Abstract
Regarding the 13 known mammalian aquaporins (AQPs), their functions in their expressing tissues, effects of their mutation/polymorphisms in humans, and effects of knockout of their genes are summarized in this review article. The roles of AQP5, an exocrine gland-type water channel, in the salivary gland under normal and pathophysiological conditions are reviewed in detail. First, the involvement of AQP5 in water secretion from acinar cells was demonstrated by measuring volume changes of acini/acinar cells, as well as activation energy (E a) in transepithelial water movement by NMR spectrometry, and a functional linkage between AQP5 and TRPV4 was suggested. Next, involvement of the parasympathetic nervous system on the AQP5 levels in the acinar cells of the submandibular and that of a β-adrenergic agonist on those in the parotid gland are described. That is, chorda tympani denervation induces autophagy of the submandibular gland, causing AQP5 degradation/metabolism, whereas isoproterenol, a β-adrenergic agonist, causes first an increase then decrease in AQP5 levels in the parotid gland, which action is coupled with the secretory-restoration cycle of amylase-containing secretory granules. The PG also responded to endotoxin, a lipopolysaccharide that activates NF-κB and MAPK pathways. Elevated NF-κB and AP-1 (c-Fos/c-Jun) form a complex that can bind to the NF-κB-responsive element on the AQP5 promoter and thus potentially downregulate AQP5 transcription. Salivary gland pathologies and conditions involving AQP5 and possible treatments are described as well.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One of the characteristics of cell membranes is their semipermeability. Because of this feature, water can move in and out of the cells. However, in epithelial cells of such tissues as the mammalian kidney collecting tubules, amphibian skin, and bladder, the water permeability is much higher compared with that of other tissues. Therefore, the existence of some other mechanism(s) had long been anticipated that could allow such high permeability.
In 1992, P. Agre at The Johns Hopkins University discovered the first water channel, aquaporin 1 (AQP1), which had been given the initial name of “channel-forming integral membrane protein of 28 kDa (CHIP 28)” [128]. AQP1 was shown to participate strongly in water movement across the cell membrane. In the following year (1993), AQP2, a second AQP, was cloned from kidney tissue by Sasaki’s group [26]. Thereafter, research in this field developed rapidly, and in 2000, Fujishoshi’s group succeeded in X-ray crystallographic analysis of the AQP1 molecule, revealing its whole structure [109]. It is now well known that AQPs exist in many living organisms from animals and plants to microorganisms [174] and that one to several molecular species of AQPs are expressed in individual tissues.
This review will first briefly overview mammalian AQPs and then focus on salivary gland AQP5 in particular relation to its physiological regulation and the water transport mechanism.
Aquaporins
AQPs are water channels constructed by serpentine-type membrane proteins. The water movement across biological membranes via AQPs is considered to be facilitated simply dependent on the osmotic gradient.
These water channels have the following characteristics [49, 55, 61]: (1) The channel protein is a six-transmembrane protein having a tandem-repeat structure. (2) It has two Asp-Pro-Ala sequences (NPA motif) in the molecule that form hemi-channel structures. These two hemi-channel structures face each other from inside and outside of the plasma membrane forming a pore through which water can pass. (3) Within the molecule, there are phosphorylation target motifs besides glycosylation target ones, which motifs participate in the regulation of the water-channel function.
After the discovery of the first AQP, a number was given to each AQP following the order of discovery, and presently 13 AQPs, AQP0–12, are known to exist in mammals.Footnote 1 These AQPs have been divided into four major subfamilies, according to the following characteristics: facilitation of permeation of glycerol besides water, altered sequence of conservative NPA box, and molecular phylogeny. The first subfamily is the water-selective AQP one, which includes AQP0, 1, 2, 4, 5, and 6. These AQPs facilitate the movement of water mainly. The second subfamily is the aquaglyceroporin one, to which AQP3 [50, 88], AQP7 [71], AQP9 [46, 157], and AQP10 [48] have been assigned. The third subfamily, named superaquaporin [51], includes AQP11 and AQP12, which are unorthodox AQPs because each has a unique NPA box with a signature cysteine residue and low homology with AQPs in the two previously mentioned groups (see the section Super aquaporins (unorthodox aquaporins) and [44, 51]). The remaining AQP, AQP8, is a water-selective AQP but has an unusual structure with a long N-terminus, short C-terminus, and high homology with γ-TIP, a plant water channel [47, 68, 94]. The phylogenic study clearly separate AQP8 from the group of water-selective AQPs in animals. Regarding mammalian AQPs, major expressing tissues, functions, physiological roles, and effects of mutation/polymorphism in human ones are summarized in Table 1.
Water-selective aquaporins
The membrane protein AQP1 was initially found in the erythrocyte, a highly water-permeable cell [128], and AQP2 [26], 3 [50], and 6 [175] were consecutively cloned from the kidney. AQP4 was cloned from the lung and brain [37, 55], whereas AQP5, from salivary gland [132]. All of them except AQP3 belong to water-selective subfamily of AQPs (Table 1). AQP4 was found to play important functions in the nervous system, whereas AQP5 functions in fluid secretion/movement in many tissues including exocrine glands and lungs. AQP6, on the other hand, localizes in vesicles inside of kidney cells and has been suggested to play a role in anion-channel function.
Aquaglyceroporins
The glycerol permeability of AQP3 was recognized when this water channel was first cloned and characterized [50]. It has an important role in the skin. A second aquaglyceroporin, AQP7, was cloned from the rat testis [45] and was shown to be permeable to glycerol, water, and urea. On the other hand, an aquaporin with high homology to rat AQP7 was cloned from human adipose tissues [71]. Based on similar tissue distribution, primary sequence, and function, Ishibashi et al. suggested that human aquaglyceroporin cloned from adipocytes is most likely the human ortholog of rat AQP7 [52]. AQP7 (designated as AQPap by Kishida) was shown to be downregulated by insulin and elevated by fasting [64, 65]. AQP9, a human water channel capable of permeation of water and urea, was first detected in leukocytes [46]. The homolog of AQP9 was cloned from rat liver, and when expressed in Xenopus oocytes, it was shown to allow passage of a wide variety of noncharged solutes including glycerol [157]. In addition, the liver AQP9 level was shown to be regulated negatively by binding with insulin at the insulin responsive element in the promoter of AQP9 [72]. The coordinated regulation of AQP9 and AQP7 by insulin and/or fasting condition suggested the pathophysiological importance of these two aquaglyceroporins in glycerol transport between the fat tissue and liver [72, 76]. As to AQP10, it was cloned from a human jejunum cDNA library [39]. AQP10 is strongly expressed in the duodenum and jejunum and supposedly functions mainly as a water transporter, although its structural homology implies that AQP10 belongs to the aquaglyceroporin subfamily [39]. Recently, AQP10 was reported to be expressed in the stratum corneum and adipocytes, in which this water channel supposedly facilitates the transport of glycerol [56, 73]. Aquaglyceroporins are important for not only the transport of glycerol between the fat tissue and liver, as mentioned above, but also for providing moisture to the skin [35, 95, 158]. Further investigation focused on AQP10 is necessary to better understand its function.
Super aquaporins (unorthodox aquaporins)
Recently, AQP11 and AQP12 were cloned and shown to be less homologous to the already known AQPs [44]. Although some water permeability of AQP11 was demonstrated in liposomes and cultured cells [51], its permeability to glycerol is unknown. AQP11-null mice develop polycystic kidneys following the formation of large intracellular vacuoles in the proximal tubule, but the function of AQP12 still remains to be clarified [51].
Aquaporin 8
As described earlier, AQP8 is structurally unusual compared to other members in the AQP family, being rather close to the plant water channel. Thus, this water channel has been separated from other classified AQPs in this review. With respect to its function, AQP8 is close to water-selective AQPs as it is permeable to water and does not permeate glycerol. Interestingly, it has the unique property of permeating H2O2 [8].
Functions other than as a water channel
In recent years, it was reported that some molecules in the AQP family function other than as water channels. For instance, AQP0 functions as an osmometer and thereby enables normal microcirculation within the lens tissue, preventing swelling of the lens fiber [16]. Simultaneously, AQP0 is involved in helping each fiber to adhere to its neighbor, resulting in narrowing of the interfibrous spaces, a feature important for maintaining lens transparency [16]. Among mammalian aquaglyceroporins (AQP3, 7, 9, and 10), at least AQP7 and AQP9 transport trivalent arsenic ions [85], and AQP3, AQP7, and AQP9 transport urea [83]. These aquaglyceroporins (AQP3, 7, 9, and 10) as well as AQP8 transport ammonia as well. It is known also that AQP6 [114, 173], AQP1 [40], and AQP8 [9] transport ions, CO2/NO, and H2O2, respectively. Furthermore, some AQPs are reportedly involved in cell adhesion, cell movement, and cell division [163]. The major characteristics of mammalian AQPs are summarized in Table 1.
Mutations and polymorphisms of human aquaporin genes
A number of mutations and polymorphism/SNP of genes in the AQP family members were reported to occur in humans. Some of them cause diseases and pathologic conditions, whereas others apparently do not have any effect, or if so, only a minor one. For example, individuals with a mutation in AQP0 [27, 30] and AQP2 [159] develop cataract and nephrogenic diabetes insipidus, respectively; a mutation in AQP1 apparently has no phenotypic effect, although affected patients have an impaired ability to concentrate urine [62, 129]. These cases along with others are summarized in Table 1.
Aquaporin gene knockout used to reveal new aquaporin functions
Phenotype analysis of gene-knockout (KO) mice can generally predict the pathophysiological roles of the gene product of interest in various tissues. Especially important cases would be those that show unexpected roles of the protein product. Today, all knockout mice for each AQP gene, except AQP6 and AQP10, has been established (AQP10 in mice has been shown to be a pseudo-gene [43, 103]). The phenotypes observed for each type of AQP-KO mouse are summarized in the literature [162] and in Table 2.
Aquaporin 5 in individual tissue
Tissues expressing aquaporin 5
Water secretion from exocrine glands, such as salivary, lachrymal, and sweat glands, and water movement in the lung alveoli are two of the most important physiological functions of these structures. The possible involvement of water-channel proteins has therefore been implied. Raina et al. cloned AQP5 mRNA for the first time from the submandibular gland (SMG), one of the major salivary glands [132]. They showed that this AQP is expressed in such exocrine glands as the parotid (PG), sublingual, and lachrymal glands, as well as in the trachea, eyes, and lungs. Later, it was demonstrated that AQP5 is also expressed in the stomach [126], Brunner’s glands in the duodenum [125, 126], pancreas [11], skin, and sweat glands [116]. Besides AQP5, several other AQPs are expressed in these tissues simultaneously, and it is recognized in general that one tissue expresses several members of the AQP family. On the other hand, most tissues having an exocrine function express AQP5. Therefore, a pivotal role is suggested for AQP5 in exocrine function.
Effects of mutation and polymorphism of aquaporin 5
Recently, missense mutations in the AQP5 gene were identified in patients suffering from autosomal-dominant diffuse nonepidermolytic palmoplantar keratoderma (referred to as palmoplantar keratoderma Bothnia type), which was mapped in Swedish and UK families to chromosomal region 12q11–12q13 [1, 10]. A variant of AQP5 (c.529A>T; p.Ile177Phe) was localized in the plasma membrane in the stratum granulosum in affected palmar epidermis, similarly as in normal subjects, thus indicating that this mutant AQP5 traffics normally [10]. A year later, another missense mutation of AQP5 (c.367A>T, p.Asn123Tyr) was identified in a large three-generation family of Chinese Han ethnicity with palmoplantar keratoderma of the Bothnia type, and study of this mutant showed that the mutant channel is leaky and more sensitive to hypotonic solution than is the wild-type one [13]. Such properties of this mutant AQP5 may account for the intensive cellular swelling resulting in the phenotype of diffuse nonepidermolytic palmoplantar keratoderma.
