viremia although the actual implication of BKV viremia in HIV patients is not clear.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Human polyomavirus BK virus (BKV) is widespread throughout the world [1, 2], and epidemiological studies have revealed that up to 90 % of adult individuals have antibodies against BKV [3]. The primary infection with BKV occurs in early childhood as an asymptomatic or mild respiratory infection. After this, self-limited infection, BKV, remains latent within the urogenital system but also in the brain and in B lymphocytes [4]. In immunocompromised patients, BKV is linked with hemorrhagic cystitis in bone marrow transplant recipients [5], polyomavirus-associated nephropathy and ureteric stenosis in kidney transplant recipients [6, 7]. Besides, BKV DNA has been found in brain tissue or cerebrospinal fluid (CSF) of both immunocompromised and immunocompetent patients with neurological symptoms [8, 9]. Moreover, there is some evidence supporting the association of BK genome with prostate cancer [10].
In HIV patients, the prolonged immunosuppression leads to the high rate of virus reactivation although active disease due to BKV is rare in HIV patients [11]. However, virus could be found in urine and blood of individuals with HIV and nephropathy and hemorrhagic cystitis associated with BKV have been shown in AIDS patients [12–14]. Atypical presentations of BKV also explained in HIV cases such as meningoencephalitis, pneumonitis and retinitis [15]. The limited studies which investigated the presence of BKV in HIV patients reported high prevalence of BKV in the urine (20–50 %) which related to the lower CD4 counts [12, 13, 16]. Seroepidemiologic studies have revealed high rate of BKV antibodies in HIV-positive patients [16, 17]; nevertheless, prevalence of BK viremia and the actual implications of this infection in HIV patient have not yet been established. Of note, with the introduction of highly active antiretroviral treatment (HAART) and development of new potent agents and their impact on restoring immune response, changing in epidemiology and presentation of BKV in HIV patients is expected.
Four distinct subtypes of BKV have been determined based on serological and molecular methods. Subtype I is considered to be the most common subtype throughout the world, subtype IV is common in Asia and part of Europe, while subtypes II and III have been detected rarely in the world [18].
Few studies carried out on BKV prevalence in dialysis patients and kidney transplant recipients in Iran [19, 20]. However, there are insufficient data on the prevalence and molecular epidemiology of BKV viremia in HIV patients, and also the role of antiretroviral treatment in this setting has not been well clarified. We therefore aimed to evaluate the prevalence and molecular characterizations of BKV in Iranian patients infected with HIV and explore the role of antiretroviral therapy in this setting.
Methods
Study population
In this cross-sectional study, 99 patients with HIV infection without any neurological or renal problems admitted to the Iranian Research Center for HIV/AIDS in Tehran, Iran, from January to April, 2014, were consecutively enrolled. This project was approved by Pasteur Institute of Iran ethical committee, and informed consent was obtained from subjects prior to their enrollment.
CD4 count was determined by flowcytometry and defined as cells/mm3.
DNA extraction and polymerase chain reactions
Viral DNA was extracted from 200 μl of plasma using RTP DNA/RNA Virus Mini Kit (Invitek, Berlin, Germany) following the manufacturer’s instructions.
DNA quality was evaluated by PCR using primers PCO3 (5′-ACACAACTGTGTTCACTAGC-3′) and PCO4 (5′-CAACTTCATCCACGTTCACC-3′) which amplify a 110-bp product from the human β-globin gene. PCR was carried out with a 25 μl amplicon mixture containing 1 μl extracted DNA, 50 mM KCl, 15 mM Tris–HCl (pH 8.0), 0.2 mM dNTP, 1.5 mM MgCl2, 10 pmol each of primers and 1.5 U Taq polymerase (YTA PCR Master Mix, Iran). β-Globin positive samples were subjected to nested PCR.
Nested PCR was performed to amplify a DNA fragment within the VP1 coding region. The first round of PCR was carried out using primer pair (BK-ext1; 5′-AAGATGGCCCCAACCAAA-3′ and BK-ext2; 5′-GCATTTCCAAGGGGTCTTC-3′) which described previously by Boukoum et al. [21] which amplify a 490-bp fragment correspond to nucleotides 1561–2051 on the VP1 gene sequence of the BKV. The first round of PCR was performed with 5 μl of DNA extract in a 20 μl of PCR mixture containing 50 mM KCl, 15 mM Tris–HCl (pH 8.0), 0.2 mM dNTP, 1.5 mM MgCl2, 10 pmol each of primers and 1.5 U Taq polymerase (YTA PCR Master Mix, Iran). Amplification profile was as follows: dsDNA was initially denatured for 3 min at 95 °C, followed by 40 cycles of 95 °C for 30 s (s), 55 °C for 30 s and 72 °C for 30 s and the final extension step at 72 °C for 3 min. Each batch included negative control (distilled water) and positive sample from previous study on dialysis patients as positive control.
Second round of PCR was performed using primers (327-1; 5′-CAAGTGCCAAAACTACTAAT-3′ and 327-2; 5′-TGCATGAAGGTTAAGCATGC-3′) that correspond to nucleotides at positions 1630–1956 on the VP1 gene sequence of the BKV. The second reaction utilized the same mixture (above), but with 327-1 and 327-2 primers and 5 μl of first-round PCR product. All cycling steps are similar to first run except final extension step which was done at 72 °C for 5 min. The expected size of the second PCR product was 335 bp.
The PCR products were electrophoresed on a 1.5 % agarose gel with the 100-bp DNA ladder (Sinaclon, Iran) and stained with ethidium bromide and visualized by ultraviolet transillumination.
DNA sequencing, genotyping and phylogenetic analysis
Nested PCR products were purified using QIAquick PCR purification kit (Qiagen, Hilden, Germany) and then sequenced directly for both directions at Pishgam Biotech Company, Tehran, Iran.
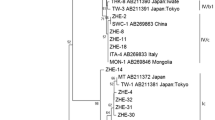
Phylogenetic analysis was based on BKV VP1 sequences of the patients described in this study, and reference sequences of various BKV subtypes downloaded from GenBank database. Simian agent 12 was used as outgroup. Nucleotide sequences were aligned using CLUSTAL W program in CLC Main Workbench 6.5 software (CLC Bio, Qiagen). Genetic distance was calculated using the Kimura two-parameter matrix. Subsequently, phylogenetic tree was constructed by the neighbor-joining (NJ) method and tested with the bootstrap resamplings (1000 replicates) using MEGA program, version 4.
The BK sequences obtained in this study were deposited in GenBank under accession numbers KP857588–KP857592.
Statistical analysis
Statistical analyses were conducted using SPSS statistics software (version 16, Chicago, IL, USA). The Chi-square test or Fisher’s exact test was used to compare variables. Data are presented as mean ± SD or, when indicated, as an absolute number and percentage. P values <0.05 were considered statistically significant.
Results
A total of 99 HIV-infected patients with mean age of 37.9 ± 10 years were enrolled in the study. Of patients, 71.7 % were male and 28.3 % were female. The mean CD4 count was 410.3 ± 211.4 cells/mm3. More than half of the patient (50.5 %) presented CD4 counts 200–499 cells/mm3, 30.3 % with CD4 counts ≥500 and 19.2 % had CD4 counts less than 200 cells/mm3. The possible routes of HIV transmission were intravenous drug use (54.6 %), heterosexual contact (34.3 %), infected blood and blood products transfusion (2 %), vertical transmission (2 %), homosexual (1 %), and in 6.1 %, the route of HIV acquisition was not identified. Of patients, 74.7 % were under HAART treatment as lamivudine (74.7 %), efavirenz (60.6 %), zidovudine (51.5 %), tenofovir (21.2 %), and the rest with lopinavir and nevirapin in different combinations.
Overall BKV DNA was detected in 8.08 % (8 of 99) of HIV patients. There was no significant difference with respect to BKV viremia and age, sex, possible route of HIV transmission, CD4 count and specific antiretroviral treatment in our study cohort. Characteristics of HIV-infected patients with BKV viremia are described in Table 1. In patients with CD4 counts ≥200 cells/mm3, viremia was found more commonly (7/80 = 8.8 %) than in those with lower counts (1/19 = 5.2 %) (not significant). In comparison with HAART-treated and not-treated patients, BKV viremia presented in 4 out of 25 naïve patients (16 %) comparing to 4 out 74 of patients receiving antiretroviral therapy (5.4 %) (P = 0.023).