Single-nucleotide polymorphism (SNP) has been detected in humans. An SNP is found in the 3′ UTR region of the AQP5 gene in a certain percentage of asthma patients, resulting in reduced production of the AQP5 protein [70]. These individuals are hypersensitive toward choline-provoked bronchoconstriction [69]. Five SNPs in AQP5 were genotyped in European Americans with chronic obstructive pulmonary disease (n = 429), and three of them showed significant association with the rate of decline in lung function [33]. Also, a positive association between SNPs in AQP5 promoter and progesterone receptor was reported [59]. Recently, high expression of AQP5 and polymorphism in the AQP5 promoter were suggested to be associated with peritumoral brain edema in meningioma patients [74].
Aquaporin 5 in the salivary glands
Expression of aquaporin 5 and other aquaporins in the salivary glands
In the rat SMG, AQP5 is expressed in the apical/lateral and basal membranes of the acinar cells [4, 112], whereas AQP1 is detected in the cell membranes of the capillaries within salivary gland tissue [2, 4, 79]. The mRNAs for AQP3 and AQP4 are expressed in the fetal, but not in the adult SMG, whereas AQP2 mRNA cannot be detected in either fetal or adult SMG [2]. The expression of AQP6 and AQP7 in the human salivary gland was examined, but the results were obscure, and such expression was not confirmed [20]. On the other hand, positive AQP8 labeling was observed in the myoepithelial cells in the salivary gland (SMG, PG, and sublingual gland), with no labeling of acinar or ductal epithelial cells [22, 166], whereas AQP11 transcripts were present in the developing and mature duct structure of the SMG, and its expression was reduced in the adults, implying some roles for AQP11 during gland development [75].
Effects of aquaporin 5 mutation on the salivary function
Inbred rats having a point mutation at nucleotide 308 (G308A) in their AQP5 gene and producing a mutant AQP5 protein were established [111, 112], and this mutant molecule has an aspartic acid at position 103 in place of glycine (AQP5-G103D) in the third transmembrane domain of AQP5. This mutation was initially found as an SNP among SD rats in the breeder’s colony. The AQP5 protein level in the SMG and other tissues is strongly reduced in these mutant rats, though the glandular mRNA level is unchanged compared with that in wild-type rats, and the Kozack sequence (GGCACCaugA), which affects the translational efficiency, was not altered in the mutant mRNA [112]. These data support the hypothesis that the reduced AQP5 protein production in the mutant rats is caused by accelerated degradation of the mutant molecule via the protein quality control system. Actually, structures positive for AQP5 are taken up by lysosomes more in the mutant SMG than in the wild-type one [58]. The water permeability of the mutant AQP5 as tested by the Xenopus oocyte expression system is normal [58]. However, water secretion from the salivary gland in vivo and in situ is significantly affected [110, 112]. Namely, the initial water secretion from the mutant SMG upon cholinergic stimulation is reduced compared with that from the wild-type gland due to its extremely low expression at the acinar cell membrane. Studies using AQP5-mutant rats can provide useful information about the effects of genetic variation of the AQP5 gene in humans. Also, AQP5-KO mice and AQP5-mutant rats are useful models for studying the physiological roles of AQP5 in the water secretion from the exocrine glands.
Effects of aquaporin 5 knockout on salivary gland function
Mice genetically altered by knocking out the AQP5 gene have been prepared and analyzed [91]. Though the appearance of the KO mice is normal, both their birth rate and growth rate are reduced. As compared with that of their wild-type counterpart, the salivary secretion and levels of some tight junction proteins in the acini are decreased in these AQP5-KO mice [60, 91], suggesting that AQP5 KO affects salivary flow via the paracellular route as well (see the section Roles of aquaporin 5 in water secretion).
Roles of aquaporin 5 in water secretion
Water is secreted from the terminal portion of exocrine glands via paracellular and transcellular routes. This secretion takes place as a result of coupling to ion transport via the ion channel. In the salivary gland, the first trigger of this process is the release of Cl− followed by Na+ movement [24, 86, 175]. The Cl− ions required for this process are co-transported into the acinar cells along with the Na+ and K+ ions via NKCC1, an Na+/K+/2Cl− co-transporter, present in the basal membrane. Evans et al. showed that saliva secretion is reduced by 60 % in NKCC1 KO mice [23]. Their study directly demonstrated that Cl− ions are accumulated in the cells by the action of NKCC1 and serve as a driving force for saliva secretion. As for the other two cations accumulated by NKCC1, Na+ is transported to the outside of the cells via Na+, K+-ATPase and K+, via K+ channels. Two K+ channels, IK1/SK4 and maxiK/Slo, have been identified, and KO of either of them does not affect saliva secretion, whereas double KO of these two K+ channels significantly reduces it [5, 136], suggesting that the accumulated K+ ions are transported to the outside of cells via both channels. These facts also support the idea that the Cl− efflux from the cells is indispensable for water secretion.
Ma et al. showed that saliva secretion after the initial 5 min and 5–10 min after pilocarpine stimulation is reduced by more than 60 % in AQP5-KO mice [91]. The extent of the effects on saliva secretion is similar between AQP5 KO and NKCC1 KO animals. In AQP5-G103D mutant rats, only a trace amount of the mutant molecule is expressed in the SMG acinar cells [112], and 15 % of that of the wild type in the PG acinar cells [139]. In these rats, a similar reduction in saliva secretion is observed during the initial 12–17 min after pilocarpine stimulation in vivo [112]. These data imply consistently that AQP5 play important roles at least at the initial phase of saliva secretion. On the other hand, Menon’s group determined water transport via the paracellular route by performing an experiment to measure the movement of FITC-dextran [60]. They demonstrated that water transport via this route is decreased in AQP5-KO mice also, although the transcellular one is much more affected by AQP5 KO. Another observation by these authors is that the levels of claudin-7, claudin-3, and occludin in the parotid gland are decreased in AQP5-KO mice. Decreased expression of these tight junction proteins is thought to be correlated with decreased paracellular permeability because such a phenomenon is actually observed in Madin-Darby canine kidney (MDCK) type II cells expressing a low level of claudin-2 in vitro [82].
Since acinar cells have the cholinergic receptor, it is most possible that cholinergic agonists, via stimulation of acinar cells, trigger transcellular water transport, leading to the rapid increase in water permeability. However, extracellular tracer studies suggest that only a small fraction of water is transported through the transcellular pathway and that the majority of water moves through the paracellular pathway [107, 108]. Thus, it is important to study the initial mechanism governing the opening/closing of the paracellular pathway in the acinus of salivary glands to elucidate the entire water secretion by the exocrine glands.
Activation energy for water transport
In order to assess the involvement of AQP5 in the abovementioned water transport by the salivary gland acinar cells, a research group examined changes in the cell volume and activation energy (E a) of diffusive water permeability (P d) in isolated parotid acinar cells obtained from AQP5-G103D mutant rats and their wild-type counterparts (Table 3; Ref. [139]). In the unstimulated wild-type acinar cells, E a determined by NMR spectrometry was shown to be 3.4 ± 0.6 kcal mol−1, and no detectable change was noted after stimulation with carbachol (CCh), a cholinergic agonist. In the unstimulated mutant acinar cells, a high E a value (5.9 ± 0.1 kcal mol−1) was detected, and it showed a minimal decrease after CCh stimulation (5.0 ± 0.3 kcal mol−1). As mentioned earlier (see the section Effects of aquaporin 5 mutation on the salivary function), since the AQP5-G103D (mutant AQP5) expressed in Xenopus oocytes has a water permeability almost the same as that of the normal AQP5 [58], this high E a value for the mutant acinar cells may not be due to the functional disorder of the mutant AQP5 but rather to the fact that a small number of AQP5 molecules are expressed in the acinar cell membrane, and therefore, the observed E a value was affected by the high E a for the water transport via the lipid bilayer (E a = 12–14 kcal mol−1) [130, 133].
Reliability of the E a value for mutant acini was verified by calculating its E a assuming that the E a for the lipid membrane per se is 12.75 kcal mol−1 [130, 133] and that the AQP5 fraction relative to the wild-type one is 15 % (based on Western blot analysis). The apparent E a value expected from the simulation curve is E a = 6 kcal mol−1, which value well agrees with the measured one.
The increase in E a for water transport would result in a decrease in osmotic water permeability (P f) of mutant acinar cells to 1/3 to 1/4 of that of wild-type rats, although the apparent P d between the two groups of rats is the same (see Table 3). These results suggest that AQP5 is essential for reducing the activation energy for water transport in the acinar cells and therefore affects their water permeability.
These data consistently support the fact that reduced saliva secretion in AQP5 KO mice, providing there is full deletion of AQP5 [60, 91], is at least in part due to the decrease in water transport across the plasma membrane between the two water transport routes, transcellular and paracellular pathways.
Hypothetical mechanism of water secretion
In vitro shrinkage of exocrine acinar cells upon cholinergic stimulation has generally been recognized [113, 115, 153] with exception of SMG C10 cells in culture, which show transient blebbing of cell membranes instead of cell shrinkage upon stimulation [3]. The lack of cell shrinkage in the latter study cannot be explained at present [3]. In the isolated acinus of the PG from wild-type rats, CCh (1 μM) stimulation induces transient swelling of the acinus, followed by rapid shrinkage of the acinar cells shortly thereafter. The transient swelling of acini and rapid shrinkage of acinar cells can explain the water shift through the transcellular and paracellular pathways, respectively [113]. The transient swelling of the acinus is accompanied by an enlargement of the luminal canal [113]. In the initial stage of water secretion, Cl− efflux into the lumen takes place first. A small amount of water is then shifted into the lumen via AQP5 present in the apical membrane. It is believed that the same amount of water then enters the cells through the basolateral membrane via AQP5. Therefore, the acinar cell volume is unchanged, and the luminal volume is increased. In the next step, rapid acinar cell shrinkage takes place at 8 s after CCh stimulation [139]. The volume of the acinar cells is decreased rapidly by 20 % by the CCh stimulation, and the decreased volume size stays at this low level as long as the agonist is present [139]. The agonist-induced shrinkage is explained by the isotonic release of KCl from the acinar cells [153], and both K+ and Cl− channels are supposed to be activated by an increase in intracellular Ca2+ [115]. As a result of rapid shrinkage of the acinar cells, the paracellular space between acinar cells increases. It is likely therefore that the permeability of the intercellular junctions between acinar cells would be increased. Indeed, 10 kDa dextran can pass through the paracellular tight junction in the acinus following CCh stimulation [141]. This increase in permeability allows a continuous secretion of saliva via the paracellular pathway.
Functional linkage between aquaporin 5 and cation channels
Transient receptor potential cation channel, subfamily V, member 4 (TRPV4) is an ion channel protein that belongs to a member of the vanilloid subfamily in the transient receptor potential (TRP) superfamily of ion channels [81, 151]. It functions to regulate the systemic osmotic pressure in various tissues such as the kidney, liver, heart neurosensory cells, and the central nervous system [151]. The cDNA encoding vanilloid receptor-related osmotically activated channels has been cloned from rat, mouse, human, and chicken [81].
Liu et al. [84] studied a possible linkage between AQP5 and TRPV4 in the salivary gland and found that hypotonic solution elicits an increase in cell volume and Ca2+ entry, followed by activation of a regulatory volume decrease (RVD). Ca2+ entry is associated with ruthenium red-sensitive nonselective cation current, suggesting the involvement of TRPV4. Acinar cells from TRPV4-KO or AQP5-KO mice do not activate the RVD upon their exposure to hypotonic solution, confirming the requirement of both channel proteins for RVD activation as well as their functional linkage. Hypotonicity increases the association and surface expression of TRPV4 and AQP5 in the salivary gland cells [84], while it reduces AQP5 abundance in the presence of TRPV4 in mouse lung epithelial cells [143].
On the other hand, caveolin-1, the main component of the caveolae plasma membranes, is suggested to be a critical component for salivary gland function [123]. The functional linkage of AQP5 with cation channels suggested above is supported by the fact that loss of caveolin-1 impairs agonist-stimulated salivary fluid secretion, transient receptor potential canonical 1-stroma interaction molecule 1 (TRPC1-STIM1) channel assembly, and altered apical targeting of AQP5. Further study should disclose the mechanism of regulation of AQP5 function and involvement of cation channels and/or other components.