Five out of eight samples were subjected to direct sequencing, and phylogenetic analysis demonstrated that all sequenced BKV isolates belonged to subtype Ib-2 (Fig. 1).
Discussion
This survey investigated the prevalence and molecular characterization of BKV in patients with HIV in Tehran, Iran. BKV DNA was detected in 8.08 % of HIV patients. We reported relatively high prevalence of BKV viremia in comparison with previous studies and also showed that viremia is significantly higher in naïve than HAART-treated cases. Moreover, we revealed that BKV Ib-2 is the only detectable genotype in our study cohort.
Seroepidemiological investigations demonstrated high prevalence of BKV antibodies in HIV-infected patients [16, 17]. BKV also has been revealed to have the capability of causing encephalitis and hemorrhagic cystitis in AIDS patients [22, 23]. However, few studies carried out on prevalence of BKV viremia in HIV patients, and the role of antiretroviral treatment in this setting has not been well clarified. Sundsfjord et al. [16] reported BKV viremia in 4.76 % of peripheral blood mononuclear cells (PBMC) of HIV-infected patients. While, in a study by Ledesma et al. [24] which was conducted on HIV-positive cases, BKV DNA was detected only in one plasma sample (1.3 %). This positive sample attributed to a patient who was under HAART treatment with a normal CD4 count. In the other study on HIV patients, BKV and JCV were detected in 8.1 and 31.6 % of urine samples, respectively, while DNA detection in PBMC samples increased to 22.8 % for JCV and 51.1 % for BKV. Besides, it was shown that DNA positivity was related to lower CD4 count [25]. In the present study, we detected BKV viremia in 8.08 % of HIV patients without any association with the degree of immunodeficiency as measured by CD4 count. This finding is in consistent with those of Sundsfjord et al. [16] who showed no correlation between BKV DNA and CD4 count, but in contrast to Degener et al. [25] and Knowles et al. [13] results that showed high viruria in lower CD4 counts. However, most of these studies carried out before the availability of HAART and could not provide accurate perspective of present BKV situation.
With the introduction of HAART and its impact on restoring immune response, course of several infections in HIV patients was changed. For instance, studies before development of HAART mostly demonstrated that BKV viruria found commonly in HIV patients with profound immunosuppression [16, 26], but study after introducing HAART mainly focused on the role of antiretroviral treatment on prevalence of BKV viruria. Ledesma et al. [24] suggested that BK viruria was more common in treated patients with CD4 > 500 cell/mm3 and also patients receiving abacavir or efavirenz more commonly show BKV viruria than patients not treated with these drugs. But only one patient showed BKV viremia in this survey. In our cohort of study, viremia was found more frequently than Ledesma et al. [24] survey which is the only investigation on HIV-treated cases. Moreover, in comparison between treated and not-treated HIV participants, BKV viremia was detected significantly in our naïve patients, although we could not find any relation to specific antiretroviral regimen. Therefore, we assume that immunity due to HAART may eliminate BKV in plasma and decrease viremia as shown in our treated group and Ledesma et al. study but not able to total clearing of virus in urine as mentioned in previous investigation by Ledesma [24]. However, in the present study, we focused on the role of treatment on BKV viremia, and as a limitation of our investigation, we did not check BKV viruria. Of note, the design of study did not include control group, although our findings could reflect a relatively high circulation of this virus in the general population which could be reactivated in the presence of immunosuppression.
BKV isolates were classified into four major subtypes based on serological and molecular methods, and the distribution pattern of BKV subtypes was defined in several investigations [13, 27]. Subtype I is being considered the predominant subtype worldwide, subtype IV is common in Asia and part of Europe, and subtypes II and III are rarely detected throughout the world [28, 29]. Subtype I sequences are further divided into four subgroups: Ia, Ib-1, Ib-2 and Ic, with a distinct geographical distribution [18]. Subgroup Ib-2 is most prevalent in Europe and West Asia, Ib-1 in Southeast Asia, Ia in Africa and Ic in Northeast Asia [29].