Verification of proposed mechanism of water secretion by use of acini expressing aquaporin 5-G103D
In mutant acini, when 1 μM CCh is applied, the acinus does not swell at all, and the agonist-induced shrinkage of acinar cells is delayed by 8 s [139]. If we suppose that the fluid might shift via the paracellular pathway, it would be expected that the acinus should swell transiently even in the mutant rats. However, no acinar swelling can be detected at all in the mutant rat. Therefore, under normal conditions, a transcellular water shift is thought to take place during this time period (after CCh), and AQP5 should be involved in such transient swelling of the acini. Since the amount of AQP5 expressed is small in mutants, even if Cl− is effluxed into the lumen, water would not be able to move quickly from the acinar cell. As a result, no transient swelling would be observed in the acinus of the mutant rat [139].
The delay in CCh-induced shrinkage of the acinar cells is also explained by the low expression of the AQP5 in the acinar cells. As discussed above, due to the higher E a value (5.9 kcal mol−1), the P f value of the mutant rats is decreased to 1/3–1/4 of that of the wild-type rats. This low water permeability may cause a delay in the water efflux from the acinar cells and may prevent the initial rapid shrinkage of the acinar cells. In the mutant rat, not only is the CCh-induced shrinkage of the acinar cells delayed by 8 s but also the decreased cell volume recovers spontaneously [139]. It is speculated that a decreased transcellular water shift prevents the Na+ and Cl− osmosis, resulting in accumulation of Na+ ions in the acinar cells, and this may cause the spontaneous recovery of acinar cell size [139].
On the other hand, as described above, the expression levels of claudin-3 and 7 (in females) or claudin-7 (in males) in AQP5-KO mice were found to be reduced to 50 % of the level in wild-type mice (see the section Effects of aquaporin 5 knockout on salivary gland function); and such a reduction has been described to be closely correlated with a reduction in paracellular water secretion [60]. Also in the PG of AQP5-G103D mutant rats, claudin-7 and ZO-1 levels tend to be lower (72 ± 6 % (P = 0.07) and 75 ± 6 % (P = 0.16) of wild-type PG, respectively) than those in wild-type rats. This reduction in expression of tight junction proteins may be the direct cause of the reduced salivary secretion via the paracellular route in the AQP5-G103D mutant rats.
Autonomic regulation of salivary gland aquaporin 5
The salivary gland is double-innervated by sympathetic and parasympathetic nerves. Generally, the sympathetic nerve provokes the release of a small amount of viscous and protein-rich saliva, whereas parasympathetic nerve action triggers that of a massive amount of dilute saliva. The sympathetic nerve originates from the thoracic vertebrae and innervates the three major salivary glands via the superior cervical ganglion. The nuclei of parasympathetic nerves, the centers of salivation, are localized in the superior and inferior salivatory nuclei in the medulla oblongata. The efferent nerve from the superior salivatory nucleus is a facial nerve that reaches the SMG and sublingual gland via the submandibular ganglion. On the other hand, the efferent nerve from the inferior salivatory nucleus is a glossopharyngeal nerve, which, via the otic ganglion, innervates the parotid gland. Both efferent nerves are thought to regulate the salivary gland through muscarinic acetyl choline receptors. In addition, the chorda timpani parasympathetic nerve and isoproterenol injection are reported to regulate AQP5 in the SMG and PG, respectively [2, 15, 79].
Regulation of SMG aquaporin 5 by chorda timpani nerve
Though secretion of saliva from the three major salivary glands greatly differs according to species and to basal and stimulated state of the gland [19], among them, the SMG generally participates to the greatest extent in salivary secretion.
The possible involvement of the autonomic nervous system in the regulation of AQP5 was first studied by measuring the level of this water channel in the SMG membrane fraction after denervation of the chorda timpani nerve [79]. Chorda timpani denervation (CTD) causes a continuous reduction in the AQP5 level in the membrane fraction, reaching 50–60 % of the control by 4 weeks. The gland weight is decreased, reaching a minimum (75–80 % of the control) by as early as 1 week after denervation [4, 79].
By immunohistochemistry, the decrease in AQP5 level elicited by CTD and its recovery by injection of cevimeline, an M3 muscarinic agonist, was confirmed [4]. AQP5, concomitantly with other membrane proteins such as dipeptidyl peptidase IV (DPPVI) and Na+, K+-ATPase α-subunit are localized in the SMG. Whereas Na+, K+-ATPase is localized in the duct cells, DPPVI as well as AQP5 has been shown to be localized in the cell membrane of the acinar cells, implying that the DPPVI protein would be an appropriate control when changes in the AQP5 level are determined. A reduction in the AQP5 level in the acinar membrane by CTD was confirmed, with no detectable change in the DPPVI level [4]. Pretreatment with cevimeline prevented the decrease in the level of AQP5 [4]. These immunohistochemical data are supported by the results of a Western blotting experiment; i.e., CTD reduced the AQP5 level in the membrane fraction, and cevimeline injection prevented this reduction. No change in the AQP5 level was observed when pilocarpine, another muscarinic agonist, was used.
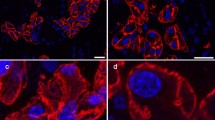
The reduction in the SMG AQP5 level caused by CTD is not due to a reduction in its mRNA level. Such a reduction appears to be due to activation of AQP5 metabolism/degradation because the AQP5 protein level in MLE-12 cells, a cultured lung cell line, is reportedly decreased by cAMP and recovered by chloroquine, a denaturant of lysosomes [144]. These data suggest that SMG AQP5 is metabolized by the lysosomal system upon CTD. Li et al. showed this to be the case, i.e., injection with chloroquine prevented the reduction in SMG AQP5 level caused by CTD [79]. Protein degradation by the lysosomal system is known as autophagy [100]. This process is involved in balancing protein synthesis, degradation, and regeneration to control the proliferation of normal cells, development, and homeostasis. Thus, it is probable that AQP5 metabolism/degradation by CTD is brought about by lysosomes via autophagy in the SMG. Actually, in the SMG, microtubule-associated protein 1 light chain 3 isoform B-II (LC3B-II), a marker protein for autophagosomes, is elevated immediately and transiently after CTD, peaking at 1 day [4]. Consecutively, lysosome-associated membrane protein 2 (Lamp 2), a lysosomal marker, is elevated and remains at a high level at 7–10 days after CTD [4]. It has also been confirmed by immunohistochemistry that AQP5 is present in these structures [4]. Thus, it is probable that active autophagosomes are increased in number first, followed by elevation of the number of lysosomes upon CTD and that AQP5 is taken up by these structures (see Fig. 1). These results well agree with the continuous decrease in the AQP5 level over a 4-week period. Also, the transient increase in the LC3B-II level, i.e., indicating the onset of autophagy, for a short period well accords with the fact that the gland weight decreases by 20–25 % upon CTD [4, 79]. No apoptosis has been detected by use of the TUNEL assay or by measuring the ratio of the levels of anti-apoptosis and pro-apoptosis proteins (bcl-2/Bax) [4]. The just-cited study showed also that the soluble fraction of SMG containing the lysosomal enzymes metabolizes/degrades AQP5 in vitro and that such an activity is elevated by CTD. All these facts and other reports [57, 78] imply that this degradation system plays important roles in regulation and/or control of AQP function.
Pathway for AQP5 metabolism/degradation in the acinar cells of the SMG in normal (untreated) rats and CTD rats (hypothesis). In acinar cells of the normal rat SMG, endocytotic vesicles incorporated inside the cell from AQP5-bearing apical membrane by endocytosis move toward lysosomes via early endosomes. In CTD rats, in addition to these pathways, phagospheres take in early endosomes to form autophagosomes, which will then fuse with lysosomes to become autolysosomes. AQP5 is incorporated into these structures and metabolized
In conclusion, SMG AQP5 is dependent on chorda timpani parasympathetic innervation, and denervation of this autonomic nerve results in stimulation of autophagy and activation of the lysosomal system, by which AQP5 is supposedly metabolized (Fig. 1). Further study is needed to disclose the details of this mechanism.
Function of PKA-target motifs in the aquaporin 5 molecule
Since AQP5 has cAMP-dependent protein kinase target motifs at the fourth loop and C-terminal tail (Ser156 and Thr259, respectively), AQP5 function may be controlled by secretagogues [36, 132]. Woo et al. reported that cAMP-dependent phosphorylation of AQP5 at its Ser156 may not be involved in the AQP5 membrane expression and trafficking in human bronchial epithelial cells [167]. Instead, they described the possibility that AQP5 phosphorylation at this site may affect cell proliferation through the Ras signaling pathway [168]. In polarized MDCK cells, AQP5 is localized at the apical membrane [164, 165]. Constructs for chimeric proteins, AQP-GFP and GFP-AQP5, having normal Thr259 or the T259A mutation, were used to transfect MDCK cells to study the function of Thr259 in AQP5 trafficking [67]. The results showed that regardless of whether or not there was a mutation at position 259, AQP-GFP is constitutively expressed at the cell membrane. By contrast, GFP-AQP5 molecules introduced into MDCK cells remain in the cytoplasm and traffic to the plasma membrane upon dbcAMP stimulation, regardless of the presence or absence of the mutation, and such movement is H-89 sensitive. These data are very similar to those seen for AQP2 [31] and suggest that phosphorylation at Thr259 is not necessary for AQP5 trafficking. In human salivary gland (HSG) cells transfected with AQP5 or an AQP5-T259A mutant construct, these molecules are constitutively localized at the plasma membrane under both resting and forskolin-stimulated conditions [36]. In the SMG and PG, Thr259, a novel phosphorylation site of AQP5, is potentially phosphorylated through cAMP signaling, but not through Ca2+ signaling, in vivo [36]. These data again suggest that phosphorylation of Thr259 of AQP5 is not important for AQP5 trafficking in salivary gland cells in vitro. The precise physiological role of Thr259-phosphorylated AQP5 is still unknown at present.
IPR-induced dynamic changes in PG aquaporin 5
AQP2, a major water channel in the renal collecting duct, is known to be regulated by the vasopressin/cAMP signaling pathway [38]. On the other hand, 8-(4-chlorophenylthio)-cAMP or the β-adrenergic receptor agonist isoproterenol (IPR) increases AQP5 mRNA and protein levels in MLE-12 cells, a cultured lung cell line, and induces the translocation of AQP5 (trafficking) [171]. Also, in the PG, one of the major salivary glands, amylase, an important mammalian digestive enzyme, is secreted by the β-agonist, in which secretion process in the cAMP signaling is functioning.
These reports imply that the cAMP signaling pathway is involved in the regulation of AQP5 in the salivary gland and that β-agonists would possibly be involved in AQP5 regulation in the PG. Chen et al. [15] studied the effects of IPR on the level of AQP5 in the PG and analyzed its relation to the secretion-reaccumulation cycle of amylase by IPR as well as to the dynamic change in secretory granules. The PG secretory granules containing a large amount of amylase protein secrete their constituents by exocytosis. During this process, the secretory granules first dock to the plasma membrane and then fuse to it. It was found that IPR first upregulates the expression of AQP5 protein in the PG membrane fraction, which expression is followed by decomposition of this water channel protein via the calpain pathway [15]. Namely, the IPR treatment has three obvious effects on AQP5 expression in the PG membrane fraction. Firstly, the AQP5 protein level rapidly rises at 1 h after IPR treatment. Secondly, the level then decreases at 6 h after IPR treatment, reaching its minimum at 12 h. Thirdly, the protein level of AQP5 begins to increase again at 12 to 24 h after the treatment. The AQP5 mRNA level, having gradually risen from 1 h after IPR treatment, reaches its peak in accordance with the pattern of increase in its protein level.
The elevation of the AQP5 protein level after the IPR injection takes place with the same timing (at 1 h) as the exocytotic amylase secretion and continues till 6 h after the injection. This elevation is thought to be the result of exocytotic transfer of AQP5 from the granule membrane to the plasma membrane. Actually, the membrane of secretory granules containing amylase is reported to express the AQP5 protein [98]. Thus, it was assumed that the amount of AQP5 in the plasma membrane is first increased by the IPR injection and then decreased by activation of the protease system (see the section IPR-induced downregulation of PG aquaporin 5).
The level of AQP5 protein in the PG membrane fraction is reduced by 85 % of the peak level (which is 200 % of the control level taken as 100 %) at 12 h after IPR treatment (to 30 % of the control level). This result is in good accord with the report that proteolytic decomposition of AQP2 protein is induced by dihydrotachysterol in the rat renal inner medullary collecting duct, although its mRNA level is unaltered [131, 138]. It is possible that IPR reduces the AQP5 protein level by affecting the posttranslational process, but not the transcriptional one.
On the other hand, the reduction in the AQP5 protein level after IPR treatment is suppressed by calpain inhibitors, but not by proteasome inhibitors nor by a lysosomal denaturant, suggesting that AQP5 is a substrate for calpain and that this water channel protein is metabolized by calpain proteolysis (see the section IPR-induced downregulation of PG aquaporin 5).
In summary, Chen et al. proposed the following mechanism (ref. [15] and Fig. 2): in accordance with the amylase secretion 1–3 h after IPR treatment, the granule membrane of secretory granules (containing amylase) becomes a part of plasma membrane by docking, resulting in elevation of AQP5 in the plasma membrane. Thereafter, from around 6 h after the IPR injection, the AQP5 protein becomes decomposed or metabolized. This reduction is due to proteolytic degradation by μ-calpain. Lastly, from around 12–24 h after IPR treatment, new AQP5 biosynthesis becomes obvious, and then the AQP5 level gradually increases toward its original one.
Hypothetical model of AQP5 dynamics coupled to the secretory-restoration cycle of amylase in acinar cells of the parotid gland. In accordance with amylase secretion, the number of AQP5 molecules in the plasma membrane is increased at 1–3 h after IPR as the granule membrane has become a part of the plasma membrane. AQP5 in the membrane is then degraded/metabolized from around 6 h after IPR, when the amylase level in the gland has been recovering. This reduction in AQP5 is due to proteolysis by μ-calpain. New AQP5 biosynthesis gradually increases at 12–48 h after IPR to return its level to the original state. AM, apical membrane; LM, lateral membrane; BM, basal membrane (from Chen et al. [15])
Downregulation of aquaporin 5 in the salivary glands
LPS-induced downregulation of PG aquaporin 5
Endotoxin or lipopolysaccharide (LPS) is a major component of the cell wall of Gram-negative bacteria, and it activates many types of cells in patients suffering from septic shock. LPS induces inflammatory proteins such as cytokines and defensins through TLR4, an important molecule in the innate immune system. The LPS/TLR4 signal transduction system has been well described [154]. Briefly, binding of ligands to the extracellular domains of TLR4 drives complex signaling systems and eventually activates NF-κB, through which numbers of inflammation-inducing proteins are elicited. In addition to the NF-κB pathway, the MAPK pathway is also activated during LPS signaling and is considered to be involved in the induction of proliferation, apoptosis, cytokine biosynthesis, and cytoskeletal reorganization. In the downstream of MAKK, there are the growth factor/chemical inducer-activated ERK1/2 pathway and the cytokine-inducible JNK and p38 pathways.
The transcription of salivary gland AQP5 and AQP1 genes is inhibited by LPS, and the mechanism underlying this inhibition was studied by using an in vitro organ culture system and inhibitors of signaling pathways [172]. Inhibitors of NF-κB and MAPK pathways did not suppress transcriptional inhibition of AQP1 by LPS. One of the reasons for this result would be that there is no NF-κB-responsive element in the AQP1 promoter. However, the transcriptional inhibition of AQP5 by LPS is completely suppressed by PDTC or MG132, an I-κB kinase inhibitor or proteasome inhibitor, respectively. In the presence of either of these inhibitors, it is conceivable that I-κB would accumulate and that the formation of free NF-κB would be suppressed. Furthermore, MAPK inhibitors, AG126 and SP600125 (inhibitors of ERK1/2 and JNK, respectively), also suppress the transcriptional inhibition of AQP5 by LPS. Namely, it has become clear that both NF-κB and MAPK pathways are involved in the suppression of transcriptional inhibition of AQP5 by LPS.
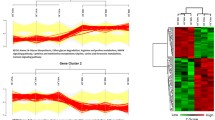
Another fact revealed from this experiment is that when the formation of any one of the three molecules p-c-Jun, p-c-Fos, (phosphorylated c-Jun and phosphorylated c-Fos formed by JNK and ERK1/2, respectively) or NF-κB is inhibited, then transcriptional inhibition of AQP5 by LPS is completely suppressed, meaning that transcriptional inhibition of AQP5 requires all three of these molecules. For confirmation of this interpretation, immunoprecipitation experiments using antibodies against the above transcription factors were performed, assuming that p-c-Jun, p-c-Fos, and NF-κB become associated to make a complex that suppresses the transcription of the AQP5 gene. PG extracts prepared 3 h after the LPS injection were reacted with Sepharose gels bearing antibodies specific for NF-κB (p65), p-c-Jun, or p-c-Fos (Fig. 3). Proteins absorbed to the gels were eluted and subjected to Western blotting and probed with anti p-c-Jun antibody. p-c-Jun was detected in the eluates from all three gels. In eluates from the anti-p-c-Jun and anti-p-c-Fos gels reacted with extracts of the PG from animals before LPS stimulation, only a small amount of p-c-Jun was detected. However, p-c-Jun was not detected at all in the eluate from the anti-NF-κB (p65) gel reacted with extracts of the PG from animals not stimulated with LPS. These results suggest that very little or no NF-κB (p65) was present in the unstimulated PG but that certain levels of p-c-Jun and p-c-Fos were present and that a complex of the three transcription factors had been formed by LPS stimulation.
Association of p-c-Jun with NF-κB subunit p65 and p-c-Fos in consequence of the LPS signaling (hypothesis). LPS injection has been shown to elevate the levels of transcription factors NF-κB, p-c-Jun, and p-c-Fos in the mouse PG in vivo [172]. The results of immunoprecipitation experiments using Sepharose gel bearing immobilized anti-NF-κB antibody, anti-p-c-Jun antibody, and anti-p-c-Fos antibody, and probed with anti-p-c-Jun, have shown that elevated p-c-Jun can bind anti-NF-κB antibody gel and anti-p-c-Fos antibody gel, suggesting that all three transcription factors form a complex. The complex of p-c-Jun, NF-κB, and p-c-Fos supposedly binds to the NF-κB-responsive element present in the promoter of AQP5. Though CREB is also elevated by LPS, its function in the transcriptional regulation of the AQP5 gene is not yet clear
Two NF-κB-responsive elements and two AP-1 binding sequences are found in the promoter of the AQP5 gene. The results of an electrophoretic mobility shift assay (EMSA) performed with 2 NF-κB probes confirmed that the binding activity toward sequences for these 2 NF-κB-responsive elements is elevated in the extract obtained from the LPS-injected mice. However, the binding activity toward the AP-1 binding sequences is not elevated in extracts prepared after the LPS injection. It is possible that most of the p-c-Jun and p-c-Fos elevated by LPS forms a complex with NF-κB, which complex then binds preferentially to the NF-κB-responsive element, not to the AP-1 binding sequences. Also, phosphorylation of ERK1/2 (p-ERK1/2 is known to activate c-Fos by phosphorylation) and c-Jun are activated by LPS, and this activation is inhibited by their respective inhibitors, AG126 and SP600125. Furthermore, nuclear translocation of p65 and p50, which are subunits of NF-κB, is activated by LPS, whereas such activation is inhibited by PDTC and MG132, confirming that the pathways to activate the above transcription factors are functioning in the PG.
Schüle et al. reported that transcription of the osteocalcin gene in ROS17/2.8 cells (rat osteoblastic cell line) transfected with c-fos and c-jun genes for Jun/Fos expression is inhibited under both vitamin-stimulated and nonstimulated conditions. These authors termed such a phenomenon as “cross coupling” [139]. By performing a CAT reporter assay, Stein et al. [146] examined the LTR promoter activity of HIV-1, which contains NF-κB-responsive sequences, and found that co-transfection of HeLa cells with this reporter gene and c-fos and c-jun genes results in a potentiation of the transcriptional activity of LTR (introduction of a mutation in the NF-κB responsive sequence disables the transcriptional activation). Thus, NF-κB and AP-1 family transcription factors p-c-Fos/p-c-Jun were proved to be physically associated to increase DNA binding capacity as well as biological activity, resulting in synergism of these two classes of transcription factors.
This section has given the PG as an example showing that NF-κB and AP-1 form a complex as a result of LPS signaling in the salivary glands and that such a complex actually potentiates transcriptional regulation (transcriptional inhibition) in this tissue [172]. In this example, the MAPK pathway is thought to generate p-c-Fos/p-c-Jun (AP-1), which then binds to NF-κB that has simultaneously been activated and thus potentiating its function. On the other hand, saliva secretion is supposedly reduced by LPS since the AQP5 transcription is strongly suppressed by the endotoxin action. A similar phenomenon is observed in the lungs where the transcription of AQP5 mRNA is suppressed by TNF-α via the NF-κB pathway, causing lung edema, but the MAPK pathway is not involved in this case [155]. Thus, potentiation of NF-κB function by AP-1 or p-c-Fos/p-c-Jun has an important physiological meaning for the proinflammatory action of LPS. The physiological function of negative regulation of AQP5 by LPS needs to be determined further.
IPR-induced downregulation of PG aquaporin 5
Purified μ-calpain cleaves AQP0 protein at 4 positions in vitro, and these cleavage sites correspond to 4 of the 21 positions that are cleaved with age in vivo [87]. Further, calpain can degrade AQP2 expressed in the inner medullary collecting duct of the kidney [131]. As described above, AQP5 is also considered to be a substrate for calpain in the IPR-treated PG. Actually, purified calpain decomposes AQP5 in the membrane fraction of the SMG [15]. It has been suggested that μ-calpain is involved in the IPR-mediated regulation of the AQP5 level since calpain is a calcium (Ca2+)-dependent cysteine protease and the level of cytosolic Ca2+ ions is elevated by IPR [41].
The reduction in the AQP5 protein level by IPR is suppressed by two calpain inhibitors, ALLM and calpeptin, but not by MG132 or lactacystin (both proteasome inhibitors) nor by CQ (a lysosomal denaturant; ref. 15). These data confirmed that AQP5 is a substrate for calpain and that IPR stimulation induces calpain proteolysis to metabolize/decompose AQP5 in the PG. Under normal condition (untreated or without IPR), on the other hand, treatment of mice with MG132, CQ, ALLM, or calpeptin in vivo increases the AQP5 protein level in the PG [15]. This fact implies that ubiquitin-proteasome and lysosomal proteases, the two major proteolytic systems, are functioning in the PG under the normal condition. These results are supported by the report that AQP2 is degraded by proteasomal and lysosomal pathways soon after its synthesis [38].
Aquaporin 5 and salivary gland malfunction under pathological conditions
Impaired saliva secretion takes place under several pathological conditions such as those in patients suffering from Sjögren’s syndrome, those who received irradiation therapy for head and neck cancers, or in patients with sialoadenitis which is caused by various types of pathogenesis.
In patients with Sjögren’s syndrome, abnormal distribution of AQP5 in acinar cells of the salivary gland and lachrymal gland was reported, based on an experiment in which affinity-purified anti-human AQP5 was utilized to localize the antigen by immunohistochemical staining [148, 156]. These studies showed that localization of AQP5 in the apical membrane of acinar cells is minimum while that in the basal membrane is positive, and defective AQP5 trafficking was suggested as the cause of the abnormal distribution of AQP5, which would have resulted in impaired salivary secretion. However, contrary reports have appeared, indicating that AQP5 in Sjögren’s patient remain in the apical membrane and that there is no difference in subcellular localization between Sjögren’s patients and normal subjects ([6] and letter to editor in [29]). These authors used anti-rat AQP5 antibodies and confirmed antibody specificity by preabsorption with the human peptide. Such discrepancies may have been caused by the use of different antibodies in the staining techniques (letter to editor and authors’ reply in [149]). Regarding this issue, however, no conclusion has yet been reached because AQP5 staining at apical membrane is observed in Sjögren’s syndrome patients even when antibody specific for human AQP5 is used [28].