This is the first study in Iran which assigns the subtype of BKV in HIV patients. BKV Ib-2 is the only detectable genotype in our study cohort from Iran. The predominant BKV subtype Ib-2 in this study is in accordance with previous surveys from Iranian, European and American populations [18, 19].
In conclusion, this study evaluated the prevalence and molecular characterization of BKV in HIV patients in HAART era. Our findings indicated that BKV viremia is relatively prevalent in patients with HIV infection and significantly higher in naïve than HAART-treated cases. Therefore, we suggested that HAART can eliminate BKV infection from plasma and decrease viremia, although further follow-up studies are required to clarify the clinical implication of BKV viremia in HIV patients.
References
Berger JR, Major EO (1999) Progressive multifocal leukoencephalopathy. Semin Neurol 19:193–200
Knowles WA, Pipkin P, Andrews N, Vyse A, Minor P, Brown DW, Miller E (2003) Population-based study of antibody to the human polyomaviruses BKV and JCV and the simian polyomavirus SV40. J Med Virol 71:115–123
Krumbholz A, Zell R, Egerer R, Sauerbrei A, Helming A, Gruhn B, Wutzler P (2006) Prevalence of BK virus subtype I in Germany. J Med Virol 78(12):1588–1598
Elsner C, Dorries K (1992) Evidence of human polyomavirus BK and JC infection in normal brain tissue. Virology 191:72–80
Rice SJ, Bishop JA, Apperley J, Gardner SD (1985) BK virus as cause of haemorrhagic cystitis after bone marrow transplantation. Lancet 2:844–845
Hirsch HH, Knowles W, Dickenmann M, Passweg J, Klimkait T, Mihatsch MJ, Steiger J (2002) Prospective study of polyomavirus type BK replication and nephropathy in renal-transplant recipients. New Engl J Med 347:488–496
Teutsch K, Schweitzer F, Knops E, Kaiser R, Pfister H, Verheyen J, Göbel H, Cingöz T, Di Cristanziano V (2015) Early identification of renal transplant recipients with high risk of polyomavirus-associated nephropathy. Med Microbiol Immunol. doi:10.1007/s00430-015-0398-x
Volz R, Jager G, Seelo K, Fuhey L, Hohifeld R (1996) BK virus encephalitis in an immunocompetent patient. Arch Neurol 53:101–103
Vago L, Cinque P, Sala E, Nebuloni M, Caidarelli R, Racca S, Ferrante P, Trabottoni G, Costanzi G (1996) JCV-DNA and BKV-DNA in the CNS tissue and CSF of AIDS patients and normal subjects. Study of 41 cases and review of the literature. J Acquir Immune Defic Syndr Hum Retrovirol 12:139–146
Delbue S, Matei DV, Carloni C, Pecchenini V, Carluccio S, Villani S, Tringali V, Brescia A, Ferrante P (2013) Evidence supporting the association of polyomavirus BK genome with prostate cancer. Med Microbiol Immunol 202(6):425–430
Nali LH, Centrone Cde C, Urbano PR, Penalva-de-Oliveira AC, Vidal JE, Miranda EP, Pannuti CS, Fink MC (2012) High prevalence of the simultaneous excretion of polyomaviruses JC and BK in the urine of HIV-infected patients without neurological symptoms in São Paulo, Brazil. Rev Inst Med Trop Sao Paulo 54(4):201–205
Behzad-Behbahani A, Klapper PE, Vallely PJ, Cleator GM, Khoo SH (2004) Detection of BK virus and JC virus DNA in urine samples from immunocompromised (HIV-infected) and immunocompetent (HIV-non-infected) patients using polymerase chain reaction and microplate hybridisation. J Clin Virol 29:224–229
Knowles WA, Pillay D, Johnson MA, Hand JF, Brown DW (1999) Prevalence of long-term BK and JC excretion in HIV infected adults and lack of correlation with serological markers. J Med Virol 59:474–479
Crum-Cianflone N, Quigley M, Utz G, Hale B (2007) BK virus-associated renal failure among HIV patients. AIDS 21:1501–1502