On the other hand, production of autoantibodies against the cell-surface muscarinic cholinergic receptor (M3) is observed in the sera from Sjögren’s syndrome patients. Mouse SMG cells treated with anti-M3 antibody fail to translocate AQP5 to the plasma membrane upon muscarinic agonist stimulation in vitro [118]. Further, the sera from Sjögren’s syndrome patients, but not from those of normal subjects, block the carbachol-induced AQP5 trafficking in HSG cells transfected with GFP-tagged human AQP5 [77]. These studies suggest that defective AQP5 trafficking toward the apical membrane in Sjögren’s syndrome patients may be due to the production of autoantibodies against M3 receptors.
Sjögren’s patients have been given infliximab (anti-TNF α) therapy under the assumption that tumor necrosis factor-α (TNF-α) would be involved as an immunopathogen in the development of this autoimmune disease. The results showed that this antibody therapy increases the unstimulated salivary flow and trafficking of AQP5 to the apical membrane in the acinar cells of the labial gland [147, 150]. It is noteworthy that TNF-α downregulates AQP5 expression in mouse lung epithelial cells via the NF-κB pathway [155] and that activation of this pathway in the mouse parotid gland downregulate AQP5 expression also [172] (see the section LPS-induced downregulation of PG aquaporin 5). These facts support the possibility that medication with anti-TNF-α/infliximab or even inhibitors of the NF-κB pathway is a candidate therapy for a successful treatment to recover from the patients’ symptoms.
Care for head and neck cancer requires surgical removal of the tumor, followed by X-ray irradiation. The negative side effects of radiotherapy will be extended to adjacent normal tissues, which include increased apoptosis and marked decreases in the expression levels of AQP5 and TGF-β in the salivary gland [17]. The basic mechanism underlying such effects and possible treatments to protect the glands from the radiotherapy are being studied [32, 101, 102]. Morgan-Bathke et al. [102] used Atg5 f/f ;Aqp5-Cre mice, which harbor a conditional KO of Atg5, in their salivary acinar cells and are deficient in autophagy. These autophagy-deficient mice have increased radiosensitivity, indicating them to be useful controls to investigate the effects of radiation and/or radiation plus medication on the physiological function of the salivary gland. These researchers found that pretreatment with IGF-1 increases autophagosome formation in normal mice, but not in their Atg5 KO counterparts. The same group showed also that the rapalogue CCI-779 significantly improves the physiological function of the salivary gland diminished by radiation, as measured by determination of the saliva flow rate [101]. Han et al. [32] reported that pretreatment with phenylephrine, an α1 adrenergic agonist, completely protect against the reduction in AQP5 protein levels by irradiation in the rat SMG, although the mechanism is unclear.
Conclusions
AQP5 is involved in the water secretion from the salivary gland acinar cells in both paracellular and transcellular routes, which involvement is supported by the fact that water permeability is actually decreased in AQP5-KO mice and in rats expressing diminished levels of AQP5. Evidence is accumulating that indicates that TRPV4, which regulates the systemic osmotic pressure, is functionally linked to AQP5 in the salivary gland. Physiologically, the AQP5 level is controlled via parasympathetic nerves in the SMG and sympathetic agonists in the PG, and autophagy and lysosome-mediated degradation, as well as calpain proteolysis, are involved in regulating it. Under the pathophysiological condition of an LPS challenge to the PG, NF-κB/MAPK pathways are activated, leading to the activation of the transcriptional factors NF-κB and AP-1 (c-Fos/c-Jun), which form a complex that binds to the NF-κB-responsive element to downregulate potentially the transcription of AQP5 mRNA. Further study is required to establish the actual molecular mechanisms by which AQP5 acts in water secretion from the salivary glands and other exocrine glands. Pathophysiological studies on AQP5 will aid in elucidating the biological significance of this channel protein in the exocrine glands.
Notes
Major intrinsic protein (MIP/MP26/MIP26) of the lens was reported before the discovery of AQP1 [127], and its function had been unknown. Since MIP26 afforded permeation of water and was highly homologous to members of the AQP family, it was later considered to be an AQP [106]. Thus the protein and gene of MIP26 are referred to as AQP0 [99, 117].
Abbreviations
- ALLM:
-
N-Ac-Leu-Leu-methininal
- AP-1:
-
Activator protein 1
- AQP:
-
Aquaporin
- CCh:
-
Carbachol
- CTD:
-
Chorda timpani denervation
- CQ:
-
Chloroquine
- DPPVI:
-
Dipeptidyl peptidase IV
- E a :
-
Activation energy
- EMSA:
-
Electrophoretic mobility shift assay
- ERK1/2:
-
Extracellular signal-regulated kinases 1/2
- GFP:
-
Green fluorescent protein
- IPR:
-
Isoproterenol
- KO:
-
Knockout
- LC3B-II:
-
Microtubule-associated protein 1 light chain 3 isoform B-II
- LPS:
-
Lipopolysaccharide
- MDCK:
-
Madin-Darby canine kidney
- MAPK:
-
Mitogen-activated protein kinase
- NF-κB:
-
Nuclear factor-kappa B
- PG:
-
Parotid gland
- P d :
-
Diffusive water permeability
- P f :
-
Osmotic water permeability
- RVD:
-
Regulatory volume decrease
- SMG:
-
Submandibular gland
- SNP:
-
Single nucleotide polymorphism
- TRPV4:
-
Transient receptor potential cation channel, subfamily V, member 4
References
Abdul-Wahab A, Takeichi T, Liu L, Lomas D, Hughes B, Akiyama M, McGrath JA, Mellerio JE (2015) Autosomal dominant diffuse non-epidermolytic palmoplantar keratoderma due to a recurrent mutation in aquaporin-5. Br J Dermatol. doi: 10.1111/bjd.13931 [Epub ahead of print]
Akamatsu T, Parvin MN, Murdiastuti K, Kosugi-Tanaka C, Yao C, Miki O, Kanamori N, Hosoi K (2003) Expression and localization of aquaporins, members of the water channel family, during development of the rat submandibular gland. Pflügers Arch-Eur J Physiol 446:641–651
Aure MH, Røed A, Galtung HK (2010) Intracellular Ca2+ responses and cell volume regulation upon cholinergic and purinergic stimulation in an immortalized salivary cell line. Eur J Oral Sci 118:237–244
Azlina A, Javkhlan P, Hiroshima Y, Hasegawa T, Yao C, Akamatsu T, Hosoi K (2010) Roles of lysosomal proteolytic systems in AQP5 degradation in the submandibular gland of rats following chorda tympani parasympathetic denervation. Am J Physiol-Gastrointest Liver Physiol 299:G1106–G1117
Begenisich T, Nakamoto T, Ovitt CE, Nehrke K, Brugnara C, Alper SL, Melvin JE (2004) Physiological roles of the intermediate conductance, Ca2+-activated potassium channel Kcnn4. J Biol Chem 279:47681–47687
Beroukas D, Hiscock J, Jonsson R, Waterman SA, Gordon TP (2001) Subcellular distribution of aquaporin 5 in salivary glands in primary Sjögren’s syndrome. Lancet 358:1875–1876
Berry V, Francis P, Kaushal S, Moore A, Bhattacharya S (2000) Missense mutations in MIP underlie autosomal dominant ‘polymorphic’ and lamellar cataracts linked to 12q. Nat Genet 25:15–17
Bienert GP, Chaumont F (2014) Aquaporin-facilitated transmembrane diffusion of hydrogen peroxide. Biochim Biophys Acta 1840:1596–604
Bienert GP, Møller AL, Kristiansen KA, Schulz A, Møller IM, Schjoerring JK, Jahn TP (2007) Specific aquaporins facilitate the diffusion of hydrogen peroxide across membranes. J Biol Chem 282:1183–1192
Blaydon DC, Lind LK, Plagnol V, Linton KJ, Smith FJ, Wilson NJ, McLean WH, Munro CS, South AP, Leigh IM, O’Toole EA, Lundström A, Kelsell DP (2013) Mutations in AQP5, encoding a water-channel protein, cause autosomal-dominant diffuse nonepidermolytic palmoplantar keratoderma. Am J Hum Genet 93:330–335
Burghardt B, Elkaer ML, Kwon TH, Rácz GZ, Varga G, Steward MC, Nielsen S (2003) Distribution of aquaporin water channels AQP1 and AQP5 in the ductal system of the human pancreas. Gut 52:1008–1016
Candreia C, Schmuziger N, Gürtler N (2010) Molecular analysis of aquaporin genes 1 to 4 in patients with Menière’s disease. Cell Physiol Biochem 26:787–792
Cao X, Yin J, Wang H, Zhao J, Zhang J, Dai L, Zhang J, Jiang H, Lin Z, Yang Y (2014) Mutation in AQP5, encoding aquaporin 5, causes palmoplantar keratoderma Bothnia type. J Invest Dermatol 134:284–287
Chanprasertyothin S, Saetung S, Rajatanavin R, Ongphiphadhanakul B (2010) Genetic variant in the aquaporin 9 gene is associated with bone mineral density in postmenopausal women. Endocrine 38:83–86
Chen G, Yao C, Hasegawa T, Akamatsu T, Yoshimura H, Hosoi K (2014) Effects of isoproterenol on aquaporin 5 levels in the parotid gland of mice in vivo. Am J Physiol-Endocrinol Metab 306:E100–E108
Chepelinsky AB (2009) Structural function of MIP/aquaporin 0 in the eye lens; genetic defects lead to congenital inherited cataract. In: Beitz E (ed) Handbook of experimental pharmacology (aquaporins), vol 190. Springer, Heidelberg, Germany, pp 265–297
Choi JH, Wu HG, Jung KC, Lee SH, Kwon EK (2009) Apoptosis and expression of AQP5 and TGF-beta in the irradiated rat submandibular gland. Cancer Res Treat 41:145–154
Chou CL, Ma T, Yang B, Knepper MA, Verkman AS (1998) Fourfold reduction of water permeability in inner medullary collecting duct of aquaporin-4 knockout mice. Am J Physiol 274:C549–C554
Dawes C, Jenkins GN (1964) The effects of different stimuli on the composition of saliva in man. J Physiol 170:86–100
Delporte C, Steinfeld S (2006) Distribution and roles of aquaporins in salivary glands. Biochim Biophys Acta 1758:1061–1070
DiGiovanni SR, Nielsen S, Christensen EI, Knepper MA (1994) Regulation of collecting duct water channel expression by vasopressin in Brattleboro rat. Proc Natl Acad Sci U S A 91:8984–8988
Elkjaer ML, Nejsum LN, Gresz V, Kwon TH, Jensen UB, Frøkiaer J, Nielsen S (2001) Immunolocalization of aquaporin-8 in rat kidney, gastrointestinal tract, testis, and airways. Am J Physiol Renal Physiol 281:F1047–F1057
Evans RL, Park K, Turner RJ, Watson GE, Nguyen HV, Dennett MR, Hand AR, Flagella M, Shull GE, Melvin JE (2000) Severe impairment of salivation in Na+/K+/2Cl−cotransporter (NKCC1)-deficient mice. J Biol Chem 275:26720–26726
Foskett JK (1990) [Ca2+]i modulation of Cl− content controls cell volume in single salivary acinar cells during fluid secretion. Am J Physiol-Cell Physiol 259:C998–C1004
Francis P, Berry V, Bhattacharya S, Moore A (2000) Congenital progressive polymorphic cataract caused by a mutation in the major intrinsic protein of the lens, MIP (AQP0). Br J Ophthalmol 84:1376–1379
Fushimi K, Uchida S, Hara Y, Hirata Y, Marumo F, Sasaki S (1993) Cloning and expression of apical membrane water channel of rat kidney collecting tubule. Nature 361:549–552
Geyer DD, Spence MA, Johannes M, Flodman P, Clancy KP, Berry R, Sparkes RS, Jonsen MD, Isenberg SJ, Bateman JB (2006) Novel single base deletional mutation in major intrinsic protein (MIP) in autosomal dominant cataract. Am J Ophthalmol 141:761–763
Gresz V, Horvath A, Gera I, Nielsen S, Zelles T (2015) Immunolocalization of AQP5 in resting and stimulated normal labial glands and in Sjögren’s syndrome. Oral Dis 21:e114–120
Groneberg DA, Gerber A, Fischer A (2001) Trafficking of lacrimal aquaporin-5 in Sjögren’s syndrome (Letter to editor). Lancet 357:2054–2055
Gu F, Zhai H, Li D, Zhao L, Li C, Huang S, Ma X (2007) A novel mutation in major intrinsic protein of the lens gene (MIP) underlies autosomal dominant cataract in a Chinese family. Mol Vis 13:1651–1656
Gustafson CE, Levine S, Katsura T, McLaughlin M, Alexio MD, Tamarappoo BK, Verkman AS, Brown D (1998) Vasopressin regulated trafficking of a green fluorescent protein-aquaporin 2 chimera in LLC-PK1 cells. Histochem Cell Biol 110:377–386
Han L, Wang L, Zhang F, Liu KJ, Xiang B (2015) Effect of phenylephrine pretreatment on the expressions of aquaporin 5 and c-Jun N-Terminal kinase in irradiated submandibular gland. Radiat Res 183:693–700
Hansel NN, Sidhaye V, Rafaels NM, Gao L, Gao P, Williams R, Connett JE, Beaty TH, Mathias RA, Wise RA, King LS, Barnes KC (2010) Aquaporin 5 polymorphisms and rate of lung function decline in chronic obstructive pulmonary disease. PLoS One 5:e14226. doi:10.1371/journal.pone.0014226
Hara M, Ma T, Verkman AS (2002) Selectively reduced glycerol in skin of aquaporin-3-deficient mice may account for impaired skin hydration, elasticity, and barrier recovery. J Biol Chem 277:46616–46621
Hara-Chikuma M, Verkman AS (2008) Roles of aquaporin-3 in the epidermis. J Invest Dermatol 128:2145–2151
Hasegawa T, Azlina A, Javkhlan P, Yao C, Akamatsu T, Hosoi K (2011) Novel phosphorylation of aquaporin-5 at its threonine 259 through cAMP signaling in salivary gland cells. Am J Physiol-Cell Physiol 301:C667–C678
Hasegawa H, Ma T, Skach W, Matthay MA, Verkman AS (1994) Molecular cloning of a mercurial-insensitive water channel expressed in selected water-transporting tissues. J Biol Chem 269:5497–5500
Hasler U, Mordasini D, Bens M, Bianchi M, Cluzeaud F, Rousselot M, Vandewalle A, Feraille E, Martin PY (2002) Long term regulation of aquaporin-2 expression in vasopressin-responsive renal collecting duct principal cells. J Biol Chem 277:10379–10386
Hatakeyama S, Yoshida Y, Tani T, Koyama Y, Nihei K, Ohshiro K, Kamiie JI, Yaoita E, Suda T, Hatakeyama K, Yamamoto T (2001) Cloning of a new aquaporin (AQP10) abundantly expressed in duodenum and jejunum. Biochem Biophys Res Commun 287:814–819
Herrera M, Hong NJ, Ortiz PA, Garvin JL (2009) Endothelin-1 inhibits thick ascending limb transport via Akt-stimulated nitric oxide production. J Biol Chem 284:1454–1460
Horn VJ, Baum BJ, Ambudkar IS (1988) β-Adrenergic receptor stimulation induces inositol trisphosphate production and Ca2+ mobilization in rat parotid acinar cells. J Biol Chem 263:12454–1260
Iandiev I, Dukic-Stefanovic S, Hollborn M, Pannicke T, Hartig W, Wiedemann P, Reichenbach A, Bringmann A, Kohen L (2011) Immunolocalization of aquaporin-6 in the rat retina. Neurosci Lett 490:130–134
Ishibashi K (2009) New members of mammalian aquaporins: AQP10-AQP12. In: Beitz E (ed) Handbook of experimental pharmacology (aquaporins), vol 190. Springer, Heidelberg, Germany, pp 251–262
Ishibashi K, Koike S, Kondo S, Hara S, Tanaka Y (2009) The role of a group III AQP, AQP11 in intracellular organelle homeostasis. J Med Invest 56:312–317
Ishibashi K, Kuwahara M, Gu Y, Kageyama Y, Tohsakai A, Suzuki F, Marumo F, Sasaki S (1997) Cloning and functional expression of a new water channel abundantly expressed in the testis permeable to water, glycerol, and urea. J Biol Chem 272:20782–20786
Ishibashi K, Kuwahara M, Gu Y, Tanaka Y, Marumo F, Sasaki S (1998) Cloning and functional expression of a new aquaporin (AQP9) abundantly expressed in the peripheral leukocytes permeable to water and urea, but not to glycerol. Biochem Biophys Res Commun 244:268–274
Ishibashi K, Kuwahara M, Kageyama Y, Tohsaka A, Marumo F, Sasaki S (1997) Cloning and functional expression of a second new aquaporin abundantly expressed in testis. Biochem Biophys Res Commun 237:714–718
Ishibashi K, Morinaga T, Kuwahara M, Sasaki S, Imai M (2002) Cloning and identification of a new member of water channel (AQP10) as an aquaglyceroporin. Biochim Biophys Acta 1576:335–340
Ishibashi K, Sasaki S (1997) Aquaporin water channels in mammals. Clin Exp Nephrol 1:247–253
Ishibashi K, Sasaki S, Fushimi K, Uchida S, Kuwahara M, Saito H, Furukawa T, Nakajima K, Yamaguchi Y, Gojobori T, Marumo F (1994) Molecular cloning and expression of a member of the aquaporin family with permeability to glycerol and urea in addition to water expressed at the basolateral membrane of kidney collecting duct cells. Proc Natl Acad Sci U S A 91:6269–6273
Ishibashi K, Tanaka Y, Morishita Y (2014) The role of mammalian superaquaporins inside the cell. Biochim Biophys Acta 1840:1507–1512
Ishibashi K, Yamauchi K, Kageyama Y, Saito-Ohara F, Ikeuchi T, Marumo F, Sasaki S (1998) Molecular characterization of human aquaporin-7 gene and its chromosomal mapping. Biochim Biophys Acta 1399:62–66
Itoh T, Rai T, Kuwahara M, Ko SB, Uchida S, Sasaki S, Ishibashi K (2005) Identification of a novel aquaporin, AQP12, expressed in pancreatic acinar cells. Biochem Biophys Res Commun 330:832–838
Jelen S, Gena P, Lebeck J, Rojek A, Praetorius J, Frøkiaer J, Fenton RA, Nielsen S, Calamita G, Rützler M (2012) Aquaporin-9 and urea transporter-A gene deletions affect urea transmembrane passage in murine hepatocytes. Am J Physiol Gastrointest Liver Physiol 303:G1279–G1287
Jung JS, Preston GM, Smith BL, Guggino WB, Agre P (1994) Molecular structure of the water channel through aquaporin CHIP. The hourglass model. J Biol Chem 269:14648–14654
Jungersted JM, Bomholt J, Bajraktari N, Hansen JS, Klærke DA, Pedersen PA, Hedfalk K, Nielsen KH, Agner T, Hélix-Nielsen C (2013) In vivo studies of aquaporins 3 and 10 in human stratum corneum. Arch Dermatol Res 305:699–704
Kamsteeg EJ, Hendriks G, Boone M, Konings IB, Oorschot V, Sluijs PV, Klumperman J, Deen PM (2006) Short-chain ubiquitination mediates the regulated endocytosis of the aquaporin-2 water channel. Proc Natl Acad Sci U S A 103:18344–18349
Karabasil MR, Hasegawa T, Azlina A, Purwanti N, Yao C, Akamatsu T, Tomioka S, Hosoi K (2011) Effects of naturally occurring G103D point mutation of AQP5 on its water permeability, trafficking, and cellular localization in the submandibular gland of rats. Biol Cell 103:69–86
Kasimir-Bauer S, Heubner M, Otterbach F, Kimmig R, Siffert W, Adamzik M (2009) Prognostic relevance of the AQP5–1364C>A polymorphism in primary breast cancer. Mol Med Rep 2:645–650
Kawedia JD, Nieman ML, Boivin GP, Melvin JE, Kikuchi K, Hand AR, Lorenz JN, Menon AG (2007) Interaction between transcellular and paracellular water transport pathways through aquaporin 5 and the tight junction complex. Proc Natl Acad Sci U S A 104:3621–3626
King LS, Agre P (1996) Pathophysiology of the aquaporin water channel. Ann Rev Physiol 58:619–618
King LS, Choi M, Fernandez PC, Cartron JP, Agre P (2001) Defective urinary-concentrating ability due to a complete deficiency of aquaporin-1. N Engl J Med 345:175–179
King LS, Nielsen S, Agre P (1996) Aquaporin-1 water channel protein in lung: ontogeny, steroid-induced expression, and distribution in rat. J Clin Invest 97:2183–2191
Kishida K, Kuriyama H, Funahashi T, Shimomura I, Kihara S, Ouchi N, Nishida M, Nishizawa H, Matsuda M, Takahashi M, Hotta K, Nakamura T, Yamashita S, Tochino Y, Matsuzawa Y (2000) Aquaporin adipose, a putative glycerol channel in adipocytes. J Biol Chem 275:20896–20902
Kishida K, Shimomura I, Kondo H, Kuriyama H, Makino Y, Nishizawa H, Maeda N, Matsuda M, Ouchi N, Kihara S, Kurachi Y, Funahashi T, Matsuzawa Y (2001) Aquaporin adipose (AQPap), adipose-specific glycerol channel. J Biol Chem 276:36251–3660
Kondo H, Shimomura I, Kishida K, Kuriyama H, Makino Y, Nishizawa H, Matsuda M, Maeda N, Nagaretani H, Kihara S, Kurachi Y, Nakamura T, Funahashi T, Matsuzawa Y (2002) Human aquaporin adipose (AQPap) gene. Genomic structure, promoter analysis and functional mutation. Eur J Biochem 269:1814–1826
Kosugi-Tanaka C, Li X, Yao C, Akamatsu T, Kanamori N, Hosoi K (2006) Protein kinase A-regulated membrane trafficking of a green fluorescent protein-aquaporin 5 chimera in MDCK cells. Biochim Biophys Acta 1763:337–344
Koyama Y, Yamamoto T, Kondo D, Funaki H, Yaoita E, Kawasaki K, Sato N, Hatakeyama K, Kihara I (1997) Molecular cloning of a new aquaporin from rat pancreas and liver. J Biol Chem 272:30329–30333
Krane CM, Fortner CN, Hand AR, McGraw DW, Lorenz JN, Wert SE, Towne JE, Paul RJ, Whitsett JA, Menon AG (2001) Aquaporin 5-deficient mouse lungs are hyper responsive to cholinergic stimulation. Proc Natl Acad Sci U S A 98:14114–14119
Krane CM, Zimmerman SL, Staton A, Azmeh R, Moredock K (2007) Single nucleotide polymorphisms in the 3′UTR of the human aquaporin 5 gene affect gene expression. In: The 5th international conference of aquaporin, exploring new functions of aquaporin, Program and Abstract Book., pp 58–59
Kuriyama H, Kawamoto S, Ishida N, Ohno I, Mita S, Matsuzawa Y, Matsubara K, Okubo K (1997) Molecular cloning and expression of a novel human aquaporin from adipose tissue with glycerol permeability. Biochem Biophys Res Commun 241:53–58
Kuriyama H, Shimomura I, Kishida K, Kondo H, Furuyama N, Nishizawa H, Maeda N, Matsuda M, Nagaretani H, Kihara S, Nakamura T, Tochino Y, Funahashi T, Matsuzawa Y (2002) Coordinated regulation of fat-specific and liver-specific glycerol channels, aquaporin adipose and aquaporin 9. Diabetes 51:2915–2921
Laforenza U, Scaffino MF, Gastaldi G (2013) Aquaporin-10 represents an alternative pathway for glycerol efflux from human adipocytes. PLoS One 8:e54474. doi:10.1371/journal.pone.0054474