Vallbracht A, Löhler J, Gossmann J, Glück T, Petersen D, Gerth HJ, Gencic M, Dörries K (1993) Disseminated BK type polyomavirus infection in an AIDS patient associated with central nervous system disease. Am J Pathol 143:29–39
Sundsfjord A, Flaegstad T, Flø R, Spein AR, Pedersen M, Permin H, Julsrud J, Traavik T (1994) BK and JC viruses in human immunodeficiency virus type 1-infected persons: prevalence, excretion, viremia, and viral regulatory regions. J Infect Dis 169(3):485–490
Flaegstad T, Permin H, Husebekk A, Husby G, Traavik T (1988) BK virus infection in patients with AIDS. Scand J Infect Dis 20:145–150
Zhong S, Randhawa PS, Ikegaya H, Chen Q, Zheng HY, Suzuki M, Takeuchi T, Shibuya A, Kitamura T, Yogo Y (2009) Distribution patterns of BK polyomavirus (BKV) subtypes and subgroups in American, European and Asian populations suggest co-migration of BKV and the human race. J Gen Virol 90(Pt 1):144–152
Kaydani GA, Makvandi M, Samarbafzadeh A, Shahbazian H, Hamidi Fard M (2015) Prevalence and distribution of BK virus subtypes in renal transplant recipients referred to Golestan Hospital in Ahvaz, Iran. Jundishapur J Microbiol 8(3):e16738
Sharif A, Sharif MR, Aghakhani A, Banifazl M, Hamkar R, Ghavami N, Eslamifar A, Ramezani A (2015) Prevalence of BK viremia in Iranian hemodialysis and peritoneal dialysis patients. Infect Dis 47(5):345–348
Boukoum H, Nahdi I, Foulongne V, Zallema D, Aloui S, Achour A, Segondy M, Aouni M (2011) Distribution of BK polyomavirus genotypes in Tunisian renal transplant recipients. J Med Virol 83(4):725–730
Barouch DH, Faquin WC, Chen Y, Koralnik IJ, Robbins GK, Davis BT (2002) BK virus-associated hemorrhagic cystitis in a human immunodeficiency virus-infected patient. Clin Infect Dis 35:326–329
Kinnaird AN, Anstead GM (2010) Hemorrhagic cystitis and possible neurologic disease from BK virus infection in a patient with AIDS. Infection 38:124–127
Ledesma J, Muñoz P, Garcia de Viedma D, Cabrero I, Loeches B, Montilla P, Gijon P, Rodriguez-Sanchez B, Bouza E; BKV Study Group (2012) BK virus infection in human immunodeficiency virus-infected patients. Eur J Clin Microbiol Infect Dis 31(7):1531–1535
Degener AM, Pietropaolo V, Di Taranto C, Rizzuti V, Ameglio F, Cordiali Fei P, Caprilli F, Capitanio B, Sinibaldi L, Orsi N (1997) Detection of JC and BK viral genome in specimens of HIV-1 infected subjects. New Microbiol 20(2):115–122
Jin L, Gibson PE, Booth JC, Clewley JP (1993) Genomic typing of BK virus in clinical specimens by direct sequencing of polymerase chain reaction products. J Med Virol 41:11–17
Baksh FK, Finkelstein SD, Swalsky PA, Stoner GL, Ryschkewitsch CF, Randhawa P (2001) Molecular genotyping of BK and JC viruses in human polyomavirus-associated interstitial nephritis after renal transplantation. Am J Kidney Dis 38:354–365
Zheng HY, Nishimoto Y, Chen Q, Hasegawa M, Zhong S, Ikegaya H, Ohno N, Sugimoto C, Takasaka T, Kitamura T, Yogo Y (2007) Relationships between BK virus lineages and human populations. Microbes Infect 9:204–213
Chehadeh W, Nampoory MR (2013) Genotypic diversity of polyomaviruses circulating among kidney transplant recipients in Kuwait. J Med Virol 85(9):1624–1631
Acknowledgments
The authors are grateful to Pasteur Institute of Iran for financial support of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Akhgari, S., Mohraz, M., Azadmanesh, K. et al. Frequency and subtype of BK virus infection in Iranian patients infected with HIV. Med Microbiol Immunol 205, 57–62 (2016). https://doi.org/10.1007/s00430-015-0426-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00430-015-0426-x