Lambertz N, Hindy NE, Adler C, Rump K, Adamzik M, Keyvani K, Bankfalvi A, Siffert W, Erol Sandalcioglu I, Bachmann HS (2013) Expression of aquaporin 5 and the AQP5 polymorphism A(−1364)C in association with peritumoral brain edema in meningioma patients. J Neurooncol 112:297–305
Larsen HS, Ruus AK, Schreurs O, Galtung HK (2010) Aquaporin 11 in the developing mouse submandibular gland. Eur J Oral Sci 118:9–13
Lebeck J (2014) Metabolic impact of the glycerol channels AQP7 and AQP9 in adipose tissue and liver. J Mol Endocrinol 52:R165–R178
Lee BH, Gauna AE, Perez G, Park YJ, Pauley KM, Kawai T, Cha S (2013) Autoantibodies against muscarinic type 3 receptor in Sjögren’s syndrome inhibit aquaporin 5 trafficking. PLoS One 8:e53113
Leitch V, Agre P, King LS (2001) Altered ubiquitination and stability of aquaporin-1 in hypertonic stress. Proc Natl Acad Sci U S A 98:2894–2898
Li X, Azlina A, Karabasil MR, Purwanti N, Hasegawa T, Yao C, Akamatsu T, Hosoi K (2008) Degradation of submandibular gland AQP5 by parasympathetic denervation of chorda tympani and its recovery by cevimeline, an M3 muscarinic agonist. Am J Physiol-Gastrointest Liver Physiol 295:G112–G123
Li Y, Liu H, Zhao H, Xu C, Zhao Y, Ma J, Chen ZJ (2013) Association of AQP8 in women with PCOS. Reprod Biomed Online 27:419–422
Liedtke W, Choe Y, Martí-Renom MA, Bell AM, Denis CS, Sali A, Hudspeth AJ, Friedman JM, Heller S (2000) Vanilloid receptor-related osmotically activated channel (VR-OAC), a candidate vertebrate osmoreceptor. Cell 103:525–535
Lipschutz JH, Li S, Arisco A, Balkovetz DF (2005) Extracellular signal-regulated kinases 1/2 control claudin-2 expression in Madin-Darby canine kidney strain I and II cells. J Biol Chem 280:3780–3788
Litman T, Søgaad R, Zeuthen T (2009) Ammonia and urea permeability of mammalian aquaporins. In: Beitz E (ed) Handbook of experimental pharmacology (aquaporins), vol 190. Springer, Heidelberg, Germany, pp 327–358
Liu X, Bandyopadhyay BC, Nakamoto T, Singh B, Liedtke W, Melvin JE, Ambudkar I (2006) A role for AQP5 in activation of TRPV4 by hypotonicity: concerted involvement of AQP5 and TRPV4 in regulation of cell volume recovery. J Biol Chem 281:15485–15495
Liu Z, Shen J, Carbrey JM, Mukhopadhyay R, Agre P, Rosen BP (2002) Arsenite transport by mammalian aquaglyceroporins AQP7 and AQP9. Proc Natl Acad Sci U S A 99:6053–6058
Lundberg A (1957) Anionic dependence of secretion and secretory potentials in the perfused sublingual gland. Acta Physiol Scand 40:101–112
Ma H, Azuma M, Shearer TR (2005) Degradation of human aquaporin 0 by m-calpain. FEBS Lett 579:6745–6748
Ma T, Frigeri A, Hasegawa H, Verkman AS (1994) Cloning of a water channel homolog expressed in brain meningeal cells and kidney collecting duct that functions as a stilbene-sensitive glycerol transporter. J Biol Chem 269:21845–21849
Ma T, Fukuda N, Song Y, Matthay MA, Verkman AS (2000) Lung fluid transport in aquaporin-5 knockout mice. J Clin Invest 105:93–100
Ma T, Hara M, Sougrat R, Verbavatz JM, Verkman AS (2002) Impaired stratum corneum hydration in mice lacking epidermal water channel aquaporin-3. J Biol Chem 277:17147–17153
Ma T, Song Y, Gillespie A, Carlson EJ, Epstein CJ, Verkman AS (1999) Defective secretion of saliva in transgenic mice lacking aquaporin-5 water channels. J Biol Chem 274:20071–20074
Ma T, Song Y, Yang B, Gillespie A, Carlson EJ, Epstein CJ, Verkman AS (2000) Nephrogenic diabetes insipidus in mice lacking aquaporin-3 water channels. Proc Natl Acad Sci U S A 97:4386–4391
Ma T, Yang B, Gillespie A, Carlson EJ, Epstein CJ, Verkman AS (1997) Generation and phenotype of a transgenic knockout mouse lacking the mercurial-insensitive water channel aquaporin-4. J Clin Invest 100:957–962
Ma T, Yang B, Verkman AS (1997) Cloning of a novel water and urea-permeable aquaporin from mouse expressed strongly in colon, placenta, liver, and heart. Biochem Biophys Res Commun 240:324–328
Maeda N, Funahashi T, Shimomura I (2008) Metabolic impact of adipose and hepatic glycerol channels aquaporin 7 and aquaporin 9. Nat Clin Pract Endocrinol Metab 4:627–634
Maekawa C, Kitahara T, Kizawa K, Okazaki S, Kamakura T, Horii A, Imai T, Doi K, Inohara H, Kiyama H (2010) Expression and translocation of aquaporin-2 in the endolymphatic sac in patients with Meniere’s disease. J Neuroendocrinol 22:1157–1164
Magdeldin S, Li H, Yoshida Y, Enany S, Zhang Y, Xu B, Fujinaka H, Yaoita E, Yamamoto T (2010) Comparison of two dimensional electrophoresis mouse colon proteomes before and after knocking out aquaporin 8. J Proteomics 73:2031–2040
Matsuki M, Hashimoto S, Shimono M, Murakami M, Fujita-Yoshigaki J, Furuyama S, Sugiya H (2005) Involvement of aquaporin-5 water channel in osmoregulation in parotid secretory granules. J Membrane Biol 203:119–126
Mitton KP, Kamiya T, Tumminia SJ, Russell P (1996) Cysteine protease activated by expression of HIV-1 protease in transgenic mice. MIP26 (aquaporin-0) cleavage and cataract formation in vivo and ex vivo. J Biol Chem 271:31803–31806
Mizushima N (2007) Autophagy: process and function. Genes Develop 21:2861–2873
Morgan-Bathke M, Harris ZI, Arnett DG, Klein RR, Burd R, Ann DK, Limesand KH (2014) The rapalogue, CCI-779, improves salivary gland function following radiation. PLoS One 9:e113183
Morgan-Bathke M, Hill GA, Harris ZI, Lin HH, Chibly AM, Klein RR, Burd R, Ann DK, Limesand KH (2014) Autophagy correlates with maintenance of salivary gland function following radiation. Sci Rep 4:5206
Morinaga T, Nakakoshi M, Hirao A, Imai M, Ishibashi K (2002) Mouse aquaporin 10 gene (AQP10) is a pseudogene. Biochem Biophys Res Commun 294:630–634
Morishita Y, Matsuzaki T, Hara-Chikuma M, Andoo A, Shimono M, Matsuki A, Kobayashi K, Ikeda M, Yamamoto T, Verkman A, Kusano E, Ookawara S, Takata K, Sasaki S, Ishibashi K (2005) Disruption of aquaporin-11 produces polycystic kidneys following vacuolization of the proximal tubule. Mol Cell Biol 25:7770–7779
Morris RG, Uchida S, Brooks H, Knepper MA, Chou CL (2005) Altered expression profile of transporters in the inner medullary collecting duct of aquaporin-1 knockout mice. Am J Physiol Renal Physiol 289:F194–F199
Mulders SM, Preston GM, Deen PM, Guggino WB, van Os CH, Agre P (1995) Water channel properties of major intrinsic protein of lens. J Biol Chem 270:9010–9016
Murakami M, Murdiastuti K, Hosoi K, Hill AE (2006) AQP and the control of fluid transport in a salivary gland. J Membr Biol 210:91–103
Murakami M, Shachar-Hill B, Steward MC, Hill AE (2001) The paracellular component of water flow in the rat submandibular salivary gland. J Physiol 537:899–906
Murata K, Mitsuoka K, Hirai T, Walz T, Agre P, Heymann JB, Engel A, Fujiyoshi Y (2000) Structural determinants of water permeation through aquaporin-1. Nature 407:599–605
Murdiastuti K (2005) Point mutation in a gene for aquaporin 5, an exocrine gland-type water channel, and its effects on the salivary gland function in rats. In: Dissertation submitted to the Graduate School of Oral Sciences, The University of Tokushima Graduate School for the Degree of Doctor of Philosophy in Dentistry
Murdiastuti K, Miki O, Yao C, Parvin MN, Kosugi C, Akamatsu T, Kanamori N, Hosoi K (2002) Divergent expression and localization of aquaporin 5, an exocrine-type water channel, in the submandibular gland of Sprague–Dawley rats. Pflügers Arch-Eur J Physiol 445:405–412
Murdiastuti K, Purwanti N, Karabasil MR, Li X, Yao C, Akamatsu T, Kanamori N, Hosoi K (2006) A naturally occurring point mutation in the rat aquaporin 5 gene, influencing its protein production by and secretion of water from salivary glands. Am J Physiol-Gastrointest Liver Physiol 291:G1081–G1088
Nakahari T, Imai Y (1998) Transient swelling of salivary acinus induced by acetylcholine stimulation: water secretion pathway in rat submandibular gland. J Membr Biol 161:287–296
Nakhoul NL, Davis BA, Romero MF, Boron WF (1998) Effect of expressing the water channel aquaporin-1 on the CO2 permeability of Xenopus oocytes. Am J Physiol 274:C543–C548
Nauntofte B (1992) Regulation of electrolyte and fluid secretion in salivary acinar cells. Am J Physiol-Gastrointest Liver Physiol 263:G823–G837
Nejsum LN, Kwon TH, Jensen UB, Fumagalli O, Frøkiaer J, Krane CM, Menon AG, King LS, Agre PC, Nielsen S (2002) Functional requirement of aquaporin-5 in plasma membranes of sweat glands. Proc Natl Acad Sci U S A 99:511–516
Németh-Cahalan KL, Hall JE (2000) pH and calcium regulate the water permeability of aquaporin 0. J Biol Chem 275:6777–6782
Nguyen KH, Brayer J, Cha S, Diggs S, Yasunari U, Hilal G, Peck AB, Humphreys-Beher MG (2000) Evidence for antimuscarinic acetylcholine receptor antibody-mediated secretory dysfunction in nod mice. Arthritis Rheum 43:2297–306
Nicchia GP, Ficarella R, Rossi A, Giangreco I, Nicolotti O, Carotti A, Pisani F, Estivill X, Gasparini P, Svelto M, Frigeri A (2011) D184E mutation in aquaporin-4 gene impairs water permeability and links to deafness. Neuroscience 197:80–88
Ohta E, Itoh T, Nemoto T, Kumagai J, Ko SBH, Ishibashi K, Ohno M, Uchida K, Ohta A, Sohara E, Uchida S, Sasaki S, Rai T (2009) Pancreas-specific aquaporin 12 null mice showed increased susceptibility to caerulein-induced acute pancreatitis. Am J Physiol-Cell Physiol 297:C1368–C1378
Okada S, Misaka T, Tanaka Y, Matsumoto I, Ishibashi K, Sasaki S, Abe K (2008) Aquaporin-11 knockout mice and polycystic kidney disease animals share a common mechanism of cyst formation. FASEB J 22:3672–3684
Pallone TL, Edwards A, Ma T, Silldorff EP, Verkman AS (2000) Requirement of aquaporin-1 for NaCl driven water transport across descending vasa recta. J Clin Invest 105:215–222
Pani B, Liu X, Bollimuntha S, Cheng KT, Niesman IR, Zheng C, Achen VR, Patel HH, Ambudkar IS, Singh BB (2013) Impairment of TRPC1-STIM1 channel assembly and AQP5 translocation compromise agonist-stimulated fluid secretion in mice lacking caveolin1. J Cell Sci 126:667–675
Papadopoulos MC, Verkman AS (2005) Aquaporin-4 gene disruption in mice reduces brain swelling and mortality in pneumococcal meningitis. J Bol Chem 280:13906–13912
Parvin MN, Kurabuchi S, Murdiastuti K, Yao C, Kosugi-Tanaka C, Akamatsu T, Kanamori N, Hosoi K (2005) Subcellular redistribution of AQP5 by vasoactive intestinal polypeptide (VIP) in the Brunner’s gland of the rat duodenum. Am J Physiol-Gastrointest Liver Physiol 288:G1283–G1291
Parvin MN, Tsumura K, Akamatsu T, Kanamori N, Hosoi K (2002) Expression and localization of AQP5 in the stomach and duodenum of the rat. Biochim Biophys Acta Mol Cell Res 1542:116–124
Pisano MM, Chepelinsky AB (1992) Genomic cloning, complete nucleotide sequence, and structure of the human gene encoding the major intrinsic protein (MIP) of the lens. Genomics 11:981–990
Preston GM, Carroll TP, Guggino WB, Agre P (1992) Appearance of water channels in Xenopus oocytes expressing red cell CHIP28 protein. Science 256:385–387
Preston GM, Smith BL, Zeidel ML, Moulds JJ, Agre P (1994) Mutations in aquaporin-1 in phenotypically normal humans without functional CHIP water channels. Science 265:1585–1587
Price HD, Thompson TE (1969) Properties of liquid bilayer membranes separating two aqueous phases: temperature dependence of water permeability. J Mol Biol 41:443–457
Puliyanda DP, Ward DT, Baum MA, Hammond TG, Harris HW Jr (2003) Calpain-mediated AQP2 proteolysis in inner medullary collecting duct. Biochem Biophys Res Commun 303:52–58
Raina S, Preston GM, Guggino WB, Agre P (1995) Molecular cloning and characterization of an aquaporin cDNA from salivary, lacrimal, and respiratory tissues. J Biol Chem 270:1908–1912
Redwood WR, Haydon DA (1969) Influence of temperature and membrane composition on the water permeability of lipid bilayers. J Theor Biol 22:1–8
Ripoche P, Gane P, Le Pennec PY, Daniels G, Cartron JP, Bailly P (2002) AQP3 deficiency in humans and the molecular basis of a novel blood group system, GIL. J Biol Chem 277:45854–45859
Rojek A, Füchtbauer EM, Füchtbauer A, Jelen S, Malmendal A, Fenton RA, Nielsen S (2013) Liver-specific aquaporin 11 knockout mice show rapid vacuolization of the rough endoplasmic reticulum in periportal hepatocytes after amino acid feeding. Am J Physiol Gastrointest Liver Physiol 304:G501–G515
Romanenko V, Nakamoto T, Srivastava A, Melvin JE, Begenisich T (2006) Molecular identification and physiological roles of parotid acinar cell maxi-K channels. J Biol Chem 281:27964–27972
Rosenberg PA, Finkelstein A (1978) Water permeability of gramicidin A-treated lipid bilayer membranes. J Gen Physiol 72:341–350
Sands JM, Flores FX, Kato A, Baum MA, Brown EM, Ward DT, Hebert SC, Harris HW (1998) Vasopressin-elicited water and urea permeabilities are altered in IMCD in hypercalcemic rats. Am J Physiol-Renal Physiol 274:F978–F985
Satoh K, Seo Y, Matsuo S, Karabasil MR, Matsuki-Fukushima M, Nakahari T, Hosoi K (2012) Roles of AQP5/AQP5-G103D in carbamylcholine-induced volume decrease and in reduction of the activation energy for water transport by rat parotid acinar cells. Pflügers Arch-Eur J Physiol 464:375–389
Schüle R, Umesono K, Mangelsdorf DJ, Bolado J, Pike JW, Evans RM (1990) Jun-Fos and receptors for vitamins A and D recognize a common response element in the human osteocalcin gene. Cell 61:497–504
Segawa A (1994) Tight junctional permeability in living cells: dynamic changes directly visualized by confocal laser microscopy. J Electron Microsc (Tokyo) 43:290–298
Shiels A, Bassnett S, Varadaraj K, Mathias R, Al-Ghoul K, Kuszak J, Donoviel D, Lilleberg S, Friedrich G, Zambrowicz B (2001) Optical dysfunction of the crystalline lens in aquaporin-0-deficient mice. Physiol Genomics 7:179–186
Sidhaye VK, Güler AD, Schweitzer KS, D’Alessio F, Caterina MJ, King LS (2006) Transient receptor potential vanilloid 4 regulates aquaporin-5 abundance under hypotonic conditions. Proc Natl Acad Sci U S A 103:4747–4752
Sidhaye V, Hoffert JD, King LS (2005) cAMP has distinct acute and chronic effects on aquaporin-5 in lung epithelial cells. J Biol Chem 280:3590–3596
Sohara E, Rai T, Sasaki S, Uchida S (2006) Physiological roles of AQP7 in the kidney: lessons from AQP7 knockout mice. Biochim Biophys Acta 1758:1106–1110
Stein B, Baldwin AS Jr, Ballard DW, Greene WC, Angel P, Herrlich P (1993) Cross-coupling of the NF-kappa B p65 and Fos/Jun transcription factors produces potentiated biological function. EMBO J 12:3879–3891
Steinfeld SD, Appelboom T, Delporte C (2002) Treatment with infliximab restores normal aquaporin 5 distribution in minor salivary glands of patients with Sjögren’s syndrome. Arthritis Rheum 46:2249–2251
Steinfeld S, Cogan E, King LS, Agre P, Kiss R, Delporte C (2001) Abnormal distribution of aquaporin-5 water channel protein in salivary glands from Sjögren’s syndrome patients. Lab Invest 81:143–148
Steinfeld SD, Delporte C (2002) Distribution of salivary aquaporin-5 in Sjögren’s syndrome. (Letter to editor and authors reply by Waterman, SA, Beroukas D (pp 1778) and Groneberg DA, Peiser C, Fischer A (pp 1778–1779)). Lancet 359:1777–1778
Steinfeld SD, Demols P, Salmon I, Kiss R, Appelboom T (2001) Infliximab in patients with primary Sjögren’s syndrome: a pilot study. Arthritis Rheum 44:2371–2375
Strotmann R, Harteneck C, Nunnenmacher K, Schultz G, Plant TD (2000) OTRPC4, a nonselective cation channel that confers sensitivity to extracellular osmolarity. Nat Cell Biol 2:695–702
Su W, Guan X, Zhang D, Sun M, Yang L, Yi F, Hao F, Feng X, Ma T (2013) Occurrence of multi-oocyte follicles in aquaporin 8-deficient mice. Reprod Biol Endocrinol 11:88. doi:10.1186/1477-7827-11-88
Suzuki Y, Ohtsuyama M, Samman G, Sata F, Sato K (1991) Ionic basis of methacholine-induced shrinkage of dissociated eccrine clear cells. J Membr Biol 123:33–41
Takeda K, Akira S (2004) TLR signaling pathways. Semin Immunol 16:3–9
Towne JE, Krane CM, Bachurski CJ, Menon AG (2001) Tumor necrosis factor-alpha inhibits aquaporin 5 expression in mouse lung epithelial cells. J Biol Chem 276:18657–18664
Tsubota K, Hirai S, King LS, Agre P, Ishida N (2001) Defective cellular trafficking of lacrimal gland aquaporin-5 in Sjögren’s syndrome. Lancet 357:688–689
Tsukaguchi H, Shayakul C, Berger UV, Mackenzie B, Devidas S, Guggino WB, van Hoek AN, Hediger MA (1998) Molecular characterization of a broad selectivity neutral solute channel. J Biol Chem 273:24737–24743
Tsukaguchi H, Weremowicz S, Morton CC, Hediger MA (1999) Functional and molecular characterization of the human neutral solute channel aquaporin-9. Am J Physiol-Renal Physiol 277:F685–F696
van Lieburg AF, Verdijk MA, Knoers VV, van Essen AJ, Proesmans W, Mallmann R, Monnens LA, van Oost BA, van Os CH, Deen PM (1994) Patients with autosomal nephrogenic diabetes insipidus homozygous for mutations in the aquaporin 2 water-channel gene. Am J Hum Genet 55:648–652
Varadaraj K, Kumari SS, Mathias RT (2010) Transgenic expression of AQP1 in the fiber cells of AQP0 knockout mouse: effects on lens transparency. Exp Eye Res 91:393–404
Vege S, Nance S, Kavitsky D, Li X, Horn T, Meny G, Westhoff CM (2013) An AQP1 allele associated with co(a-b-) phenotype. Immunohematology 29:1–4
Verkman AS (2005) Novel roles of aquaporins revealed by phenotype analysis of knockout mice. Rev Physiol Biochem Pharmacol 155:31–55
Verkman AS, Hara-Chikuma M, Paradopoulos MC (2008) Aquaporins—new players in cancer biology. J Mol Med 86:523–529
Wellner RB, Baum BJ (2001) Polarized sorting of aquaporins 5 and 8 in stable MDCK-II transfectants. Biochem Biophys Res Commun 285:1253–1258
Wellner RB, Hong S, Cotrim AP, Swaim WD, Baum BJ (2005) Modifying the NH2 and COOH termini of aquaporin-5: effects on localization in polarized epithelial cells. Tissue Eng 11:1449–1458
Wellner RB, Redman RS, Swaim WD, Baum BJ (2006) Further evidence for AQP8 expression in the myoepithelium of rat submandibular and parotid glands. Pflugers Arch 451:642–645
Woo J, Chae YK, Jang SJ, Kim MS, Baek JH, Park JC, Trink B, Ratovitski E, Lee T, Park B, Park M, Kang JH, Soria JC, Lee J, Califano J, Sidransky D, Moon C (2008) Membrane trafficking of AQP5 and cAMP dependent phosphorylation in bronchial epithelium. Biochem Biophys Res Commun 366:321–327
Woo J, Lee J, Kim MS, Jang SJ, Sidransky D, Moon C (2008) The effect of aquaporin 5 overexpression on the Ras signaling pathway. Biochem Biophys Res Commun 367:291–298
Yadav BK, Oh SY, Kim NK, Shin BS (2014) Association of rs2075575 and rs9951307 polymorphisms of AQP-4 gene with leukoaraiosis. J Stroke Cerebrovasc Dis 23:1199–206
Yang B, Folkesson HG, Yang J, Matthay MA, Ma T, Verkman AS (1999) Reduced osmotic water permeability of the peritoneal barrier in aquaporin-1 knockout mice. Am J Physiol 276:C76–C81
Yang F, Kawedia JD, Menon AG (2003) Cyclic AMP regulates aquaporin 5 expression at both transcriptional and post-transcriptional levels through a protein kinase A pathway. J Biol Chem 278:32173–32180
Yao C, Purwanti N, Karabasil MR, Azlina A, Javkhlan P, Hasegawa T, Akamatsu T, Hosoi T, Ozawa K, Hosoi K (2010) Potential down-regulation of salivary gland AQP5 by LPS via cross-coupling of NF-kappa B and p-c-Jun/c-Fos. Am J Pathol 177:724–734
Yasui M, Hazama A, Kwon T-H, Nielsen S, Guggino WB, Agre P (1999) Rapid gating and anion permeability of an intracellular aquaporin. Nature 402:184–187
Zardoya R (2005) Phylogeny and evolution of the major intrinsic protein family. Biol Cell 97:397–414
Zeng W, Lee MG, Muallem S (1997) Membrane-specific regulation of Cl channels by purinergic receptors in rat submandibular gland acinar and duct cells. J Biol Chem 272:32956–32965
Zhao D, Qian L, Verkman AS (2006) Mouse model of inducible nephrogenic diabetes insipidus produced by floxed aquaporin-2 gene deletion. Am J Physiol Renal Physiol 291:F465–472
Acknowledgments
Parts of this review are based on studies conducted in the Department of Molecular Oral Physiology, Institute of Biomedical Sciences, Tokushima University (formerly, Institute of Health Biosciences, The University of Tokushima), Japan. The author appreciates deeply the laboratory staff and graduate students who participated in the project, as well as the Ministry of Education, Culture, Sports, Science, and Technology, Japan, for having supported the project for many years. The author would like to acknowledge Professor Y. Seo, Dokkyo Medical University School of Medicine; Professor K. Inenaga, Kyushu Dental University; Dr. M. Murakami, National Institute for Physiological Sciences; and Dr. T. Nakahari, Osaka Medical College, for collaboration in some of the studies cited and for thoughtful discussion regarding the water transport mechanism. The author also expresses his gratitude to Dr. Larry Frye for reviewing this article and gives thanks to all other people who contributed to the project.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hosoi, K. Physiological role of aquaporin 5 in salivary glands. Pflugers Arch - Eur J Physiol 468, 519–539 (2016). https://doi.org/10.1007/s00424-015-1749-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-015-1749-6